Abstract
Innovations in the field of long-acting injectable drug development are increasingly being reported. More advanced in vitro and in vivo characterization can improve our understanding of the injection space and aid in describing the long-acting injectable (LAI) drug’s behavior at the injection site more mechanistically. These innovations may enable unlocking the potential of employing a model-based framework in the LAI preclinical and clinical space. This review provides a brief overview of the LAI development process before delving deeper into the current status of modeling and simulation approaches in characterizing the preclinical and clinical LAI pharmacokinetics, focused on aqueous crystalline suspensions. A closer look is provided on in vitro release methods, available biopharmaceutical models and reported in vitro/in vivo correlations (IVIVCs) that may advance LAI drug development. The overview allows identifying the opportunities for use of model-informed drug development approaches and potential gaps where further research may be most warranted. Continued investment in improving our understanding of LAI PK across species through translational approaches may facilitate the future development of LAI drug products.
Graphical Abstract

Similar content being viewed by others
Introduction
Long-acting injectable (LAI) drugs have revolutionized the field of chronic disease treatment, as a class of formulations for which administering a single dose intramuscularly (IM) or subcutaneously (SC) may result in stable drug substance release for a duration ranging from weeks (olanzapine, ZYPREXA RELPREVV (1)) to months (paliperidone palmitate, INVEGA HAFYERA (1)). This interesting approach may enable oral medication burden reduction, thereby enhancing patient adherence to treatment, improving efficacy, and reducing adverse effects and disease relapse due to missed doses (1, 2). Additional benefits may be a reduction of peak to trough plasma concentrations due to the slow release rate of LAI formulations, potentially improving safety and tolerability, as well as increasing bioavailability for compounds with a large first-pass effect. The use of LAIs could be an option to prevent drug–drug interactions (DDIs) occurring at the gastrointestinal level (3). The long study duration for LAIs in both the preclinical and clinical development space to study the extended therapeutic coverage has pushed an increased interest in applying in silico approaches, or a model-based framework, to support early selection of molecules and formulations (2, 4,5,6). With several innovations being reported in the field, modeling and simulation increasingly contribute to reducing and replacing animal studies, supporting formulation design, and enhancing the mechanistic understanding of the physiological processes contributing to the observed pharmacokinetic (PK) profile (5,6,7,8). Moreover, modeling and simulation can support managing drug–drug interactions and studying the PK in special populations (3).
This review provides an introductory framework to modeling and simulation of long-acting injectables intended for systemic delivery, with a focus on preclinical and clinical PK.
The focus is on small molecules formulated as aqueous crystalline API suspensions. While there is overlap for other LAI formulation platforms as well as local delivery technologies in terms of model-based drug development approaches, they are out of scope for this article.
Even though significant progress has been made and a variety of LAIs have been commercialized over the past decades, significant challenges remain in how to streamline the development of safe and effective LAIs. The challenges and opportunities related to the mechanistic understanding of underlying processes contributing to the LAI observed PK profile, the utility and use of modeling and simulation in the drug development process, and translation from preclinical species to human are discussed in this review.
Clinical Development Strategy of Long-Acting Injectables
There has been a growing interest in and attention to the benefits long-acting injectables could provide to patients and caregivers (2, 9). Existing oral drug substances may be re-developed into new formulations aiming at extended systemic drug concentrations to provide new treatment options for patients. This has resulted in the predominance of new reformulations over new molecular entities (NME) (i.e., the drug substance is a new chemical substance that is marketed for the first time) for LAI marketed products (2, 9). In this approach, one can use the available information on clinical PK and preclinical and clinical safety to guide the development journey of the drug product. The field is however changing, and an increased number of NMEs are being developed with specific use as LAI only (1, 2, 9). This approach allows, in contrast to the strategy of developing new formulations for existing chemical entities, optimization of the physicochemical and PK property space towards a favorable combination of low clearance, ultra-high potency, and optimal release properties. Compared to the reformulation of existing oral products, screening of compounds for development as LAI only entails having to select the most promising compounds based on limited data only available in discovery. To date, limited in silico and in vitro screening tools tailored to LAI are available; however, recently potential approaches are being reported to the field based on in vitro data and preclinical data (5, 6). Which of the two strategies would result in the most time and cost-efficient development timelines is unclear to date. This may depend on how challenging the development of the immediate-release formulation would be. Another consideration is if the immediate-release formulation is needed to reach steady-state exposures in a relatively short time frame, i.e., to have an oral lead-in phase followed by administration of the LAI product (3, 9, 10). The immediate-release formulation may be preferable to address safety concerns before administering the LAI if the LA product cannot be withdrawn once administered (9, 10). Otherwise, the drug would persist in the systemic circulation which is a concern in the event of an adverse reaction and potential DDIs (9, 10). However, there is no regulatory guidance or prerequisite that mandates an oral formulation development before LAI development. Potentially other types of LA formulations (implants, microneedle patches) could allow a system to reach the desired plasma concentration more rapidly, while simultaneously providing an option of removal and discontinuing the exposure (11, 12). The contraceptive implants wherein the drug substance may be prodrugs or active metabolites are examples of LA administration without requiring an oral formulation (13). The decision on developing such oral formulation before the LAI when the commercial intent is LAI formulation only should be based on careful assessment of the time, resource, and opportunity cost involved in choosing whether to go directly for LAI development.
For both strategies, other safety-related concerns unique to LAIs, such as local tolerability, burst release leading to peak concentrations, and the necessity for long washout period when exposure would need to be reduced, still need to be characterized (9). Developing an existing oral drug substance into a LAI allows leveraging available PK and safety data from the oral product to shorten LAI development times (9). However, absorption, distribution, metabolism, and excretion (ADME) and safety properties should still be investigated and should be sufficiently similar to allow this potential reduction in time. The development of an entirely new LAI prodrug (i.e., an NME, not derived from an existing oral drug substance) is also a potential option.
LAI Design Space: Drug Substance and Drug Product Features
Drug Substance Features for LAI Development
The design of LAIs differs from that of other types of injectables or from oral drug products. For a drug substance to be potentially in scope for LAI development, different criteria should be considered and compared to the target product profile (2, 14):
-
Potency: the potency of a drug candidate against a target indication should be high and is of importance because of maximum dose and volume limitations for injection (subcutaneously less than 2 ml per injection site, intramuscularly up until 5 ml per injection site (1)).
-
Clearance pathways: the total clearance of the drug candidate should be low to enable sufficiently high concentrations for therapeutic efficacy in view of dose limitations and administration requirements. In addition, the drug substance should be metabolically stable at the injection site.
-
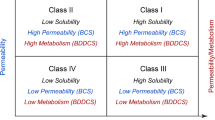
Physicochemical properties: the drug’s physicochemical properties (e.g., pKa, lipophilicity, molecular weight, solubility in aqueous/organic media, solubility at the injection site, intrinsic dissolution rate) are critical properties that can impact the in vivo release and absorption kinetics as well as the compatibility with the injection medium and formulation technology. Slow, steady release kinetics may be investigated to reach prolonged exposures but are not straightforward to obtain and control and can be impacted by both formulation and physiological parameters. As illustrated by Shah et al. (5), a low solubility and slow intrinsic dissolution rate are preferred for a prolonged release when formulated as a crystalline suspension. The development of a prodrug or different form can be considered to improve physicochemical properties for an LAI (9). An example of this approach was the development of paliperidone palmitate, a prodrug of paliperidone with extremely low water solubility, which dissolves slowly at the injection site and is then hydrolyzed to paliperidone to become available for absorption (15). For large molecules, systemic absorption into the vascular system is restricted, and lymphatic absorption can become dominant (8). Furthermore, interactions with the local tissue should be considered.
-
Stability in drug product and during manufacturing (sterilization process, …).
-
Safety and local tolerability at the injection site.
Early, preliminary assessments of these properties starting from drug discovery stages may support molecular design, compound selection for LAI development, and the selection of appropriate formulation platforms.
