- Research
- Open access
- Published:
A rapid review to inform the policy and practice for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care
Health Research Policy and Systems volume 22, Article number: 34 (2024)
Abstract
Background
More than 35% of Aboriginal and Torres Strait Islander adults live with cardiovascular disease, diabetes, or chronic kidney disease. There is a pressing need for chronic disease prevention and management among Aboriginal and Torres Strait Islander people in Australia. Therefore, this review aimed to synthesise a decade of contemporary evidence to understand the barriers and enablers of chronic disease prevention and management for Aboriginal and Torres Strait Islander People with a view to developing policy and practice recommendations.
Methods
We systematically searched for peer-reviewed published articles between January 2014 to March 2023 where the search was performed using subject headings and keywords related to “Aboriginal and Torres Strait Islander peoples,” “Chronic Disease,” and “Primary Health Care”. Quality assessment for all included studies was conducted using the Aboriginal and Torres Strait Islander Quality Appraisal Tool. The data were extracted and summarised using a conventional content analysis approach and applying strength-based approaches.
Results
Database searches identified 1653 articles where 26 met inclusion criteria. Studies varied in quality, primarily reporting on 14 criteria of the Aboriginal and Torres Strait Islander Quality Appraisal Tool. We identified six key domains of enablers and barriers of chronic disease prevention and management programs and implied a range of policy and practice options for improvement. These include culturally acceptable and safe services, patient-provider partnerships, chronic disease workforce, primary health care service attributes, clinical care pathways, and accessibility to primary health care services. This review also identified the need to address social and cultural determinants of health, develop the Aboriginal and Torres Strait Islander and non-Indigenous chronic disease workforce, support multidisciplinary teams through strengthening clinical care pathways, and engage Aboriginal and Torres Strait Islander communities in chronic disease prevention and management program design and delivery.
Conclusion
Enabling place-based partnerships to develop contextual evidence-guided strategies that align with community priorities and aspirations, with the provision of funding mechanisms and models of care through policy and practice reforms will strengthen the chronic disease prevention and management program for Aboriginal and Torres Strait Islander people.
Introduction
Aboriginal and Torres Strait Islander people have continuously demonstrated strength, tenacity, and resilience in the face of a high burden of chronic disease associated with profound health, social, economic and cultural and wellbeing impacts. The disproportionate burden of chronic disease—particularly cardiovascular disease (CVD), type II diabetes and chronic kidney disease (CKD)—is driven by the effects of colonisation. These effects include intergenerational trauma, racism and commercial determinants such as the introduction of ultra-processed foods, tobacco, sugar-sweetened beverages, and alcohol [1, 2].
More than 35% of Aboriginal and Torres Strait Islander adults report having CVD, diabetes or CKD, 38% have two of these conditions and 11% have all three [3]. Nearly 70% of Australia’s burden of disease from CVD is attributable to modifiable risk factors including high blood pressure, dietary risks, high body weight, high cholesterol and smoking [4]. These risk factors, and subsequent disease, can be prevented. This prevention can be primordial (by addressing the structural drivers at a population level, such as food supply and recreation facilities) or primary (through identifying people at risk and taking individual steps to reduce that risk).
Primary prevention and management of chronic disease among Aboriginal and Torres Strait Islander people in Australia predominantly occurs in primary care settings. Universal primary care in Australia is largely funded through a fee-for-service model via the Medicare Benefits Scheme (MBS), with some augmentation for Aboriginal and Torres Strait Islander people through the Indigenous Australian’ Health Programme [5]. Primary care is delivered by a range of providers, including Aboriginal Community Controlled Health Organisations (ACCHOs) which are governed by a local board, Aboriginal Medical Services run by State and Territory governments, and private primary care services (sometimes referred to as ‘mainstream’ providers). Chronic disease services in primary care include risk assessment, support for healthy behaviours, referrals to allied health and pharmacology for risk reduction. High quality, culturally safe primary care can prevent the development of disease, and manage complications, for individuals and communities [6,7,8]. Strengthening primary care is a key strategic priority of the Australian government, [9, 10] peak bodies and other stakeholders working to improve the health and well-being of Aboriginal and Torres Strait Islander communities [11, 12].
