The practices of a healthcare professional ending the life of a patient on request (euthanasia), and of a healthcare professional supplying a patient with the means to end their life (assisted suicide), have been proposed since the late 19th century as means to alleviate the suffering of people with life-limiting illnesses. However, it was not until the end of the 20th century that euthanasia and assisted suicide (EAS) became established in The Netherlands, and assisted suicide (but not euthanasia) became established in Switzerland and in the state of Oregon in the USA. In the 21st century other jurisdictions, including Canada, Columbia, New Zealand and the states of Victoria and Western Victoria in Australia, have adopted similar proposals variously termed ‘medical assistance in dying’, ‘medical aid in dying’, ‘physician aid in dying’, ‘voluntary assisted dying’, ‘physician-assisted dying’ or, more generally, ‘assisted dying’. In recent years, it has been argued that the term ‘assisted suicide’ is misleading because ‘the practice of physician aid in dying is distinct from the behaviour that has been traditionally and ordinarily described as “suicide”’.Reference Creighton, Cerel and Battin1 Clearly it is possible to make a distinction between these practices. For example, it is possible to give separate estimates for rates of death under the provisions of ‘physician aid in dying’ legislation and rates of death by suicide in the general population. The question is whether the conceptual or empirical differences between these practices are such as to make the language of ‘assisted suicide’ inapplicable or inappropriate. This is highly contested.Reference Kious and Battin2–Reference Jones5
Different terminal conditions are associated with EAS: one study based in The Netherlands reported that the most common diagnosis across the regions was cancer.Reference Koopman and Putter6 Data from Belgium shows that rates of EAS for dementia have increased over time.Reference Dierickx, Deliens, Cohen and Chambaere7 In some jurisdictions, EAS for primary psychiatric indications is permitted. These include The Netherlands, Belgium and Switzerland; Canada has recently passed legislation to permit EAS where there is no terminal illness, from 2023.Reference Evenblij, Pasman, Pronk and Onwuteaka-Philipsen8 The criteria can be challenging to establish where the primary condition the person is seeking relief from is a mental illness, and research has recently attempted to identify how the criteria of ‘irremediable suffering’ is met.Reference van Veen, Evans, Ruissen, Vandenberghe, Beekman and Widdershoven9
A recent systematic review of the characteristics of EAS for psychiatric indications suggested that the characteristics of people who die by EAS for mental health reasons are very similar to the characteristics of people who die by ‘traditional’ suicide, with high numbers having psychiatric disorders and a history of self-harm.Reference Calati, Olié, Dassa, Gramaglia, Guillaume and Madeddu10 This review indicated that the demographics of the two groups have key differences, with EAS being more common in women, and traditional suicide more common in men. Suicidal ideation and behaviours may be associated with a range of mental illnesses and conditions, including psychosis, depression, personality disorders and even adjustment disorders.Reference Too, Spittal, Bugeja, Reifels, Butterworth and Pirkis11,Reference Casey, Jabbar, O'Leary and Doherty12 Depression and suicidal thoughts are not uncommon in end-of-life care, and there are guidelines for the management of depression in palliative care that build on the evidence base for treatment in this area.Reference Rayner, Price, Evans, Valsraj, Higginson and Hotopf13 At the very least, there are similarities between suicide in the general population and cases of EAS for mental health reasons or for cases of physical health with concomitant mental illness.
Terminology and rationale
This paper uses EAS as an umbrella term to refer to euthanasia and/or assisted suicide. The paper uses the term ‘non-assisted suicide’ for suicide that occurs in the general population without assistance of a medical kind, i.e. suicide that is not EAS. This paper uses ‘self-initiated death’ to cover death by EAS and/or by non-assisted suicide.