Drug Product Features and LAI Formulation Technologies
Figure 1 displays an overview of characteristics of FDA approved LAI drug products from Li et al. (11). Most drug products were reported to be based on “dissolution-based formulations,” biodegradable systems, or non-degradable implants. “Dissolution-based formulations” are formulated as crystalline suspensions of slowly dissolving drug particles, either in nano- or micrometer range, in aqueous or oily vehicles. Their release depends largely on drug substance properties, such as solubility and particle size, and the interaction of the formulation with the physiology. Crystalline suspensions can allow high drug loadings, and they are applicable mostly to poorly soluble compounds (11). To date, tailoring their release rate is not straightforward. The development of a prodrug can be a strategy to alter the physicochemical properties of a drug substance and allow administration as a suspension (9). Alternatively, controlled-release formulations can be developed, e.g., via encapsulation in biodegradable polymer systems or in non-degradable implants, formed either prior to injection or in situ. The drug release can, for the former case, be altered via the degradation mechanisms of the polymer and diffusion through the matrix or, for the latter case, via release from the implanted device (11). Biodegradable polymer systems allow tailoring the drug release duration, with commercial products spanning weeks up to 6 months, but are more limited in drug loading/maximum dose and involve a more complex manufacturing process. Similarly, non-degradable implants enable modulation of the drug release but need to be removed from the site of injection afterwards. A detailed overview of different controlled-release formulation technologies developed for LAI applications falls outside of the scope of this article and is covered in several review articles (2, 11, 14, 16). Nguyen et al. provided an overview of marketed intramuscular administered aqueous suspensions (17) with more detailed discussion around the dose, formulation specifications such as drug and excipients concentrations and suspension particle size diameter, and drug physicochemical properties. Moreover, examples of intramuscularly administered aqueous suspensions in development are described.
Characteristics of FDA-approved products with long-acting drug delivery. a Type of release mechanism for different long-acting delivery formulations, b durations of release for at least 1 month up to 6 years, and c various formulation approaches and dosage forms. (Figure from Li et al. (11))
Different biopharmaceutical aspects need to be accounted for during the selection of a suitable formulation platform for parenteral administration: (a) The platform and excipients must be compatible with the drug substance and provide sufficient physical and chemical stability during manufacturing and “throughout the drug product shelf life.” Drug products must be homogeneous and resuspendable. (b) The syringeability and injectability should be adequate to allow efficient injection into the subcutaneous or intramuscular space. (c) The drug load can be an important aspect to keep the injection volume below acceptable limits when needing to administer higher quantities of drug. (d) Drug product features can impact the release and absorption rate of drug. Although in vivo absorption kinetics are complex, the formulation selection can be a strategy to alter the release (5, 17,18,19). (e) The choice of technology and excipients can affect the immune response, and their impact on tolerability should be evaluated (19,20,21).
The Interplay Between Formulation-Controlled and Physiology-Controlled Elements
Drug release from LAI depot formulations is complex, and the mechanisms governing drug release and absorption in vivo are multiple. These involve elements that are related to the physico-chemistry of the drug itself, the combined formulation properties, and the physiology at the site of administration (17, 22, 23). Typically, it is the drug and formulation characteristics, which are often assumed to drive the drug release, that receive most attention in drug discovery and during chemistry, manufacturing, and controls (CMC) development. These parameters constitute handles which can be quantified and tweaked in an iterative process. Conversely, the interaction between the LAI drug delivery system and the physiological conditions at the injection site should not be overlooked. Based on a number of animal studies, it is generally assumed that drug absorption from SC or IM poorly soluble drug depots is mainly driven by the drug release rate from the dosage form, rather than being limited by permeation or vascular perfusion (24, 25). However, the release process in itself can be very complex and is believed to be intimately linked with, and influenced by, the local physiology (e.g., site-specific differences with regard to pH, interstitial fluid composition and flow, and other factors influencing solubility) and the evolving properties of the formulation depot and the tissues at the injection site (Fig. 2) among other variables (22, 26,27,28,29,30).
Schematic of possible mechanisms affecting the pharmacokinetics after IM or SC administration of long-acting injectable products (Figure from Medlicott et al. (26))
The host response to LAI depot formulations has been the subject of growing research interest in the past decade, especially in the field of aqueous nano- and microsuspensions of crystalline drug (20, 31). The IM or SC injection of crystalline drug suspensions, with long in vivo residence times, elicits what is generally called a foreign body reaction at the site of injection (32, 33). A foreign body reaction is an innate host response to non-self (bio)materials aiming at confining and/or removing solid materials from the body. This is a universal response (at least in most mammals), which, when occurring in a controlled fashion, is tolerated and is in fact beneficial to the host (34).
Aqueous suspensions have been the focus of detailed mechanistic investigations in animal models (1, 18, 25, 33, 35). For instance, upon IM/SC injection of a LAI suspension, individual drug particles and the formulation depot as a whole will typically be recognized as non-self. The body’s natural response is to contain the materials and, when able to, to break down the drug depot. This occurs through a localized inflammatory reaction (e.g., edema, macrophage infiltration, depot encapsulation, fibrosis), of which the exact attributes (i.e., type, extent, and kinetics of the host response) depend in part on formulation properties (e.g., particle size and excipients). Often, macrophages will be attracted in large numbers to the injection site, after which they will gradually infiltrate the LAI suspension depot. In doing so, macrophages have been shown to internalize large amounts of drug particles intracellularly through phagocytosis (20, 25, 31, 36). As a result, over time, the drug release mechanism will shift from purely dissolution-driven flip-flop kinetics to a more intricate drug release process that consists of a combination of extracellular and intracellular dissolution, passive permeation from within macrophages to the extracellular compartment, and passive diffusion and lymphatic drainage among other processes, before being absorbed systemically.
Clinical observations of the local tolerability to SC/IM LAIs correlate well with the injection site reactions that have been reported with different LAI nano-/microsuspensions in several preclinical animal species (incl. rats, dogs, and nonhuman primates) (19, 25, 31, 33, 35, 37,38,39,40,41,42). The role of local inflammation and the impact of macrophages on drug release from LAI nano-/microsuspensions (i.e., assuming typical particle size range and formulation compositions) may therefore be expected to be similar in animals and in humans. Nonetheless, some differences in injection site reaction profiles (e.g., the precise rate and extent of the cellular infiltration) and in flip-flop PK after injection of LAI suspensions could be influenced by (i) species-related differences in anatomy and physiology (22, 26, 30, 35); (ii) differences related to injection site, injection procedure, and dose effects (22, 26, 30, 35, 43,44,45); and (iii) different drug, particle, and formulation properties (21, 22, 32, 46,47,48).
In Vivo Evaluation of LAIs, Pharmacokinetic Assessment, and Translation from Animal to Human
The observed in vivo PK of LAI drug substances is complex, resulting from an interplay of formulation-controlled and physiology-controlled elements. In the multiphasic PK profile of a LAI suspension (Fig. 3a), first, an initial absorption phase can be discerned which is attributed to drug substance and formulation factors and is linked to dissolution rate (Fig. 3b). This fast initial absorption phase needs to be accommodated to avoid an unacceptable spike in the plasma concentrations. The LAI PK profile gradually progresses to the slow-release terminal phase which is characterized by flip-flop PK (3, 49, 50), resulting from the absorption rate being slower than the elimination rate (in contrast to typical PK in which the elimination rate is slower than the absorption rate). This is reflected in the LAI PK profile by an unchanged terminal slope when clearance changes (Fig. 3c), since the slope reflects the absorption rate. This terminal phase is assumed to result from the dynamic depot characteristics at later stages after dosing and likely influenced by the injection site reaction capable of modulating the drug release (Fig. 3d), as described in the previous section. There may be an intermediate lag phase observed as well, which presents as a second maximum in the PK profile (Fig. 3a) before the largest fraction of the dose is released in the terminal phase. This second bump is however not always present, and factors that determine the peak concentration in this bump are not clear to date (20, 51). Similar PK parameters compared to oral drug products are characterized, such as Cmax, area under the curve (AUC), and extent of release (based on exposure expressed as AUC and comparing to exposure after IV dosing) (1, 6, 50). However, in a complex LAI PK profile with multiple peaks, peak concentrations in the different phases of the PK profile could be of interest to be characterized, especially when Cmax is not located in the initial fast absorption phase. In addition, the release rate from the depot is derived from the PK profile.