Understanding how primary care services, prevention and management programs can best meet the needs of Aboriginal and Torres Strait Islander people, who are living with or at risk of chronic disease, is critical to addressing disparity in outcomes. A review conducted by Gibson et al. in 2015 explored chronic disease care for Indigenous communities globally, but there has been no comprehensive contextual evidence available focusing on Aboriginal and Torres Strait Islander people [13]. Therefore, there is a need for local evidence disease on chronic prevention and management for Aboriginal and Torres Strait Islander people in Australia. The Aboriginal and Torres Strait Islander People’s Health Assessment (MBS item number 715) is an annual health check funded for Aboriginal and Torres Strait Islander people and a cornerstone of early detection for chronic disease [14]. The number of Health Assessments fell for the first time in 2020 and 2021 after years of sustained growth [15]. The reduction in Health Assessments is likely to reflect disruption to routine primary care services during the COVID-19 pandemic [16].
Our team were contracted by the Australian Commonwealth Department of Health and Aged Care to understand best practice delivery of chronic disease care for Aboriginal and Torres Strait Islander people in 2020. The effects of the COVID-19 pandemic accelerated the need for this research and necessitated a pivot to rapid review strategy. The Oxford Centre for Evidence-Based Medicine highlights [17] that rapid review methodology can be used to meet the needs of commissioning bodies in policy-relevant timeframes. Therefore, this rapid review aims to synthesise contemporary and contextually relevant barriers and enablers for chronic disease care in primary care settings for Aboriginal and Torres Strait Islander people with a view to developing near term policy and practice recommendations.
Methods
This review applied the SelecTing Approaches for Rapid Reviews (STARR) decision tool that includes interaction with commissioners, scoping the literature, selecting approaches to literature search, methods for data extraction and evidence synthesis [18]. It was conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guideline [19]. We searched two databases (Medline and Web of Science) to identify relevant studies from January 2014 to March 2023. These two databases were chosen because of following reasons: (i) Medline database provides access to articles from 5,200 journals in about 40 languages covering the biomedical and life sciences including Aboriginal and Torres Strait Islander peoples as a MeSH Headings and (ii) Web of Science is the world’s oldest interdisciplinary and widely used database of research publications that covers over 34,000 journals today.
This timeframe follows on from a systematic review conducted by Gibson et al. [13] which included data up to December 2013. This rapid review mirrors the Gibson methodology with two main changes: i) narrowing focus from Indigenous communities globally to Aboriginal and Torres Strait Islander contexts in Australia, ii) narrowing focus from all chronic diseases to focus on the three major contributors to chronic disease burden (cardiovascular disease, diabetes and chronic kidney disease). The review was performed between January to August 2023.
In this review, Aboriginal and Torres Strait Islander researchers and Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members were actively engaged and consulted in all steps, from the inception of the research questions to the completion of this review. Throughout the process, the research team met monthly with the Australian Commonwealth Department of Health and Aged Care during the period of this review to inform the scope of evidence synthesis.
Positionality: The senior author of this review Pearson (nee Gibson, first author of the 2015 review), is Kuku Yalnji/Torres Strait Islander health systems researcher. KB-B (Torres Strait Islander) and JC (Gumbaynggir) are experienced researchers with particular expertise in quality assessment of Aboriginal and Torres Strait Islander research studies. UNY (Madhesi, Nepal) is an implementation scientist, JD is a non-Indigenous medical student and RW is a non-Indigenous practising general practitioner and researcher.
Operational definition of key terminology used in this review:
-
a)
Holistic care or support: The care process that involved strategies to support mental, physical, cultural and spiritual health which is beyond the individual level that values family and community capacity and governance [20].
-
b)
Systems thinking: Systems thinking is conceptual orientation concerned with inter-relationships between different levels, institutions, systems, and people nested within social, cultural, economic, political contexts to deliver a holistic care [21].
-
c)
Place-based partnerships: Place-based partnerships involve collaborative arrangements the unique needs and circumstances of both the community and service provider. In this context, place-based partnerships involve a formal partnership among government, service providers and First Nations representatives. These partnerships are specific to geographical locations and population groups and are aimed at designing or delivering services that directly respond to community needs, aspirations and local priorities, while valuing local cultural values [22, 23].
