Abstract
The genetic mechanisms underlying the regulation of adrenarche are unknown. The aim of the study was to find out whether ACTH receptor (MC2R) promoter polymorphism associates with premature adrenarche (PA) and its characteristics. DNA samples of 74 prepubertal children with PA and their age- and gender-matched 97 healthy controls were genotyped for the −2 bp T/C diallelic MC2R promoter polymorphism (MC2R −2 T>C) All children were examined clinically, and hormonal measurements after an overnight fast and a low-dose ACTH stimulation test were performed. In controls, the baseline ACTH/cortisol ratio was significantly higher (p = 0.002) in subjects with the polymorphism than in the T/T group indicating decreased ACTH sensitivity. The frequency of the MC2R −2 T>C polymorphism was significantly higher in PA children with premature pubarche than in those with milder signs of PA or in control children (p = 0.04). In children with PA, the polymorphism associated with higher baseline serum dehydroepiandrosterone (p = 0.03), androstenedione (p = 0.02), plasma ACTH (p = 0.03) levels and with lower birth weight (p = 0.02). Our study provides evidence that the MC2R promoter polymorphism modulates the hypothalamo-pituitary-adrenal axis in children and may play a role in altered regulation of adrenarche.
Similar content being viewed by others
Main
Premature adrenarche (PA) was previously regarded as a benign variant of normal sexual development, but recent studies have connected it with risk of developing ovarian hyperandrogenism and metabolic disorders. PA is defined as an increase of adrenal androgen production before the age of 8 y in girls and 9 y in boys with clinical findings including appearance of pubic or axillary hair, acne, adult-type body odor and oily hair. Girls are much more frequently affected than boys (1,2).
The mechanisms underlying the initiation of adrenarche and maintenance of adrenal androgen production are still unknown. Pituitary gland secretes adrenocorticotropic hormone (ACTH) that stimulates adrenal glucocorticoid and androgen production, but there are no significant changes seen in circulating ACTH levels during adrenarche (3,4). Most authorities regard the role of ACTH in adrenarche as being merely permissive. However, without the action of ACTH, a rise in dehydroepiandrosterone (DHEA) cannot happen. The lack of adrenarche in patients with familial glucocorticoid deficiency syndrome due to ACTH resistance provides evidence for a significant role of ACTH in the regulation of adrenarche (5).
Many studies indicate genetic regulation in adrenal androgen production. There is significant heterogeneity in adrenal secretion of DHEA in response to ACTH, whereas there is little inter-subject variability in cortisol secretion (6). Besides the age- and gender-dependent variation of adrenal androgen levels, there is a significant genetic component in the residual variation of dehydroepiandrosterone sulfate (DHEAS) (7,8). The brothers of women with polycystic ovary syndrome have been documented to have elevated DHEAS levels as their sisters do (9). Despite clear evidence for a significant genetic component in adrenal androgen production, the mechanisms of genetic regulation are still mainly unknown.
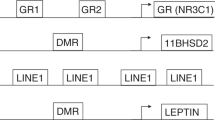
A G protein-coupled membrane receptor mediates the effects of ACTH on adrenocortical cells by elevating intracellular cAMP and activating steroidogenesis. ACTH receptor belongs to the melanocortin receptors and is called melanocortin-2 receptor (MC2R) (10,11). The human MC2R gene maps to chromosome 18p11.2 (12), and one intron separates the coding exon 2 from an upstream untranslated exon 1 (13). Recently, a polymorphism within the MC2R promoter transcription initiation site at position −2 bp altering the consensus sequence from CTC to CCC (MC2R −2 T>C) was described. This functional polymorphism results in lower promoter activity in vitro due to changes in transcription initiation, and it is associated with lower cortisol and DHEA secretion in response to ACTH stimulation in vivo (14,15).
We hypothesized that the functional MC2R −2 T>C polymorphism could play a role in the polygenic pathogenesis of PA. We therefore studied the association of this polymorphism with PA and its characteristics.
SUBJECTS AND METHODS
Subjects.