Although EAS has been legalised in several countries in the past 20 years, it remains subject to intense debate. One area of contention is the relationship between EAS and rates of suicide (either including or not including assisted suicide). Some proponents have claimed EAS will help reduce suicide, paradoxically, as people will feel comforted by the knowledge that there is an option for them to leave their suffering, should it become unbearable.Reference Posner14,Reference Nicolini, Kim, Churchill and Gastmans15 They suggest that introducing EAS will reduce the number of self-initiated deaths or, even if self-initiated deaths increase, non-assisted suicides will be reduced, as people will be more likely to choose a death in a medically supported setting than a potentially violent death by suicide. Prompted by this, England's Health Secretary requested data on suicide rates among terminally ill people in April 2021, to provide evidence for the debate on the legalisation of EAS in England and Wales.Reference Iacobucci16 Conversely, opponents of EAS have made the claim that making EAS available will not only increase the rate of self-initiated deaths, it will likely increase, or at least not decrease, rates of non-assisted suicide. The argument is that by making EAS legally available, society is making it acceptable to intentionally end one's own life, a message which is at variance with, and may undermine the consistent messaging of, suicide prevention groups and campaigns.Reference Berghmans, Widdershoven and Widdershoven-Heerding17
Aims
In this review we examine the relationship between the introduction of EAS and rates of non-assisted suicide and self-initiated death. In particular, the review seeks to assess whether there is evidence of an association, either positive or negative, between the introduction of EAS and rates of non-assisted suicide, or between the introduction of EAS and rates of self-initiated death.
Method
This study is a systematic review of the association between EAS and suicide. It was based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines for systemic review and meta-analysis. We did not require ethical approval as the study involved secondary analysis of anonymised data. A protocol was pre-registered with PROSPERO (identifier CRD42021277581).
To allow for a robust systematic review of the relationship between EAS and self-initiated death and/or non-assisted suicide, we conducted a search of the following databases: PubMed, Scopus, PsycINFO and Science Direct. We included all articles from the beginning of records until 2021. We restricted the search to those studies published in the English language and in peer-reviewed journals. We included original research papers only, and did not include case reports or series, or systematic or narrative reviews.
We used the following search terms: (euthanasia[title] OR assisted[title] OR ‘assistance in’[title] OR ‘aid in’[title]) AND (suicid*[title]). The searches were conducted on 21 December 2021. We based our search terms on the review conducted by Calati et al.Reference Calati, Olié, Dassa, Gramaglia, Guillaume and Madeddu10 A hand search was conducted of the reference list of all studies selected for full review.
We included studies that focused on EAS and reported data on population-based suicide rates. Where the title suggested a paper suitable for inclusion we examined the abstract, and following this, where both title and abstract suggested an article eligible for inclusion, the full article was examined for suitability for inclusion based on the inclusion criteria. The citations of all included studies were hand-searched for any additional studies meeting the inclusion criteria. Any discrepancies between the two reviewers (C.J.A. and A.M.D.) were resolved by consultation with the third author (D.A.J.). Abstracts that did not refer to both EAS and rates of non-assisted suicide were excluded. Three reviewers (C.J.A., A.M.D. and D.A.J.) examined the full texts and graded them independently.
Quality assessment
A quality assessment was performed. We used two established assessments for assessing the quality of papers for inclusion: the Oxford quality assessment and the Newcastle–Ottawa Scale (NOS).
The NOS was used to assess the quality of non-randomised controlled studies.Reference Wells, Shea, O'Connell, Peterson, Welch and Losos18 The NOS is a reliable tool for appraising the methodological quality of research.Reference Del Carpio, Paul, Paterson and Rasmussen19,Reference Cook and Reed20 The NOS contains eight items, which are categorised into three dimensions: the selection, comparability and the outcomes of studies. The NOS ranges from zero to nine stars, as follows: selection of the study group (up to four stars/points), comparability of cohorts (up to two stars/points) and ascertainment of outcome (up to three stars/points). High-quality studies achieve more than seven stars, medium-quality studies between four and six stars and poor-quality studies achieve fewer than four stars.
Results
The combined search strategies yielded a total of 11 273 titles to be screened, and 6808 remained after the removal of duplicates (Fig. 1). Following review of titles, 199 remained. In most cases where titles were excluded, this was on the basis that the term ‘suicide’ occurred in the title only in the pairing ‘assisted suicide’ and there was no indication of relevance to non-assisted suicide. After examination of title and abstracts, 18 remained, and these studies were reviewed in full. No further studies were added following a hand search of the references of the included studies.
