Abstract
Background
Throat pain and airway discomfort are the most commonly upsetting conditions for patients’ wellbeing after surgery. However, little is known about the problem and associated factors, especially in developing countries like Ethiopia. Therefore, this work determined the magnitude, severity, and associated factors of throat discomfort within 24 h after elective surgery.
Results
The majority (63.2%, or 211) of the participants were female, with a mean age of 35.7 ± 9.7 years. The overall postoperative throat discomfort was observed in 122 (36.5%) patients, and it was severe in 20.5% of them. However, the severity level declined over time to 21.9% (21/96), 15.3% (18/118), and 5.6% (5/89), respectively, on the 1st, 6th, and 24th hours, as indicated by participants. Utilization of a larger ETT (AOR = 6.26, CI 2.13–18.43, P = 0.001), surgery lasting two or more hours (AOR = 11.20, CI 3.53–35.50, P = 0.000), awake extubation (AOR = 0.16, CI 0.05–0.43 P = 0.000), frequent episodes of hypotension (AOR = 12.85, CI 4.56–36.18, P = 0.000), and a less experienced anesthetist (AOR = 18.10, CI 6.51–50.31, P = 0.000) were significantly associated with throat discomfort.
Conclusions
Post-extubation throat discomfort complaints are high (36.5%). Due attention has to be given to minimize or prevent perioperative frequent episodes of hypotension, higher ETT size utilization, blood loss, and the duration of surgery as much as possible. Postoperative throat discomfort should not be ignored. And we recommend that patient reassurance and orientation with analgesia has to be considered during the postoperative period.
Similar content being viewed by others
Background
During surgery and anesthesia care, it is supposed to satisfy the demand for patient care and minimize associated complications. A safe and secure airway is achieved by an endotracheal tube (ETT), which is performed by an anesthetist or anesthesiologist. In our case, Ethiopia, it is widely done by anesthetists. However, throat pain and airway discomfort are common, uncomfortable, and distressing sequels after general anesthesia that mainly affect the postoperative patient's comfort (Cirilla et al. 2015; Muderris et al. 2019). Many pieces of research have been done worldwide regarding the incidence and factors associated with POST, which are overwhelmingly varied, ranging from 20 to 70% (Hu et al. 2013; Navarro and Baughman 1997; Edomwonyi et al. 2006; Kalil et al. 2014). In Ethiopia, very few researchers have addressed very few variables and have found the incidence of throat pain to be 45.6% in Ethiopian referral hospitals (Birhanu and Akalu 2017).
Several studies tried to address a number of possible factors contributing to the development of postoperative throat pain, like being female (Gupta et al. 2014; Alcock et al. 1993), the technical difficulty of intubation and suxamethonium use (Bum et al. 2012), airway suctioning, the long duration of surgery, laryngeal mask utilization (Xu et al. 2012), or mucosal injury with laryngoscopy, pharyngeal airway use, and larger endotracheal tubes or cuff pressure (Canbay et al. 2008; Gemechu et al. 2014; Cormack and Lehane 1984; Mencke and Noeldge-Schomburg 2010).
Many studies revealed that being female has been significantly associated with postoperative throat pain (Cirilla et al. 2015; McHardy and Chung 1999; Ahmed et al. 2007; Jaensson Llo and UN. 2010), while others still did not find any difference between the sexes (Edomwonyi et al. 2006; McHardy and Chung 1999; Lee et al. 2017).
An existing study often showed highly variable results. As one might expect and know, the current practice of airway management methods and surgical approaches also varies widely from institution to institution. In addition to this, there is limited information about the incidence, severity, and contributing factors of postoperative throat discomfort in developing countries like Ethiopia, where there are no adequate resources and qualified manpower.
Furthermore, the stage of extubation, estimated blood loss, intraoperative hypotension, cough on ETT, and others have not been considered in the so-far research. In this study, those variables were described once their association with postoperative airway-related discomfort was identified. Therefore, this study was conducted as a preliminary step to determine the magnitude and severity of postoperative throat discomfort at Ambo University Referral Hospital and analyze possible factors that contribute to its occurrence.