The study group comprised 171 Finnish children. Recruitment of these subjects has been documented previously (16). For the subjects with premature adrenarche, the criteria for entry into the study were any clinical sign(s) of adrenarche, including pubic/axillary hair, acne, adult-type body odor, and oily hair before the age of 8 y in girls and 9 y in boys. All eligible children were invited to the study between October 2004 and January 2006 from our Northern Savo Hospital District in Eastern Finland with a population of 250,000. Study subjects were collected among the patients admitted to the pediatric outpatient clinic of Kuopio University Hospital because of any hyperandrogenic symptoms. In addition, information letters were sent to the well-baby and school clinics of health care centers, and announcements were published in local newspapers. Seventy-six eligible children were found, and 74 (97.4%) of them were willing to participate (64 girls and 10 boys). A total of 38 children had premature pubarche (PP-PA) and the others had milder signs of premature adrenarche (nonPP-PA). Steroidogenic enzyme defects and virilizing tumors were excluded biochemically and by adrenal ultrasonography. Ninety-seven healthy age- and gender-matched controls (79 girls and 18 boys) without any signs of adrenarche were a random sample of children from the same district, obtained from the Finnish population register. Invitation letters were sent to the families of the children selected from the list by order sampling in each age and gender group, and approximately 20% of the control child population invited were willing to participate. Control children were examined during the same time period as the PA subjects. Children with central puberty, any endocrine disorder or long-term medication were excluded from both groups. At examination, girls in both groups had to be less than 9 y and boys less than 10 y of age. The study protocol was approved by the Research Ethics Committee of Kuopio University Hospital. Informed written consent from parents and assent from children were obtained for participation in the study, including collection and genotyping of DNA samples.
Clinical assessment.
The appearance time of the adrenarchal signs was obtained by interviewing the parents. Birth weight, birth length, and gestational age data were obtained from hospital records. The birth measures were converted to SD scores by plotting them on the growth charts and adjusting the birth measures for duration of gestation and gender (17). Height was measured with a calibrated Harpenden stadiometer three times and recorded to the nearest 0.1 cm. Weight was recorded to the nearest 0.1 kg. Weight was converted to percentages in relation to the median weight-for-height by using the national reference values (18). To exclude the presence of central puberty, the Tanner stage was determined by a single investigator (P.U.).
Endocrine-metabolic assessment.
An i.v. cannula was placed for blood sampling and ACTH administration. Baseline samples for plasma ACTH, serum cortisol, DHEA, DHEAS, and androstenedione (Δ4-A) measurements were drawn from all subjects after an overnight fast between 9:00 am and 10:00 am. Synthetic ACTH 1–24 (Synacthen; Novartis Pharma GmbH, Nürnberg, Germany) was administered 1 μg/1.73 m2 i.v. Serum samples for cortisol, DHEA and Δ4-A were taken 30 min after ACTH administration. After separation, all serum samples were immediately frozen and stored at −70°C until assayed.
Hormonal assays.
Serum DHEAS and Δ4-A concentrations were determined with the Coat-A-Count Radioimmunoassays (Diagnostic Products Corporation, Los Angeles, CA). The intra-assay CV was 3.8–5.3% and the inter-assay CV was 6.3–11% in the DHEAS assay depending on the hormone concentration, while those for the Δ4-A assay were 3.2–9.4% and 4.1–15.6%, respectively. DHEA was measured with an in-house immunoradiometric assay as described previously (4). Plasma ACTH concentrations were analyzed by an immunoradiometric assay (Nichols Institute Diagnostics, San Juan Capistrano, CA) for the first 125 subjects. The inter-assay CV was 6.4–8.4%. For the last 56 subjects, plasma ACTH concentrations were analyzed by the Immulite chemiluminescent immunometric assay (Diagnostic Products Corporation). The intra-assay CV was 3.1–9.6% and inter-assay CV was 5.1–9.4%. Serum cortisol concentrations were determined with the Immulite 2000 Cortisol chemiluminescence immunoassay (Diagnostic Products Corporation). The intra-assay CV was 5.2–7.4% and the inter-assay CV was 6.8–9.4%.
Genotyping.
