Abstract
Motivated by a series of work demonstrating the effect of molecular charge on antibody pharmacokinetics (PK), physiological-based pharmacokinetic (PBPK) models are emerging that relate in silico calculated charge or in vitro measures of polyspecificity to antibody PK parameters. However, only plasma data has been used for model development in these studies, leading to unvalidated assumptions. Here, we present an extended platform PBPK model for antibodies that incorporate charge-dependent endothelial cell pinocytosis rate and nonspecific off-target binding in the interstitial space and on circulating blood cells, to simultaneously characterize whole-body disposition of three antibody charge variants. Predictive potential of various charge metrics was also explored, and the difference between positive charge patches and negative charge patches (i.e., PPC-PNC) was used as the charge parameter to establish quantitative relationships with nonspecific binding affinities and endothelial cell uptake rate. Whole-body disposition of these charge variants was captured well by the model, with less than 2-fold predictive error in area under the curve of most plasma and tissue PK data. The model also predicted that with greater positive charge, nonspecific binding was more substantial, and pinocytosis rate increased especially in brain, heart, kidney, liver, lung, and spleen, but remained unchanged in adipose, bone, muscle, and skin. The presented PBPK model contributes to our understanding of the mechanisms governing the disposition of charged antibodies and can be used as a platform to guide charge engineering based on desired plasma and tissue exposures.
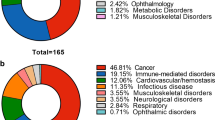
Graphical Abstract






Similar content being viewed by others
Data Availability
All relevant data have been included in this paper. Raw data can be provided upon reasonable request.
References
Gupta P, Makowski EK, Kumar S, Zhang Y, Scheer JM, Tessier PM. Antibodies with weakly basic isoelectric points minimize trade-offs between formulation and physiological colloidal properties. Mol Pharm. 2022;19(3):775–87. https://doi.org/10.1021/acs.molpharmaceut.1c00373.
Dostalek M, Prueksaritanont T, Kelley RF. Pharmacokinetic de-risking tools for selection of monoclonal antibody lead candidates. MAbs. 2017;9(5):756–66. https://doi.org/10.1080/19420862.2017.1323160.
Kingsbury JS, Saini A, Auclair SM, Fu L, Lantz MM, Halloran KT, et al. A single molecular descriptor to predict solution behavior of therapeutic antibodies. Sci Adv. 2020;6(32):eabb0372. https://doi.org/10.1126/sciadv.abb0372.
Jain T, Sun TW, Durand S, Hall A, Houston NR, Nett JH, et al. Biophysical properties of the clinical-stage antibody landscape. Proc Natl Acad Sci USA. 2017;114(5):944–9. https://doi.org/10.1073/pnas.1616408114.
Makowski EK, Wu L, Gupta P, Tessier PM. Discovery-stage identification of drug-like antibodies using emerging experimental and computational methods. MAbs. 2021;13(1):1895540. https://doi.org/10.1080/19420862.2021.1895540.
Negron C, Fang J, McPherson MJ, Stine WB Jr, McCluskey AJ. Separating clinical antibodies from repertoire antibodies, a path to in silico developability assessment. MAbs. 2022;14(1):2080628. https://doi.org/10.1080/19420862.2022.2080628.
Raybould MIJ, Marks C, Krawczyk K, Taddese B, Nowak J, Lewis AP, et al. Five computational developability guidelines for therapeutic antibody profiling. Proc Natl Acad Sci USA. 2019;116(10):4025–30. https://doi.org/10.1073/pnas.1810576116.
Ahmed L, Gupta P, Martin KP, Scheer JM, Nixon AE, Kumar S (2021) Intrinsic physicochemical profile of marketed antibody-based biotherapeutics. Proc Natl Acad Sci U S A. 118(37). https://doi.org/10.1073/pnas.2020577118.
Zhang Y, Wu L, Gupta P, Desai AA, Smith MD, Rabia LA, et al. Physicochemical rules for identifying monoclonal antibodies with drug-like specificity. Mol Pharm. 2020;17(7):2555–69. https://doi.org/10.1021/acs.molpharmaceut.0c00257.