Methods
Study area setting and period
This study was conducted at Ethiopia university teaching and referral hospital, from July 1 to December 30, 2021. The hospital provides a range of health care services through specialty units in surgery, internal medicine, pediatrics, gynecology and obstetrics, ENT, and other minor departments. The hospital was supposed to serve 3.5 million people and had four major operation theaters (tables) on which both emergency and elective surgery was performed. The elective surgery that gets operated on each day ranges from 4 to 10 (on average, 6 patients) each day, with an approximate total of more than 1800 surgical procedures in a year. Elective surgeries were scheduled mainly in orthopedic surgery, maxillofacial and dental surgery, ophthalmology, general surgery, gynecologic surgery, and obstetric specialty units.
All patients were anesthetized using standard intravenous anesthetics (2 mg/kg of propofol, 4 mg/kg of thiopental, and 2 mg/kg of suxamethonium), and maintenance was either halothane or isoflurane.
An intubation was made with an endotracheal tube (ETT) size of 6.0 to 7.5 mm internal diameter (ID) tube using a standard Macintosh laryngoscope blade.
Study design
An institutional-based cross-sectional study was employed.
Source and study population
All patients who undergo surgery under general anesthesia during the study period and who meet inclusion criteria during the study period.
Inclusion criteria
All patients whose age was 18 years or older and who underwent surgery were included in the study.
Exclusion criteria
Patients who are classified as ASA-3 or above, have a recent or ongoing upper respiratory tract infection (URTI), have a history of recent nasogastric tube insertion or nasal intubation, have double-lumen ETT, or have pre-existing voice change or difficulty swallowing were excluded from the study.
Sample size and sampling procedure
Using a single population proportion formula and a throat pain proportion of 59.6% at Gondar University Teaching Hospital (Gemechu et al. 2014), with a 95% CI and a 5% margin of error.
The sample size calculated to be n = 370.
To recruit each study subject we used a systematic sampling technique (k = 2). The data were collected from the participant after every two patients. The first patient was arbitrarily selecting from the participants’ list (scheduling board) when the first-day data collection started.
Study variable
Dependent
Presence of throat discomfort after elective surgery (yes/no).
Severity level was graded by asking the patient to indicate on a visual analogue scale (VAS; 0 no pain, < 3 mild, 4–6 moderate, > 7 severe, and 10 the worst pain imaginable) OR own five finger was used representing thumb no complain, index finger mild, middle finger moderate, ring finger severe, and little finger the most imaginable discomfort.
Independent
Sociodemographic characteristics
Age, sex, body mass index (BMI)
Surgical-related characteristics
Surgical diagnosis, duration of surgery/ETT in the trachea, Estimated Blood Loss in milliliter, intraoperative frequency of hypotension episodes and types of surgical procedure,
Anesthetic related characteristics
ASA classification, duration of anesthesia, ETT size, extubation mode (deep/awake), cough while ETT inside, and anesthetist’s experience.
Data collection
Data was collected through patient interviews and card review using a semi-structured questionnaire during postoperative time trying to point out at which the pain was worst immediately (at 1st or 6th hours or 24 h), after the patient fully recovered from anesthesia and felt comfortable answering the interviewer’s question. Even though there is no clear time to assess postoperative throat discomfort, it would be better as early as possible, as many scholars suggest (Orandi et al. 2013; Liu et al. 2010; Estebe et al. 2002). Demographic data; age, sex, weight, height, American Society of Anesthesiologists (ASA) physical status, surgical procedure type, duration of intubation, size of a cuffed endotracheal tube (ETT) used extubation mode, intraoperative recorded hypotension, estimated intraoperative blood loss (EBL), and anesthetists year of experience were recorded on the prepared sheet form. The interviewer asks a direct question about dysphagia and or dysphonia-related symptoms, including “choking,” “coughing,” “hard to chew,” “hard to swallow,” “lump in the throat,” and “trouble swallowing,” and any hoarseness or voice change after surgery.