DNA was isolated from full blood samples using the Wizard Genomic DNA Purification Kit (Promega, Madison, WI). The samples were genotyped for the MC2R −2 T>C polymorphism which disrupts an existing SacI restriction site CTC, using PCR and restriction enzyme digestion modified from the previously described (14). The forward primer 5′-GGG ATG ACA TTT ATT CAA GG-3′ starting at position −112 and the reverse primer 5′-AAG CAG GAA CTT TCT GGG-3′ starting at position +38 were used. PCR was performed with DyNAzyme II DNA polymerase (Finnzymes Oy, Espoo, Finland). After an initial denaturation step of 2 min at 96°C, PCR cycling was done for 35 cycles of 96°C for 25 s, 56°C for 25 s, 72°C for 30 s, and the final extension step at 72°C was for 5 min. PCR products were digested for 3 h at 37°C with SacI (10 U; New England Biolabs, Frankfurt, Germany). Fragments were separated on a 2.5% agarose gel. Samples with the C/C genotype revealed one band (150 bp), those with T/T revealed two bands (111 and 39 bp), and those with C/T revealed three bands (150, 111, and 39 bp). The genotype was confirmed by sequencing the C/C sample and randomly selected 10 C/T and 4 T/T samples with the ABI Prism BigDye Terminator v3.1 Cycle Sequencing Kit and an ABI PRISM 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA) in accordance with the manufacturer's instructions.
Data analysis.
Results are reported as mean (95% confidence interval). Statistical analysis was performed with SPSS 14.0 statistical package (SPSS Inc., Chicago, IL). The state of adrenarche according to the ACTH receptor promoter polymorphism was analyzed by Fisher's exact test. The Mann-Whitney U test was used in comparing variables between the genotype groups among the subjects with PA or controls, and between the subjects with PA and controls among the genotype groups. p < 0.05 was considered statistically significant.
RESULTS
The frequency of MC2R-2 T>C polymorphism was assessed in 171 Finnish children, 143 girls and 28 boys. The prevalence of the respective alleles was T/T homozygosity 86.0%, C/T heterozygosity 13.5% and C/C homozygosity 0.5%. These distributions were comparable to those reported in another Caucasian population (14), and were consistent with Hardy-Weinberg equilibrium (p = 0.92). The polymorphism group (T/C&C/C) was formed from the C/T heterozygotes and the C/C homozygote. There was no significant difference in the frequency of MC2R −2 T>C polymorphism between the control and the whole PA group (control vs. PA; T/C&C/C, 10.3% vs. 17.8%; p = 0.2). The MC2R promoter genotype distribution was similar in the control group and PA children without pubarche (Table 1). The frequency of the polymorphism was 28% in children with premature pubarche (PP), which was significantly higher than in the controls and the nonPP-PA children (p = 0.04; Table 1). When all children were divided into two groups by DHEAS concentration (DHEAS > 1.0 μM respecting biochemical adrenarche, n = 89; DHEAS < 1.0 μM, n = 81), the frequency of MC2R −2 T>C polymorphism was higher in the group of children with higher DHEAS level [T/C&C/C 16 (18.0%) vs. 7 (8.6%); p = 0.076]. However, the difference did not reach statistical significance.
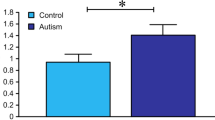
Table 2 summarizes the characteristics of the healthy controls and PA children, as subgrouped by the MC2R promoter genotype. Among the controls, the baseline hormone levels did not differ between the MC2R genotype groups. However, 30 min after ACTH stimulation, the mean serum cortisol concentration was 15% lower in the polymorphic than in the T/T subgroup, although the difference did not reach statistical significance (p = 0.05; Table 2). As an indicator of ACTH sensitivity, the baseline ACTH/cortisol ratio was calculated and it was significantly higher in the polymorphic than in the T/T subgroup (p = 0.002; Table 2). Among the PA children, there was no significant difference in the ACTH stimulated mean serum cortisol concentration or in the baseline ACTH/cortisol ratio between the genotype groups (Table 2). On the other hand, the PA subjects with the polymorphism had significantly higher baseline plasma ACTH, serum DHEA, and Δ4-A levels in comparison with the PA subjects with the T/T genotype (Table 2). The mean baseline serum cortisol concentration was 47% (p = 0.07) and the mean ACTH stimulated cortisol 20% higher (p = 0.02) in the PA subjects with the polymorphism compared with the controls with the same genotype (Table 2).
As an indicator of shifting steroidogenesis from glucocorticoids to adrenal androgens, we calculated the ratio of cortisol to Δ4-A. The children with the polymorphism had lower cortisol/Δ4-A ratios than those with the T/T genotype [114 (86,142) vs. 169 (152,185); p = 0.008]. The children with the polymorphism also had lower ACTH stimulated ratio of cortisol to Δ4-A [211 (154,269) vs. 306 (270,341); p = 0.005]. However, when the subgroups of children with PA and controls were analyzed separately, the difference between the genotype groups was not significant.
