Abstract
Background
Chorea hyperglycemia basal ganglia syndrome is a rare disorder causing involuntary movements in both upper and lower limbs. Uncontrolled hyperglycemia causes neurotransmitter derangements in basal ganglia resulting in involuntary movements. These cases pose different challenges to anaesthesiologist in both general and regional anaesthesia.
Case presentation
Here, we discuss a case of chorea hyperglycemia basal ganglia syndrome with lower limb gangrene posted for knee amputation done under spinal anaesthesia. Our patient had recurrent choreiform movements due to non-compliance to diabetic medications. Strict glycemic control always aids in reduction of choreiform movements along with improved wound healing.
Conclusions
Tight glycemic control and good anesthetic plan in perioperative period can reduce morbidity in patients affected with chorea hyperglycemia basal ganglia syndrome.
Similar content being viewed by others
Background
Chorea hyperglycemia basal ganglia syndrome (CHBG) is a rare condition characterized by hemichorea-hemiballism with uncontrolled blood sugars, the prevalence of which constitutes only 1% of all chorea-ballism cases (Gómez-Ochoa et al. 2018). It has a predilection towards elderly females of Asian ethnicity (Cosentino et al. 2016). Strict glycemic control is the cornerstone in its prevention and management. There are no reports of patients with CHBG requiring anesthetic or surgical care. We present a case of CHBG with lower limb soft tissue infection posted for above knee amputation managed under spinal anesthesia.
Case presentation
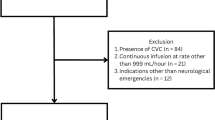
A 69-year-old female, of BMI 18, known diabetic for past 10 years presented with left lower limb diabetic gangrene and was planned for left above knee amputation. Past history revealed involuntary movements involving her right upper and lower limb 5 years back for which she was evaluated. Her laboratory investigations showed elevated sugars of 400 mg/dl with negative urinary ketones. Rheumatic chorea was ruled out by negative history for carditis and arthritis, which was corroborated by low ASO (anti-streptolysin-O) titer. Hyperthyroidism was ruled out by normal TSH (thyroid stimulating hormone) value of 1.23. Coagulation profile, electrolytes, ceruloplasmin levels, erythrocyte sedimentation rate, renal, and liver functions were normal. Echocardiography showed mild aortic sclerosis with normal ejection fraction.
MRI (magnetic resonance imaging) had T1 hyperintensity in left basal ganglia without any blooming or restriction suggestive of metabolic etiology (Fig. 1). As there was no diffusion restriction, stroke as an etiology for chorea was ruled out. Brain SPECT (single photon emission computed tomography) scan showed moderate hypoperfusion in left basal ganglia. In view of hyperglycemia and MRI suggesting metabolic etiology for basal ganglia hyperintensity, she was diagnosed with chorea hyperglycemia basal ganglia syndrome. She was treated with oral hypoglycemics and tetrabenazine, after which chorea resolved.
In her present admission, blood sugar was 300 mg/dl, with no ketoacidosis. HbA1C-8%. She had been non-compliant to diabetic drugs. Examination revealed normal higher mental functions and choreiform movements involving orofacial region, tongue, and right upper limb more than the lower limb. These movements were associated with hypotonia of right upper and lower limb. Though she had no respiratory distress or auscultatory abnormalities, she had abnormal breathing pattern due to chorea-induced respiratory dyskinesia. Since patient had lower extremity gangrene with pus pockets, we considered early surgery for source control of ongoing development of sepsis. We chose spinal anesthesia as with general anesthesia, there was risk of respiratory muscle dysfunction, aspiration, and reported prolonged apnea. Under strict aseptic precautions, spinal anesthesia was administered in sitting position with 2 ml of 0.5% hyperbaric bupivacaine through a 25-G Quincke needle and a sensory level of T10 was obtained. Surgery lasted for 1 h. Since random blood sugar was high (256 mg/dl), insulin infusion was started for sugar control. Intraoperatively lower limb chorea abolished after spinal and upper limb movements were reduced with midazolam. Post-operatively, chorea manifested in the lower limb after spinal level regressed and reduced over a period of 5 days once tight blood sugar control was achieved.