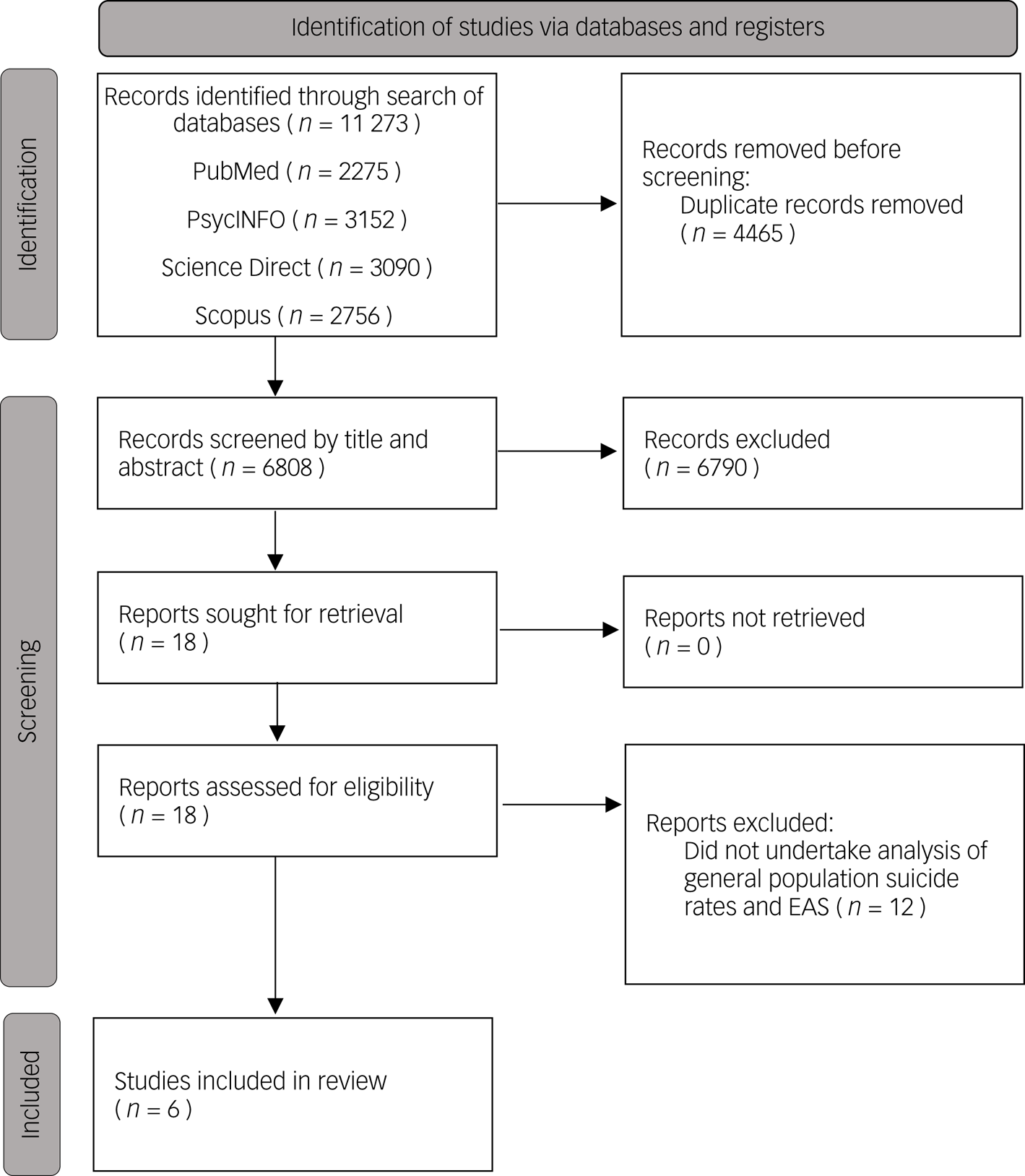
Fig. 1 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram for selection of studies in the systematic review. EAS, euthanasia and assisted suicide.
As all of these studies were retrospective and conducted at a population level, the level of detail regarding individuals was limited. We found six studies that met our inclusion criteria. The main details around methodology and primary findings are outlined in Table 1.