Shehata L, Maurer DP, Wec AZ, Lilov A, Champney E, Sun T, et al. Affinity maturation enhances antibody specificity but compromises conformational stability. Cell Rep. 2019;28(13):3300-8-e4. https://doi.org/10.1016/j.celrep.2019.08.056.
Starr CG, Tessier PM. Selecting and engineering monoclonal antibodies with drug-like specificity. Curr Opin Biotechnol. 2019;60:119–27. https://doi.org/10.1016/j.copbio.2019.01.008.
Kelly RL, Sun T, Jain T, Caffry I, Yu Y, Cao Y, et al. High throughput cross-interaction measures for human IgG1 antibodies correlate with clearance rates in mice. MAbs. 2015;7(4):770–7. https://doi.org/10.1080/19420862.2015.1043503.
Hotzel I, Theil FP, Bernstein LJ, Prabhu S, Deng R, Quintana L, et al. A strategy for risk mitigation of antibodies with fast clearance. MAbs. 2012;4(6):753–60. https://doi.org/10.4161/mabs.22189.
Kraft TE, Richter WF, Emrich T, Knaupp A, Schuster M, Wolfert A, et al. Heparin chromatography as an in vitro predictor for antibody clearance rate through pinocytosis. Mabs. 2020;12(1):1683432. https://doi.org/10.1080/19420862.2019.1683432.
Avery LB, Wade J, Wang M, Tam A, King A, Piche-Nicholas N, et al. Establishing in vitro in vivo correlations to screen monoclonal antibodies for physicochemical properties related to favorable human pharmacokinetics. MAbs. 2018;10(2):244–55. https://doi.org/10.1080/19420862.2017.1417718.
Sharma VK, Patapoff TW, Kabakoff B, Pai S, Hilario E, Zhang B, et al. In silico selection of therapeutic antibodies for development: viscosity, clearance, and chemical stability. Proc Natl Acad Sci U S A. 2014;111(52):18601–6. https://doi.org/10.1073/pnas.1421779112.
Grinshpun B, Thorsteinson N, Pereira JN, Rippmann F, Nannemann D, Sood VD, et al. Identifying biophysical assays and in silico properties that enrich for slow clearance in clinical-stage therapeutic antibodies. MAbs. 2021;13(1):1932230. https://doi.org/10.1080/19420862.2021.1932230.
Chung S, Nguyen V, Lin YL, Lafrance-Vanasse J, Scales SJ, Lin K, et al. An in vitro FcRn- dependent transcytosis assay as a screening tool for predictive assessment of nonspecific clearance of antibody therapeutics in humans. MAbs. 2019;11(5):942–55. https://doi.org/10.1080/19420862.2019.1605270.
Goulet DR, Watson MJ, Tam SH, Zwolak A, Chiu ML, Atkins WM, et al. Toward a combinatorial approach for the prediction of IgG half-life and clearance. Drug Metab Dispos. 2018;46(12):1900–7. https://doi.org/10.1124/dmd.118.081893.
Datta-Mannan A, Thangaraju A, Leung D, Tang Y, Witcher DR, Lu JR, et al. Balancing charge in the complementarity-determining regions of humanized mAbs without affecting pI reduces non-specific binding and improves the pharmacokinetics. MAbs. 2015;7(3):483–93. https://doi.org/10.1080/19420862.2015.1016696.
Schoch A, Kettenberger H, Mundigl O, Winter G, Engert J, Heinrich J, et al. Charge-mediated influence of the antibody variable domain on FcRn-dependent pharmacokinetics. Proc Natl Acad Sci U S A. 2015;112(19):5997–6002. https://doi.org/10.1073/pnas.1408766112.
Liu S, Verma A, Kettenberger H, Richter WF, Shah DK. Effect of variable domain charge on in vitro and in vivo disposition of monoclonal antibodies. MAbs. 2021;13(1):1993769. https://doi.org/10.1080/19420862.2021.1993769.
