Abstract
Human milk fat globule (HMFG) glycoproteins can prevent infections by microorganisms in breast-fed infants; the MUC-1 mucin inhibits binding of S-fimbriated Escherchia coli to buccal mucosa, and lactadherin may prevent symptomatic rotavirus infections. In this study, the survival of these HMFG glycoproteins in the stomach of human milk-fed preterm infants (gestational age = 27.5 ± 0.4 wk) was assessed, and levels in their mother's milk determined, using specific RIAs. Butyrophilin, a major component of HMFG membrane that has no demonstrated antimicrobial activity, was studied for comparison. The levels of mucin, lactadherin, and butyrophilin in 41 milk samples of 20 mothers were 729 ± 75, 93 ± 10, and 41 ± 3 µg/mL, respectively. Mucin and lactadherin were significantly higher in early milk samples (<15 d postpartum) than in later milk samples (15-90 d postpartum), whereas butyrophilin showed no such difference. Significant amounts of mucin and lactadherin were found in almost all gastric aspirates of human milk-fed infants, even 4 h after feeding (mucin, 270 ± 30 µg/mL; lactadherin, 23.2 ± 4.4 µg/mL), whereas butyrophilin was rapidly degraded in the majority of aspirates. Western blot analysis demonstrated that the immunoreactive mucin, lactadherin, and butyrophilin in the milk-fed gastric aspirates had the expected native molecular weights. Mucin and lactadherin survived at all gastric pH values, whereas butyrophilin was found only at pH > 4. Neither lactadherin nor butyrophilin were detected in gastric aspirates of formula-fed infants (gestational age = 27.8 ± 0.5 wk), whereas the very low level of mucin (9.1 ± 1.1 µg/mL) in this group is presumably cross-reacting gastric mucin. These results demonstrate that two HMFG glycoproteins implicated in prevention of infection, MUC-1 mucin and lactadherin, survive and maintain their integrity in the stomachs of human milk-fed preterm infants.
Similar content being viewed by others
Main
The immune response is not well developed at birth (1,2). The preterm infant is even more deficient in this respect than those at full-term (3). A large number of studies have shown that breast-fed infants have lower incidence of gastrointestinal and respiratory system infections than do bottle-fed infants (4–6).
Although many of these studies were carried out in developing countries (5,7), a protective effect of breast-feeding has also been reported in developed countries (6,8,9). Indeed, in addition to protection against specific microorganisms provided by the high concentration of IgA (1,10,11), human milk is rich in other components that provide nonspecific, broad range protection against infection (12–16). Among these components are human milk fat globule glycoproteins, such as mucins (13,15) and lactadherin (14,17), both of which may act as receptor analogs and thereby inhibit the adhesion of enteric and respiratory microorganisms (13,14,16).
The MUC-1 mucin and lactadherin, both major components of the milk fat globule membrane, have been extensively studied qualitatively, whereas quantitative studies of their levels in mother's milk are limited. One report suggests approximately 40 µg/mL mucin in the milk of mothers of full-term infants (15). The level of lactadherin in human milk is unknown. The cDNA cloning of the MUC-1 mucin reveals a small cytoplasmic segment, a transmembrane domain, and an extended extracellular domain consisting primarily of a variable number of 20 amino acid tandem repeats that are extensively O-glycosylated, being rich in proline, serine, and threonine (18). Most antibodies against the MUC-1 mucin recognize polypeptide epitopes in an immunodominant region of the tandem repeat (19–21). The MUC-1 mucin is expressed by most secretory epithelial cells, but the milk mucin differs considerably from that of other tissues in glycosylation (21). Lactadherin is an N-glycosylated 46-kD glycoprotein containing an N-terminal RGD (ArgGlyAsp)-containing cell adhesion sequence that binds to the αvβ3-integrin and a C-terminal sequence with homology to the phosphatidylserine-binding C1/C2 domain of coagulation factors V and VIII (22). The RGD cell adhesion sequence is inserted within a EGF-like motif (23). These two principal domains of lactadherin are conserved in lactadherin from human, mouse, rat, and bovine milk, whereas the latter three species contain an second EGF-like sequence (22).
Because of the greater need of premature infants for protection against infection, it was of interest to qualify these glycoproteins in the milk of mothers of very low bith weight infants and to examine whether concentrations change as a function of length of lactation during the first 3 mo after delivery. Furthermore, we have also quantified mucin and lactadherin in gastric aspirates obtained from the infants to ascertain whether these milk glycoproteins maintain their integrity and therefore might be able to act in the stomach and intestine of the newborn. For comparison, we have also quantified human butyrophilin (24), another major component of the MFG membrane without any known protective function (25), in milk and gastric aspirates of the same mothers and their infants, respectively.
METHODS
Subjects. Thirty-two preterm infants were the subjects of this study. All infants were initially maintained on total parenteral nutrition. Partial gastric gavage feedings were started when judged appropriate by the neonatalogist in charge. Enteral feedings were either mother's own milk or formula (SMA Super Preemie formula, Wyeth Ayerst Laboratory, Philadelphia, PA). The studies were approved by the Institutional Review Board of Georgetown University Hospital, and informed consent was obtained from the parent(s).
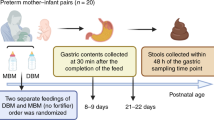
Milk collection. Twenty of the mothers who decided to breast-feed expressed milk with the aid of a Medela or Egnell breast pump into sterile containers before feeding to the infants. Between expression and feeding, the milk was kept in the refrigerator or freezer according to need. Aliquots from freshly expressed milk were transferred to sterile plastic tubes for storage at -70°C until analysis.