a Illustration of a multiphasic PK profile of a LAI crystalline suspension. b The influence of changing the dissolution rate on the initial fast absorption phase. c The influence of changing the clearance on the LAI PK profile under flip-flop pharmacokinetics. d The influence of the injection site reaction capable of modulating the drug release rate
The gaps in the mechanistic understanding of the different processes after IM or SC injection in both preclinical species and human and their relative contribution in each of the different phases result in a challenging deconvolution of the LA PK profile. To date, this poses a burden on making an informed choice of the preclinical model(s) to study LAI PK and the translation of those preclinical data to support formulation development and human dose simulations (6). More specifically, the influence of the following elements on the choice of the preclinical model(s) is not clear to date:
-
Interspecies similarities and differences in injection site physiology and inflammatory response
-
PK parameter of interest: extent of burst release, peak concentrations in the different phases of the PK profile, the release rate from the in vivo depot, and extent of release (based on exposure expressed as AUC and comparing to exposure after IV dosing)
-
IM versus SC administration
-
Studying LA PK versus studying local tolerability
-
Effect of factors such as dose, dose volume, and drug concentration
For subcutaneous administration, it is often suggested that the minipig is considered as the most appropriate translational preclinical model, based on the observation that the structure of the hypodermis of minipigs is the most similar to human compared to other species (52, 53). It is however unclear if this is also the case for the underlying physiological processes and translation of LAI PK parameters.
Recently, a comprehensive overview was published of the preclinical species that have been used in the development of marketed LAI products, which are similar to the ones used in oral drug product development: mouse, rat, rabbit, dog, minipig, and monkey (1). Since to date there is no clarity on the most predictive preclinical species, it is difficult to derive the rationale for each of the marketed products. Bauer et al. assumed the choice of the animal model(s) was determined by considerations such as the chosen preclinical efficacy model or trade-offs such as cost versus drug development stage (1). In non-rodent species, clinically relevant volumes can be injected; however, in early LAI formulation screenings, rodent species in which smaller volumes need to be injected are preferred because of ethical considerations (1). Another published review of animal and human PK of LAI suspensions after IM injection of aqueous crystalline API suspensions (17) was conducted to identify the factors that influence in vivo formulation performance, such as suspension’s particle size effect, dose effect, suspension strength, stabilizing excipient, and drug lipophilicity. The influence of the specific IM administration site on the drug exposure and the effect of variables such as gender and BMI were also explored (17). For LAI aqueous suspensions, a first report was presented by Johnson et al. for simulating the human dose based on preclinical data in dog and rabbit (6). In the PK dataset comprising seven compounds, the effects of dose, suspension particle size, route of administration, and injection location on LAI PK were investigated. Two different approaches were applied and compared: a constant 0-order release input rate approach and a preclinical LAI PK input rate deconvolution method. When approaching the clinical LAI doses via a constant IV infusion approach, clinical doses were underpredicted 2- to fivefold. For simulations aimed at covering the target concentration for 1 month or less, based on the LAI PK input rate deconvolution approach from dog or rabbit to human, human input rates and dose estimates were simulated within about a threefold margin. However, it was shown that simulations for longer coverage of the target concentration and of human Cmax values proved to be challenging. Furthermore, there was no clear indication for either rabbit or dog data to be more predictive for clinical PK profiles (6). Continued investment in characterizing interspecies similarities and differences between LAI PK parameters and human dose simulation approaches may facilitate formulation development.
Perspectives on the Modeling and Simulation Field: Where Are We Now, Where Should We Be Heading?
The early clinical development of LAIs follows a similar path as oral therapies—beginning with a clinical assessment of the drug safety, tolerability, and PK in healthy volunteers before evaluation in target patient population. The development of LAIs in this phase may often be expensive since the assessment of safety and exposure could span over weeks to months with single dose and even longer with repeat dose settings. Nevertheless, these data are critical to design the clinical program. Model-informed drug development (MIDD) is an approach that integrates information from in vitro, preclinical, and clinical studies into a mathematical model-based framework to support development (9). The MIDD approach has come a long way since the early 1990s and is now an integral part of drug discovery and development with ever expanding applications, also entailing in vitro–in vivo correlations (IVIVCs) (4). The MIDD framework has been sought to bring more efficiency and expediency in the development of LAIs. Moreover, the utility of implementing model-based approaches in development of LAIs is well recognized by the regulatory agencies. There is an ongoing effort by USFDA including allocation of research grants to further explore potential of various modeling and simulation approaches to aid the clinical development and regulatory decision-making for LAIs (54). These efforts encompass areas from real time and accelerated dissolution methods to IVIVC approaches and developing model informed BE evaluation strategies for LAIs.
A modeling and simulation framework may support the LAI drug development in different areas, i.e., to
-
a)
Simulate early LAI dose projections based on preclinical and human extrapolated target efficacious concentrations, clearance, and drug release rate using empirical PK models.
-
b)
Simulate the desired exposure above the hypothesized efficacious concentration and below the hypothesized toxic concentration in chronic treatment, e.g., using empirical PBPK or Pop-PK models.
-
c)
Simulate if lead-in oral treatment might be necessary to reach steady-state exposures within an acceptable time frame and put forward a potential replacement strategy from the current administration route to the SC or IM LAI treatment, e.g., using Pop-PK models.
-
d)
Guide LAI formulation development and the design of clinical studies, e.g., using Pop-PK models or semi-mechanistic biopharmaceutical models.
-
e)
Aid in the design and validation of clinically relevant dissolution methods, build a safe space, and set drug product specifications, e.g., via in vitro–in vivo relationships (IVIVRs) and mathematical correlations (IVIVCs) (55). FDA guidelines exist for the development and evaluation of IVIVCs for extended-release formulations for oral administration (56); however, such IVIVC guidance are not currently available for LAI products. IVIVCs make use of numerical deconvolution, whereas mechanistic approaches aim at simulating the individual absorption and disposition processes.
-
f)
Potentially wave clinical trials (completely or reducing their scope), e.g., using Pop-PK models or IVIVCs.
The complex interplay between formulation and physiological processes for LAI drug products renders the development of correlations, and the implementation of models challenging and to date clinical assessment is still needed. Several LAI PK modeling and simulation approaches have been explored in the field to attempt to describe the irregular shape of the PK profile of LAIs. This section provides an overview of empirical and biopharmaceutical in silico models and mathematical IVIVCs.
Empirical Models
Empirical PK models generalize the drug disposition scheme into simplified compartmental structures. These have no anatomical or direct physiological significance, but are solely defined to empirically describe the observed PK profiles. Both the parameters (e.g., rate constants) and the structure (e.g., the compartments) are derived from fitting the experimental data (i.e., a posteriori definition of model structure and parameters). These models are routinely applied in the (pre-)clinical drug development and can provide many useful insights, though remain descriptive in nature.
In the case of LAI drug delivery, the LAI PK may be captured by one/two/multi-compartment modeling and/or population PK approaches, by applying parallel zero-order and first-order release (15, 45, 57), parallel fast and slow first-order release (19), or using convolution-based modeling approaches (58,59,60). The various modeling approaches listed here serve different purposes and are not necessarily interchangeable. The choice of using any of the described modeling approaches will be driven by the intended application of the analyses.
Empirical Long-Acting Pop-PK Models
Population PK modeling is a tool to describe the time course of observed drug exposure in subjects and to study sources of variability in this exposure, evaluating data from all individuals in a population simultaneously using a nonlinear mixed effects model (61). In a clinical setting, population PK models could potentially provide a first indication of the LAI dose resulting in PK profiles with comparable exposure when switching from oral treatments (62). However, to date developing these models does require LAI clinical data (15, 57, 62). When these clinical data are available, the model-based framework could help in assessment of trial designs, different dosing regimens, and study sample sizes for potential PK-based BE assessments (61, 63). The models developed with clinical LAI data may support characterizing the complex absorption profiles specific to the LAI being evaluated. Most Pop-PK approaches utilize empirical models to describe these formulation-specific release rates and absorption profiles and assess the impact of formulation-related variables such as injection volume, dose strength, formulation concentration on drug PK (45). These models assist in understanding the variability across subjects and how that may impact the clinical systemic drug exposure (64). The models need to be updated with new data in an iterative manner. Moreover, the impact of formulation characteristics on drug exposure may also be studied with such framework in presence of clinical study data (65).