Table 1 Characteristics and summary of the included studies examining population suicide rates and EAS
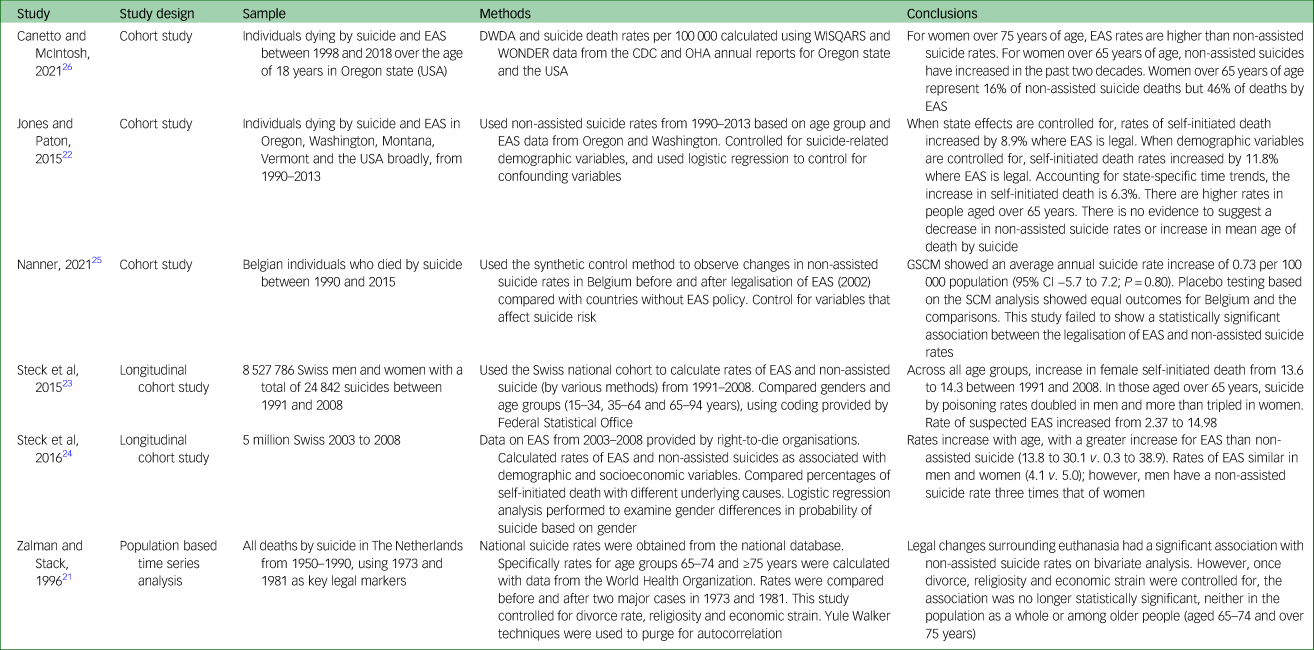
EAS, Euthanasia and Assisted Suicide; DWDA, Death with Dignity Act; WISQARS, Web-based Injury Statistics Query and Reporting System; WONDER, Wide Ranging Online Data for Epidemiologic Research; CDC, Center for Disease Control; OHA, Oregon Heath Authority; GSCM, Generalised synthetic control method; SCM, synthetic control method.
The earliest study that sought to establish the relationship between EAS and suicide was by Zalman and Stack.Reference Zalman and Stack21 Published in 1996, this study aimed to examine whether legal changes around the acceptability of EAS were associated with changes in the non-assisted suicide rates (numbers of deaths by suicide per 100 000 population) in the nation as a whole. This was not legislation for EAS, but rather changes in case law, which resulted in widespread changes in availability and practice. No reliable data were available for the rates of EAS, which is a significant limitation of this analysis. There was a significant positive association between EAS and suicide rates at both time points on bivariate analysis; however, once divorce, religiosity (as measured by the sale of religious books) and economic strain (as measured by unemployment rates) were controlled for, the association was no longer statistically significant, although it remained positive. Given the size of the population, this positive change is meaningful in itself: statistical significance is used in smaller samples to estimate whether an association is the result of chance. It is worth noting that raw population suicide rates rose throughout the period of the study (i.e. through the various legislative changes examined) from approximately six per 100 000 to approximately ten per 100 000.Reference Zalman and Stack21
In 2015, Jones and Paton examined EAS and non-assisted suicide rates in USA states where EAS had been legalised or decriminalised (Washington, Oregon, Vermont and Montana), and reported increased rates of both suicide and self-initiated death between 1990 and 2013.Reference Jones and Paton22 Data on rates of non-assisted suicide were obtained from the Centers for Disease Control and Prevention in all four states, and data on EAS were obtained from the regulators in Washington and Oregon; however, data on EAS rates in Montana and Vermont were not available. Rates of self-initiated death (which Jones and Paton termed ‘total suicide’) rose in all four states, and this was significant after controlling for unemployment rate, income, race and ethnicity, religious adherence, laws on cannabis use and drink driving, and state-specific trends – an increase of 6.5% in the population of the four states, and an increase of 14.5% in those aged 65 years and older.Reference Jones and Paton22 Rates of non-assisted suicide rose significantly by 4.4% after controlling for state and year effects and socioeconomic factors. However, this result was not robust to the inclusion of state-specific trends, after which the association was positive, but not statistically significant.