Bumbaca Yadav D, Sharma VK, Boswell CA, Hotzel I, Tesar D, Shang Y, et al. Evaluating the use of antibody variable region (Fv) charge as a risk assessment tool for predicting typical cynomolgus monkey pharmacokinetics. J Biol Chem. 2015;290(50):29732–41. https://doi.org/10.1074/jbc.M115.692434.
Li B, Tesar D, Boswell CA, Cahaya HS, Wong A, Zhang J, et al. Framework selection can influence pharmacokinetics of a humanized therapeutic antibody through differences in molecule charge. MAbs. 2014;6(5):1255–64. https://doi.org/10.4161/mabs.29809.
Stüber JC, Rechberger KF, Miladinović SM, Pöschinger T, Zimmermann T, Villenave R, et al. Impact of charge patches on tumor disposition and biodistribution of therapeutic antibodies. AAPS Opn. 2022;8(1):1–18.
Igawa T, Tsunoda H, Tachibana T, Maeda A, Mimoto F, Moriyama C, et al. Reduced elimination of IgG antibodies by engineering the variable region. Protein Eng Des Sel. 2010;23(5):385–92. https://doi.org/10.1093/protein/gzq009.
Hardiansyah D, Ng CM. Minimal physiologically-based pharmacokinetic model to investigate the effect of charge on the pharmacokinetics of humanized anti-HCV-E2 IgG antibodies in Sprague-Dawley rats. Pharm Res. 2022. https://doi.org/10.1007/s11095-022-03204-2.
Varkhede N, Forrest ML. Understanding the monoclonal antibody disposition after subcutaneous administration using a minimal physiologically based pharmacokinetic model. J Pharm Pharm Sci. 2018;21(1s):130s–48s. https://doi.org/10.18433/jpps30028.
Hu S, D’Argenio DZ. Predicting monoclonal antibody pharmacokinetics following subcutaneous administration via whole-body physiologically-based modeling. J Pharmacokinet Pharmacodyn. 2020;47(5):385–409. https://doi.org/10.1007/s10928-020-09691-3.
Hu S, Datta-Mannan A, D’Argenio DZ. Physiologically based modeling to predict monoclonal antibody pharmacokinetics in humans from in vitro physiochemical properties. MAbs. 2022;14(1):2056944. https://doi.org/10.1080/19420862.2022.2056944.
Hu S, Datta-Mannan A, D’Argenio DZ. Monoclonal antibody pharmacokinetics in cynomolgus monkeys following subcutaneous administration: physiologically based model predictions from physiochemical properties. AAPS J. 2022;25(1):5. https://doi.org/10.1208/s12248-022-00772-4.
Jones HM, Zhang Z, Jasper P, Luo H, Avery LB, King LE, et al. A physiologically-based pharmacokinetic model for the prediction of monoclonal antibody pharmacokinetics from in vitro data. CPT Pharmacometrics Syst Pharmacol. 2019;8(10):738–47. https://doi.org/10.1002/psp4.12461.
Sampei Z, Haraya K, Tachibana T, Fukuzawa T, Shida-Kawazoe M, Gan SW, et al. Antibody engineering to generate SKY59, a long-acting anti-C5 recycling antibody. Plos One. 2018;13(12):e0209509. https://doi.org/10.1371/journal.pone.0209509.
Crowell SR, Wang K, Famili A, Shatz W, Loyet KM, Chang V, et al. Influence of charge, hydrophobicity, and size on vitreous pharmacokinetics of large molecules. Transl Vis Sci Technol. 2019;8(6):1. https://doi.org/10.1167/tvst.8.6.1.
Triguero D, Buciak JL, Pardridge WM. Cationization of immunoglobulin G results in enhanced organ uptake of the protein after intravenous administration in rats and primate. J Pharmacol Exp Ther. 1991;258(1):186–92.
Shah DK, Betts AM. Towards a platform PBPK model to characterize the plasma and tissue disposition of monoclonal antibodies in preclinical species and human. J Pharmacokinet Pharmacodyn. 2012;39(1):67–86. https://doi.org/10.1007/s10928-011-9232-2.