Data quality control and analysis process
A pretest was done on 5% of the sample size before actual data collection and necessary corrections and modifications were made to the questionnaires. Each questionnaire was checked for completeness and entered into SPSS.V.20 statistical software for analysis. Bivariate and multivariate logistic regression analysis was used to determine the association of various factors with the outcome variable. In logistic regression analysis, each explanatory variable with an outcome variable was assessed for its association, and those variables whose p value < 0.25 were taken as candidate variables for multiple logistic regressions for further analysis of their true association. Variables with a P value < 0.05 were reported with 95% CI as a statistically significant variable.
Ethics approval and consent to participate
Ethical clearance and approval was obtained from IRB committee—with project code of CMHS/S-R-Anesth/02/13—and permission were confirmed from hospital administration. An informed written consent was obtained from each study participant before actual data collection. The confidentiality and privacy of the study participant were kept secret using questionnaire coding. Data was collected after their volunteer participation was confirmed with their signature. Those patients who had had pain were linked to the responsible physician for treatment.
Results
Demographic characteristics
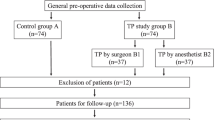
Three hundred seventy (370) patients participated from a total of 747 elective surgeries performed during the study period. Of which, 334 (90.3%) participants’ data were included for analysis (and 36 were excluded because 4 nasal tubes were used, 14 prior throat complaints, and 18 with incomplete documentation). The majority of the participants were female (63.2%), ASA-I (American Society of Anesthesiologists) (77.5%), 18–24 BMI (68%), and older than 30 years (66.8%) with a mean of 35.7 ± 9.7 years (Table 1).
Anesthesia and surgery-related characteristics
All patients were anesthetized using standard intravenous anesthetics (2 mg/kg of propofol or 4 mg/kg thiopental and 2 mg/kg suxamethonium) and intubated with an endotracheal tube (ETT) size of 6.0 to 7.5 mm using Macintosh blade laryngoscope. Most surgical procedures lasted more than 2 h in 175 (52.4%) and ranged from a minimum duration of 40 min to a maximum of 3½ hours. About 46.4% of the participants had recorded intraoperative hypotension episodes; of which 78.7% (122) had had more than two times episodes. The commonly performed surgery includes general, orthopedics, cesarean delivery, and gynecology in a different position (Table 2).
Outcome and possible risk factors
Postoperative throat discomfort was complained by 122 (36.5%) participants within 24 h after extubation. The majority 98(78.8%) of them noticed the discomfort immediately (within an hour) as soon as they got consciousness (Fig. 1).
The severity level seems declining over time courses; only 5.6% of the compliant experiences severe discomfort on the 3rd round visit compared to that of 1st and 2nd round visit, 21.9% and 15.3%, respectively. However, the overall throat discomfort were found to be severe in 25(20.5%), moderate in 38(31.1%), and mild in 59(48.4%).
The likely hood of throat discomfort complaints among patients extubated in a deep state of anesthesia decreases by 0.16 odd (AOR = 0.16, CI 0.05–0.43 P = 0.000) compared to awake extubation. Whereas the complaints has positive association with frequent (three or more) episodes of intraoperative hypotension (AOR = 12.85, CI 4.56–36.18, P = 0.000), after a larger size of an endotracheal tube (ETT) (AOR = 6.26, CI 2.13–18.43, P = 0.001), the surgery lasted two or more hours duration (AOR = 11.20, CI 3.53–35.50, P = 0.000), and less experienced (< 2 years) anesthetists by 18.10 more when compared to the counterpart patients (AOR = 18.10, CI 6.51–50.31, P = 0.000) (Table 3).