Also in 2015, Steck et al reported an overall reduction in suicide rates during the period of their study (1991–2008) based on the Swiss National Cohort. This reduction was broadly similar to the decline in suicide rates in European Union countries, and was associated with reduced access to lethal means (specifically firearms in the case of Switzerland) and improved access to mental healthcare.Reference Steck, Zwahlen and Egger23 Despite this, there was a rise in the mortality rate in older people, especially women. There was a significant increase in people dying by EAS. Suicide by poisoning doubled between the years 1991–1993 and 2006–2008 in men aged 65–94 years, and tripled in women in the same age bracket, where 80% of deaths by poisoning were attributed to EAS. The paper suggests that ‘further research is needed to clarify the reasons for the tripling of rates in assisted suicides in women, and the doubling of rates in men, and to what extent this difference might reflect greater vulnerability of women compared with men’.Reference Steck, Zwahlen and Egger23
A second study by the same authors, also from the Swiss National Cohort published the following year in the British Journal of Psychiatry, examined non-assisted suicide and EAS in the years 2003–2008, in a population of over 5 million people.Reference Steck, Egger and Zwahlen24 Overall, there were 5708 deaths by non-assisted suicide and 1325 by EAS. It reported fluctuations in non-assisted suicide rates (900–983 per annum), and an increase in EAS rates from 187 in 2003 to 246 in 2008. Women were overrepresented in the EAS group compared with the non-assisted suicide group, and had higher proportions of mental illness. Living alone and having no children were associated with higher rates of non-assisted suicide and EAS. Non-assisted suicide and EAS were more prevalent in people without a religious affiliation, and higher in Protestants than in Catholics, but these differences were greater in EAS than in non-assisted suicide. Higher education was positively associated with EAS, but negatively with non-assisted suicide. The authors argued that increases in EAS changed the epidemiology of suicide in Switzerland such that ‘analyses that distinguish between assisted and unassisted suicide are required to inform preventative interventions’.Reference Steck, Egger and Zwahlen24
In 2021, Nanner examined suicide rates in Belgium, using a synthetic control and generalised synthetic control methods (i.e. a control group was created by an algorithm) based on suicide rates in other European Union countries. The Netherlands and Switzerland were excluded from the study and although Luxembourg was included in the construction of the control, the study did not provide an analysis of the impact of EAS on non-assisted suicide rates in Luxembourg.Reference Nanner25 Data on suicide rates were extracted from Organisation for Economic Co-operation and Development data, and there was no data reported on rates of EAS in Belgium. Both analyses generated positive but non-significant associations of EAS and non-assisted suicide, with generalise synthetic control methods estimating an increase in the non-assisted suicide rate of 0.73 per 100 000 population (95% CI −5.7 to 7.2).Reference Nanner25
Canetto and McIntosh examined the relationship between EAS and non-assisted suicide in the state of Oregon in the USA over a 20-year period (1998–2018), following the legalisation of EAS.Reference Canetto and McIntosh26 They calculated the mortality rates by non-assisted suicide and EAS, and reported that women aged over 65 years represented almost half of all EAS deaths, and that EAS was the most common cause of self-initiated death in older women. Over this period, rates of EAS among older women increased by 496.4%, and increased among older men by 563.6% (before the legislation, rates would have been zero, so increased rates are to be expected). In this time period, non-assisted suicide rose by 56.4% among older women, whereas it fell by 10.9% among older men. Suicide by firearms was the leading cause of self-initiated death among older men. All-cause self-initiated death rose both among older women and older men.Reference Canetto and McIntosh26