Chang HY, Wu S, Meno-Tetang G, Shah DK. A translational platform PBPK model for antibody disposition in the brain. J Pharmacokinet Pharmacodyn. 2019;46(4):319–38. https://doi.org/10.1007/s10928-019-09641-8.
Chang HY, Wu S, Chowdhury EA, Shah DK. Towards a translational physiologically-based pharmacokinetic (PBPK) model for receptor-mediated transcytosis of anti-transferrin receptor monoclonal antibodies in the central nervous system. J Pharmacokinet Pharmacodyn. 2022;49(3):337–62. https://doi.org/10.1007/s10928-021-09800-w.
Chen Y, Balthasar JP. Evaluation of a catenary PBPK model for predicting the in vivo disposition of mAbs engineered for high-affinity binding to FcRn. AAPS J. 2012;14(4):850–9. https://doi.org/10.1208/s12248-012-9395-9.
Harrold JM, Abraham AK. Ubiquity: a framework for physiological/mechanism-based pharmacokinetic/pharmacodynamic model development and deployment. J Pharmacokinet Pharmacodyn. 2014;41(2):141–51. https://doi.org/10.1007/s10928-014-9352-6.
Siev M, Yu X, Prados-Rosales R, Martiniuk FT, Casadevall A, Achkar JM. Correlation between serum and plasma antibody titers to mycobacterial antigens. Clin Vaccine Immunol. 2011;18(1):173–5. https://doi.org/10.1128/CVI.00325-10.
Vugmeyster Y, Szklut P, Wensel D, Ross J, Xu X, Awwad M, et al. Complex pharmacokinetics of a humanized antibody against human amyloid beta peptide, anti-Abeta Ab2, in nonclinical species. Pharm Res. 2011;28(7):1696–706. https://doi.org/10.1007/s11095-011-0405-x.
Goyon A, Excoffier M, Janin-Bussat MC, Bobaly B, Fekete S, Guillarme D, et al. Determination of isoelectric points and relative charge variants of 23 therapeutic monoclonal antibodies. J Chromatogr B Analyt Technol Biomed Life Sci. 2017;1065–1066:119–28. https://doi.org/10.1016/j.jchromb.2017.09.033.
Onsum MD, Geretti E, Paragas V, Kudla AJ, Moulis SP, Luus L, et al. Single-cell quantitative HER2 measurement identifies heterogeneity and distinct subgroups within traditionally defined HER2-positive patients. Am J Pathol. 2013;183(5):1446–60. https://doi.org/10.1016/j.ajpath.2013.07.015.
DeFazio-Eli L, Strommen K, Dao-Pick T, Parry G, Goodman L, Winslow J. Quantitative assays for the measurement of HER1-HER2 heterodimerization and phosphorylation in cell lines and breast tumors: applications for diagnostics and targeted drug mechanism of action. Breast Cancer Res. 2011;13(2):R44. https://doi.org/10.1186/bcr2866.
Glassman PM, Balthasar JP. Physiologically-based pharmacokinetic modeling to predict the clinical pharmacokinetics of monoclonal antibodies. J Pharmacokinet Pharmacodyn. 2016;43(4):427–46. https://doi.org/10.1007/s10928-016-9482-0.
Grotte G. Passage of dextran molecules across the blood-lymph barrier. Acta Chir Scand Suppl. 1956;211:1–84.
Rippe B, Haraldsson B. Fluid and protein fluxes across small and large pores in the microvasculature. Application of two-pore equations. Acta Physiol Scand. 1987;131(3):411–28. https://doi.org/10.1111/j.1748-1716.1987.tb08257.x.
Rippe B, Haraldsson B. Transport of macromolecules across microvascular walls: the two-pore theory. Physiol Rev. 1994;74(1):163–219. https://doi.org/10.1152/physrev.1994.74.1.163.