Discussion
Achieving a safe and secure airway by endotracheal tube (ETT) plays a vital role during anesthesia care services. However, airway-related complaints after surgery under general anesthesia has been continued to be challenging and overwhelming the comfort patients during postoperative time sore throat, hoarseness, dysphagia, neck pain, difficulty to cough, and dysphonia are among the commonest problems after endotracheal tube extubation (ETT) (Muderris et al. 2019; Hu et al. 2013; Burgard et al. 1996).
Anesthesia science and practices had advanced too much distance in decreasing postoperative morbidity and mortality; within the last few decades. However, the problem is much worse in sub-Saharan countries.
The prevalence of postoperative airway-related complaints is widely varied, ranging from 20 to 70% (Hu et al. 2013; Navarro and Baughman 1997; Edomwonyi et al. 2006; Kalil et al. 2014). In developed countries, universities or teaching hospitals in Iran (Farazmehr et al. 2021), Saudi Arabia (Aqil et al. 2017), and China (Li et al. 2021); the incidence is (documented as low as 26.3%, 36.3%, and 16.2–31.9%, respectively. Whereas, in Nigeria teaching hospital, it was found to be as high as 63% (Edomwonyi et al. 2006) and 58.9% (Doukumo et al. 2011). In Ethiopia, the two studies conducted in the northern part of the country at Gondar and Debretabor teaching hospital showed 59.6% and 48.8%, respectively (Gemechu et al. 2014; Fenta et al. 2020).
Here in Ambo University referral hospital, we found the overall prevalence of postoperative throat discomfort after 24 h is 36.5%. Our study relatively found less prevalence than the others. However, incongruent with our result a study conducted in a Turkey teaching hospital found 37.7% throat pain complaints (Muderris et al. 2019). This variation could be explained as the inconsistent standard of care followed during perioperative time; which is challenging in resource-limited settings like AURH, where the burden of illness and mortality from potentially treatable conditions is higher than in resource-rich settings where standards of operating procedures guidelines are implemented. Barriers to providing quality care in different settings include a lack of epidemiological data and contextual evidence for medical decision-making, gaps in health systems organization and resources, and institutional barriers to implementation. On top of this, the discrepancy might be due to sample sizes and data collection time differences. On the other hand, the educational level and understanding level of the question to be replied might be responded to differently.
In this study, we found larger endotracheal tube (7.0–7.5) is associated (AOR = 6.26, 95% CI = 2.13–18.43, p = 0.001) with postoperative throat discomfort. A different researcher had reported similar findings (McHardy and Chung 1999; Jaensson Llo and UN. 2010; Farazmehr et al. 2021; Li et al. 2021).
This is explained for two reasons: direct mechanical trauma and prolonged vascular compression resulting in low blood flow to the mucosa that might be followed by the inflammation process. With similar justification, prolonged surgery (two or more hours) duration of procedures (AOR = 11.20, 95% CI = 3.53–35.50, p = 0.00), and less experienced (less than 2 years) anesthesia provider (AOR = 18.10, 95% CI = 6.51–50.31, p = 0.00) were found to be associated with the postoperative airway related discomfort and complain. This is because more manipulation and repeated attempts at laryngoscopy are common in less experienced anesthetists. On the other hand, long-standing compression of the underlying laryngeal mucosal surfaces by inflated EET cuff pressure is accompanied by low perfusion to the area and mucosal injury from hypo perfusion. Incongruent with our findings, the different researchers explained this scenario (Edomwonyi et al. 2006; Kalil et al. 2014; Ahmed et al. 2007). Unlike other studies, we did not find an association between gender and throat discomfort. Other researcher also found no difference in sore throat complaints between males and females (Farazmehr et al. 2021). In the future, this area needs to be studied in-depth.
This study depicts that the severity of complaint of throat discomfort decreases over time; on the 1st Vs 6th, Vs 24th-hour interviews 21.9%, 15.3%, and 5.6%, respectively complained of a severe form of discomfort. This finding is supported by Farazmehr et al.; they found that the prevalence of sore throat post-laryngeal mask use within 1, 6, and 12 h after the surgery was 16.5–36.1%, 13.6–33.3%, and 10.7–28.7%, respectively (Farazmehr et al. 2021). There are also other researchers who identified that throat pain is declining after 6 h (Aqil et al. 2017; Christiansen et al. 2021).
