Abstract
We previously have demonstrated that hypocapnia aggravates and hypercapnia protects the immature rat from hypoxicischemic brain damage. To ascertain cerebral blood flow (CBF) and metabolic correlates, 7-d postnatal rats were subjected to hypoxia-ischemia during which they were rendered either hypo-(3.5 kPa), normo- (5.1 kPa), or hypercapnic (7.3 kPa) by the inhalation of either 0, 3, or 6% CO2, 8% O2, balance N2. CBF during hypoxia-ischemia was better preserved in the normo- and hypercapnic rat pups; these animals also exhibited a stimulation of cerebral glucose utilization. Brain glucose concentrations were higher and lactate lower in the normo- and hypercapnic animals, indicating that glucose was consumed oxidatively in these groups rather than by anaerobic glycolysis, as apparently occurred in the hypocapnic animals. ATP and phosphocreatine were better preserved in the normo- and hypercapnic rats compared with the hypocapnic animals. Cerebrospinal fluid glutamate, as a reflection of the brain extracellular fluid concentration, was lowest in the hypercapnic rats at 2 h of hypoxia-ischemia. The data indicate that during hypoxia-ischemia in the immature rat, CBF is better preserved during normo- and hypercapnia; the greater oxygen delivery promotes cerebral glucose utilization and oxidative metabolism for optimal maintenance of tissue high energy phosphate reserves. An inhibition of glutamate secretion into the synaptic cleft and its attenuation of N-methyl-D-aspartate receptor activation would further protect the hypercapnic animal from hypoxic-ischemic brain damage.
Similar content being viewed by others
Main
In a previous investigation, we showed that hypocapnia aggravates and hypercapnia protects the immature rat from hypoxic-ischemic brain damage(1). The rationale for the conduct of the study related to clinical investigations which suggested that premature infants who required mechanical ventilation to prevent or minimize hypoxemia arising from respiratory distress syndrome are at increased risk for the development of periventricular leukomalacia if hypocapnia occurs during the course of respiratory management(2–4). CO2 potentially has multiple effects on CBF and metabolism with or without superimposed hypoxia-ischemia. Accordingly, we conducted experiments to ascertain the effect of varying concentrations of CO2 on CBF and metabolism of immature rats subjected to hypoxia-ischemia.
METHODS
Dated, pregnant Sprague-Dawley rats were purchased from a commercial breeder (Charles River Laboratories, Wilmington, MA) and housed in individual cages. Offspring, delivered vaginally, were reduced to 10/litter at birth, and were reared with their dams until time of experimentation at 7 d of postnatal age.
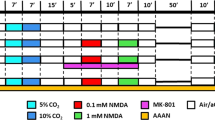
Induction of cerebral hypoxia-ischemia. To produce brain damage caused by cerebral hypoxia-ischemia, 7-d postnatal rats were anesthetized with halothane (4% induction; 1.0-1.5% maintenance), 30% O2, balance nitrous oxide. Under anesthesia, the rat pups underwent permanent ligation of the right common carotid artery as previously described(5). To induce systemic hypoxia, the rats were individually positioned head-first within the barrel of a 20-mL syringe, as previously described(6). The barrels themselves were aligned in parallel, adjacent to each other, and attached to a plexiglass platform. The smaller aperature of each barrel was attached to polyethylene tubing, which, in turn, was attached to a gas tank containing either room air or a gas mixture containing O2, CO2, and N2. Each rat pup was snuggly positioned within the barrel via the larger aperature for 15 min, after which they were exposed to either room air (controls) or the hypoxic gas mixture. The larger aperature of the barrel also served as the outlet for the gas. The internal temperature of each barrel was intermittently monitored with a microthermistor probe connected to a servo-controlled heating lamp positioned 2 feet directly above the barrel apparatus to maintain an environmental temperature of 37 °C. The rat pups were exposed to the gas mixture for varying durations up to 2 h, an interval known to produce brain damage in the form of either selective neuronal necrosis or infarction of the cerebral hemisphere ipsilateral to the carotid artery occlusion(7). Control animals consisted of nonligated littermates exposed to room air for the same duration as the hypoxic-ischemic animals.
The O2-CO2-N2 gas mixtures to which the immature rats were exposed were calibrated commercially to ensure a precise inhalant concentration of O2. One group of carotid artery-ligated immature rat pups was exposed to a gas mixture containing 3.07% CO2, 7.83% O2, balance N2, while littermate controls simultaneously were exposed in separate jars to 7.94% O2, balance N2. A second group of rat pups was exposed to 6.19% CO2, 8.15% O2, balance N2, while littermate controls simultaneously were exposed to 7.94% O2, balance N2. Accordingly, experimental and control littermates were exposed to O2 concentrations varying by no more than 0.11%.