Scoping the literature:
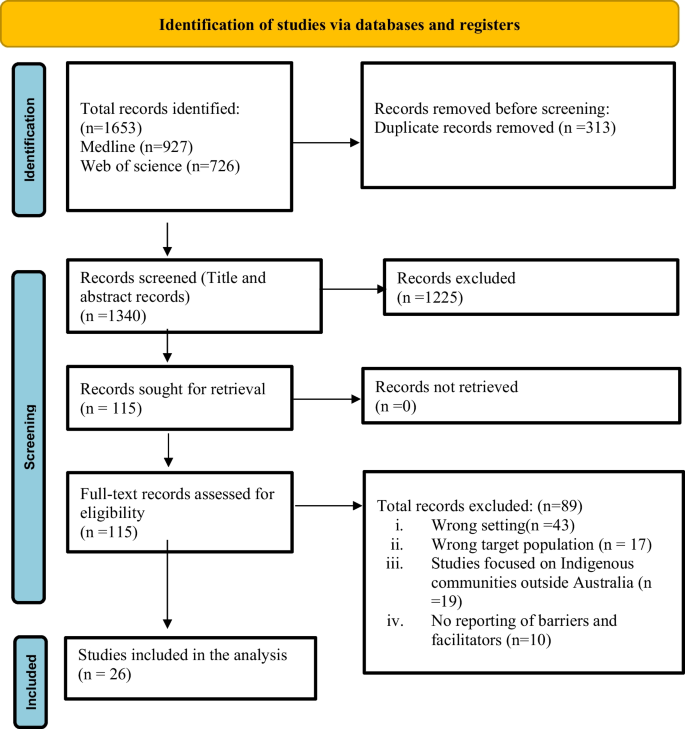
The search was performed using a combination of subject headings and keywords related to “Aboriginal and Torres Islander peoples,” “Chronic Disease,” and “Primary Health Care” using “OR” and “AND” iterated from the search strategy described in a study by Gibson et al. [13] The search strategy has been provided in Box 1. The search results obtained from two databases were imported to Endnote and uploaded on the Covidence platform for title and abstract and full-text screening [24]. Three reviewers (UNY, JMD and RW) independently screened the titles and abstracts of potential studies for eligibility based on inclusion and exclusion criteria (Table 1). Full-text articles were assessed by two reviewers and any disagreement that appeared during the screening process was resolved through discussion with the third reviewer (RW). The details of the screening process are documented as a PRISMA flow diagram (Fig. 1).
Box 1: Search strategy
1. PubMed/Medline | |
|---|---|
Search#1 | (Indigenous [tiab] OR Aborigin* [tiab] OR Torres Strait Islander [tiab] OR First Nation [tiab] OR Oceanic Ancestry Group [Mesh]) |
Search#2 | (Chronic disease [tiab] OR Chronic illness [tiab] OR Cardiovascular disease [tiab] OR Heart disease [tiab] OR Atherosclerosis [tiab] OR Stroke [tiab] OR Arrhythmia [tiab] OR Heart attack [tiab] OR Myocardial infarction [tiab] OR Hypertension [tiab] OR Kidney disease [tiab] OR renal disease [tiab] OR Diabet* [tiab] OR Chronic disease [Mesh] OR Cardiovascular disease [Mesh] OR Kidney Diseases [Mesh] OR Diabetes Mellitus [Mesh]) |
Search#3 | (Primary health [tiab] OR primary care [tiab] Community [tiab] OR rural [tiab] OR Remote [tiab] OR Outreach [tiab] OR intervention [tiab] OR program* [tiab] OR general practice [tiab] OR "Primary health care" [Mesh] OR "Health Services, Indigenous" [Mesh]) |
Search#4 | Australia |
Search#5 | #1 AND #2 AND #3 AND #4 |
Limits: Publication date from 01/01/2014 to 28/03/2023; English language | |
2. Web of Science | |
(((ALL = (Chronic disease OR Chronic illness OR Chronic respiratory disease OR Obstructive lung disease OR Chronic obstructive pulmonary disease OR Bronchiectasis OR Asthma OR Cardiovascular disease OR Heart disease OR Atherosclerosis OR Stroke OR Arrhythmia OR Heart attack OR Myocar Results for (((ALL = (Chronic disease OR Chronic illness OR Chronic respiratory disease OR Obstructive lung disease OR Chronic obstructive pulmonary disease OR Bronchiectasis OR Asthma OR Cardiovascular disease OR Heart disease OR Atherosclerosis OR Stroke OR Arrhythmia OR Heart attack OR Myocardial infarction OR Hypertension OR Kidney disease OR renal disease OR Diabetes Or depression OR Chronic disease OR Respiratory Tract Diseases OR Cardiovascular disease OR Kidney Diseases OR Diabetes Mellitus)) AND ALL = (Primary health OR primary care OR intervention OR program OR general practice OR Primary health care OR Health Services)) AND ALL = (Indigenous OR Aboriginal OR Torres Strait Islander OR First Nation)) AND ALL = (Australia) and Review Article (Exclude—Document Types) and Letter or Meeting Abstract or Editorial Material (Exclude—Document Types) and Proceeding Paper or Early Access or Data Paper or Correction (Exclude—Document Types)dial infarction OR | |
Data extraction
An iterative process was used to define data extraction domains. A total of fourteen potential domains were identified from the systematic review conducted by Gibson et al., alongside the He Pikinga Waiora Implementation Framework [25] and an access framework for Aboriginal and Torres Strait Islander people [26]. Further, three discussions were held within the team and with other Aboriginal and Torres Strait Islander researchers that identified eight domains of interest for both barriers and enablers (design attributes, chronic disease workforce, patient/provider partnership, clinical care pathways, access-accessibility, access-acceptability, system thinking and knowledge translation). A data