We observed that some participants were recovered within 6 h (two individuals) and 33 patients within 24 h. This can be explained by the swelling secondary to inflammation becoming resolved as time elapsed among patients whose inflammation is not severe enough (Kapadia et al. 2021).
The implication of the paper
As one might expect and know, current practice of airway management methods and surgical approaches widely varies from institution to institution. This paper will widen the insight of emphasis to be given to the preventable risk factors of postoperative throat discomfort specially in the limited resource countries. It will help to prevent or minimize postoperative-associated complications and mortality.
Limitation of the study
Although this study provided valuable information, there are some limitations that could be addressed in another study. A chart review might be retrieved with incomplete information and the patients were interviewed at an inconvenient time. In addition, data on other variables needed to observe intactness of recurrent laryngeal nerve injury, vocal cord examination, and ETT cuff pressure monitoring during the intraoperative period; to predict whether the throat discomfort resulted from airway instrumentation or direct surgical insults during procedure; were not addressed due to the impossibility of the resource available and accesses in our setup.
Conclusions
During anesthesia care, securing an airway using an endotracheal tube is a very important part of care. However, throat pain and airway discomfort continue to be upsetting conditions of patient comfort after surgery in resource-limited countries. The overall postoperative throat discomfort complaint within 24 h after endotracheal tube (ETT) extubation was high (36.5%) and it was severe at 21.3% (26/122).
Due attention has to be given in the case of larger ETT-sized utilization, surgery lasting > 2 h duration, awake extubation, frequent episodes of intraoperative hypotension, and less experienced anesthetist.
Availability of data and materials
The data set used and analyzed in this study is available from corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted odd ratio
- ASA:
-
American Society of Anesthesiologist physical status
- AURH:
-
Ambo University Referral Hospital
- BP:
-
Blood pressure
- COR:
-
Crude odd ratio
- EBL:
-
Estimated blood loss
- EBVt:
-
Estimated total blood volume
- ETT:
-
Endotracheal tube
- GA:
-
General anesthesia
- HPT:
-
Hypotension
- LMA:
-
Laryngeal mask airway
- mmHg:
-
Millimeter mercury
- NGT:
-
Nasogastric tube
- OPV:
-
Oropharyngeal view
- PACU:
-
Post-anesthesia care unit
- POST:
-
Post-operative sore throat
- PVC:
-
Polyvinylchloride
- SPSS:
-
Statistical package for social sciences
- URTI:
-
Upper respiratory tract infection
- VAS:
-
Visual analog scale
References
Ahmed A, Abbasi S, Ghafoor HB, Ishaq M (2007) Postoperative sore throat after elective surgical procedures. J Ayub Med Coll Abbottabad Apr-Jun 19(2):12–14 PMID: 18183710
Alcock R, Peachey T, Lynch M, Mcewan T (1993) Comparison of alfentanil with suxamethonium in facilitating nasotracheal intubation in day-case anaesthesia. Br J Anaesth 70(1):34e7. https://doi.org/10.1093/bja/70.1.34
Aqil M, Khan MU, Mansoor S, Mansoor S, Khokhar RS, Narejo AS (2017) Incidence and severity of postoperative sore throat: a randomized comparison of Glidescope with Macintosh laryngoscope. BMC Anesthesiol 17(1):1–8. https://doi.org/10.1186/s12871-017-0421-4
Birhanu MS, Akalu LG (2017) Magnitude and associated risk factors of post-operative sore throat following surgery by general anesthesia with endotracheal intubation in black lion hospital, addis ababa Ethiopia. Int J Anesthesiol Res 5(2):409e13. https://doi.org/10.19070/2332-2780-1700084