The PA subjects with the polymorphism had mean birth weight 0.7 SDS lower than the PA subjects with the T/T genotype (p = 0.02; Table 2). There was also a tendency for shorter birth length in the PA subjects with the polymorphism than in those with the T/T genotype (p = 0.08; Table 2). The PA subjects with the polymorphism had mean birth length 1.0 SDS shorter than the controls with the polymorphism (p = 0.02; Table 2). The birth measures of the PA subjects with the T/T genotype did not differ from those of the controls with the same genotype.
DISCUSSION
The etiology of premature adrenarche is complex and polygenic. Both intra- and interfamilial phenotypic and genotypic variability have been observed among adolescent subjects with female hyperandrogenism (19). The development of PP has been associated with multiple sequence variants, especially in genes involved in steroid synthesis (20,21) and androgen action (22,23).
In our study, the MC2R −2 T>C polymorphism was present in children with PP-PA at a higher frequency than in healthy children or non-PP-PA children. Our PA children with the MC2R −2 T>C polymorphism had higher baseline ACTH, DHEA, and Δ4-A levels, and lower birth weight than the PA children with the T/T genotype. In our previous study of the same children, the group of girls with nonPP-PA was found to have milder metabolic changes and slightly lower DHEAS levels than the girls with PP-PA (16). In this study, we found no differences in weight-for-height between the PA subjects with the MC2R −2 T>C polymorphism and those without it. On the other hand, no statistically significant differences were found in birth weight SD scores between the controls, nonPP-PA and PP-PA groups in the previous study (16).
Slawik and coworkers suggested that the MC2R −2 T>C polymorphism results in lower expression of the MC2R which may be compensated by higher plasma ACTH concentrations under basal conditions. During major stress, the reduced ACTH sensitivity of the adrenal cortex could become clinically relevant (14). Our finding of the higher ACTH/cortisol ratio in the polymorphic group of the healthy controls is in accordance with the previously reported higher ACTH/cortisol ratio among healthy adult men with the polymorphism (14). Interestingly, there was no difference in the ACTH/cortisol ratio between the subjects with the polymorphism and those without it in the PA subgroup.
Our subjects differed markedly by age, gender and adrenal function from those in the study of Slawik and coworkers. They assessed the frequency of the polymorphism in a large cohort over 1200 unrelated, healthy male blood donors, but the ACTH and CRH stimulation tests were performed only for 21 subjects with the age range of 20–35 y (n; 8 T/T; 7 C/T; 6 C/C) (14). The same subjects with T/T and C/C genotypes were further studied for DHEA and DHEAS responses to prolonged ACTH stimulation, and a significantly lower DHEA response was observed in subjects with the C/C genotype during the 60–340 min time frame (15). In our study, there was no significant difference in the androgen responses between the PA subjects with the polymorphism and those without it at 30 min after ACTH administration. In the healthy controls, adrenal glands had not yet started to produce significant amounts of androgens, and no difference in androgen levels between the genotype groups was seen. The differences between the used ACTH tests and the subjects may explain the diverse results in these two studies. In addition, our study group included only one subject with the C/C genotype. The heterozygous subjects have been reported to show intermediate values in the previous study (14). Because of the relatively small sample size and genetic homogeneity of the Finnish population, our results should be confirmed in other populations or, even more preferably, by large genome-wide association studies.
Slawik and coworkers reported no data on pubertal development or birth measures (14). Our PA subjects with the MC2R −2 T>C polymorphism had lower birth weight than those with the T/T genotype. Furthermore, the subjects with PA had shorter birth length than the controls among the children with the polymorphism. In the T/T group, there was no significant difference in birth measures between the PA and control children. Several studies have documented that children with low birth weight are more likely to manifest PA (24). PP in girls has been associated with subsequent development of ovarian hyperandrogenism, central obesity, hyperlipidemia, and insulin resistance during postpuberty, particularly in those subjects with a history of low birth weight and a rapid catch-up in weight postnatally (25,26). In addition, the relationship between lower birth weight and higher childhood adrenal androgen levels is continuous throughout the range of normal birth weights and is similar in boys and girls (27).
The reports on the association between size at birth and cortisol concentrations later in life are conflicting. However, the meta-analysis revealed an inverse association between birth weight and circulating cortisol level (28). It is not immediately apparent how premature adrenarche would be related to increased ACTH stimulated cortisol level observed in our PA subjects with the MC2R −2 T>C polymorphism compared with healthy controls with the polymorphism. Raised ACTH and cortisol levels do not necessarily associate with increased production of DHEA and DHEAS in children with Cushing disease or ectopic ACTH-producing tumors, but the secretion of Δ4-A may increase in these conditions (29). Among our PA subjects, especially the Δ4-A levels were higher in the polymorphic PA subgroup compared with the T/T PA subgroup.