extraction tool was prepared to extract information about the study characteristics (title, author, publication year, study setting, study objective, study design, types of services) and eight domains decided from the discussions mentioned above. A data extraction tool was shared with the Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members at the National Centre for Aboriginal and Torres Strait Islander Wellbeing Research at the Australian National University for their input. Based on inputs from Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members and team discussion, some domains were consolidated and made an agreement of extracting data focusing six domains (culturally acceptable and safe services, patient provider partnerships, chronic disease workforce, primary health care service attributes, clinical care pathways and accessibility to primary health care services) the final data extraction tool included study characteristics and six domains (Fig. 2)focusing both barriers and enablers. The data extraction tool was piloted on five included studies that facilitated shared understanding of approach to data extraction between team members. The data were extracted by UNY and JMD between May to June 2023.
Evidence synthesis and quality appraisal
Quality assessment for all included studies was conducted using the Aboriginal and Torres Strait Islander Quality Appraisal Tool that privileges Aboriginal and Torres Strait Islander people’s (knowing) epistemology, (being) ontology, (doing) axiology and ethical research governance [27]. The extracted data were analysed and summarised using a conventional content analysis approach [28] that allows the categories and the name of the categories to flow from the data and applying strength-based approaches [29].
Findings
Study selection and its characteristics
For the period 2013- 2023, a total of 1653 articles were retrieved from Medline (n = 927) and Web of Science (n = 726) databases. Of the total, 313 were duplicates which left 1340 articles for screening. Following the screening, 115 studies were selected for the full-text review. Upon full-text review, 89 articles were excluded, leaving 26 articles to be included for extraction and evidence synthesis. Service delivery models of the included studies were ACCHOs, government-run Aboriginal Medical Services and private general practice. The majority of the studies applied qualitative or mixed-method evaluation approaches (see Additional file 1).
Quality appraisal results
All studies met two criteria from the Aboriginal and Torres Strait Islander Quality Appraisal Tool: priority determined by community (criterion 1) and use of an Indigenous research paradigm (criterion 9). Over 92% studies met criteria for community protocols (criterion 5), 80% of studies met criteria addressing community consultation and engagement (criterion 2), Aboriginal and Torres Strait Islander leadership (criterion 3) and 76% studies had demonstrated Aboriginal and Torres Strait Islander governance in research (criterion 4). While 30% or less of the studies addressed existing intellectual and cultural property (criterion 6 and 7), 70% studies met the following criteria: Aboriginal and Torres Strait Islander people control over collection and management of research materials (criteria 8), use of strength based approach and acknowledging practices that have harmed Aboriginal and Torres Strait Islander communities (criterion 10) translation of findings into sustainable changes (criterion 11), benefit the participants and Aboriginal and Torres Strait Islander communities (criterion 12), demonstrate capacity strengthening for Aboriginal and Torres Strait Islander people (criterion 13), and researchers have opportunities to learn from each other (criterion 14). Details are provided in Table 2.
Enablers and barriers to the implementation of chronic disease initiatives
Enablers and barriers (see Additional file 2) are presented under six thematic domains and relevant sub-themes presented below:
-
1.