Measurement of CBF. CBF was measured in carotid arteryligated rat pups during the course of hypoxia-ischemia, using a modification of the indicator fractionation technique, as previously described(8). Specifically, at 90 min of hypoxia-ischemia, rat pups exposed to either 0, 3, or 6% carbon dioxide were injected s.c. with 5 μCi of iodo-[14C]antipyrine (DuPont NEN, Boston, MA). The injection was made into the back of the rat, roughly in the midline. Precisely 1 min after the injection, each animal was decapitated, and arterialized blood was collected from the severed neck vessels into a heparinized glass capillary tube. Ten microliters of blood pipetted from the capillary tube were added to a scintillation vial containing 1 mL of Soluene-350 (United Technologies Packard, Downers Grove, IL). After shaking overnight in a mechanical shaker, the solution was combined with 9 mL of Dimilume-30 (United Technologies Packard). Samples then were counted on a Beckman LS-350 liquid scintillation counter (Beckman Instruments, Fullerton, CA). The brain of each rat pup was removed from its skull, and a small specimen (approximately 50 mg) of the right cerebral hemisphere in the distribution of the middle cerebral artery was removed and placed in a preweighed scintillation vial. After reweighing of the vial to ascertain the weight of the brain tissue specimen, 1 mL of Soluene-350 was added to the vial. After mixing overnight, the solution was combined with 9 mL of Dimilume-30 and isotopically counted.
CBF was calculated from the concentration of the iodo-[14C]antipyrine tracer in the blood and brain tissue specimen at 1 min, assuming linearity in the input function from 0 to 1(8). The brain:blood partition coefficient (λ) was assumed to equal 0.94(9).
Measurement of CGU. CGU was measured in hypoxic-ischemic rat pups exposed to 0, 3, or 6% CO2. A modification of the Sokoloff technique(10) was used to measure CGU, using 2-DG as the radioactive tracer(11, 12). Specifically, rat pups undergoing hypoxia-ischemia were injected s.c. with 2.5 μCi of 2-DG(Amersham Corp., Arlington Heights, IL), after which the animals were decapitated at either 2, 5, 10, 20, 30, 45, or 60 min. Arterialized blood was collected from the severed neck vessels into heparinized capillary tubes which were centrifuged at 3000 × g for 5 min to separate the plasma from red cells. A portion (10 μL) of plasma was used to determine glucose concentration on a micro-glucose analyzer (Beckman Glucostat; Beckman Instruments, Palo Alto, CA), and 10 μL of the remaining portion were solubilized in 1.0 mL of Soluene-350. After mixing overnight in a mechanical shaker, the solution was combined with 9.0 mL of Dimilume-36. Samples were then counted in a Beckman LS-350 liquid scintillation spectrometer. Measurements of the glucose (μmol/mL) and 2-DG (dpm/mL) contents of each plasma sample allowed for calculation of the integrated 2-DG/glucose specific activity (dpm/μmol) over 60 min.
The heads of the rat pups killed at 60 min postinjection of 2-DG were immediately (<1 s) frozen in liquid nitrogen to stop intermediary metabolism. Each brain was then removed from its skull in a cold box set at-20 °C, and a portion (50 mg) of the right cerebral hemisphere in the distribution of the middle cerebral artery was dissected, powdered under liquid nitrogen, and weighed on a micro-analytical balance. Perchloric acid extracts of each specimen then were prepared as previously described(13). The solutions were neutralized to pH 7.0 with 2 M KHCO3, a portion (0.5 mL) of which was diluted in 9.5 mL of Dimilume-36 and isotopically counted. The remainder of the neutralized extract was passed over an ion-exchange column, formate form (Bio-Rad Econocolumn, Richmond, CA). Neutral compounds, including free (nonphosphorylated) 2-DG and glucose, were eluted with 3 mL of water, a portion of which (0.5 mL) was diluted in 9.5 mL of Dimilume-36 and counted. The amount of 2-DG metabolized to 2-DG-6-phosphate was determined by substracting the 2-DG counts from the total counts obtained before ion-exchange. From the data, the percentage of total 2-DG in brain that was metabolized to 2-DG-6-phosphate was calculated. The lumped constant of each rat pup killed at 60 min postinjection of 2-DG was calculated using a nomogram for adult rat brain published by Pardridge et al.(14), which allows calculation of individual lumped constant values determined by the concentration of glucose in brain relative to that in plasma. CGU was calculated as previously described(11) by substituting the measured values of the percentage 2-DG metabolized for the rate constants K1*, K2*, and K3* (2-DG) and K1,K2, and K3 (glucose).