Convolution-based approaches have been implemented and compared to the more traditional population approach resulting in similar ability to characterize LAI PK (15, 45, 57, 66). The convolution-based approach convolves an input function with a disposition and elimination function to describe the drug concentration time profile. The input and disposition functions are often described by parametric models (58). Gomeni et al. stated that the convolution-based approach could potentially be extended into an IVIVC framework. Establishing mathematical links between in vitro dissolution rates and in vivo absorption rates may facilitate drug formulation property developments (59). Finally, a response surface analysis could be employed to optimize specific parameters that drive the drug exposure and subsequent effect (60, 65). While use of these model-informed drug development approaches may expedite to some extent the development of LAIs by obviating the need to study every formulation, release profile, and dosing regimen, these approaches do not remove the need to, as applicable, study multiple LAI formulations, release profiles, and dosing regimens. There is a great deal of art to translate the learnings as one progresses through the development cycle. In vitro, preclinical and clinical data need to be generated to allow building these models and evaluating formulations. Bridging the gap from the in vitro and/or preclinical space to the clinic is complex and calls for the evaluation of multiple LAI formulations in vitro and in vivo.
Darville et al. (19) constructed a two-compartmental absorption model, coupled to a one-compartmental disposition model, to simulate the release and absorption for small-molecule crystalline paliperidone palmitate suspensions after IM injection in rats (Fig. 4a). A parallel absorption process was proposed based on the observed biphasic in vivo profiles: an initial absorption process from the dissolution of API immediately after injection and a second, slow absorption process governed by macrophage infiltration and release of drug particles. The long-term terminal PK profiles were dominated by the second, slower release and absorption process. As shown in Fig. 4, simulated PK profiles yielded good model fits for the observed data.
a Proposed model describing the PAL PK following a single IM injection of PP-LAI in the rat. Ka1 and ka2 contain first-order absorption rate constants for the fast and slow absorption process, respectively. b Visual predictive checks for the ln-transformed paliperidone (PAL) plasma concentration–time data by different study treatments. Open circles: observed data; solid black line: median population prediction; gray area: 90% prediction interval for virtual population simulations. (Figures from Darville et al. (19))
The population PK modeling of clinical data allows characterizing the systemic profiles and potentially proposes different dosing regimens that may achieve a specific target exposure metric. Within a FIH stetting, the single dose data can be modeled for repeat dose settings. The impact of using an oral lead-in, dose holidays, etc. may be simulated via Pop-PK models. These models may also provide a reasonable starting point for dose assessments in other populations, e.g., pediatrics. They may allow in silico evaluation of impact of differences in physiological factors on drug exposure. One example is to assess the changes in absorption rate when dosing children who may present differences in available muscle mass and adipose tissue. It is important to remember that adequate clinical data at different doses and sufficient duration may be needed to have a robust Pop-PK model that can be used to simulate different dosing regimens.
Empirical Long-Acting PBPK Models
Currently, there is often insufficient information to construct a fully mechanistic bottom-up physiologically based pharmacokinetic (PBPK) model for LAIs. Consequently, reported LAI PBPK models described the administration site empirically with a zero-order or first-order input function to the systemic PBPK model, exemplified in Fig. 5. Hence, such “empirical long-acting PBPK models” utilize a PBPK drug disposition description, linked to an empirical description of the long-acting kinetics. They are useful in leveraging existing clinical PK data from the oral drug product in supporting LAI development, e.g., to simulate potential drug–drug interactions (DDIs) with concomitant medications based on clinical DDI data following oral administration. Moreover, they can be used to study the application of LAIs to prevent DDIs occurring at the gastrointestinal level (3). Rajoli et al. demonstrated the use of PBPK when re-developing existing oral drug molecules for novel use as LAI in the field of HIV antiretroviral therapy and tuberculosis, in both adult populations (67,68,69,70) and children and adolescent populations (71). For anti-tuberculosis agents, the PBPK model simulated which combination of dose and release kinetics would be required by a theoretical formulation or device. For instance, to allow once monthly intramuscular dosing for delamanid and rifapentine and to show for bedaquiline and isoniazid rather weekly to biweekly administration would be necessary (68). Furthermore, the same group reported the use of PBPK to determine dose and release rate combinations following monthly IM injections of antiretrovirals formulated as solid drug nanoparticles (67), after intradermal delivery via microneedle array patches (70, 72) and for a SC implant (73). For the application of PBPK in DDI assessments between long-acting and oral drug products, clinical DDI data following oral administration were used in modeling co-medication of antiretrovirals cabotegravir and rilpivirine as long-acting IM injections and oral rifampicin. Available PBPK models simulated that coadministration would result in subtherapeutic concentrations of both cabotegravir and rilpivirine caused by the induction potential of rifampicin (3, 69, 74), showing in this case example, bypassing the gastrointestinal tract did not mitigate the DDI concern (3).
Example of a whole-body PBPK model to which a compartment was added to define the intramuscular depot and the blood capillaries surrounding the IM depot, describing the pharmacokinetics of injectable LA formulations using an empirical first-order release approach. IM, intramuscular; LV, left ventricle; RV, right ventricle. (Figure from Rajoli et al. (67))
A more mechanistic PBPK approach was reported by Perazzolo et al. to model the disposition in nonhuman primates of SC administered nanoparticles of HIV drugs (lopinavir, ritonavir, and tenofovir) and describe the lymphocyte-targeted slow-release features of these nanoparticles (75,76,77). Perazzolo et al. stated the nonhuman primate lymphatic network architecture can be adjusted to represent the human system, therefore providing the opportunity for human dose simulations.
Towards Biopharmaceutical LAI Models
Biopharmaceutical Considerations
Fully mechanistic in silico models apply a bottom-up approach to simulate the PK. They have been applied to support oral applications to model the absorption processes and support drug product development, to identify potential critical bioavailability attributes, and to help in setting clinically relevant specs (78, 79). PBPK models rely on a description of the physiology and behavior of the drug and formulation after administration as well as on in vivo relevant in vitro input data. However, the behavior of LAI formulations post-injection is more complex, and the development of in vitro methods together with mechanistic models is still an emerging area (14). The absorption process depends on a complex interplay between formulation, drug characteristics, and the local physiology at the injection site (17, 80). The mechanism of drug release strongly depends on the formulation technology. In case of crystalline suspensions, it is governed by a slow and gradual dissolution of often poorly soluble drugs. Parameters such as particle size and stabilizing excipients can therefore affect the release (18, 24). In addition to the release mechanism of the formulation itself, the local physiology, metabolism, and host response need to be accounted for.
A recent review article by Dubbelboer et al. (80) highlighted the increased activity over the past decade in developing PBPK models for SC administrations. The development of mechanistic models for biopharmaceutical applications consists of 3 key parameters (81): (i) providing a mechanistic framework to describe drug absorption, (ii) developing an in vivo relevant in vitro drug release method, and (iii) the availability of PK data for model development and validation. These parameters are illustrated specifically for LAI applications in Fig. 6. The available knowledge and biopharmaceutical tools for LAI drug products are not as advanced as for oral products, and the implementation of mechanistic models can aid in increasing the level of understanding and support the design of in vitro setups.
In Vitro Release Methods
Mechanistic models aim at capturing the interplay between physiology and formulation properties to assess the potential in vivo performance. These models should include the mechanisms of drug release and absorption that are relevant to the interaction between drug product and physiology. Key elements to the successful development of mechanistic models are therefore a thorough mechanistic understanding of the factors that limit release and absorption as well as the availability of in vivo relevant in vitro dissolution methods that capture these mechanisms of drug release (78, 81).
Given that the field of LAIs is emerging, guidelines for the design and use of in vitro dissolution methods are limited. Recommended dissolution methods by the US FDA for LAI aqueous suspensions include compendial USP apparatus II (paddle) and IV (flow-through) using buffer media with the potential addition of surfactants or solvents (82). USP recently published a draft informational chapter on “In vitro release test methods for parenteral drug preparations” (83). In certain cases, compendial release methods have shown to enable discrimination between formulation parameters such as particle size or different stabilizing polymers for LAI aqueous suspensions (18, 84). The USP IV apparatus offers a more dynamic environment and may be more suitable for extended-release formulations. Furthermore, adapted designs, including donor-acceptor compartments, dialysis systems, and adapters, were developed to simulate depot volumes and characteristics and/or slow down the in vitro release (85,86,87). The physiology of the injection space is unique, and efforts have been undertaken to capture the IM or SC matrix structure and components in in vitro release setups using synthetic gels and ex vivo tissues (8, 88,89,90). More biorelevant release methods are relevant to support formulation development as of early development stages and are still an active area of research. Their in vivo relevance should ideally be proven for multiple compounds and formulations.