Each of these studies was graded according to Oxford and NOS assessments (Table 2). All studies scored similarly on the Oxford quality assessment. On the NOS, three scored as high-quality studies (Jones and Paton,Reference Jones and Paton22 Steck et alReference Steck, Zwahlen and Egger23 and Steck et alReference Steck, Egger and Zwahlen24), two as medium-quality studies (Nanner,Reference Nanner25 and Canetto and McIntosh,Reference Canetto and McIntosh26 although Nanner was the stronger of the two) and one as poor-quality (Zalman and StackReference Zalman and Stack21). Zalman and StackReference Zalman and Stack21 suffered from lack of EAS data and lack of clarity as to whether suicide figures included EAS deaths, hence lack of case definition and no controls outside The Netherlands. Canetto and McIntoshReference Canetto and McIntosh26 provided data for EAS and non-assisted suicide, and stratified data by gender as well as age. However, they provided no controls for socioeconomic factors, and no estimate of significance for the changes in rates of non-assisted suicide and of self-initiated death. NannerReference Nanner25 developed a control model based on other European countries and provided a measure of significance. However, the study was limited in that it did not consider EAS data and only included one EAS country. Jones and PatonReference Jones and Paton22 considered the introduction of EAS in four different states at four different time points, and were able to control for time and state effects as well as socioeconomic factors and state-specific linear trends. Both studies by Steck et alReference Steck, Zwahlen and Egger23,Reference Steck, Egger and Zwahlen24 provided a detailed comparison of characteristics of cases of EAS and non-assisted suicide by analysis of the Swiss National Cohort. This was a longitudinal study of mortality in the Swiss population, based on linkage of census data with mortality records from 1990 to 2008 and including data on more than 7 million individuals.
Table 2 Quality assessment of the included studies
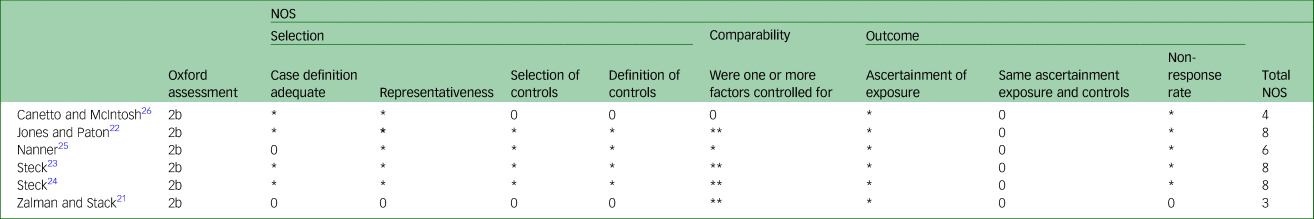
NOS, Newcastle–Ottawa Scale. The NOS ranges from 0–9 stars as follows: selection of the study group (up to 4 stars/points), comparability of cohorts (up to 2 stars/points) and ascertainment of outcome (up to 3 stars/points). High-quality studies achieve more than 7 stars, medium-quality studies 4–6 stars and poor-quality studies fewer than 4 stars.
Discussion
This systematic review found that there are few studies examining the association between EAS and rates of non-assisted suicide and/or rates of self-initiated death: only six studies met the inclusion criteria. The quality of these studies varied widely. All used different methods, thus precluding meta-analysis.
These studies cover four different jurisdictions: Switzerland, The Netherlands, Belgium and the USA. It is notable that most studies (four out of six) and all of those that scored as high quality (three), focused on Switzerland or the USA rather than on The Netherlands or Belgium. Neither of the studies from the Belgium or The Netherlands sought to analyse EAS data nor assess whether the introduction of EAS was associated with an increase in overall self-initiated death. Perhaps this is because EAS has long been an accepted part of practice in these jurisdictions.