Collection of gastric aspirates. The studies were conducted in the morning and were started 2-3.5 h after the end of the previous meal. A nasogastric tube (French #8) was passed to the stomach, and the gastric content was aspirated into a syringe. Volume, pH, and appearance were recorded, and the pH of the sample was adjusted when necessary to 4.0-4.5 with a few drops of 0.1 N NaOH to avoid storage at very low pH. All specimens were collected on ice and stored at -70°C until analysis.
Mucin quantitation. Milk mucin was quantified in each milk and gastric aspirate sample using two competitive RIAs the differed in the detecting ant-mucin MAb used, either Mc5 or BrE3. Microtiter plates were coated with the fusion protein NP11-2 containing the sequence of the MUC-1 mucin tandem repeat (26), as previously described (27). Just before an assay, the plates were washed with RIA buffer (10% bovine serum, 0.03% Triton X-100, and 0.05% sodium azide in PBS). Thirty microliters of a serial dilution of mucin standard or sample were added to the NP11-2-coated wells, in triplicate. To each well, 20 µL of anti-mucin antibody were then added (1.5 µg/mL in RIA buffer). The plates were covered with a nonporous tape and incubated overnight at room temperature. The wells were then washed four times with RIA buffer, and 50 µL of 125I-labeled goat anti-mouse IgG (200,000 cpm/50 µL, specific activity 10 µCi/µg) were added per well and allowed to react for 3 h at room temperature. Iodination of Ig was done by the chloramine-T method (28). Finally, the wells were again washed with RIA buffer and counted for radioactivity. Affinity-purified mucin from delipidated HMFG (27), diluted in RIA buffer (0.01, 0.03, 0.1, 0.3, 1, 3, and 10 µg/mL), was used as a standard. The milk and gastric aspirate samples from milk-fed infants were sonicated in a water bath sonicator (Bronsonic 221, Bronson, Shelton, CT), and then diluted 1:100 and 1:1000 in RIA buffer. The gastric aspirate samples from formula-fed infants were sonicated and diluted 1:10 and 1:100. Both anti-mucin MAbs used in the assays recognized repeated polypeptide epitopes on the tandem repeat sequence of the mucin core protein. Mc5 recognizes the amino acid sequence AspThrArgProAlaPro and BrE3 recognizes the sequence ThrArgPro on the mucin tandem repeat (21). Glycosylation of the mucin tandem repeat increases the binding of Mc5 to its epitopes (21). The BrE3 epitope is masked by glycosylation, and binding of BrE3 to the native glycosylated milk mucin is explained by heterogeneous glycosylation of the multiepitopic tandem repeat, leaving some repeats nonglycosylated (21). Comparison of Mc5 and BrE3 assays of mucin concentration in each sample allowed quantitative evaluation of different glycoforms of the MUC-1 mucin that were present. The mucin standard curve was plotted on a semi-log scale (counts/min versus log concentration). The concentration of mucin in the samples (diluted 1/1000 for all milk samples and 1/100 and 1/1000 for gastric aspirates of milk-fed infants) was determined by comparison with the linear segment (between 0.03 and 3.0 µg/mL) of the mucin standard curve plotted on semilog scale. The minimal detectable concentration with the assays was 0.05 µg/mL. Because the lowest dilution of samples assayed was 1/10 (for aspirates of formula-fed infants), the minimal detectable concentration in any samples was 0.5 µg/mL. The variability in the mucin assay was determined by calculating the %CV for multiple assays. The mean %CV (± SEM) for interassay variability was 18.4 ± 2.0% and for intraassay variability was 11.0 ± 1.0%.
Lactadherin and butyrophilin quantitation. Lactadherin and butyrophilin were assayed using a quantitative end point dilution radioimmunobinding method. Serial dilutions (1/100-1/10,000) of human milk and gastric aspirate samples were dried onto methylated BSA-coated microtiter plates (50 µL/well) as we have previously described (29). Milk and gastric aspirates were sonicated for 10 min using a water bath sonicator, before dilution in detergent buffer (0.3% Triton X-100, 0.02% NaN3 in PBS). Lactadherin, purified by a Triton X-114 phase partition method (22) and human butyrophilin (24), purified by preparative SDS-PAGE, were used as standards. The concentration of the purified proteins was determined by a bicinchoninic protein assay (Pierce, Rockford IL).
Fifty microliters of the MAb Mc3 or Mc13 (30), diluted in RIA buffer to 5 µg/mL, were added per well. MAb Mc3 identifies an epitope on the EGF-like/RGD domain of human lactadherin (22), whereas MAb Mc13 identifies human butyrophilin (24). Both Mc3 and Mc13 recognize polypeptide epitopes on these glycoproteins, because deglycosylation of the antigens does not decrease their ability to recognize the proteins on Western blot analysis (J.A.P., unpublished results). The wells were covered and incubated with agitation for 2-3 h before being washed five times with RIA buffer. Then 50 µL of 125I-labeled goat anti-mouse IgG (200,000 cpm/well) were added to each well, the plates were incubated for 1-3 h and washed, and the wells were cut off and counted for radioactivity. Positive and negative controls were included in each assay. The dilutions of the milk and gastric aspirate samples that resulted in counts/min bound to the well that fell within the linear portion of standard curves (between 10 and 100 ng/mL for both lactadherin and butyrophilin) of diluted purified proteins were used to determine the concentration of lactadherin and butyrophilin in the samples. The minimal detectable concentration of both lactadherin and butyrophilin in an assay was therefore 10 ng/mL. Because the lowest dilution of samples was 1/100, the minimum concentration in the samples was 1 µg/mL for both assays. The interassay and intraassay variability for the lactadherin were 20.8 ± 2.4% and 4.8 ± 0.7% (%CV, mean ± SEM), respectively. For butyrophilin, the interassay and intraassay variability (%CV) were 20.9 ± 2.8% and 5.7 ± 1.1%, respectively.