Measurement of brain metabolite concentrations. Rat pups exposed to varying concentrations of CO2 were quick frozen in liquid nitrogen at either 1 or 2 h of hypoxia-ischemia. The brain of each rat pup then was removed from its skull in a cold box set at -20 °C, and a portion(50 mg) of the right cerebral hemisphere in the distribution of the middle cerebral artery was dissected, powdered under liquid nitrogen, and weighed on a micro-analytical balance. Neutralized perchloric acid extracts of the cerebral hemisphere then were prepared as previously described(13). Concentrations of glucose, pyruvate, lactate,α-ketoglutarate, glutamate, PCr, creatine, ATP, ADP, and AMP were measured fluorometrically with pyridine nucleotides and appropriate enzymes(13, 15).
The pHi was determined using brain tissue concentrations of PCr, creatine, ATP, and ADP according to the equation: where K'ck represents the creatine kinase equilibrium, as previously described(16).
Measurement of CSF glutamate. Rat pups exposed to hypoxia-ischemia with varying concentrations of CO2 were removed from the syringe barrel at 1 or 2 h, immediately after which a sample of CSF (10μL) was obtained from the cisterna magna, as previously described(17). An exact aliquot (5 μL) was diluted 1:10 in 0.5 M perchloric acid and frozen until time of analysis of the concentration of glutamate, determined fluorometrically(15).
Statistical analysis. Statistical analysis of the data included the t test and analysis of variance with a Bonferroni correction for multiple comparison of means, where appropriate.
Institutional approval. The experiments described here were reviewed by the Animal Care and Use Committee of The Milton S. Hershey Medical Center, The Pennsylvania State University, and approved on October 1, 1992.
RESULTS
Data pertaining to CBF during hypoxia-ischemia are shown in Figure 1. Control CBF averaged 67 mL/100 g/min, a value similar to that previously reported for 7-d postnatal rats(18). CBF, measured at 90 min of hypoxia-ischemia, was lowest in those animals not concurrently exposed to CO2, with significantly higher values in those rat pups exposed to 3 and 6% CO2(p < 0.05). CBF values were similar in the 3 and 6% CO2-exposed animals.
CBF during hypoxia-ischemia in immature rats exposed to varying concentrations of carbon dioxide. CBF measurements were obtained from the cerebral hemisphere ipsilateral to the common carotid artery occlusion at 90 min of hypoxia-ischemia. Values represent means ± SEM for six to eight animals in each group.
CGU was measured from 40 to 100 min of hypoxia-ischemia and was the average rate of utilization during this interval in all experimental groups(Table 1). The control value of 15.4 μmol/100 g/min was nearly double that previously reported for 7-d postnatal rats(11, 12). The higher value in the present study probably relates to the stress produced by prolonged positioning in the syringe barrel. Interestingly, CGU was not significantly increased in those rat pups not exposed to CO2 during hypoxia-ischemia. Animals exposed to 3 and 6% CO2 exhibited rates of CGU 166 and 155% of the control value, respectively.
Concentrations of cerebral glycolytic and tricarboxylic acid cycle intermediates during hypoxia-ischemia are shown in Table 2. Brain glucose was lowest in those animals not exposed to CO2 at both 1 and 2 h of hypoxia-ischemia, with intermediate values in the 3% CO2-exposed group, and values similar to control in the 6% CO2-exposed group. In contrast, pyruvate and lactate were highest, at least at 1 h, in those animals not exposed to CO2. Indeed, there was essentially no change in these two glycolytic metabolites in the 6% CO2-exposed group at 1 h of hypoxia-ischemia, with only a slight increase in lactate at 2 h. α-Ketoglutarate was substantially reduced only in those animals not exposed to CO2 at 2 h of hypoxia-ischemia. Changes in glutamate were relatively minor in all groups.
Alterations in cerebral high energy phosphate reserves during hypoxia-ischemia are shown in Table 3. Major reductions in PCr and ATP were seen especially at 2 h of hypoxia-ischemia in those rat pups not exposed to CO2. Intermediate values were seen in the group exposed to 3% CO2, whereas ATP was well preserved in the group exposed to 6% CO2, with only a slight reduction in PCr at 2 h of hypoxia-ischemia. Elevations-or lack thereof-in ADP and AMP reflected concurrent reductions in ATP.