Bum H, Dae J, Kim H, Jeong Y (2012) The effect of cuff pressure on postoperative sore throat after Cobra perilaryngeal airway. J Anesth 26:225e9. https://doi.org/10.1007/s00540-011-1293-2
Burgard G, Möllhoff T, Prien T (1996) The effect of laryngeal mask cuff pressure on postoperative sore throat incidence. J Clin Anesth 8(3):198–201. https://doi.org/10.1016/0952-8180(95)00229-4
Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar U (2008) Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth 100(4):490e3. https://doi.org/10.1093/bja/aen023
Christiansen P, Pedersen CH, Selter H, Odder L, Riisager JP, Damgaard K, Westmark S, Bruun NH, Melgaard D (2021) How does tube size affect patients’ experiences of postoperative sore throat and hoarseness? A randomised controlled blinded study. J Clin Med 10(24):5846. https://doi.org/10.3390/jcm10245846. PMID:34945142;PMCID:PMC8708773
Cirilla DJ 2nd, Ngo J, Vaisman V, Daly C, Ata A, Sandison M, Roberts K (2015) Does the incidence of sore throat postoperatively increase with the use of a traditional intubation blade or the Glide Scope? J Clin Anesth. Elsevier Inc. 27(8):646–51. https://doi.org/10.1016/j.jclinane.2015.06.005
Cormack RS, Lehane J (1984) Difficult tracheal intubation in obstetrics. Anaesthesia 39(11):1105–1111. https://doi.org/10.1111/j.1365-2044.1984.tb08932.x. PMID: 6507827
Doukumo D, Faponle A, Adenekan A, Olateju S, Bolaji B (2011) Effects of lidocaine and k-y jellies on sore throat, cough, and hoarseness following endotracheal anaesthesia. J West Afr Coll Surg 1(3):44–61
Edomwonyi NP, Ekwere IT, Omo E, Rupasinghe A (2006) Postoperative throat complications after tracheal intubation. Ann Afr Med 5(1):28–32
Estebe JP, Dollo G, Le Corre P, Le Naoures A, Chevanne F, Le Verge R, Ecoffey C (2002) Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg 94:227–230. https://doi.org/10.1097/00000539-200201000-00044
Farazmehr K, Aryafar M, Gholami F, Dehghanmanshadi G, Hosseini SS (2021) A prospective study on the incidence of sore throat after use of laryngeal mask airway during general anesthesia. Ann Med Surg (Lond) 26(68):102595. https://doi.org/10.1016/j.amsu.2021.102595. PMID: 34401120; PMCID: PMC8353405
Fenta E, Teshome D, Melaku D, Tesfaw A (2020) Incidence and factors associated with postoperative sore throat for patients undergoing surgery under general anesthesia with endotracheal intubation at Debre Tabor General Hospital, North central Ethiopia: A cross-sectional study. Int J Surg Open 25:1–5. https://doi.org/10.1016/j.ijso.2020.06.003
Gemechu BM, Gebremedhn EG, Melkie TB. (2014): Risk factors for postoperative throat pain after general anaesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, Pan Afr Med J 2017;27(127). https://doi.org/10.11604/pamj.2017.27.127.10566
Gupta D, Agrawal S, Sharma JP (2014) Evaluation of preoperative Strepsils lozenges on incidence of postextubation cough and sore throat in smokers undergoing anesthesia with endotracheal intubation. Saudi J Anaesth 8:244e8. https://doi.org/10.4103/1658-354X.130737
Hu B, Bao R, Wang X, Liu S, Tao T, Xie Q, Yu X, Li J, Bo L, Deng X (2013) The size of endotracheal tube and sore throat after surgery: a systematic review and meta-analysis. PLoS One 8(10):e74467. https://doi.org/10.1371/journal.pone
JaenssonLlo M, UN. (2010) Endotracheal tube size and sore throat following surgery: a randomized-controlled study. Acta Anaesthesiol Scand 54(6):147e53. https://doi.org/10.1016/j.ijso.2020.06.003
Kalil DM, Silvestro LS, Austin PN (2014) Novel preoperative pharmacologic methods of preventing postoperative sore throat due to tracheal intubation. AANA J 82(3):188–197