Critical bioavailability attributes and in vivo release mechanisms need to be understood for successful in vitro method development. Next to the experimental conditions, the selection of medium can exhibit significant impact on the release profile as well (60, 87, 91, 92). For development purposes, capturing the complexity of biological fluids in more biorelevant media can be of importance. Several studies investigated the properties of the injection site to inform selection of temperature, pH, buffer, and composition of more biorelevant media (91, 92). Furthermore, the stability during dissolution and at the injection site may need to be evaluated in in vitro assays. Accelerated dissolution methods can be beneficial to reduce development time. However, their in vivo relevance need to be evaluated: accelerated conditions may impact the drug release mechanism and may result in a changing rank order of the performance between various formulations. The apparatus and media being used should therefore aim to capture the intrinsic release mechanisms of the drug product (60, 87, 93, 94).
In addition to the in vitro release mechanism and duration of release, the in vivo behavior in terms of depot formation, physiology, and host response further complicates the establishment of in vitro–in vivo relationships and correlations. The development of both biorelevant and clinically relevant release methods should therefore go hand in hand with modeling and an increased understanding of the in vivo factors that constitute the PK. Finally, machine learning models are finding their way to the LAI modeling space. This was recently demonstrated for the formulation design and in vitro release of polymeric LAIs, however to date not yet for LAI suspensions (95).
Semi-mechanistic Long-Acting Models
Recent papers specified the parameters that need to be accounted for to mechanistically simulate the PK of LAI formulations after IM and SC injection (17, 80):
-
Drug and formulation properties (Sect. 3): e.g., particle size, API physicochemical properties, formulation viscosity, concentration, and excipients added.
-
Parametrization of the injection space, describing, for instance, tissue and interstitial fluid composition, capillary density, and lymphatic flow.
-
Interactions between the injected drug product and the injection space, including mechanisms, such as depot formation, inflammatory response, and local metabolism, that affect the in vivo behavior and PK (19, 25).
The construction and predictiveness of mechanistic models for LAI applications are limited by two important aspects: (a) a mechanistic description of the injection space and its interplay with drug and formulation parameters and (b) the availability of biorelevant in vitro methods. Another limiting factor is the scarce published knowledge on the impact of metabolism at the injection site and related expression of enzymes and transporters in this environment. Modeling approaches therefore started more empirically, e.g., based on one-/two-compartmental absorption models (80), gradually increasing in complexity to include some of the key mechanisms listed above. In addition, models need to be trained with (pre-)clinical data to improve their accuracy. The current section distinguishes between (semi-)mechanistic models with a focus on in vitro input and PBPK models that are based on (pre-)clinical data.
In a recent publication, Shah et al. (5) presented the application of a 1-compartmental absorption model to estimate the interplay between drug potency, disposition, absorption rate, and dose. The absorption rate was simulated as a first-order process and release from a crystalline microsuspension which was assumed as a starting case. The approach could serve two purposes: First, for an early assessment of a compound’s feasibility for development as an LAI over a certain target duration. Second, the simulated in vivo release rate was compared to an in vitro release rate calculated from intrinsic dissolution rate experiments to support initial formulation development. The proposed in vitro–based model was trained with in vivo data and showed qualitative agreement for the commercial LAI products that were studied. When applying such an approach, the potential variability in release rate as well as uncertainty in potency and disposition parameters needs to be accounted for.
Several mechanisms limit the predictiveness of current mechanistic models. Injected particles can start agglomerating post-injection, resulting in much slower in vivo dissolution than simulated based on the particle size and solubility (29, 96). Furthermore, the distribution of particles in the tissue may be impacted by parameters such as particle size, shape, formulation viscosity, and added excipients. Previous studies have also illustrated an interplay between formulation parameters and the inflammatory response (18, 20), on its turn impacting the PK. The importance of accounting for the inflammatory response was outlined in the Pop-PK model of Darville et al. (12). A better understanding and parametrization of such mechanisms is needed to advance current LAI mechanistic models and increase their application space.
Mathematical IVIVCs
An alternative approach for simulating the PK and the impact of formulation variables exists in the modeling and direct implementation of in vitro data via in vitro/in vivo correlations (IVIVCs) (56). Jablonka et al. 85] characterized the in vitro release of liposomal formulations using the dispersion-releaser (DR) technology, containing a USP type 2 dissolution apparatus with a stirred donor compartment that contains the injected formulation and that is separated from the vessel by means of a dialysis membrane. In vitro release profiles were fitted by a mathematical model. Fitted release profiles were directly implemented in the PBPK model and able to qualitatively describe in vivo PK profiles in rat and human. Aiming for a more biorelevant description of the injection space, Lou et al. (8) recently developed a subcutaneous absorption and release emulator, ESCAR (Emulator of SubCutaneous Absorption and Release), comprising a SC injection chamber with simulated SC medium and connected to separate blood and lymphatic circulation chambers. In vitro release rates for different milled and unmilled aqueous suspensions were fitted with a Weibull equation and compared to in vivo rat PK profiles by means of a PBPK model. Simulated PK profiles were able to capture in vivo trends, and an IVIVC could be constructed. The same setup was used to study the potential effects of particle settling of suspensions on drug release (97).
The development of IVIVCs requires an in vitro method that captures rate-limiting factors of in vivo absorption and that is in vivo relevant (55). Given the complexity of the post-injection behavior of LAI formulations, the development of such correlations is hence not straightforward. To date, to our knowledge, only few IVIVC examples have been published (98, 99), and for LAI suspensions, only one reported example is present in the field for a preclinical rabbit model (100). The development of mechanistic IVIVRs may offer a better understanding of key mechanisms and critical bioavailability attributes. As the name suggests, a successful IVIVC may go a long way to reduce extensive clinical work when changing manufacturing sites, release rates within established safe space, … Nevertheless, developing an IVIVC model is resource intensive and needs a well-planned approach early in LAI drug development. It entails developing multiple LAI formulations with different release rates with corresponding clinical data.
Conclusion and Outlook
The intent of this review was to provide an overview of LAI development and modeling and simulation of preclinical and clinical LAI PK of aqueous crystalline suspensions. To date, LAI development is fraught with challenges irrespective of the formulation platform. These challenges are summarized in Table I.
The appearance of NMEs intended for LAI development only presents new opportunities to have drugs tailored to provide a favorable combination of low clearance, ultra-high potency, and release rate properties (2). In turn, this has led to new challenges wherein in silico modeling and simulation approaches may help guide towards potentially interesting compounds in the discovery stage.
As discussed in this article, different modeling approaches can be leveraged throughout the development process. There is often a lack of sufficient information to construct a fully mechanistic bottom-up LAI model. Modeling approaches have therefore often described the administration site (semi-)empirically, e.g., with zero-order or first-order input functions, similar to how LAI population PK models are structured. More advanced in vivo characterization and imaging can increase the comprehension of the injection space and aid in describing the drug’s behavior at the injection site more mechanistically for modeling purposes (6, 25, 101, 102). Alternative modeling approaches are also being explored, and machine learning models are entering the LAI modeling field to potentially aid in formulation design and in vitro release characterization (95).
Establishing successful in vitro–in vivo relationships may also advance mechanistic PBPK and physiologically based biopharmaceutics modeling (PBBM). Recent years have seen an increase in efforts to develop biorelevant release methods for LAI purposes (8, 85,86,87,88,89,90). Including relevant physiological complexities in such in vitro setups, aiming to describe in vivo relevant release mechanisms, may allow more in-depth investigation of the impact of formulation characteristics which, in its turn, can be included in mechanistic models. More understanding could be generated around the impact of drug substance and product properties on the drug distribution and depot formation. Furthermore, such in vitro setups may enhance the establishment of in vitro–in vivo correlations. Capturing the inflammatory response remains challenging. More understanding of the time course of the host response to the injected depot and how this influences observed release at the injection site could support a better deconvolution of the plasma PK profile and its different phases. In an ideal situation, the formulation composition could be tailored to obtain a desirable plasma LAI PK profile, with an optimal release rate and low peak to trough plasma concentrations. Finally, the development of cell-culture assays may reduce animal studies by allowing to characterize the host response in vitro (95).