Considering the complexity of the samples tested and the dependence of both lactadherin and butyrophilin assays on the nonspecific binding of these constituents to microtiter plates, it was important to determine whether the gastric aspirate samples cause a "matrix effect" that could significantly influence the results. To determine this, gastric aspirates from milk- and formula-fed infants were added to known amounts of the purified proteins and assayed for the proteins, and the results were compared with assays performed on the purified proteins diluted in detergent buffer alone. The gastric aspirates were diluted 1/100 and 1/1000 in detergent buffer and added to concentrations of either lactadherin or butyrophilin ranging from 0.01 to 10 µg/mL. The presence of the gastric fluids at either dilution had no effect on the slope of dilution curves but did caused a minor shift in the curve. For lactadherin, the gastric fluids diluted 1/100 caused a 48% reduction in the measured concentration, whereas a 1/1000 dilution caused only a 15% reduction. For butyrophilin, the gastric fluids diluted 1/100 gave a 54% reduction, and a 1/1000 dilution caused a 20% increase in the measured concentration. Because the concentrations of both lactadherin and butyrophilin were determined in samples diluted 1/1000 or more, we conclude that the maximum error from any matrix effect would be 20%. Because the levels of these proteins we detect in gastric aspirates of milk-fed infants are 10-100-fold higher than the minimal assay sensitivities or in aspirates of formula-fed infants, this matrix effect does not influence our conclusion that significant amounts of lactadherin are present in stomachs of the majority milk-fed infants and may have resulted in an underestimation of the persistence of these constituents in the gastric aspirates.
Western blot analysis of gastric aspirates. The integrity of the glycoproteins in gastric aspirates was analyzed by Western blot SDS-PAGE. Milk and gastric aspirate samples were loaded onto precast 4-15% gradient SDS-polyacrylamide gels (Bio-Rad, Hercules, CA) and run in the presence of 0.025 M Tris-HCl, pH 8.3, 0.192 M glycine, 0.1% SDS. After transferring to nitrocellulose membranes, the proteins were detected using MAb Mc5 for the mucin, MAbs Mc8 and Mc16 for lactadherin, and MAb Mc13 for butyrophilin. Mc5, Mc8, and Mc16 identify defined peptide epitopes on their respective proteins, as determined by epitope mapping (21). The defined epitope for Mc13 on butyrophilin has not been determined, but it recognizes the polypeptide moiety, because it binds to deglycosylated butyrophilin just as well as to the native glycoprotein on Western blots.
Statistics. For the comparison of the levels of milk mucin measured by the two anti-mucin MAbs, Mc5 and BrE3, in the milk and gastric aspirate samples, we determined the correlation coefficient, r, and the equation for the regression coefficients by plotting the data on Harvard Graphics. The significance (p) of the correlation between the Mc5 and BrE3 assays was then determined from these r values.
RESULTS
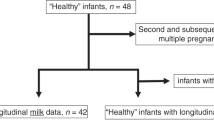
Clinical data on the infants studied are given in Table 1. All infants were premature (24-30-wk gestational age), 20 of the infants were milk-fed, and 12 infants were formula-fed. Fifty-seven gastric aspirate samples were taken from the human milk-fed infants and 31 samples from the formula-fed infants (Table 1). In some cases, the time interval between feedings was recorded, which allowed the assessment of survival of the milk proteins in the gastric aspirates as a function of time after feeding. In both the milk-fed and formula-fed groups there were a few occasions when the samples were taken before initiation of gastric gavage feeding, when the infants were maintained on total parenteral nutrition (14 gastric aspirates). These latter samples formed a third group (no oral feeding).
Longitudinal variation of HMFG glycoprotein content in milk during the first three months of lactation. To provide reference values for assessment of survival of milk HMFG glycoproteins in the stomachs of the infants, we initially measured the levels of lactadherin, mucin, and butyrophilin in 41 milk samples, taken at various times postpartum (0-90 d) from the mothers of the 20 milk-fed infants included in the study. Overall, there was considerable variation in levels of all three glycoproteins, both when comparing the levels in milk samples from different mothers and in samples from the same mother taken at different times during lactation (Fig. 1). For both the milk mucin and lactadherin, the levels were significantly higher in early lactation, up to d 15 postpartum, compared with milk samples taken 20 d postpartum and beyond (Table 2 and Fig. 1). Furthermore, consecutive samples taken from the same mother, in general, showed a decrease in milk mucin and lactadherin with increasing length of lactation (Fig. 1). In contrast, butyrophilin showed no consistent trend with length of lactation (Fig. 1). There appeared to be greater differences when comparing butyrophilin levels in different women than when comparing levels in milk samples taken from the same women at different times postpartum. In some women, milk butyrophilin increased with length of lactation, whereas in others the level decreased. In general, the women who started with higher milk butyrophilin, maintained higher levels during later lactation, compared with women who started with lower levels. The mean molar concentration of lactadherin (∼46 kD) and milk mucin (∼400 kD) in the combined milk samples were similar, 2.0 and 1.8 mM, respectively. Butyrophilin (∼70 kD) was present at a lower relative molar concentration of 0.6 mM. When comparing the levels of these three proteins in individual samples, there was a significant (p < 0.001) correlation between levels of mucin and lactadherin, whereas there was no correlation between the level of butyrophilin and lactadherin and only a marginally significant (p < 0.05) correlation between butyrophilin and mucin levels in the milk samples.