Discussion
Chorea hyperglycemia basal ganglia syndrome (CHBG) also known as non-ketotic hyperglycemic hemichorea or diabetic striatopathy, is a condition caused by chronic hyperglycemia. The triad of CHBG involves non-ketotic hyperglycemia, chorea-ballism, and basal ganglia hyperintensities on neuroimaging (Chang et al. 2017). The exact mechanism is not well understood. Hyperglycemia cause local shift of aerobic brain metabolism to anaerobic metabolism. Also, hyperglycemia induced hyperviscosity causes a reduced regional cerebral blood flow. During anaerobic metabolism, GABA (gamma amino butyric acid) becomes the main energy source for brain leading to its depletion (Chang et al. 2017). During ketosis, ketones are used as energy source, and GABA is produced from acetoacetate. GABA being an inhibitory neurotransmitter, its depletion leads to excitatory output and involuntary movements. This is postulated as the reason for chorea-ballism not occurring in ketosis (Aquino et al. 2015). The predilection of CHBG in postmenopausal women is explained by estrogen deficiency causing sensitization of nigrostriatal dopamine receptors (Sitburana and Ondo 2006).
MRI hyperintensities involve putamen in all cases, and caudate nucleus in 50% of cases (Cosentino et al. 2016). Other conditions causing hyperintense T1 abnormalities on MRI include carbon monoxide, methanol, cyanide poisoning, and hyperammonemia from cirrhosis (Sperling and Bhowansingh 2018). Our patient did not have any history or laboratory findings suggestive of these conditions. Hemichorea can occur in other conditions and so other causes of hemichorea, like stroke, neoplasm, thyrotoxicosis, liver dysfunction, Wilson disease, and rheumatic chorea, were ruled out based on the absence of neuropsychiatric symptoms, biochemical, and neuroradiological findings (Sperling and Bhowansingh 2018). Huntington chorea unlike other chorea presents with hypertonia rather than hypotonia.
Previous hospital record showed that the patient had involuntary movements involving only the right upper and lower limbs. However, at presentation involuntary movements were seen in orofacial region, tongue, and neck. We choose spinal anesthesia in our patient because in general anesthesia, risk of aspiration could be there due to disco-ordinated movements and residual neuromuscular blockade. Even though the elderly population exhibit increased sensitivity to succinylcholine, chorea patients may exhibit prolonged apnea following induction with thiopentone and succinyl choline (Esen et al. 2006). As surgery was of shorter duration, we wanted to avoid general anesthesia induced unnecessary risk of prolonged apnea and delayed extubation. Also, in postoperative period, risk of aspiration is very high due to sedative effects of anesthetic agents compounded with weakened airway reflexes.
Neuraxial anesthesia is relatively contraindicated in sepsis patients due to presence of coagulopathy, systemic infection, and weakened action of local anesthetics in vicinity of infection or acidosis. But our patient had bleeding time—1 min, clotting time—4 min and 30 s, PT/INR (prothrombin time/international normalized ratio)—12 s/1.3, platelet count— 2.23lakhs/mm3. Also, she had raised TLC (total leucocyte count) of 16,000/mm3, neutrophils 90%, mild metabolic acidosis. Considering the risk benefit ratio and pros and cons of spinal anesthesia over general anesthesia in this CHBG scenario, we decided to administer spinal anesthesia in our patient.
Proper positioning for spinal anesthesia is challenging since these patients have continuous movements and can have self-sustain injury during positioning. We allotted two separate personnel to obtain sitting position for spinal anesthesia. Painful lower limb lesion with involuntary movements precluded lateral positioning for spinal. After achieving subarachnoid block, patient was covered with warmers to prevent shivering and hypothermia.