Applying model-based approaches has the potential to address the challenges mentioned in Table I by bridging the knowledge gap on translating the preclinical to the clinical space (6). Such an approach would enable more effective use of in vitro methods, reducing the reliance on preclinical evaluation during drug development and improving translation to human. Support and co-development in MIDD programs by health authorities can potentially allow innovative clinical study designs with reduced clinical timelines and will facilitate future regulatory evaluation of LAI products in development (4, 9, 54, 103). The integration of the current available knowledge and identification of the areas in need of further progress, in literature and during future LAI-focused conferences, will promote future collaborative engagement with stakeholders in academia, industry, and health authorities and facilitate the development and accessibility of long-acting therapeutics.
References
Bauer A, Berben P, Chakravarthi SS, Chattorraj S, Garg A, Gourdon B, et al. Current state and opportunities with long-acting injectables: industry perspectives from the innovation and quality consortium “long-acting injectables” working group. Pharm Res. Springer. 2023:1–31.
Bassand C, Villois A, Gianola L, Laue G, Ramazani F, Riebesehl B, et al. Smart design of patient-centric long-acting products: from preclinical to marketed pipeline trends and opportunities. Expert Opin Drug Deliv. 2022:1265–83.
Bettonte S, Berton M, Marzolini C. What is the significance of the pharmacokinetic profile and potential drug–drug interactions of long-acting intramuscular cabotegravir and rilpivirine? Expert Opin Drug Metab Toxicol. 2023;19(5):243–7.
Madabushi R, Seo P, Zhao L, Tegenge M, Zhu H. Review: role of model-informed drug development approaches in the lifecycle of drug development and regulatory decision-making. Pharm Res. Springer. 2022;39(8):1669–80.
Shah JC, Hong J. Model for long acting injectables (depot formulation) based on pharmacokinetics and physical chemical properties. AAPS J. 2022;24(3):44.
Johnson AR, Ballard JE, Leithead A, Miller C, Faassen F, Zang X, et al. A retrospective analysis of preclinical and clinical pharmacokinetics from administration of long-acting aqueous suspensions. Pharm Res. 2023:1–16.
Bassand C, Villois A, Gianola L, Laue G, Ramazani F, Riebesehl B, et al. Smart design of patient-centric long-acting products: from preclinical to marketed pipeline trends and opportunities. Expert Opin Drug Deliv. 2022:1265–83.
Lou H, Hageman MJ. Development of an in vitro system to emulate an in vivo subcutaneous environment: small molecule drug assessment. Mol Pharm. 2022:4017–25.
Arya V, Hodowanec AC, Troy SB, Struble KA. Long-acting formulations for the prevention and treatment of human immunodeficiency virus (HIV)-1 infection: strategic leveraging and integration of multidisciplinary knowledge to advance public health. Clin Infect Dis. 2022;75:S498-501.
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER). Human immunodeficiency virus-1 infection: developing systemic drug products for pre-exposure prophylaxis guidance for industry. 2019.
Li W, Tang J, Lee D, Tice TR, Schwendeman SP, Prausnitz MR. Clinical translation of long-acting drug delivery formulations. Nat Rev Mater. 2022;7(5):406–20.
Chen Z, He J, Qi J, Zhu Q, Wu W, Lu Y. Long-acting microneedles: a progress report of the state-of-the-art techniques. Drug Discov Today. 2020;25:1462–8.
Croxatto HB. Progestin implants. Steroids. 2000;65:681–5.
Nkanga CI, Fisch A, Rad-Malekshahi M, Romic MD, Kittel B, Ullrich T, et al. Clinically established biodegradable long acting injectables: an industry perspective. Adv Drug Deliv Rev. Elsevier B.V.; 2020. p. 19–46.
Magnusson MO, Samtani MN, Plan EL, Jonsson EN, Rossenu S, Vermeulen A, et al. Population pharmacokinetics of a novel once-every 3 months intramuscular formulation of paliperidone palmitate in patients with schizophrenia. Clin Pharmacokinet. 2017;56:421–33.
Rhee Y-SC-WPPPD and HMM. Sustained-release injectable drug delivery. Pharm. Technol. 2010;6:8–13.
Nguyen VTT, Darville N, Vermeulen A. Pharmacokinetics of long-acting aqueous nano-/microsuspensions after intramuscular administration in different animal species and humans - a review. AAPS J. NLM (Medline). 2023;25(1):4.
Guo X, Zhang M, Guo Y, Liu H, Yang B, Gou J, et al. Impact of jet pulverization and wet milling techniques on properties of aripiprazole long-acting injection and absorption mechanism research in vivo. Int J Pharm. 2022;612:121300
Darville N, Van Heerden M, Mariën D, De Meulder M, Rossenu S, Vermeulen A, et al. The effect of macrophage and angiogenesis inhibition on the drug release and absorption from an intramuscular sustained-release paliperidone palmitate suspension. J Control Release. 2016;230:95–108.
Chamanza R, Darville N, van Heerden M, de Jonghe S. Comparison of the local tolerability to 5 long-acting drug nanosuspensions with different stabilizing excipients, following a single intramuscular administration in the rat. Toxicol Pathol. 2018;46:85–100.
Ahsan F, Rivas IP, Khan MA, Torres Suarez AI. Targeting to macrophages: role of physicochemical properties of particulate carriers-liposomes and microspheres-on the phagocytosis by macrophages. J Controll Release. 2002;79:9–40.
Ballard BE. Biopharmaceutical considerations in subcutaneous and intramuscular drug administration. J Pharm Sci. 1968;57:357–78.
Zuidema J, PFAJM and DGSMJE. Release and absorption rate aspects of intramuscularly injected pharmaceuticals. Int J Pharm. 1988;47:1–12.
Nguyen V, Bevernage J, Darville N, Tistaert C, Van Bocxlaer J, Rossenu S, et al. Linking in vitro intrinsic dissolution rate and thermodynamic solubility with pharmacokinetic profiles of bedaquiline long-acting aqueous microsuspensions in rats. Mol Pharm. 2021;18:952–65.
Jucker BM, Alsaid H, Rambo M, Lenhard SC, Hoang B, Xie F, et al. Multimodal imaging approach to examine biodistribution kinetics of cabotegravir (GSK1265744) long acting parenteral formulation in rat. J Control Release. 2017;268:102–12.
Medlicott NJ, Waldron NA, Foster TP. Sustained release veterinary parenteral products. Adv Drug Deliv Rev. 2004;56:1345–65.
McDowell A and NJM. Anatomy and physiology of the injection site: implications for extended release parenteral systems. Long acting injections and implants. 2012;57–71.
Anderson JM, Niven H, Pelagalli J, Olanoff LS, Jones RD. The role of the fibrous capsule in the function of implanted drug-polymer sustained release systems. J Biomed Mater Res. 1981;15(6):889–902.
Hirano KTI and HY. Studies on the absorption of practically water-insoluble drugs following injection. II. Intramuscular absorption from aqueous suspensions in rats. Chem Pharm Bull. 1981;29:817–27.
Zuidema J, Kadir F, Titulaer HAC, Oussoren C. Release and absorption rates of intramuscularly and subcutaneously injected pharmaceuticals (II). Int J Pharm. 1994;105:189–207.
Van den Mooter G, De Meulder M, Darville N, De Jonghe S, Vermeulen A, Vynckier A, et al. Modeling the time course of the tissue responses to intramuscular long-acting paliperidone palmitate nano-/microcrystals and polystyrene microspheres in the rat. Toxicol Pathol. 2015;44:189–210.
Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100.
Paquette SM, Dawit H, Hickey MB, Merisko-liversidge E, Almarsson Ö, Deaver DR. Long-acting atypical antipsychotics: characterization of the local tissue response. Pharm Res. 2014;31:2065–77.