Longitudinal variation in milk mucin (A), lactadherin (B), and butyrophilin (C) in milk samples collected for mothers of preterm infants. Each symbol represents an individual mother, and those symbols connected by lines are samples from the same mother collected at different times postpartum. Mucin was assayed using MAb Mc5. See "Methods."
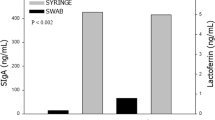
Glycoprotein content in gastric aspirates of human milk-fed and formula-fed preterm infants. The infants were gradually introduced to gastric gavage feeding while still maintained on i.v. feeding. The gastric aspirates were, therefore, collected from milk-fed or formula-fed infants at different degrees of gavage feeding (Fig. 2). This included <50% milk-fed, >50% milk-fed, or formula-fed and exclusively enterally fed infants for 2, 4, and 8 wk (Fig. 2). In the 20 milk-fed infants, milk mucin was found in all gastric aspirates (57/57), and lactadherin in 40 of 57 aspirates. In both cases, there was a very wide range of values in the gastric aspirates, but significant levels of mucin and lactadherin were present, some values were as high as in some milk samples. The mean concentrations of mucin and lactadherin in the combined gastric aspirate samples were 36 and 25%, respectively, of the mean concentrations of the combined milk samples (Table 2). The lowest levels of the mucin and lactadherin were found in the group with less than 50% milk-feeding. In contrast, butyrophilin was detected in only 6 of the 57 gastric aspirates of these milk-fed infants. The mean concentration of butyrophilin in the combined aspirate samples was only 2% of the mean concentration in the milk samples (Table 2). The six aspirates in which butyrophilin was detected (ranging from 3.8 to 15 µg/mL) were significantly above the level of detection of the assay (1 µg/mL). The remaining aspirates were below the level of detection, therefore less than 2% the mean concentration found in milk. This clearly indicates that there is a selective breakdown of butyrophilin compared with lactadherin and mucin in the stomach of these milk-fed infants.
ucin (A), lactadherin (B), and butyrophilin (C) in gastric aspirates of milk-fed preterm infants with different degrees of oral feeding. NPO = no oral feeding; <50% = less than 50% oral feeding; >50% = more than 50% oral feeding; 2wk = 2 wk of oral feeding; 4wk = 4 wk of oral feeding; 8wk = 8 wk of oral feeding. Mucin was assayed using MAb Mc5. See "Methods."
Lactadherin and butyrophilin were not detected in the gastric aspirates of formula-fed infants. Considering the sensitivity of the assays (1 µg/mL for both), there is less than 1 and 2%, respectively, of the concentrations of lactadherin and butyrophilin found in milk (Table 2). On the other hand, minimal levels of mucin were found in gastric aspirates of formula-fed infants. This mucin material detected is most likely cross-reacting gastric mucin produced by the gastric mucosa, because it is qualitatively different with regard to reactivity with the two anti-MUC-1 mucin MAbs, Mc5 and BrE3 (Table 2), and because gastric aspirates from the infants who received no oral feeding had higher levels of this mucin than the formula-fed group (see "Discussion").
To determine whether the HMFG glycoproteins found in the gastric aspirates of milk-fed infants maintain their integrity, gastric aspirates that were found to contain the immunoreactive glycoproteins were analyzed by Western blot SDS-PAGE. In the several gastric aspirate samples analyzed, MUC-1 mucin and lactadherin were found to migrated in identical positions compared with the respective glycoproteins from whole milk of the infants' mothers (Fig. 3) with no breakdown products observed. In the case of butyrophilin the intact molecule was detected, but there were also bands of smaller apparent molecular weight, indicating breakdown products, which is consistent with the major thesis of this study. With respect to the large molecular weight polymorphic mucin, the larger species do not enter the 4-15% gradient gel, but the positions of the smaller species from the mother and her infant's gastric aspirate that enter the gel were identical (Fig. 3). Intact lactadherin was detected in the several gastric aspirates tested by two anti-lactadherin MAbs, Mc8 and Mc16, both of which identify polypeptide epitopes in the C-terminal end of the protein (21). Neither mucin, lactadherin, nor butyrophilin were detected by Western blot analysis of gastric aspirates of formula-fed infants (not shown).
Western blot/SDS-PAGE analysis of a gastric aspirate that contains immunoreactive mucin, lactadherin, and butyrophilin. Lanes 1, 3, and 5, whole milk sample of mother of the infant whose gastric aspirate was analyzed. Lanes 2, 4, and 6, gastric aspirate sample of infant. Lanes 1 and 2, Western blot with anti-mucin MAb Mc5 (M = position of mucin). Lanes 3 and 4, Western blot with anti-lactadherin MAb Mc8 (L = position of lactadherin). Lanes 5 and 6, Western blot with anti-butyrophilin MAb Mc13 (B = position of butyrophilin). Positions of molecular weight standards (×1000) are along left margin. See "Methods."