Baxter LT, Zhu H, Mackensen DG, Jain RK. Physiologically based pharmacokinetic model for specific and nonspecific monoclonal antibodies and fragments in normal tissues and human tumor xenografts in nude mice. Cancer Res. 1994;54(6):1517–28.
Ferl GZ, Wu AM, DiStefano JJ 3rd. A predictive model of therapeutic monoclonal antibody dynamics and regulation by the neonatal Fc receptor (FcRn). Ann Biomed Eng. 2005;33(11):1640–52. https://doi.org/10.1007/s10439-005-7410-3.
Davda JP, Jain M, Batra SK, Gwilt PR, Robinson DH. A physiologically based pharmacokinetic (PBPK) model to characterize and predict the disposition of monoclonal antibody CC49 and its single chain Fv constructs. Int Immunopharmacol. 2008;8(3):401–13. https://doi.org/10.1016/j.intimp.2007.10.023.
Sepp A, Berges A, Sanderson A, Meno-Tetang G. Development of a physiologically based pharmacokinetic model for a domain antibody in mice using the two-pore theory. J Pharmacokinet Pharmacodyn. 2015;42(2):97–109. https://doi.org/10.1007/s10928-014-9402-0.
Li Z, Shah DK. Two-pore physiologically based pharmacokinetic model with de novo derived parameters for predicting plasma PK of different size protein therapeutics. J Pharmacokinet Pharmacodyn. 2019;46(3):305–18. https://doi.org/10.1007/s10928-019-09639-2.
Sepp A, Meno-Tetang G, Weber A, Sanderson A, Schon O, Berges A. Computer-assembled cross-species/cross-modalities two-pore physiologically based pharmacokinetic model for biologics in mice and rats. J Pharmacokinet Pharmacodyn. 2019;46(4):339–59. https://doi.org/10.1007/s10928-019-09640-9.
Li Z, Li Y, Chang HP, Yu X, Shah DK. Two-pore physiologically based pharmacokinetic model validation using whole-body biodistribution of trastuzumab and different-size fragments in mice. J Pharmacokinet Pharmacodyn. 2021;48(5):743–62. https://doi.org/10.1007/s10928-021-09772-x.
Li Z, Yu X, Li Y, Verma A, Chang HP, Shah DK. A two-pore physiologically based pharmacokinetic model to predict subcutaneously administered different-size antibody/antibody fragments. AAPS J. 2021;23(3):62. https://doi.org/10.1208/s12248-021-00588-8.
Niederalt C, Kuepfer L, Solodenko J, Eissing T, Siegmund HU, Block M, et al. A generic whole body physiologically based pharmacokinetic model for therapeutic proteins in PK-Sim. J Pharmacokinet Pharmacodyn. 2018;45(2):235–57. https://doi.org/10.1007/s10928-017-9559-4.
Pardridge WM, Kang YS, Yang J, Buciak JL. Enhanced cellular uptake and in vivo biodistribution of a monoclonal antibody following cationization. J Pharm Sci. 1995;84(8):943–8. https://doi.org/10.1002/jps.2600840808.
Grevys A, Frick R, Mester S, Flem-Karlsen K, Nilsen J, Foss S, et al. Antibody variable sequences have a pronounced effect on cellular transport and plasma half-life. iSci. 2022;25(2):103746. https://doi.org/10.1016/j.isci.2022.103746.
Belting M. Heparan sulfate proteoglycan as a plasma membrane carrier. Trends Biochem Sci. 2003;28(3):145–51. https://doi.org/10.1016/S0968-0004(03)00031-8.
Kreuger J, Spillmann D, Li JP, Lindahl U. Interactions between heparan sulfate and proteins: the concept of specificity. J Cell Biol. 2006;174(3):323–7. https://doi.org/10.1083/jcb.200604035.
Varki A. Sialic acids in human health and disease. Trends Mol Med. 2008;14(8):351–60. https://doi.org/10.1016/j.molmed.2008.06.002.
Boswell CA, Tesar DB, Mukhyala K, Theil FP, Fielder PJ, Khawli LA. Effects of charge on antibody tissue distribution and pharmacokinetics. Bioconjug Chem. 2010;21(12):2153–63. https://doi.org/10.1021/bc100261d.