Calculated pHi in control immature rats averaged 7.18(Fig. 2). Intracellular pH decreased to comparable levels in the three experimental groups at 1 h of hypoxia-ischemia. At 2 h of hypoxia-ischemia, pHi was lowest in those rat pups not exposed to CO2, compared with the 3 and 6% CO2-exposed groups (p< 0.05). Intracellular pH values were comparable in the 3 and 6% CO2-exposed animals at 2 h of hypoxia-ischemia.
Calculated pHi during hypoxia-ischemia in immature rats exposed to varying concentrations of carbon dioxide. Intracellular pH was calculated from the changes which occur in PCr, creatine, ATP, and ADP, as described in “Methods,” Data for PCr, ATP, and ADP derived from Table 3; data for creatine not shown. Values represent means ± SEM for five to six animals in each group.
CSF concentrations of glutamate, as a reflection of brain extracellular concentrations (see “Discussion”), were not significantly increased above control in any of the experimental groups at 1 h of hypoxia-ischemia (Fig. 3). In addition, there were no significant differences in glutamate concentrations among the three experimental groups. At 2 h of hypoxia-ischemia, CSF glutamate was increased by approximately 60% in those rat pups exposed to no CO2 or 3% CO2 (p < 0.05). Both elevations were significantly higher than the minimal increase seen in the 6% CO2-exposed group at the same interval (p < 0.05).
DISCUSSION
The results of the present study must be interpreted in the context of data derived from a prior investigation conducted in our laboratory(1). In the prior study, it was determined that immature rats subjected to hypoxia-ischemia without concurrent CO2 exposure exhibit Pco2 approximating 3.5 kPa (26 mm Hg), whereas rat pups exposed to 3 and 6% CO2 during hypoxia-ischemia exhibit Pco2 values of 5.1 kPa (38 mm Hg) and 7.3 kPa (55 mm Hg), respectively. Neuropathologic analysis at 30 d of postnatal age in rats previously exposed to hypoxia-ischemia with varying concentrations of CO2 at 7 d of postnatal age revealed that the hypocapnic animals show the worst brain damage, whereas the hypercapnic animals show the least brain injury. From the data, we concluded that hypocapnia aggrevates and mild hypercapnia protects the perinatal brain from hypoxic-ischemic damage.
In the present investigation, CBF was better preserved during hypoxia-ischemia in the normo- and hypercapnic immature rats compared with the hypocapnic animals. The improved cerebrovascular perfusion and cerebral oxygen delivery presumably resulted from less severe cardiovascular depression and associated systemic hypotension in these groups(1). An additional factor which would improve CBF during either normo- or hypercapnia might be a greater dilation of the cerebrovascular bed than expected during hypoxia-ischemia in associated with hypocapnia. In this regard, Ruta et al.(19) recently showed in adult rats that middle cerebral artery occlusion combined with hypocapnia is associated with a greater reduction in blood flow to a wider area of the ipsilateral cerebral hemisphere than occurs with middle cerebral artery occlusion alone, suggesting that hypocapnia increases the size of the ischemic brain region at risk for infarction.
The cerebral metabolic data presented here clearly show an enhanced cerebral glucose utilization in the normo- and hypercapnic immature rats compared with the hypocapnic animals. Indeed, cerebral glucose utilization in the hypocapnic rat pups was not significantly higher than control, despite hypoxia-ischemia, owing probably to its inhibition by intracellular acidosis during the interval when glucose utilization was measured (40-100 min) (see Fig. 2). Tissue acidosis is known to inhibit glycolytic flux at the phosphofructokinase reaction(20). In this regard, tissue lactate concentrations during hypoxia-ischemia in the hypocapnic rats were up to 3-fold higher than values observed in the normo- and hypercapnic animals at the same interval (see Table 2). The lack of any substantial lactacidosis in the normo- and hypercapnic animals combined with higher tissue concentrations of glucose andα-ketoglutarate at 2 h of hypoxia-ischemia (see Fig. 2 and Table 2) as well as the enhanced cerebral glucose utilization (see above) indicate that glucose was consumed oxidatively in these groups rather than by anaerobic glycolysis, as apparently occurred in the hypocapnic animals. The oxidative consumption of glucose during hypoxia-ischemia would provide more reducing equivalents to mitochondria for the production of the high energy phosphate reserves, ATP and phosphocreatine, which were, in fact, better preserved in the normo- and hypercapnic animals(see Table 3).