Effect of gastric pH and time after feeding on amount of milk glycoproteins in gastric contents of preterm infants. Two factors that could affect the levels of HMFG glycoproteins in the gastric aspirates were analyzed in this study: 1) the time interval between feeding and collection of the aspirates, and 2) the pH of the gastric fluid. In general, the gastric aspirates were collected 2-3.5 h after feeding. Because in about half of the collections the actual time interval between feedings was recorded, it allowed an analysis of the survival time of these samples in the stomach of the infants. As can be seen in Figure 4, there is a trend of decreasing concentration of all three proteins with greater time interval between feeding and aspirate collection; however, even after 3.5 h there were significant amounts of both mucin and lactadherin in some gastric aspirates. Of the four samples that had detectable levels of butyrophilin in this group of aspirates, two were collected 3 h after feeding.
The pH in the gastric aspirate samples collected ranged from 1 to 7. Significant levels of mucin and lactadherin were detected throughout the entire pH range (Fig. 5). In contrast, butyrophilin could be detected only when gastric aspirate pH was above 4.0 (Fig. 5). The data indicate that butyrophilin is pH-labile, contrary to the other two milk glycoproteins studied.
DISCUSSION
In this study we have quantified three glycoproteins (MUC-1 mucin, lactadherin, and butyrophilin) in the milk of women who delivered prematurely and have assessed the stability and integrity of these glycoproteins in the stomach of their milk-fed preterm infants. We have chosen to study these glycoproteins because of their specific functions. Lactadherin and MUC-1 mucin have been shown to provide protection against infection of invasive microorganisms (13–15). Butyrophilin has been described as a structural component of the human milk fat globule (31), but it may have other functions, one of which could be as a specific receptor, suggested by its amino acid sequence (24,25). Although these glycoproteins appear to be functionally important in milk and in the infant, their quantity in milk, especially as a function of duration of lactation, has not been assessed previously. The data show that quantitative changes of mucin and lactadherin parallel those of the changes in the size of milk fat globules during early lactation, when size increases from a diameter of 0.5 µm in colostrum to about 4.0 µm in mature milk. This change is accomplished faster in the mammary gland of women who deliver at term (32) and takes somewhat longer after premature delivery (33). This might explain the high levels of mucin and lactadherin, components of the milk fat globule membrane during the first 2 wk of lactation when total membrane content is highest. Butyrophilin does not follow this pattern, probably because it is closely associated with the core globule triglyceride (34). Indeed, although there were significant correlations between mucin, lactadherin, and milk phospholipid (p = 0.001-0.05), butyrophilin, a lipophilic constituent of the milk fat globule membrane, was significantly correlated (p = 0.001) to the total lipid of the milk fat globule core, but not to the phospholipid of the milk fat globule membrane (35). Indeed, the level of butyrophilin increases in many milk specimens in the course of lactation (Fig. 1) in parallel with the raise in milk triglyceride content (36).
Our study shows that considerable amounts of lactadherin and mucin are still present in the stomach 2–3 h after feeding, indicating that, contrary to butyrophilin, the former two glycoproteins are resistant to gastric conditions such as low pH and pepsin activity. This finding is not very surprising in light of the remarkable resistance of human milk glycoproteins, such as IgA, lactoferrin, lysozyme, and the digestive enzymes bile salt-dependent lipase and amylase, in the digestive tract of the newborn (37–40). This resistance is probably associated with the high degree of glycosylation, a property not only of the glycoproteins secreted by the mammary gland. The relatively high gastric pH of the newborn (41) prevents the proteolytic action of pepsin, which is optimal at pH 1.8. Furthermore, pepsin activity is very low in the newborn (41) compared with the adult (42). The presence of bioactive fragments of lactoferrin, lysozyme, and IgA in the stools (37–39) and urine (39,43,44) of breast-fed infants has been reported earlier. Indeed, large fragments of mucin (∼200,000 daltons) and even intact mucin (45) that maintain their ligand activity and inhibit adhesion of microorganisms to epithelial cells (46,47) have recently been isolated from the stools of breast-fed infants (46).