Primary health care service attributes
-
a)
Aboriginal and Torres Strait Islander engagement and Aboriginal leadership in system design: Aboriginal and Torres Strait Islander project leadership and community engagement were overwhelmingly identified as key determinants for system design [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. Engagement through outreach cultural community events and stakeholder partnerships appear to amplify these effects [48]. Six studies investigated how information was exchanged between knowledge-users and researchers throughout the studies [30, 38, 44,45,46,47]. Knowledge users included Aboriginal and Torres Strait Islander communities, primary health care providers (ACCHOs and mainstream providers), Aboriginal and/ or Torres Strait Islander health workers and practitioners, other service providers, and policymakers. Alongside this, one study acknowledged the utilisation of cultural and scientific evidence to provide best-practice healthcare [37]. Aboriginal and Torres Strait Islander project leadership consistently facilitated trust and satisfaction. Use of evidence-based clinical care guideline in project implementation within community and services were other key benefits of knowledge translation.
-
b)
Primary health car responsive to local community needs: Prospective analysis of potential barriers for program development were essential to program success, in order to actively address these in the program design and implementation. Many studies clearly demonstrated how barriers were overcome through tailored solutions including: outreach services to save patient time and cost [30, 31, 45, 49]; free of charge services [31, 49,50,51]; 24-h culturally safe service [32, 37, 50]; and telehealth specialist services [51, 52]. Outreach services (delivered outside of the clinic facility) included home medication delivery, general visits by health workers to build trust and screening for conditions at community-based events. Services which were free at point of care included medications, nicotine patches, hospital specialist clinics, supplementary services (e.g. cooking class, aged care services), and preventive initiatives (e.g. blood pressure measurement, glucose monitor and health promotion activities). Innovative primary care models for Aboriginal and Torres Strait Islander patients included flexible appointment systems [32, 37, 50], multidisciplinary teams for providing holistic care [37, 38, 51], and clinical audits for quality improvement were also effective [31, 34, 39, 45, 46]. Incorporating chronic disease prevention into primary care occurred through health promotion initiatives [30, 35, 37, 50, 51], and patient-led prevention initiatives and management plans [30, 46, 50] were also found to be invaluable in addressing community needs. Six studies explicitly emphasised the importance of adequate resources and flexible funding for primary care services to meet local Aboriginal and Torres Strait Islander community priorities and needs [30, 32, 36,37,38,39].
-
c)
A holistic approach to care: Aligned with Aboriginal and Torres Strait Islander peoples’ perception of health, holistic support [30, 38, 44] and care coordination was critical, necessitating flexible funding, and systems thinking and innovative, locally-adapted reforms [30, 31, 46]. Social referral approaches that connected people to non-clinical services were an important component in Aboriginal community controlled primary care settings, for example: connecting patients to exercise groups, providing access to housing, opportunities for hobbies, or home care services such as ‘Meals on Wheels’ [38, 40, 41, 53].
-
d)
Primary care access: Several barriers were identified, including: a lack of support specific to Aboriginal and Torres Strait Islander leadership [34, 39, 51, 53, 54]; competing priorities of healthcare service delivery [30, 34, 39]; and a lack of funding specifically address social determinants of health [31, 55]. These were more pronounced in Aboriginal PHC. There were also insufficient resources to engage stakeholders in the co-development of primary care programs. This contributed to poor connections and relationships between multidisciplinary teams in health centres and other actors, including clinical information management systems [34, 48, 51, 54], and high turnover of trained staff [34, 50, 54]. Some studies highlighted challenges in creating culturally appropriate services, due to the heterogeneity of Aboriginal and Torres Strait Islander populations [32, 39, 55]. Moreover, accessing primary care services was particularly challenging for people with the greatest health needs [31], including those with limited health literacy which made it difficult for people to engage with chronic disease care [48, 49].
-
2
Chronic disease workforce
-
a)
Creating supportive environment and building capacity of primary healthcare workforce: Enabling safe and good work environments for Aboriginal and Torres Strait Islander Health Workers and Practitioners [30, 35, 54], and a shared sense of purpose amongst staff to address the complex needs of patients [30, 47] were consistently identified as enablers. Eight studies highlighted the importance of dedicated staff for chronic disease management, with clear delegation of responsibilities and a positive team culture created through an engaging and collaborative work environment [30, 36, 37, 39, 43, 46, 51, 54]. Establishing the health care workforce with chronic disease ‘portfolios’ were considered more able to provide recurrent, culturally safe, preventative, and responsive healthcare for Aboriginal and Torres Strait Islander people because they had a greater chance of forming trusting relationships [32, 41, 48, 50]. Included studies highlighted the need for training and development of the primary healthcare workforce [30, 31, 33, 55]. Four studies had a particular focus on local Aboriginal and Torres Strait Islander Health Workers and Practitioners including the importance of recruitment and retention strategies [31, 34, 39, 46], alongside a need to clarify their roles, provide Aboriginal and Torres Strait Islander role models [40, 41, 50, 52], and ensure they are involved in clinical decision making [30, 33, 35, 37, 39, 43, 44, 52, 54]. The importance of intensive cultural safety training for staff to deliver safe care was emphasised in five studies [37, 47, 49, 54, 55].