The CBF and metabolic changes described above readily explain why immature rats exposed to either normocapnia or hypercapnia during hypoxia-ischemia ultimately exhibit less brain damage than hypocapnic animals. However, the results appear insufficient to explain the greater neuropathologic protection of hypercapnia compared with normocapnia. Some differences in the cerebral metabolic alterations between the normo- and hypercapnic rats did exist, notably the marked attenuation in tissue lactacidosis and the better preservation of tissue glucose in the hypercapnic animals. Furthermore, CSF glutamate in the hypercapnic rats at 2 h of hypoxia-ischemia was 32% lower than values obtained from either the normo- or hypocapnic animals at the same interval. If it is assumed that CSF (cisterna magna) glutamate reflects the concentration of the metabolite in the extracellular compartment of the brain at some prior interval (e.g. 30-60 min)(21), then the lower level at 2 h of hypoxia-ischemia in the hypercapnic animals suggests a relative inhibition in the secretion of the excitatory amino acid into the synaptic cleft. In vitro studies have suggested that acidosis of the brain extracellular compartment blunts the neurotoxicity of excitatory amino acid neurotransmitters, especially glutamate, via an inhibition in the NMDA cell surface receptor(22–24). A down-regulation of NMDA-gated ion channel currents with a secondary reduction in intracellular calcium accumulation during hypoxia-ischemia might also occur [for review, see Tombaugh and Sapolsky(25)].
In conclusion, the present investigation provides insight into the basic mechanisms by which hypocapnia aggravates, and hypercapnia protects, the perinatal brain from hypoxic-ischemic damage. CBF is better preserved during normo- and hypercapnia; the greater oxygen delivery promotes cerebral glucose utilization and oxidative metabolism for optimal production and maintenance of tissue high energy phosphate reserves. An inhibition of glutamate secretion into the synaptic cleft with its attentuation of NMDA receptor activation would further protect the hypercapnic animal from hypoxic-ischemic brain damage.

Abbreviations
- PCr:
-
phosphocreatine
- NMDA:
-
N- methyl-D-aspartate
- CBF:
-
cerebral blood flow
- CSF:
-
cerebrospinal fluid
- CGU:
-
cerebral glucose utilization
- pHi:
-
intracellular pH
- 2-DG:
-
2-deoxy-[14C]glucose
References
Vannucci RC, Towfighi J, Heitjan DF, Brucklacher RM 1995 Carbon dioxide protects the perinatal brain from hypoxic-ischemic damage: an experimental study in the immature rat. Pediatrics 95: 868–874.
Greisen G, Munck H, Lou H 1987 Severe hypocarbia in preterm infants and neurodevelopmental deficit. Acta Pediatr Scand 86: 401–404.
Graziani L, Spitzer AR, Mitchell DG, Merton DA, Stanley C, Robinson N, McKee L 1992 Mechanical ventilation in preterm infants: neurosonographic and developmental studies. Pediatrics 90: 515–522.
Ikonen RS, Janas MO, Koidikko MJ, Laippala P, Kuusinen EJ 1992 Hyperbilirubinemia, hypocarbia and periventricular leukomalacia in preterm infants. Relationship to cerebral palsy. Acta Pediatr 81: 802–807.
Rice JE, Vannucci RC, Brierley JB 1981 The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9: 131–141.
Vannucci RC, Brucklacher RM, Vannucci SJ 1996 The effect of hyperglycemia on cerebral metabolism during hypoxia-ischemia in the immature rat. J Cereb Blood Flow Metab (in press)
Towfighi J, Yager JY, Housman C, Vannucci RC 1991 Neuropathology of remote hypoxic-ischemic damage in the immature rat. Acta Neuropathol 81: 578–587.
Ringel M, Bryan RM, Vannucci RC 1991 Regional cerebral blood flow during hypoxia-ischemia in the immature rat: Comparison of iodoantipyrine and iodoamphetamine as radioactive tracers. Dev Brain Res 59: 231–235.
Lyons DT, Vasta F, Vannucci RC 1987 Autoradiographic determination of regional cerebral blood flow in the immature rat. Pediatr Res 21: 471–476.