The presence of similar bioactive mucin in meconium and stools of formula-fed infants (46) indicates that mucin intrinsic to the gastrointestinal system may also contribute to the protection of the newborn. The three HMFG glycoproteins in the gastric aspirates of the milk-fed infants are clearly the result of milk feeding, because there were no detectable levels of lactadherin or butyrophilin in any of the 31 gastric aspirates collected from the 12 formula-fed infants, regardless of the degree of feeding, and only minimal levels of mucin were detectable (Table 2). We assume that what we detect in the gastric aspirates of formula-fed infants with the anti-mucin antibodies is cross-reacting MUC-1 mucin produced by the gastric mucosa or other cells of the gastrointestinal tract. It is known that the MUC-1 mucin is expressed by all secretory epithelial cells; however, the mucin in different epithelial cells has different specificities for anti-MUC-1 mucin antibodies based on the pattern of glycosylation (20). Evidence for this is that higher levels of cross-reacting material, with both antibodies used in our mucin assays, were detected in gastric aspirates of infants who received no oral feeding (only i.v. feeding) (Table 2). The gastric aspirates from infants receiving no oral feeding were collected from both infants that were subsequently in the milk-fed or in the formula-fed groups. These 14 gastric aspirates (12 infants from the subsequently formula-fed group and 2 infants from the subsequently milk-fed group) had no detectable levels of lactadherin or butyrophilin, but had significantly higher levels of mucin compared with the formula-fed group (Table 2). We attribute the higher levels of mucin in infants maintained an total parenteral nutrition compared with the formula-fed infants, to the detection of cross-reacting MUC-1 mucin produced by the gastric mucosa. With no oral feeding there would be less dilution of any of the mucin produced in situ, which would be diluted with the formula in the formula-fed infants. Furthermore, the mucin in gastric aspirates of premature infants appears to be qualitatively different from the mucin in milk and in the gastric aspirates of milk-fed infants. The two MAb used in our assays, Mc5 and BrE-3, react with distinct and defined epitopes on the tandem repeat domain of the MUC-1 mucin. Mc5 recognizes the amino acid sequence AspThrArgProAlaPro but its affinity is increased by glycosylation of the mucin (21). On the other hand, BrE-3 recognizes the amino acid epitope ThrArgPro, and this epitope is masked by glycosylation (21). When the values obtained by the mucin assays with these two MAbs are compared in the milk samples, regression analysis shows a very significant correlation (p < 0.001) with a regression coefficient of 1.044, indicating a near 1 to 1 correlation between the two assays. When a similar analysis is done with Mc5 and BrE-3 assays of the gastric aspirate samples from the infants with no oral feeding, regression analysis also shows a highly significant correlation (p < 0.001), whereas the regression coefficient is 0.26, indicating that for every unit increase in the BrE-3 assay there are 4 units of increase in the Mc5 values. In both cases the standard curve is obtained with affinity-purified milk mucin. The Mc5 and BrE-3 assays on gastric aspirate samples of milk-fed infants also have a highly significant correlation coefficient (p < 0.001), with a regression coefficient of 0.96. This difference in the regression coefficients indicates that the mucin detected in the gastric aspirates obtained from infants receiving no enteral feeding is qualitatively different from that in milk and gastric aspirates of milk-fed infants, probably representing cross-reacting gastric MUC-1 mucin.
Western blot analysis of gastric aspirates that contained the glycoproteins by the immunoassays demonstrated intact molecules migrating at identical positions to those found in whole milk of the infants' mother. Also, the similarity in the regression coefficients (approximately 1.0) between the Mc5 and BrE3 assays, suggests that the tandem repeat domain and its characteristic pattern of glycosylation of the mucin is maintained intact in the gastric aspirates. In addition, the maintenance of integrity of the mucin is supported by the observation that intact, bioactive mucin can be recovered from feces of milk-fed infants (45). With regard to lactadherin, the fact that it is detected with MAb Mc3 in the immunoassay suggests that the cell adhesion domain (EGF-like/RGD) is in its native configuration. We have previously shown that MAb Mc3 inhibits lactadherin-promoted cell adhesion and its binding to lactadherin can be abolished by heat treatment under reducing conditions (22). Because epitope mapping of lactadherin using overlapping peptides spanning the entire sequence was unable to detect any binding of Mc3, this antibody appears to bind to an epitope requiring the proper tertiary folded structure (21). Further support for the intactness of lactadherin in the aspirates is that Mc3 binds to the N-terminal portion of lactadherin and Mc8 and Mc16 (used in the Western blot analysis) bind to defined epitopes in the C-terminal portion (21). For only butyrophilin was there any evidence of breakdown products in the Western blot analysis.
Some studies show that endogenous glycoproteins of the gastrointestinal mucosa might be able to protect the digestive system of the newborn from invasive microorganisms (48). This protective effect could, however, be markedly reduced in formula-fed infants because of the dilution of the glycoprotein concentration by the ingested formula. The high amounts of mucin and lactadherin present in the milk of women who deliver prematurely may contribute, therefore, significantly to neonatal protection from infection. Indeed, milk glycoproteins such as lactadherin protect against agents associated with widespread morbidity and mortality such as rotavirus (14,17), the most common viral agent of infantile gastroenteritis in both developing and industrialized countries (49,50). Likewise, mucin, the most abundant in milk of the three HMFG glycoproteins that we have studied, prevents the adhesion to epithelial cells of S-fimbriated E. coli, a major pathogen causing sepsis and meningitis in newborns (51). The protective effect of these and other nonimmunologic HMFG components of human milk has recently been reviewed (52). The present study indicates that premature infants can benefit from the protective function of human milk and suggests that efforts should be made to provide their mother's milk especially during the early postnatal period.