Despite these divergences in analysis and the differences in practice between the four jurisdictions, there are some common results. No study found a negative association between EAS and non-assisted suicide. Canetto and McIntosh reported a reduction in non-assisted suicide in older men in Oregon between 1998 and 2018, but the overall non-assisted suicide rate in older people in that state increased over that period and the non-assisted suicide rate in older women increased by more than 50%.Reference Canetto and McIntosh26 Furthermore, those studies that controlled for socioeconomic factors all found a positive association between EAS and rates of non-assisted suicide, although generally these results were not statistically significant.Reference Zalman and Stack21,Reference Jones and Paton22,Reference Nanner25
There is no evidence from these studies to date to support the hypothesis that EAS reduces non-assisted suicide. More high-quality research is needed before it can be determined definitively whether there is no association between introduction of EAS and rates of non-assisted suicide, or whether there might be a small positive association, as suggested by some estimates in the study by Jones and Paton.Reference Jones and Paton22
Nanner argues that, although there is no evidence that the availability of EAS prevents death by suicide, it may reduce suicidal feelings.Reference Nanner25 He cites a study of 100 consecutive applications for euthanasia on the basis of a mental health in Belgium.Reference Thienpont, Verhofstadt, Van Loon, Distelmans, Audenaert and De Deyn27 Of these, eight were accepted but patients withdrew because ‘knowing they had the option gave them peace of mind to continue living; ergo, there was some alleviation of suicidal ideation’. However, Nanner does not acknowledge that, of these 100 patients, 43 had died by the end study period: 35 by EAS, one by palliative sedation (used in Belgium as an alternative to EAS), six by non-assisted suicide and one from anorexia nervosa; eight were still pursuing their euthanasia requests. An intervention that results in 42% of suicidal patients dying by self-initiated death over a 5-year period would not appear to be an effective means to alleviate suicidal ideation.
In relation to self-initiated deaths, Jones and Paton provide evidence for a significant increase of 6.5% in the USA, after controlling for state and year effects, socioeconomic factors and state-specific trends.Reference Jones and Paton22 The increase was 14.5% for those aged over 65 years. Steck et alReference Steck, Zwahlen and Egger23found that although suicide rates in Switzerland generally declined, a ‘substantial increase’ in EAS in older women resulted in ‘a net increase in the rate of suicide overall [i.e., of self-initiated death] in women’. At that time, rates of self-initiated death in men in Switzerland were decreasing but less so in older men because of EAS. Furthermore, since that time, rates of EAS have risen in all jurisdictions where it is legally available, and this has driven increases in self-initiated death.Reference Jones28 The change in rate of self-initiated death in Oregon between 1998 and 2018 for those aged over 65 years can be derived from the figures provided by Canetto and McIntosh.Reference Canetto and McIntosh26 Over this period, self-initiated death among those aged over 65 years increased by 59.6%m with an increase in older men of 23.3% and an increase in older women of 190.2%. Nanner provides no figures for EAS. However, since the introduction of the euthanasia law in Belgium in 2002, officially reported deaths by EAS have increased consistently year on year, with 2022 deaths by EAS recorded in 2015, up from 235 deaths in 2003. Nanner reports no significant decrease in non-assisted suicide in Belgium between 2002 and 2015, which suggests a substantial increase in self-initiated death.Reference Nanner25 Of these papers, only Jones and Paton provide confidence intervals for the estimated increase in self-initiated death after the introduction of EAS.Reference Jones and Paton22 Nevertheless, Canetto and McIntosh and Steck both provide evidence of large increases in EAS driving overall increases in rates of self-initiated death, and no paper provides evidence that would conflict with this conclusion.Reference Steck, Zwahlen and Egger23,Reference Steck, Egger and Zwahlen24,Reference Canetto and McIntosh26
One feature that was not part of the initial research question, but has emerged from the review, is the importance of considering gender when exploring associations between EAS, rates of non-assisted suicide and rates of self-initiated death. Canetto and McIntosh and both studies by Steck et al show that the change in self-initiated death after the introduction of EAS may be far greater in older women than in older men.Reference Steck, Zwahlen and Egger23,Reference Steck, Egger and Zwahlen24,Reference Canetto and McIntosh26 This is an omission in the studies by Jones and Paton, and Nanner.Reference Jones and Paton22,Reference Nanner25 The reasons why women may be more likely to die by EAS have been outlined variously as empowerment and disempowerment, depending on the perspective of the commentators. Data from suggests that women are more likely to seek EAS, with fears of being a burden: this consideration may be a factor in the gender disparity.Reference Canetto and McIntosh26,Reference Girma and Paton29 These disparities may be associated with lifelong disadvantages in social, occupational and economic areas in the context of women perceiving they are not as highly valued as men, and may have internalised a view that their value is relative to their service to others. Women also have higher incidences of depressive illnesses, which may indicate an unmet mental health need.
Several authors have drawn on this literature on suicide contagion as the basis for claims about the potential impact of EAS on non-assisted suicide rates or rates of self-initiated death.Reference Frei, Schenker, Finzen, Dittmann, Kraeuchi and Hoffmann-Richter30–Reference Neuner, Hübner-Liebermann, Hajak and Hausner32 However, whether there is such an effect and, if so, the size of this effect and the factors that might exacerbate or mitigate it, must be established independently. This review shows that there has been little quantitative research exploring this association to date. More research is urgently required to inform the debate around the legalisation of EAS in those jurisdictions where EAS is prohibited, and to inform suicide prevention strategy in jurisdictions where EAS is legally available.