Williams DF. There is no such thing as a biocompatible material. Biomaterials. 2014;35:10009–14.
Van ’t Klooster GVJ, Hoeben E, Borghys H, Looszova A, Bouche M, Velsen F Van, et al. Pharmacokinetics and disposition of rilpivirine (TMC278) nanosuspension as a long-acting injectable antiretroviral formulation. 2010;54:2042–50.
Yue H, Wei W, Yue Z, Lv P, Wang L, Ma G, et al. Particle size affects the cellular response in macrophages. Eur J Pharm Sci. 2010;41:650–7.
De Meulder M, Vynckier A, van Heerden M, Darville N, Van den Mooter G, Sterkens P, et al. Intramuscular administration of paliperidone palmitate extended-release injectable microsuspension induces a subclinical inflammatory reaction modulating the pharmacokinetics in rats. J Pharm Sci. 2014;103:2072–87.
Hough D, Lindenmayer J-P, Gopal S, Melkote R, Lim P, Herben V, et al. Safety and tolerability of deltoid and gluteal injections of paliperidone palmitate in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:1022–31.
Berwaerts J, Liu Y, Gopal S, Nuamah I, Xu H, Savitz A, CD, SA, RB, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72.8:830–9.
Lindenmayer J. Long-acting injectable antipsychotics: focus on olanzapine pamoate. Neuropsychiatr Dis Treat. 2010;6:261–7.
Spreen WR, Margolis DA, Pottage JC. Long-acting injectable antiretrovirals for HIV treatment and prevention. Curr Opin HIV AIDS. 2013;8:565–71.
Verloes R, van ‘t Klooster G, Baert L, van Velsen F, Bouche M-P, Spittaels K, et al. TMC278 long acting–a parenteral nanosuspension formulation that provides sustained clinically relevant plasma concentrations in HIV-negative volunteers. Abstract TUPE0042, presented at the XVII International AIDS Conference. 2008.
McLennan DN, PCJH, and CSA. Subcutaneous drug delivery and the role of the lymphatics. Drug Discov Today Technol. 2005;2:89–96.
Oussoren C, Zuidema J, Crommelin DJA, Storm G. Lymphatic uptake and biodistribution of liposomes after subcutaneous injection I. Influence of the Anatomical Site of Injection. McLennan. 1997;7:85–99.
Samtani M, Vermeulen A, Stuyckens K. Population pharmacokinetics of intramuscular paliperidone palmitate in patients with schizophrenia. 2009;48:585–600.
Champion JA,, and Samir Mitragotri. Role of target geometry in phagocytosis. Proc Natl Acad Sci. 2006;103.13:4930–4.
Owens I, Donald E, Nicholas AP. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int J Pharm. 2006;307(1):93–102.
Tabata Y, Yoshito Ikada. Macrophage phagocytosis of biodegradable microspheres composed of L‐lactic acid/glycolic acid homo‐and copolymers. J Biomed Mater Res. 1988;22.10:837–58.
Yáñez JA, RCM, SCL, FML, & DNM. Flip-flop pharmacokinetics–delivering a reversal of disposition: challenges and opportunities during drug development. Ther Deliv. 2011;2:643–72.
Correll CU, Kim E, Sliwa JK, Hamm W, Gopal S, Mathews M, et al. Pharmacokinetic characteristics of long-acting injectable antipsychotics for schizophrenia: an overview. CNS Drugs. Adis. 2021;35(1):39–59.
Schwendeman SP, Shah RB, Bailey BA, Schwendeman AS. Injectable controlled release depots for large molecules. J Controll Release. Elsevier. 2014;190:240–53.
Allmendinger A, Mueller R, Schwarb E, Chipperfield M, Huwyler J, Mahler HC, et al. Measuring tissue back-pressure - in vivo injection forces during subcutaneous injection. Pharm Res. 2015;32:2229–40.
Shahriar M, Rewanwar A, Rohilla P, Marston J. Understanding the effect of counterpressure buildup during syringe injections. Int J Pharm. 2021;602:120530.
Lee J, Gong Y, Bhoopathy S, DiLiberti CE, Hooker AC, Rostami-Hodjegan A, et al. Public workshop summary report on fiscal year 2021 generic drug regulatory science initiatives: data analysis and model-based bioequivalence. Clin Pharmacol Ther. John Wiley and Sons Inc. 2021;110(5):1190–5.
Pastorin G, Benetti C, Wacker MG. From in vitro to in vivo: a comprehensive guide to IVIVC development for long-acting therapeutics. Adv Drug Deliv Rev. Elsevier B.V.; 2023.
Department of Health and Human Services F and DAC for DE and R (CDER). Guidance for industry. extended release oral dosage forms: development, evaluation, and application of in vitro/in vivo correlations. 1999.
Neyens M, Crauwels HM, Perez-Ruixo JJ, Rossenu S. Population pharmacokinetics of the rilpivirine long-acting formulation after intramuscular dosing in healthy subjects and people living with HIV. J Antimicrob Chemother. 2021;76:3255–62.
Gomeni R, Bressolle-Gomeni F. Modeling complex pharmacokinetics of long-acting injectable products using convolution-based models with nonparametric input functions. J Clin Pharmacol. 2021;61:1081–95.
Gomeni R, Bressolle-Gomeni F. Convolution-based approach for modeling the paliperidone extended release and long-acting injectable (LAI) PK of once-, and three-monthly products administration and for optimizing the development of new LAI products. J Pharmacokinet Pharmacodyn. 2022;50(2):89–96.
Gomeni RFB, MF. Response surface analysis and nonlinear optimization algorithm for maximization of clinical drug performance: application to extended-release and long-acting injectable paliperidone. J Clin Pharmacol. 2016;56:1296–306.
Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development. CPT Pharmacometrics Syst Pharmacol. 2012;1(9):1–14.
Russu A, Kern Sliwa J, Ravenstijn P, Singh A, Mathews M, Kim E, et al. Maintenance dose conversion between oral risperidone and paliperidone palmitate 1 month: practical guidance based on pharmacokinetic simulations. Int J Clin Pract. 2018;72.:e13089.
Gajjar P, Dickinson J, Dickinson H, Ruston L, Mistry HB, Patterson C, et al. Determining bioequivalence possibilities of long acting injectables through population PK modelling. European Journal of Pharmaceutical Sciences. 2022;179:106296.
Shimizu H, Neyens M, De Meulder M, Gopal S, Tsukamoto Y, Samtani MN, et al. Population pharmacokinetics of paliperidone palmitate (once-monthly formulation) in Japanese, Korean, and Taiwanese patients with schizophrenia. Clin Pharmacol Drug Dev. 2020;9:224–34.
Gomeni R, Fang L (Lucy), Bressolle-Gomeni F, Spencer TJ, Faraone S V., Babiskin A. A general framework for assessing in vitro/in vivo correlation as a tool for maximizing the benefit-risk ratio of a treatment using a convolution-based modeling approach. CPT Pharmacometrics Syst Pharmacol. 2019;8:97–106.
Hard ML, Mills RJ, Sadler BM, Wehr AY, Weiden PJ, von Moltke L. Pharmacokinetic profile of a 2-month dose regimen of aripiprazole lauroxil: a phase I study and a population pharmacokinetic model. CNS Drugs. 2017;31:617–24.
Rajoli RKR, Back DJ, Flexner C, Owen A, Siccardi M. Physiologically based pharmacokinetic modelling to inform development of intramuscular long-acting nanoformulations for HIV. Clin Pharmacokinet. 2015;54:639–50.
Rajoli RKR, Podany AT, Moss DM, Swindells S, Flexner C, Owen A, et al. Modelling the long-acting administration of anti-tuberculosis agents using PBPK : a proof of concept study. Int J Tuberc Lung Dis. 2018;22.8:937–44.
Rajoli RKR, Curley P, Chiong J, Back D, Flexner C, Owen A, et al. Predicting drug-drug interactions between rifampicin and long-acting cabotegravir and rilpivirine using physiologically based pharmacokinetic modeling. J Infect Dis. 2019;219:1735–42.
Rajoli RKR, Flexner C, Chiong J, Owen A, Donnelly RF, Larrañeta E, et al. Modelling the intradermal delivery of microneedle array patches for long-acting antiretrovirals using PBPK. Eur J Pharm Biopharm. 2019;144:101–9.