Wiig H, Tenstad O. Interstitial exclusion of positively and negatively charged IgG in rat skin and muscle. Am J Physiol Heart Circ Physiol. 2001;280(4):H1505–12. https://doi.org/10.1152/ajpheart.2001.280.4.H1505.
Gilchrist SA, Parker JC. Exclusion of charged macromolecules in the pulmonary interstitium. Microvasc Res. 1985;30(1):88–98. https://doi.org/10.1016/0026-2862(85)90041-x.
Praaning-van Dalen DP, Brouwer A, Knook DL. Clearance capacity of rat liver Kupffer, Endothelial, and parenchymal cells. Gastroenterology. 1981;81(6):1036–44.
St-Amour I, Pare I, Alata W, Coulombe K, Ringuette-Goulet C, Drouin-Ouellet J, et al. Brain bioavailability of human intravenous immunoglobulin and its transport through the murine blood-brain barrier. J Cereb Blood Flow Metab. 2013;33(12):1983–92. https://doi.org/10.1038/jcbfm.2013.160.
Vink H, Wieringa PA, Spaan JA. Evidence that cell surface charge reduction modifes capillary red cell velocity-flux relationships in hamster cremaster muscle. J Physiol. 1995;489(Pt 1):193–201. https://doi.org/10.1113/jphysiol.1995.sp021041.
Wang W, Lu P, Fang Y, Hamuro L, Pittman T, Carr B, et al. Monoclonal antibodies with identical Fc sequences can bind to FcRn differentially with pharmacokinetic consequences. Drug Metab Dispos. 2011;39(9):1469–77. https://doi.org/10.1124/dmd.111.039453.
Rossini S, Noe R, Daventure V, Lecerf M, Justesen S, Dimitrov JD. V region of IgG controls the molecular properties of the binding site for neonatal Fc receptor. J Immunol. 2020;205(10):2850–60. https://doi.org/10.4049/jimmunol.2000732.
Kelly RL, Yu Y, Sun T, Caffry I, Lynaugh H, Brown M, et al. Target-independent variable region mediated effects on antibody clearance can be FcRn independent. MAbs. 2016;8(7):1269–75. https://doi.org/10.1080/19420862.2016.1208330.
Hardiansyah D, Ng CM. Minimal physiologically-based pharmacokinetic model to investigate the effect of pH dependent FcRn affinity and the endothelial endocytosis on the pharmacokinetics of anti-VEGF humanized IgG1 antibody in cynomolgus monkey. Eur J Pharm Sci. 2018;125:130–41. https://doi.org/10.1016/j.ejps.2018.09.015.
Dellian M, Yuan F, Trubetskoy VS, Torchilin VP, Jain RK. Vascular permeability in a human tumour xenograft: molecular charge dependence. Br J Cancer. 2000;82(9):1513–8. https://doi.org/10.1054/bjoc.1999.1171.
Sun Y, Cai H, Hu Z, Boswell CA, Diao J, Li C, et al. Balancing the affinity and pharmacokinetics of antibodies by modulating the size of charge patches on complementarity-determining regions. J Pharm Sci. 2020;109(12):3690–6. https://doi.org/10.1016/j.xphs.2020.09.003.
Funding
This work was funded by the Center of Protein Therapeutics at the University at Buffalo. DKS is supported by National Institute of General Medical Sciences grant [GM114179], National Institute of Allergy and Infectious Diseases grant [AI138195], and National Cancer Institute grants [R01CA246785 and R01CA256928].
Author information
Authors and Affiliations
Contributions
S.L. and D.K.S. conceptualized the study. S.L. performed data collection and modeling analysis. S.L. wrote the first draft and D.K.S. revised the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Shah, D.K. Physiologically Based Pharmacokinetic Modeling to Characterize the Effect of Molecular Charge on Whole-Body Disposition of Monoclonal Antibodies. AAPS J 25, 48 (2023). https://doi.org/10.1208/s12248-023-00812-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-023-00812-7