In this review, the authors did not discover any other systematic literature review considering the potential association between EAS, rates of non-assisted suicide and rates of self-initiated death. This contrasts with the related topic of the impact of media reporting of suicides on suicide rates, variously termed suicide contagion or the ‘Werther effect’. This has been the focus of many original research papers and several systematic reviews and meta-analyses.Reference Cheng, Li, Silenzio and Caine33–Reference Niederkrotenthaler, Kirchner, Till, Sinyor, Tran and Pirkis36 This evidence base has, in turn, informed the development of guidance for the media on reporting suicide, the implementation of which has itself been the subject of review.Reference Mishara and Dargis37
In some jurisdictions where EAS has been decriminalised, it remains an offence to counsel, incite or encourage suicide.Reference Mishara and Weisstub38 This suggests that, even in jurisdictions where it is legal, EAS should not be promoted, and that, in parallel with efforts to prevent non-assisted suicide, consideration should be given to strategies to address the factors that make people vulnerable to death by EAS. There is a clear need for mental healthcare and suicide prevention among people with physical illnesses who would be eligible for EAS in some jurisdictions.Reference Haste, Charlton and Jenkins39,Reference Cheatle40 This review has found that that the availability of EAS is not associated with a reduction in non-assisted suicide, and that it may result in an increase in self-initiated deaths in women. The challenge of effective suicide prevention among older adults and those with chronic or terminal illnesses remains.
Limitations of this review include the small number of studies internationally that have explored the association between EAS and suicide in the general population. The primary research is itself limited by the challenges in controlling for the multitude of factors that affect both suicide and EAS. The only study that outlined the underlying diagnosis was the 2016 Swiss-based study by Steck et al, which reported that approximately 5% of people who died by EAS had a diagnosis of a mental illness.Reference Steck, Egger and Zwahlen24 This reflects the paucity of research in this area and indicates that there is a need to build the evidence base for better management of mental illnesses associated with suicidality, especially in people with physical (including terminal) illnesses. A further limitation is the fact that the data included in this study were all derived from the peer-reviewed literature and did not include independently produced reports. Also, this review may have missed some studies published in non-English language journals, as they were excluded from the searches. Finally, there may be a future role for a more focused systematic review to examine the effects of gender on uptake of EAS in more detail, where available.
This systematic review suggests that there is no association between EAS and reduced suicide rates in the countries where it is legislated for. This has consequences for the overall suicide prevention efforts in these and other countries, and may have particular implications for older women. The paucity of studies that could be included in this systematic review indicates a need for robust research into the covariates of suicidal ideation and self-initiated death in countries where EAS is legislated for. There is a need for specific research to examine the reasons for the disproportionate impact on the mortality of older women, and the impact of such legislation on groups with pre-existing psychiatric diagnoses or mental health problems. Further research should include consultations with expert individuals and groups in the jurisdictions where EAS is legal.
In conclusion, the findings of this review do not support the claims made that the introduction of EAS results in reduced rates of non-assisted suicide. Several studies reported increases in overall rates of self-initiated death and, in some cases, increases non-assisted suicide, although this latter increase was generally not significant when sociodemographic factors were controlled for. The studies based in Switzerland and Oregon suggest that older women might be disproportionately vulnerable to EAS where this is legislated for, and when the higher rates of depressive illnesses among women are considered, this may indicate a need to address suicide prevention more assertively in this population.
Data availability
The data that support the findings of this study are available from the corresponding author, A.M.D., upon reasonable request.
Author contributions
A.M.D., C.J.A. and D.A.J. all contributed to the formulation of the research question and designing of the study. A.M.D. and C.J.A. provided independent review of the data, with final inclusion of studies agreed by all authors. A.M.D. wrote the first draft of the manuscript. All authors were involved in writing the paper and approved the final draft.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
D.A.J. is Director of the Anscombe Bioethics Centre, an academic institute that engages with the moral questions arising in clinical practice and biomedical research. All other authors declare no competing interests.









eLetters
No eLetters have been published for this article.