If general anesthesia needs to be administered, primary focus should aim to provide airway protection with endotracheal intubation and rapid sequence induction. Centrally acting anti-cholinergics and pethidine should be avoided as they can worsen chorea by causing neurotransmitter imbalances. If required, glycopyrrolate can be used as it does not cross blood brain barrier. Induction agents like thiopentone and midazolam exhibit increased sensitivity in such patients. Hence such patients require less dosage and titrated administration should be practiced. Inhalational agents carry risks of increased shivering, generalized spasms and prolonged recovery (Esen et al. 2006). TIVA (total intravenous anesthesia) using propofol is a good alternative. Avoid metoclopramide as it can exaggerate choreiform movements. Ondansetron can be used as a good alternative to metoclopramide. Also sedatives should be cautiously administered in these patients in titrated doses. Extubation after general anesthesia in patients with respiratory dyskinesia would be an added challenge. So, extra edge of caution has to be exercised while extubating such patients.
Our patient had a relapse of hemichorea after the initial event which occurred 5 years back. Recurrence of chorea in cases of CHBG has already been described, following a new hyperglycemic episode especially in the setting of infection.
Conclusions
Prevention and treatment of CHBG lies in glycemic control (Aquino et al. 2015). CHBG presents a benign spectrum of myriad diabetic complications, posing additional difficulties to the patient, thus emphasizing the need for strict glycemic adherence. We have addressed specific issues related to this case, like glycemic control, airway management, positioning concerns, and choice of anesthetic agents. Recent literature search regarding this case does not address all these issues which we faced during our experience in this case. Hence, such patients, when planned for an emergency surgery, should be managed meticulously after appropriate planning to avoid undue complications.
Availability of data and materials
Not applicable
Abbreviations
- CHBG:
-
Chorea hyperglycemia basal ganglia syndrome
- ASO:
-
Anti-streptolysin-O
- TSH:
-
Thyroid stimulating hormone
- MRI:
-
Magnetic resonance imaging
- SPECT:
-
Single photon emission computed tomography
- GABA:
-
Gamma amino butyric acid
- PT/INR:
-
Prothrombin time/International normalized ratio
- TLC:
-
Total leucocyte count
- TIVA:
-
Total intravenous anesthesia
References
Aquino JHW, Spitz M, Pereira JS (2015) Hemichorea-hemiballismus as the first sign of type 1b diabetes during adolescence and its recurrence in the setting of infection. J Child Neurol 30(10):1362–1365
Chang X, Hong W, Yu H, Yao Y (2017) Chorea associated with nonketotic hyperglycemia: A case report with atypical imaging changes. Medicine (Baltimore) 96(45):e8602
Cosentino C, Torres L, Nuñez Y, Suarez R, Velez M, Flores M (2016) Hemichorea/hemiballism associated with hyperglycemia: report of 20 cases. Tremor Hyperkinetic Mov N Y N 6:402
Esen A, Karaaslan P, Can Akgün R, Arslan G (2006) Successful spinal anesthesia in a patient with Huntington’s chorea. Anesth Analg 103(2):512–513
Gómez-Ochoa SA, Espín-Chico BB, Pinilla-Monsalve GD, Kaas BM, Téllez-Mosquera LE (2018) Clinical and neuroimaging spectrum of hyperglycemia-associated chorea-ballism: systematic review and exploratory analysis of case reports. Funct Neurol 33(4):175–187
Sitburana O, Ondo WG (2006) Tetrabenazine for hyperglycemic-induced hemichorea-hemiballismus. Mov Disord 21(11):2023–2025
Sperling M, Bhowansingh R (2018) Chorea hyperglycemia basal ganglia syndrome in a 63-year-old male. Case Rep Med e9101207. https://doi.org/10.1155/2018/9101207. PMID: 30532787
Acknowledgements
Nil
Funding
None
Author information
Authors and Affiliations
Contributions
Author TA has substantially conducted and contributed to the work, and drafted and revised the manuscript. Author DC conducted and contributed to the work and assisted in drafting and revision of manuscript. AK substantially analyzed the work and revised the intellectual content of the work. SS has substantially conducted and contributed to the work, and drafted and revised the manuscript. All the authors approved the final version and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Informed written consent obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arikrishnan, T., Chakravarthy, D., Kuberan, A. et al. Anesthetic management of a patient with chorea hyperglycemia basal ganglia syndrome planned for above knee amputation. Ain-Shams J Anesthesiol 14, 50 (2022). https://doi.org/10.1186/s42077-022-00249-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00249-8