-
b)
Barriers to sustainable chronic disease workforce at primary health care services: Nine studies noted staff shortages and high staff turnover as adversely impacting continuity of care [32,33,34, 39, 43, 46, 50, 51, 53], and three studies noted inadequate clinical training for non-Indigenous staff [32, 46, 53]. Workforce limitations contributed to lack of time and resources to reach the patients that needed healthcare the most [31, 45, 46]. Nine studies specifically emphasised the substantial shortages, high turnover, and high rates of burnout of Aboriginal and Torres Strait Islander staff [33, 34, 39, 43, 46, 51, 53,54,55]. Work overload, inadequate support and a sense of being undervalued contributed to these issues [32, 33, 43]. Four studies noted shortages of specialists as a key barrier to integrated chronic disease management pathway [34, 43, 46, 47].
-
3.
Patient-provider partnerships
-
a)
Optimal care achieved by effective trustful patient-provider partnerships: Eight studies found that enablers of trusting patient-provider relationships included strengthening patient knowledge through interactive learning, culturally appropriate conversation, and strengths-focused clinical engagement [30, 32, 33, 35, 38, 50, 53, 55]. Numerous studies highlighted that holistic care required mechanisms for communities, families/carers and community leaders to be engaged with service providers [30, 45, 52,53,54]. ACCHOs were generally identified as meeting these needs by offering culturally safe care, longer consultation times to facilitate patient/provider partnerships [32, 37], and communicating with the community when there were changes in services, or the implementation of new programs [31].
-
b)
Contextual barriers to patient-provider partnership: Barriers to partnership included competing priorities for patients [53], patient experiences of racism and discrimination [32], patient discomfort with non-Indigenous services [32], and patients sensing that their holistic needs were unmet [42]. Two studies reported that limited health literacy with little shared provider-consumer understanding of chronic conditions were barriers to forming positive relationships [31, 46]. Three studies noted a general lack of connection between the clinician and patient but did not interrogate the contributors to this [32, 49, 55].
-
4.
Clinical care pathways
-
a)
Enablers to effective clinical information systems: Nine studies found in-house information technology support within primary healthcare services was crucial for effective patient referral, coordination, and follow-up care [30,31,32, 34, 38, 39, 43, 46, 55]. Of these, two highlighted the importance of partnership-enabled integration across health service organisations using a shared electronic health record system, disease registration multidisciplinary care plans, and a patient recall system [30, 36]. While translation of evidence-based care guidelines were not mentioned, five studies explained the importance of capacity building of staff and investment in systems development for the effective use of clinical information systems [30, 34, 39, 43, 51].
-
b)
Barriers to efficient clinical information systems: Information technology barriers were profound, including poor integration information technology systems, mixed paper and electronic records [43, 46, 51, 53], and poor infrastructure – most notably internet access [34, 52, 54]. Four studies noted shortages of trained and regular staff to implement new pathways, as a key barrier to integrated chronic disease management pathways [34, 43, 46, 47]. Inconsistent models of care [44], and poor communication between different hospital and primary care systems [50] were also barriers.
-
5.
Access to primary health care services
Many of the recognised domains of healthcare access (accessibility, accommodation, availability, accessibility and affordability) were identified [56].
-
a)
People and family-centred reforms improve access to adequate primary care: Enablers of access to primary health care services were identified in ten studies [30,31,32, 38,39,40,41, 43, 45, 49, 53]. Transportation support was a determining and/or motivating factor for clients to access health services [31, 38, 39] Other studies [45, 49] [43] identified accommodation factors, particularly flexible appointment systems, reduced waiting times and co-location with allied health services as key enablers. In this review, a number of motivational factors were identified for people to attend services, including support or referral from family members, higher motivation to look after oneself following the death of a family member, and motivation texts or invitational messages for health check from service providers [32, 41, 53]. In addition, one study identified providing financial incentives as an enabler for health checks [32].