Abbreviations
- HMFG:
-
human milk fat globule
- RGD:
-
arginine-glycine-aspartic acid
- EGF:
-
epidermal growth factor
- CV:
-
coefficient of variation
REFERENCES
Goldman AS 1993 The immune system of human milk: antimicrobial, antiinflammatory, and immunomodulating properties. Pediatr Infect Dis 12: 664–672
Adderson EE, Johnson JM, Shakelford PG, Carroll WL 1992 Development of the human antibody repertoire. Pediatr Res 32: 257–263
Goldman AS, Chheda S, Keeney SE, Schmalstieg PC, Schanler R 1994 Immunologic protection of the premature newborn by human milk. Semin Perinatol 18: 495–501
Cunningham AS 1987 Breast-feeding and health. J Pediatr 110: 658–659
Jason JM, Nieburg P, Marks JS 1984 Mortality and infectious disease associated with infant feeding practices in developing countries. Pediatrics 74: 702–727
Beaudry M, Dufour R, Marcoux S 1995 Relation between infant feeding and infections during the first six months of life. J Pediatr 126: 191–197
Forsyth JS 1995 The relationship between breast-feeding and infant health and development. Proc Nutr Soc 54: 407–418
Dewey KG, Heinig MJ, Normmsen-Rivers LA 1995 Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 126: 696–702
Lucas A, Cole TJ 1990 Breastmilk and neonatal necrotising enterocolitis. Lancet 336: 1519–1523
Xanthou M, Bines J, Walker WA 1995 Human milk and intestinal host defense in newborns: an update. Adv Pediatr 42: 171–208
Howie PW, Forsyth JS, Ogston SA, Clark A, Florey CD 1990 Protective effect of breast-feeding against infection. BMJ 300: 11–16
Nujens JH, van Berkel PHC, Schanbacher FL 1996 Structure and biological actions of lactoferrin. J Mam Gl Biol Neopl 1: 285–295
Schroten H, Hanisch FG, Plogmann R, Hacker J, Uhlenbruck G, Nobis-Bosch R, Wahn V 1992 Inhibition of adhesion of S-fimbriated Escherichia coli in buccal epithelial cells by human milk fat globule membrane components: a novel aspect of the protective function of mucins in the nonimmunoglobulin fraction. Infect Immun 60: 2893–2899
Yolken RH, Peterson JA, Vonderfecht SL, Fouts ET, Newburg DS 1992 Human milk mucin inhibits rotavirus replication and prevents experimental gastroenteritis. J Clin Invest 90: 1984–1991
Patton S, Gendler SJ, Spicer AP 1995 The epithelial mucin, MUC-1 of milk, mammary gland and other tissues. Biochim Biophys Acta 1241: 407–424
Laegreid A, Kolst-Otnaess AB, Orstavik I, Carlsen KH 1986 Neutralizing activity in human milk fractions against respiratory syncytial virus. Acta Paediatr Scand 75: 696–701
Newburg DS, Peterson JA, Ruiz-Palacios GM, Matson DO, Morrow AL, Shultz J, de Lourdes Guerrero M, Chaturvedi P, Newburg SO, Scallan CD, Taylor MR, Ceriani RL, Pickering LK 1996 Protection of breast-fed children against symptomatic rotavirus infection by human milk lactadherin. Lancet 351: 1160–1164
Wreschner DH, Hareuveni M, Tsarfaty I, Smorodinsky N, Horev J, Zaretsky J, Kotkes P, Weiss M, Lathe R, Dion A, Keydar I 1990 Human epithelial tumor antigen cDNA sequences. Differential splicing may generate multiple protein forms. Eur J Biochem 189: 463–473
Burchell JM, Taylor-Papadimitriou J, Boshell M, Gendler SJ, Duhig T 1989 A short sequence, within the amino acid tandem repeat of a cancer-associated mucin, contains immunodominant epitopes. Int J Cancer 44: 691–696
Ceriani RL, Peterson JA, Lamport DTA 1992 Epitope expression on the breast epithelial mucin. Breast Cancer Res Treat 24: 103–113
Peterson JA, Couto JR, Ceriani RL 1995 Selection of tumor specific epitopes on target antigens for radioimmunotherapy of breast cancer. Cancer Res 55: 281–286
Taylor MR, Couto JR, Scallan C, Ceriani RL, Peterson JA 1997 Lactadherin, a membrane-associated glycoprotein expressed in human milk and breast carcinoma cells, promotes RGD-dependent cell adhesion through integrins. DNA Cell Biol 16: 861–869
Couto JR, Godwin S, Taylor MR, Ceriani RL, Peterson JA 1996 Cloning and sequence analysis of human breast epithelial antigen BA46 reveals an RGD cell adhesion sequence presented on an EGF-like domain. DNA Cell Biol 15: 281–286
Taylor MR, Peterson JA, Ceriani RL, Couto JR 1996 Cloning and sequence analysis of human butyrophilin reveals a potential receptor function. Biochim Biophys Acta 1306: 1–4
Jack LJ, Mather IH 1990 Cloning and analysis of cDNA encoding bovine butyrophilin, an apical glycoprotein expressed in mammary tissue and secreted in association with the milk-fat globule membrane during lactation. J Biol Chem 265: 14481–14486
Larocca D, Peterson JA, Walkup G, Ceriani RL 1992 High level expression in E. coli of an alternate reading frame of pS2 mRNA that encodes a mimotope of human breast epithelial mucin tandem repeat. Hybridoma 11: 191–201
Ceriani RL, Larocca D, Peterson JA, Enloe S, Amiya R, Blank EW 1992 A novel serum assay for breast epithelial antigen using a fusion protein. Anal Biochem 201: 178–184
Greenwood F, Hunter M, Glover J 1963 The preparation of 131I-labeled human growth hormone of high specific radioactivity. Biochem J 89: 114–123
Ceriani RL 1984 Solid phase identification and molecular weight determination of cell membrane antigens with monoclonal antibodies. In: Bechtol KB, McKern TJ, Kennett R (eds) Monoclonal Antibodies and Functional Cell Lines. Progress and Applications. Plenum Press, New York, 398–402.