Hypothalamo-pituitary-adrenal axis regulates its own functions. Glucocorticoids inhibit ACTH and corticotropin releasing hormone secretion by a long feedback, behind which a regulatory network of great complexity has been revealed (30). MC2R is expressed also in the human pituitary gland (31), and it has been postulated that ACTH may regulate its own secretion through ultra-short loop negative feedback at the pituitary level (32). Interestingly, ACTH increases the expression of its own MC2R mRNA and binding sites in adult (33) and fetal (34) human adrenocortical cells. On the other hand, glucocorticoids enhance ACTH receptor mRNA levels in ovine adrenocortical cells, and the trophic action of ACTH on its own receptors may thus be mediated by ACTH-induced steroidogenesis (35).
There are many physiologic and pathologic conditions in which a dissociation of adrenal androgen and cortisol secretion in response to ACTH is seen. The secretion of adrenal androgens has a distinct pattern from that of cortisol during fetal development, adrenarche and aging (24). Dissociation between plasma adrenal androgens (decreased) and cortisol (increased) has been reported in Cushing's disease (29), in critical and chronic illness (36–38), and even in functional hypothalamic amenorrhea (39). It has been postulated that in times of critical or chronic illness, steroid synthesis may be diverted from adrenal androgens to glucocorticoids to allow maintenance of high glucocorticoid levels which are crucial for coping with the illness (40). On the other hand, low DHEAS level has been suggested to be a marker and sign of exhausted adrenal reserve in critical illness (37). Indicated by the lower basal and stimulated cortisol/Δ4-A ratios in the children with the polymorphism, it is possible that decreased ACTH sensitivity due to the MC2R −2 T>C polymorphism shifts the adrenal steroidogenesis to the androgen pathway from cortisol synthesis. Thus, the mechanism would be opposite to the abovementioned stress syndromes.
We conclude that the higher baseline ACTH/cortisol ratio in healthy controls supports the previously reported lower ACTH sensitivity associating with the MC2R −2 T>C polymorphism. In addition, the frequency of this polymorphism was higher in PP-PA children than in healthy controls or in nonPP-PA children. In PA children, the MC2R −2 T>C polymorphism associated with lower birth weight and higher plasma ACTH and serum DHEA and Δ4-A concentrations. The etiology of premature adrenarche is complex and polygenic. Together with other genetic variations, polymorphism of the ACTH receptor is associated with the development of premature adrenarche.
Abbreviations
- Δ4-A:
-
androstenedione
- DHEA:
-
dehydroepiandrosterone
- DHEAS:
-
dehydroepiandrosterone sulfate
- MC2R:
-
melanocortin-2 receptor, ACTH receptor
- nonPP-PA:
-
premature adrenarche without pubarche
- PA:
-
premature adrenarche
- PP:
-
premature pubarche
- PP-PA:
-
premature adrenarche with premature pubarche
References
Voutilainen R, Perheentupa J, Apter D 1983 Benign premature adrenarche: clinical features and serum steroid levels. Acta Paediatr Scand 72: 707–711
Ibanez L, Dimartino-Nardi J, Potau N, Saenger P 2000 Premature adrenarche–normal variant or forerunner of adult disease?. Endocr Rev 21: 671–696
Ehrhart-Bornstein M, Hinson J, Bornstein S, Scherbaum W, Vinson G 1998 Intraadrenal interactions in the regulation of adrenocortical steroidogenesis. Endocr Rev 19: 101–143
Apter D, Pakarinen A, Hammond G, Vihko R 1979 Adrenocortical function in puberty - serum ACTH, cortisol and dehydroepiandrosterone in girls and boys. Acta Paediatr Scand 68: 599–604
Weber A, Clark A, Perry L, Honour J, Savage M 1997 Diminished adrenal androgen secretion in familial glucocorticoid deficiency implicates a significant role for ACTH in the induction of adrenarche. Clin Endocrinol (Oxf) 46: 431–437