Rajoli RKR, Back DJ, Rannard S, Meyers CF, Flexner C, Owen A, et al. In silico dose prediction for long-acting rilpivirine and cabotegravir administration to children and adolescents. Clin Pharmacokinet. 2018;57:255–66.
Kinvig H, Cottura N, Lloyd A, Frivold C, Mistilis J, Jarrahian C, et al. Evaluating islatravir administered via microneedle array patch for long-acting HIV pre-exposure prophylaxis using physiologically based pharmacokinetic modelling. Eur J Drug Metab Pharmacokinet. 2022;47:855–68.
Rajoli RKR, Demkovic ZR, Flexner C, Owen A, Siccardi M. Predicting pharmacokinetics of a tenofovir alafenamide subcutaneous implant using physiologically based pharmacokinetic modelling. Antimicrob Agents Chemother. 2020;64(8):1110–28.
Bettonte S, Berton M, Stader F, Battegay M, Marzolini C. Management of drug-drug interactions between long-acting cabotegravir and rilpivirine and comedications with inducing properties: a modeling study. Clin Infect Dis. 2023;76:1225–36.
Perazzolo S, Shireman LM, Koehn J, McConnachie LA, Kraft JC, Shen DD, et al. Three HIV drugs, atazanavir, ritonavir, and tenofovir, coformulated in drug-combination nanoparticles exhibit long-acting and lymphocyte-targeting properties in nonhuman primates. J Pharm Sci. 2018;107:3153–62.
Perazzolo S, Shireman LM, Shen DD, Ho RJY. Physiologically based pharmacokinetic modeling of 3 HIV drugs in combination and the role of lymphatic system after subcutaneous dosing. Part 1: Model for the Free-Drug Mixture. J Pharm Sci. 2022;111:529–41.
Perazzolo S, Shen DD, Ho RJY. Physiologically based pharmacokinetic modeling of 3 HIV drugs in combination and the role of lymphatic system after subcutaneous dosing. Part 2: Model for the Drug-combination Nanoparticles. J Pharm Sci. 2022;111:825–37.
Pepin XJH, Parrott N, Dressman J, Delvadia P, Mitra A, Zhang X, et al. Current state and future expectations of translational modeling strategies to support drug product development, manufacturing changes and controls: a workshop summary report. J Pharm Sci. 2021;10(2):555–66.
Wu F, Shah H, Li M, Duan P, Zhao P, Suarez S, et al. Biopharmaceutics applications of physiologically based pharmacokinetic absorption modeling and simulation in regulatory submissions to the U.S. Food and Drug Administration for new drugs. AAPS J. 2021;3:1–14.
Dubbelboer IR, Sjögren E. Physiological based pharmacokinetic and biopharmaceutics modelling of subcutaneously administered compounds – an overview of in silico models. Int J Pharm. 2022;21:121808.
U.S. Department of Health and Human Services F and DAC for DE and R (CDER). The use of physiologically based pharmacokinetic analyses — biopharmaceutics applications for oral drug product development, manufacturing changes, and controls. Guidance for Industry. 2020.
Shohin IE, Grebenkin DY, Malashenko EA, Stanishevskii YM, Ramenskaya Gv. A brief review of the FDA dissolution methods database. Dissolut Technol. 2016;23(3):6–10.
USP-NF. Rockville MUSP. United States Pharmacopeia General Chapter, 〈1001〉 In vitro release test methods for parenteral drug preparations. 2022.
Rudd ND, Reibarkh M, Fang R, Mittal S, Walsh PL, Brunskill APJ, et al. Interpreting in vitro release performance from long-acting parenteral nanosuspensions using USP-4 dissolution and spectroscopic techniques. Mol Pharm. 2020;17:1734–47.
Jablonka L, Ashtikar M, Gao GF, Thurn M, Modh H, Wang JW, et al. Predicting human pharmacokinetics of liposomal temoporfin using a hybrid in silico model. Eur J Pharm Biopharm. 2020;149:121–34.
Probst M, Schmidt M, Tietz K, Klein S, Weitschies W, Seidlitz A. In vitro dissolution testing of parenteral aqueous solutions and oily suspensions of paracetamol and prednisolone. Int J Pharm. 2017;532:519–27.
Bao Q, Wang X, Zou Y, Wang Y, Burgess DJ. In vitro release testing method development for long-acting injectable suspensions. Int J Pharm. 2022;622:121840.
Kozak J, Rabiskova M, Lamprecht A. Muscle tissue as a surrogate for in vitro drug release testing of parenteral depot microspheres. AAPS PharmSciTech. 2021;22:1–12.
McCartan A, Mackay J, Curran D, Mrsny RJ. Modelling intramuscular drug fate in vitro with tissue-relevant biomimetic hydrogels. Int J Pharm. 2022;X 4:100125.
Kinnunen HM, Sharma V, Contreras-Rojas LR, Yu Y, Alleman C, Sreedhara A, et al. A novel in vitro method to model the fate of subcutaneously administered biopharmaceuticals and associated formulation components. J Control Release. 2015;214:94–102.
Kinnunen HM, Mrsny RJ. Improving the outcomes of biopharmaceutical delivery via the subcutaneous route by understanding the chemical, physical and physiological properties of the subcutaneous injection site. J Controll Release. 2014;182:22–32.
McCartan AJS, Curran DW, Mrsny RJ. Evaluating parameters affecting drug fate at the intramuscular injection site. J Controll Release. 2021;336:322–35.
Forrest WP, Reuter KG, Shah V, Kazakevich I, Heslinga M, Dudhat S, et al. USP apparatus 4: a valuable in vitro tool to enable formulation development of long-acting parenteral (LAP) nanosuspension formulations of poorly water-soluble compounds. AAPS PharmSciTech. 2018;19:413–24.
Weng Larsen S, Larsen C. Critical factors influencing the in vivo performance of long-acting lipophilic solutions-impact on in vitro release method design. AAPS J. 2009.;11:762–70.
Bannigan P, Bao Z, Hickman RJ, Aldeghi M, Häse F, Aspuru-Guzik A, et al. Machine learning models to accelerate the design of polymeric long-acting injectables. Nat Commun. 2023;14:35.
Hirano K, IT, & YH. Studies on the absorption of practically water-insoluble drugs following injection V: subcutaneous absorption in rats from solutions in water immiscible oils. J Pharm Sci. 1982;71:495–500.
Lou H, Hageman MJ. Development of drug release model for suspensions in ESCAR (Emulator of SubCutaneous Absorption and Release). AAPS J. 2023;25:29.
Andhariya J v., Shen J, Choi S, Wang Y, Zou Y, Burgess DJ. Development of in vitro-in vivo correlation of parenteral naltrexone loaded polymeric microspheres. J Controll Release. 2017;255:27–35.
Shen J, Choi S, Qu W, Wang Y, Burgess DJ. In vitro-in vivo correlation of parenteral risperidone polymeric microspheres. J Control Release. 2015;218:2–12.
Bao Q, Wang X, Wan B, Zou Y, Wang Y, Burgess DJ. Development of in vitro-in vivo correlations for long-acting injectable suspensions. Int J Pharm. 2023;634:122642.
Probst M, Kühn JP, Scheuch E, Seidlitz A, Hadlich S, Evert K, et al. Simultaneous magnetic resonance imaging and pharmacokinetic analysis of intramuscular depots. J Control Release. 2016;227:1–12.
Kalicharan RW, Baron P, Oussoren C, Bartels LW, Vromans H. Spatial distribution of oil depots monitored in human muscle using MRI. Int J Pharm. 2016;505:52–60.
Zhao L, Kim MJ, Zhang L, Lionberger R. Generating model integrated evidence for generic drug development and assessment. Clin Pharmacol Ther. 2019;105(2):338–49.
Author information
Authors and Affiliations
Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work (writing, review, and editing) and approved it for publication.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Communicated by Huybrecht T'jollyn and Oliver Ackaert.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siemons, M., Schroyen, B., Darville, N. et al. Role of Modeling and Simulation in Preclinical and Clinical Long-Acting Injectable Drug Development. AAPS J 25, 99 (2023). https://doi.org/10.1208/s12248-023-00864-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00864-9