Peterson JA, Zava DT, Duwe AK, Blank EW, Battifora H, Ceriani RL 1990 Biochemical and histological characterization of antigens preferentially expressed on the surface and cytoplasm of breast carcinoma cells identified by monoclonal antibodies against the human milk fat globule. Hybridoma 9: 221–235
Patton S, Keenan T 1975 The milk fat globule membrane. Biochim Biophys Acta 415: 273–309
Ruegg M, Blanc B 1981 The fat globule size distribution in human milk. Biochim Biophys Acta 666: 7–14
Simonin C, Ruegg M, Sidiropoulos D 1984 Comparison of the fat content and fat globule size distribution of breast milk from mothers delivering term and preterm. Am J Clin Nutr 40: 820–824
Heid HW, Winter S, Bruder G, Keenan TW, Jarasch ED 1983 Butyrophilin, an apical plasma membrane-associated glycoprotein characteristic of lactating mammary glands of diverse species. Biochim Biophys Acta 728: 228–238
Hamosh M, Peterson JA, Henderson TR, Mehta NR, Scallan C, Kiwan R, Taylor MR, Ceriani RL, Hamosh P 1997 The milk fat globule of human milk: relationships between glycoproteins and lipids. FASEB J 11: A238
Bitman J, Wood DL, Hamosh M, Hamosh P, Mehta NR 1983 Comparison of the lipid composition of breast milk from mothers of term and preterm infants. Am J Clin Nutr 38: 300–312
Schanler RJ, Goldblum RM, Garza TC, Goldman AS 1986 Enhanced fecal excretion of selected immune factors in very low birth weight infants fed fortified human milk. Pediatr Res 76: 711–715
Davidson LA, Lonnerdal B 1987 Persistence of human milk proteins in the breast-fed infant. Acta Paediatr Scand 20: 733–740
Goldman AS, Garza C, Schanler RJ, Goldblum RM 1990 Molecular forms of lactoferrin in stool and urine from infants fed human milk. Pediatr Res 27: 252–255
Hamosh M 1995 Enzymes in human milk. In: Jensen R (ed). Handbook of Human Composition. Academic Press, San Diego, CA, 388–428.
Armand M, Hamosh M, Mehta NR, Angelus PA, Philpott JR, Henderson TR, Dwyer NK, Lairon D, Hamosh P 1996 Effect of human milk or formula on gastric function and fat digestion in the premature infant. Pediatr Res 27: 429–437
Armand M, Hamosh M, Di Palma JS, Gallagher J, Benjamin SB, Philpott JR, Lairon D, Hamosh P 1995 Dietary fat modulates gastric lipase activity in healthy adults. Am J Clin Nutr 62: 74–80
Goldblum RM, Schanler RJ, Garza C, Goldman AS 1989 Human milk feeding enhances the urinary excretion of immunologic factors in low birth weight infants. Pediatr Res 25: 184–188
Prentice A 1987 Breast-feeding increases concentrations of IgA in infant's urine. Arch Dis Child 62: 792–795
Patton S 1994 Detection of large fragments of the human milk mucin MUC-1 in feces of breast-fed infants. J Pediatr Gastroenterol Nutr 18: 225–230
Schroten H, Lethen A, Hanish FG 1992 Inhibition of adhesion of S-fimbriated Escherichia coli to epithelial cells by meconium and feces of breast-fed and formula-fed newborns: mucins are the major inhibitory component. J Pediatr Gastroenterol Nutr 82: 150–158
Schroten H, Plogmann R, Hanisch FG, Hacker J, Nobis-Bosch R, Wahn V 1993 Inhibition of adhesion of S-fimbriated E. coli to buccal epithelial cells by human skim milk is predominantly mediated by mucins and depends on the period of lactation. Acta Paediatr 82: 6–11
Chen CC, Baylor M, Bass DM 1993 Murine intestinal mucins inhibit rotavirus infection. Gastroenterology 105: 84–92
Rodriguez WJ, Kim HW, Brandt CD, Schwartz RH, Gardner MK, Jeffries B, Parrott RH, Kaslow RA, Smith JI, Kapikian AZ 1987 Longitudinal study of rotavirus infection and gastroenteritis inn families served by a pediatric medical practice: clinical and epidemiologic observations. Pediatr Infect Dis J 6: 170–176
Blacklow MD, Greenberg HB 1991 Viral gastroenteritis. N Engl J Med 325: 252–264
Karhonen TK, Valtonen MV, Parkkinen J, Vaisanen V, Rhen J, Finne J, Osrkov F, Orskov I, Swenson SB, Makela PH 1985 Serotypes, hemolysin production and receptor recognition of Escherichia coli strains associated with neonatal sepsis and meningitis. Infect Immun 48: 486–491
Peterson JA, Patton S, Hamosh M 1998 Glycoproteins of the human milk fat globule in the protection of the breast-fed infant against infection. Biol Neonate 74: 143–162
Author information
Authors and Affiliations
Additional information
Supported in part by National Institutes of Health Grants CA61258, CA39932, and HD34286.
Rights and permissions
About this article
Cite this article
Peterson, J., Hamosh, M., Scallan, C. et al. Milk Fat Globule Glycoproteins in Human Milk and in Gastric Aspirates of Mother's Milk-Fed Preterm Infants. Pediatr Res 44, 499–506 (1998). https://doi.org/10.1203/00006450-199810000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199810000-00006
This article is cited by
-
Goat and buffalo milk fat globule membranes exhibit better effects at inducing apoptosis and reduction the viability of HT-29 cells
Scientific Reports (2019)
-
Palaeoproteomic identification of breast milk protein residues from the archaeological skeletal remains of a neonatal dog
Scientific Reports (2019)
-
Differential proteomic analysis of milk fat globule membrane proteins in human and bovine colostrum by iTRAQ-coupled LC-MS/MS
European Food Research and Technology (2017)
-
Mothers' Milk Feedings in the Neonatal Intensive Care Unit: Accuracy of the Creamatocrit Technique
Journal of Perinatology (2002)
-
The B7–CD28 superfamily
Nature Reviews Immunology (2002)