Kapadia AA, Shafiq F, Raza A (2021) Post operative sore throat: Comparison between macintosh versus video laryngoscope in patients intubated by trainee anaesthetists - a randomised control trial. Pakistan J Med Sci 37(3):764–769. https://doi.org/10.12669/pjms.37.3.3365
Lee JY, Sim WS, Kim ES, Lee MS, Kim KD, Na RY, Park D, Park JH (2017) (2017): Incidence and risk factors of postoperative sore throat after endotracheal intubation in Korean patients. J Int Med Res 45(2):744–752. https://doi.org/10.1177/0300060516687227
Li X, Wang X, Zhao Y, Jiang Z, Lv X, Nie X, Li T, Wang X, Dai L, Liu S (2021) Incidence of postoperative sore throat after using a new technique of insertion of a second generation Laryngeal Mask Airway: A randomised controlled trial. Eur J Anaesthesiol 38(3):285–293. https://doi.org/10.1097/EJA.0000000000001378
Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, Zhang M, Hang Y (2010) Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicentre study. Anesth Analg 111:1133–1137. https://doi.org/10.1213/ANE.0b013e3181f2ecc7
McHardy FE, Chung F (1999) Postoperative sore throat: cause, prevention and treatment. Anaesthesia 54(5):444–453. https://doi.org/10.1046/j.1365-2044.1999.00780.x
Mencke T, Noeldge-Schomburg G (2010) Laryngeal morbidity after use of the laryngeal mask airway. Acta Anaesthesiol Scand 54:127e8
Muderris T, Tezcan G, Sancak M, Gul F, Ugur G (2019) Oral flurbiprofen spray for postoperative sore throat and hoarseness: a prospective, randomized, double-blind, placebo-controlled study. Minerva Anestesiol 85(1):21–22. https://doi.org/10.23736/S0375-9393.18.12703-9
Navarro RM, Baughman VL (1997) Lidocaine in the endotracheal tube cuff reduces postoperative sore throat. J Clin Anesth 9(5):394–397. https://doi.org/10.1016/s0952-8180(97)00068-8. PMID: 9257206
Orandi A, Orandi A, Najafi A, Hajimohammadi F, Soleimani S, Soleimani S, Zahabi S (2013) Postintubation sore throat and menstruation cycles. Anesth Pain Med 3:243–249. https://doi.org/10.5812/aapm.11416
Xu YJ, Wang SL, Ren Y, Zhu Y, Tan ZM (2012) A smaller endotracheal tube combined with intravenous lidocaine decreases post-operative sore throat. Acta Anaesthesiol Scand 56:1314e20. https://doi.org/10.1111/j.1399-6576.2012.02768.x
Acknowledgements
We thank all participants, hospital administration and data collectors for their cooperation and time during the whole process.
Funding
We did not receive any financial support from commercial or business company.
Author information
Authors and Affiliations
Contributions
All authors (HJ and ZB) equally worked from the initiation of study design and the interpretation of data. Both authors participated in the writing, critically revised, and approve the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval were obtained from Ambo University College of Medicine and Health Science “institutional research review board (IRB) committee—with project code of CMHS/S-R-Anesth/02/13” to undertake research and publish the result.
We attest that any human studies undertaken as part of this research is in compliance with regulation of our institution and generally accepted guidelines governing such work in the country, Ethiopia. We obtain informed consent from each participant before the commencement of the research work.
Consent for publication
The participants were informed the result will not provide an identifiable individual or personal information; however, statistical descriptive data would be published.
Competing interests
Both authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jisha, H., Bekele, Z. Postoperative throat discomfort and associated factors among surgical patients at Ethiopian Teaching Hospitals: cross-sectional study. Ain-Shams J Anesthesiol 15, 53 (2023). https://doi.org/10.1186/s42077-023-00350-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-023-00350-6