Azziz R, Fox LM, Zacur HA, Parker CR, Boots LR 2001 Adrenocortical secretion of dehydroepiandrosterone in healthy women: highly variable response to adrenocorticotropin. J Clin Endocrinol Metab 86: 2513–2517
Rotter JI, Wong FL, Lifrak ET, Parker LN 1985 A genetic component to the variation of dehydroepiandrosterone sulfate. Metabolism 34: 731–736
Yildiz BO, Goodarzi MO, Guo X, Rotter JI, Azziz R 2006 Heritability of dehydroepiandrosterone sulfate in women with polycystic ovary syndrome and their sisters. Fertil Steril 86: 1688–1693
Legro RS, Driscoll D, Strauss JF III, Fox J, Dunaif A 1998 Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proc Natl Acad Sci USA 95: 14956–14960
Buckley DI, Ramachandran J 1981 Characterization of corticotropin receptors on adrenocortical cells. Proc Natl Acad Sci USA 78: 7431–7435
Gantz I, Fong T 2003 The melanocortin system. Am J Physiol Endocrinol Metab 284: E468–E474
Mountjoy KG, Robbins LS, Mortrud MT, Cone RD 1992 The cloning of a family of genes that encode the melanocortin receptors. Science 257: 1248–1251
Naville D, Jaillard C, Barjhoux L, Durand P, Begeot M 1997 Genomic structure and promoter characterization of the human ACTH receptor gene. Biochem Biophys Res Commun 230: 7–12
Slawik M, Reisch N, Zwermann O, Maser-Gluth C, Stahl M, Klink A, Reincke M, Beuschlein F 2004 Characterization of an adrenocorticotropin (ACTH) receptor promoter polymorphism leading to decreased adrenal responsiveness to ACTH. J Clin Endocrinol Metab 89: 3131–3137
Reisch N, Slawik M, Zwermann O, Beuschlein F, Reincke M 2005 Genetic influence of an ACTH receptor promoter polymorphism on adrenal androgen secretion. Eur J Endocrinol 153: 711–715
Utriainen P, Jääskeläinen J, Romppanen J, Voutilainen R 2007 Metabolic syndrome and its components in children with premature adrenarche. J Clin Endocrinol Metab 92: 4282–4285
Pihkala J, Hakala T, Voutilainen P, Raivio K 1989 [Characteristic of recent fetal growth curves in Finland]. Duodecim 105: 1540–1546
Sorva R, Perheentupa J, Lankinen S, Tolppanen EM 1990 Variation of growth in height and weight of children. II. After infancy. Acta Paediatr Scand 79: 498–506
Sanders EB, Aston CE, Ferrell RE, Witchel SF 2002 Inter- and intrafamilial variability in premature pubarche and polycystic ovary syndrome. Fertil Steril 78: 473–478
Witchel SF, Smith R, Tomboc M, Aston CE 2001 Candidate gene analysis in premature pubarche and adolescent hyperandrogenism. Fertil Steril 75: 724–730
Petry CJ, Ong KK, Michelmore KF, Artigas S, Wingate DL, Balen AH, de Zegher F, Ibáñez L, Dunger DB 2005 Association of aromatase (CYP 19) gene variation with features of hyperandrogenism in two populations of young women. Hum Reprod 20: 1837–1843
Ibanez L, Ong K, Mongan N, Jääskeläinen J, Marcos M, Hughes I, De Zegher F, Dunger D 2003 Androgen receptor gene CAG repeat polymorphism in the development of ovarian hyperandrogenism. J Clin Endocrinol Metab 88: 3333–3338
Vottero A, Capelletti M, Giuliodori S, Viani I, Ziveri M, Neri T, Bernasconi S, Ghizzoni L 2006 Decreased androgen receptor gene methylation in premature pubarche: A novel pathogenetic mechanism?. J Clin Endocrinol Metab 91: 968–972
Auchus RJ, Rainey WE 2004 Adrenarche—physiology, biochemistry and human disease. Clin Endocrinol (Oxf) 60: 288–296
Ibanez L, Potau N, Chacon P, Pascual C, Carrascosa A 1998 Hyperinsulinaemia, dyslipaemia and cardiovascular risk in girls with a history of premature pubarche. Diabetologia 41: 1057–1063
Ibanez L, Potau N, Francois I, de Zegher F 1998 Precocious pubarche, hyperinsulinism, and ovarian hyperandrogenism in girls: relation to reduced fetal growth. J Clin Endocrinol Metab 83: 3558–3562