-
b)
Unaddressed social determinants prevent access to primary care services: Barriers to accessing primary health care services related to socio-economic factors, health system factors and lack of health promotion factors. Socio-economic factors included accessibility and affordability considerations; lack of transport [30,31,32, 44, 46, 49, 50, 53,54,55], inability to afford health and social services, and medication costs [31, 32, 44, 47, 49]. Some studies alluded to socioeconomic factors being prioritised over primary care attendance, including household crowding and food insecurity. Ensuring that services account for competing priorities, including family and cultural responsibilities, was an important enabler [45, 55].
-
c)
System related access barriers: Health system factors included high staff turnover, lack of availability of appointments, long waiting periods, physically inaccessible clinics [43, 44, 46], poor leadership of primary care services [32, 45, 47,48,49], and limited internet and computer access [47]. Inadequate awareness of available services was also problematic [31, 33, 49]; initiatives run by primary care services had limited uptake when the community was not made aware of these programs [46]. Health systems need to be able to deliver services and information multimodally. For example, not all patients have phones or phone credit all the time, so several forms of communication may be required.
-
6.
Culturally acceptable and safe services
-
a)
Enablers to deliver culturally safe and acceptable services: Cultural safety is essential to the development of a mutually respectful relationship between providers and Aboriginal and Torres Strait Islander people. A systems level approach is needed to address racism experienced by Aboriginal and Torres Strait Islander people in primary care settings [30, 44]. Strategies for addressing or achieving cultural safety varied by context, but the role of Aboriginal and Torres Strait Islander healthcare workers including cultural brokerage was emphasised in two studies [31, 52]. The need for gender-specific services and gender sensitivity was emphasised by five papers as an important part of providing culturally safe care. This included delivery of programs such as gender-based exercise groups, private consultation areas for males and females, gender specific health assessment days, and employing male and female Aboriginal and Torres Strait Islander healthcare workers [31, 41, 45, 46, 52]. The provision of culturally safe services also included a need for culturally appropriate education materials, artwork, and Aboriginal and Torres Strait Islander people’s voices and images as signifiers of belonging [30, 44,45,46, 53]. Three studies recognised the importance of enabling Aboriginal and Torres Strait Islander patients and staff access to flexibly attend to family, community, cultural and spiritual responsibilities, and obligations to provide a culturally safe service [37, 42, 44]. One study identified the need for robust anonymous feedback systems for staff and patients to improve culturally safe care delivery [47].
-
b)
Barriers to deliver culturally safe and acceptable services: Barriers to delivering culturally safe and acceptable services related to systems, structures and lived experiences. Systems issues to providing culturally safe services included language barriers [32], poor health literacy among patients [54], long wait times due to staff shortages [32, 50, 54], a sense that services were superficial/rushed [31, 42], and lack of physical space to provide holistic care or gender-based services [43, 44, 46]. Lived experiences of treatment of Aboriginal and Torres Strait Islander people within Western systems, including health and social services, elicits feelings of harm rather than help: a fear of discrimination and racism was a key barrier to Aboriginal and Torres Strait Islander patients accessing healthcare services in five studies [31, 32, 44, 49, 53] alongside fear of diagnosis due to historical trauma [53]. These barriers were amplified where there was limited access to Indigenous-specific services [32, 44, 46]. One study mentioned a tokenistic approach where very limited community input to governance, planning, and program design was sought to develop culturally safe initiatives [46].
Discussion
This is the first review since 2014 [13] to present the barriers and enablers of implementing chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people. The enablers and barriers found in this study have several policy and practice implications that should be considered in design, implementation, and funding targets for future chronic disease prevention and management programs.