Sokoloff L, Reivich M, Kennedy C, Des Rosiers MH, Patlak CS, Pettigrew KD, Sakurada O, Shinohara M 1977 The [14C] deoxyglucose method for the measurement of local cerebral glucose utilization: theory, procedure and normal values in the conscious and anesthetized albino rat. J Neurochem 28: 897–916.
Vannucci RC, Christensen MA, Stein DT 1989 Regional cerebral glucose utilization in the immature rat: effect on hypoxia-ischemia. Pediatr Res 26: 208–214.
Vannucci RC, Yager JY, Vannucci SJ 1994 Cerebral glucose and energy utilization during the evolution of hypoxic-ischemic brain damage in the immature rat. J Cereb Blood Flow Metab 14: 279–288.
Vannucci RC, Duffy TE 1974 The influence of birth on carbohydrate and energy metabolism in rat brain. Am J Physiol 226: 933–940.
Pardridge WM, Crane PD, Mietus LJ, Oldendorf WH 1982 Nomogram for 2-deoxy-glucose lumped constant for rat brain cortex. J Cereb Blood Flow Metab 2: 197–202.
Lowry OH, Passonneau JV 1972 A Flexible System of Enzymatic Analysis. Academic Press, New York
Yager JY, Brucklacher RM, Vannucci RC 1991 Cerebral oxidative metabolism and redox state during hypoxia-ischemia and early recovery in immature rats. Am J Physiol 261:H1102–H1108.
Vannucci RC, Duffy TE 1975 Cerebral oxidative and energy metabolism of fetal and neonatal rats during anoxia and during recovery. Am J Physiol 230: 1269–1275.
Mujsce DJ, Christensen MA, Vannucci RC 1990 Cerebral blood flow and edema in perinatal hypoxic-ischemic brain damage. Pediatr Res 27: 450–453.
Ruta TS, Drummond JC, Cole DJ 1993 The effect of acute hypocapnia on local cerebral blood flow during middle cerebral artery occlusion in isoflurane anesthetized rats. Anesthesiology 78: 134–140.
Lowry OH, Passonneau JV, Hasselberger FX, Schulz DW 1964 Effect of ischemia on known substrates and cofactors of the glycolytic pathway in brain. J Biol Chem 239: 18–30.
Bito LZ, Davson H 1966 Local variations in cerebrospinal fluid composition and its relationship to the composition of the extracellular fluid of the cortex. Exp Neurol 14: 264–280.
Tombaugh GC, Sapolsky RM 1990 Mild acidosis protects hippocampal neurons from injury induced by oxygen and glucose deprivation. Brain Res 506: 343–345.
Takadera T, Shimada Y, Mohri T 1992 Extracellular pH modulates N-methyl-D-aspartate receptor mediated neurotoxicity and calcium accumulation in rat cortical cultures. Brain Res 572: 126–131.
Kaku DA, Giffard RG, Choi DW 1993 Neuroprotective effects of glutamate antagonists and extracellular acidity. Science 260: 1516–1518.
Tombaugh GC, Sapolsky RM 1993 Evolving concepts about the role of acidosis in ischemic neuropathology. J Neurochem 61: 793–803.
Author information
Authors and Affiliations
Additional information
Supported by Program Project HD-30704 (R.C.V.) and by Grant HD-31521(S.J.V.) from The National Institute of Child Health and Human Development.
Rights and permissions
About this article
Cite this article
Vannucci, R., Brucklacher, R. & Vannucci, S. Effect of Carbon Dioxide on Cerebral Metabolism during Hypoxia-Ischemia in the Immature Rat. Pediatr Res 42, 24–29 (1997). https://doi.org/10.1203/00006450-199707000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00005
This article is cited by
-
Effects of permissive hypercapnia on intraoperative cerebral oxygenation and early postoperative cognitive function in older patients with non-acute fragile brain function undergoing laparoscopic colorectal surgery: protocol study
BMC Geriatrics (2023)
-
Optimal Targets of the First 24-h Partial Pressure of Carbon Dioxide in Patients with Cerebral Injury: Data from the MIMIC-III and IV Database
Neurocritical Care (2022)
-
Neuroprotective Role of Acidosis in Ischemia: Review of the Preclinical Evidence
Molecular Neurobiology (2021)
-
Therapeutic hypercapnia reduces blood–brain barrier damage possibly via protein kinase Cε in rats with lateral fluid percussion injury
Journal of Neuroinflammation (2019)
-
Relationship between PCO2 and unfavorable outcome in infants with moderate-to-severe hypoxic ischemic encephalopathy
Pediatric Research (2016)