Ong KK, Potau N, Petry CJ, Jones R, Ness AR, Honour JW, de Zegher F, Ibanez L, Dunger DB 2004 Opposing influences of prenatal and postnatal weight gain on adrenarche in normal boys and girls. J Clin Endocrinol Metab 89: 2647–2651
van Montfoort N, Finken MJ, le Cessie S, Dekker FW, Wit JM 2005 Could cortisol explain the association between birth weight and cardiovascular disease in later life? A meta-analysis. Eur J Endocrinol 153: 811–817
Hauffa BP, Kaplan SL, Grumbach MM 1984 Dissociation between plasma adrenal androgens and cortisol in Cushing's disease and ectopic ACTH-producing tumour: relation to adrenarche. Lancet 1: 1373–1376
Watts AG 2005 Glucocorticoid regulation of peptide genes in neuroendocrine CRH neurons: a complexity beyond negative feedback. Front Neuroendocrinol 26: 109–130
Morris DG, Kola B, Borboli N, Kaltsas GA, Gueorguiev M, McNicol AM, Ferrier R, Jones TH, Baldeweg S, Powell M, Czirjak S, Hanzely Z, Johansson JO, Korbonits M, Grossman AB 2003 Identification of adrenocorticotropin receptor messenger ribonucleic acid in the human pituitary and its loss of expression in pituitary adenomas. J Clin Endocrinol Metab 88: 6080–6087
Boscaro M, Sonino N, Paoletta A, Rampazzo A, Mantero F 1988 Evidence for ultra-short loop autoregulation of adrenocorticotropin secretion in man. J Clin Endocrinol Metab 66: 255–257
Lebrethon MC, Naville D, Begeot M, Saez JM 1994 Regulation of corticotropin receptor number and messenger RNA in cultured human adrenocortical cells by corticotropin and angiotensin II. J Clin Invest 93: 1828–1833
Mesiano S, Fujimoto VY, Nelson LR, Lee JY, Voytek CC, Jaffe RB 1996 Localization and regulation of corticotropin receptor expression in the midgestation human fetal adrenal cortex: implications for in utero homeostasis. J Clin Endocrinol Metab 81: 340–345
Picard-Hagen N, Penhoat A, Hue D, Jaillard C, Durand P 1997 Glucocorticoids enhance corticotropin receptor mRNA levels in ovine adrenocortical cells. J Mol Endocrinol 19: 29–36
Luppa P, Munker R, Nagel D, Weber M, Engelhardt D 1991 Serum androgens in intensive-care patients: correlations with clinical findings. Clin Endocrinol (Oxf) 34: 305–310
Beishuizen A, Thijs L, Vermes I 2002 Decreased levels of dehydroepiandrosterone sulphate in severe critical illness: a sign of exhausted adrenal reserve?. Crit Care 6: 434–438
Dimopoulou I, Stamoulis K, Ilias I, Tzanela M, Lyberopoulos P, Orfanos S, Armaganidis A, Theodorakopoulou M, Tsagarakis S 2007 A prospective study on adrenal cortex responses and outcome prediction in acute critical illness: results from a large cohort of 203 mixed ICU patients. Intensive Care Med 33: 2116–2121
Bomba M, Gambera A, Bonini L, Peroni M, Neri F, Scagliola P, Nacinovich R 2007 Endocrine profiles and neuropsychologic correlates of functional hypothalamic amenorrhea in adolescents. Fertil Steril 87: 876–885
Bornstein SR, Chrousos GP 1999 Clinical review 104: adrenocorticotropin (ACTH)- and non-ACTH-mediated regulation of the adrenal cortex: neural and immune inputs. J Clin Endocrinol Metab 84: 1729–1736
Acknowledgements
Ms Mari Tuovinen and Ms Minna Heiskanen are thanked for their skilful assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Kuopio University Hospital, Pediatric Research Foundation, Academy of Finland, The Finnish Medical Foundation and Sigrid Jusélius Foundation.
Rights and permissions
About this article
Cite this article
Lappalainen, S., Utriainen, P., Kuulasmaa, T. et al. ACTH Receptor Promoter Polymorphism Associates With Severity of Premature Adrenarche and Modulates Hypothalamo-Pituitary-Adrenal Axis in Children. Pediatr Res 63, 410–414 (2008). https://doi.org/10.1203/PDR.0b013e3181659c14
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181659c14
This article is cited by
-
Family of melanocortin receptor (MCR) genes in mammals—mutations, polymorphisms and phenotypic effects
Journal of Applied Genetics (2013)