The most striking addition to our findings, relative to the 2014 [13] review, is the acknowledgment of Aboriginal and Torres Strait Islander culture (including staff, protocols, leadership, practices and ways of doing business) as a key enabler to engagement and care delivery. Partly, this is attributable to this review’s narrower focus on the Australian context. It also likely reflects increasingly detailed academic descriptions of the ways in which leadership and governance tangibly affect care delivery as part of contemporary Closing the Gap reform. All studies included in this review made some acknowledgement of culture, albeit with variations in how deeply culture was considered as an enabler of care. Our review team grappled with how best to reflect this focus on culture, given that it is both a distinct concept and intimately embedded in all thematic domains. Ultimately, we have chosen to keep Aboriginal and Torres Strait Islander culture as a separate domain to ensure that culture is given independent consideration, in addition to attention within other thematic domains. It is evident that access to culturally appropriate, affordable and comprehensive services are vital for preventing and managing chronic conditions [37]. There is no one-size-fits-all approach for models of care for Aboriginal and Torres Strait Islander communities, and programs must be tailored to local context. Recent studies have identified numerous opportunities for improving access to primary care services: creating welcoming spaces, improving the cultural safety of healthcare services, building strong trustworthy relationships between patients and providers, and building primary healthcare workforce capacity [37, 57, 58]. The span of this theme is necessarily broad, encompassing Aboriginal and Torres Strait Islander leadership, physically welcoming spaces, training for non-Indigenous staff, time to build trusting relationships. Ensuring that culture is prospectively and proactively considered in funding and delivery of primary care of chronic disease should be a priority for practitioners and policy makers.
There is clear evidence that addressing holistic needs of Aboriginal and Torres Strait Islander people enables greater engagement, rather than a narrow clinical focus on physical aspects of health. This requires primary care services to acknowledge and address the broader social and cultural determinants of health for Aboriginal and Torres Strait Islander people. Many of these have a direct impact on both chronic disease risk factors and capacity to access care (chronic disease management), including poor access to healthy and nutritious food, inadequate housing, rurality, lack of transportation, and financial barriers [59, 60].Some of these disparities more pronounced in remote and rural Australia, where Aboriginal and Torres Strait Islander communities are further marginalised by distance and poverty [61, 62]. Enablers of chronic disease care, such as outreach services, transportation, and referrals networks to other allied health and community groups are more likely to be effective where holistic approaches are adopted. This is consistent with data from the Australian Institute of Health and Welfare highlighting the experiences of social inequity in Aboriginal and Torres Strait Islander communities and the positive impact on health outcomes when inequities are reduced [63]. Previous studies [13, 64] have identified various obstacles to accessing primary health care services which include inadequate infrastructure, inflexible and inadequate funding to care for people holistically. Evidence also suggests that for Aboriginal and Torres Strait Islander people, travel to access health care means being separated from their country, family and social network that directly impacts their health and wellbeing as described by Milroy’s Dance of Life [65]. While government subsidies are in place, travel and accommodation costs incurred by Aboriginal and Torres Strait Islander people to access healthcare, may require upfront payment or indirect costs, perpetuating financial barriers for Aboriginal and Torres Strait Islander people living in rural and remote areas [66]. Therefore, it is crucial that primary health care initiatives take a holistic and system thinking approach to program design, considering the impact of social and cultural determinants on the health of individual, family members and their communities, with every attempt to reduce systemic barriers to access to healthcare where possible.This is only possible when funding mechanisms and models of care are flexible enough to account for local and individual contexts.
The profound impact of workforce was clear throughout this review. Recruiting, and retaining staff and effective training, were found to be key barriers to implementing and maintaining holistic patient-centred chronic disease prevention and management programs [13, 67]. Evidence has shown that Aboriginal and Torres Strait Islander people prefer support delivered by Aboriginal and/or Torres Strait Islander staff and clinicians who have a better understanding of Indigenous wellbeing [64, 68]. Despite the growth of the Aboriginal and/or Torres Strait Islander health workforce over time, this expansion has not matched the Aboriginal and Torres Strait Islander population growth [69] and increasing incidence of chronic disease. Unsurprisingly, being members of the community, they serve, Aboriginal and/or Torres Strait Islander Health Workers play an essential and unique role in delivering culturally safe and holistic care. However, a demanding work environment, low salary, inadequate support, [70] and demanding cultural brokerage with non-Indigenous colleagues [70, 71] contribute to burnout that contributes to poor retention rates of Aboriginal and Torres Strait Islander primary care staff. This requires urgent attention, by individual primary care providers and through the National Aboriginal and Torres Strait Islander Health Workforce Strategic Framework and Implementation Plan 2021 – 2031 [72]. Given the ongoing need for the non-Indigenous workforce in fulfilling workforce gaps required to deliver services for Aboriginal and Torres Strait Islander people, building cultural competence, continuing appropriate training and education pathways and strategies, providing job security and adequate remuneration are also crucial to address primary care workforce issues including the overburdening of the Aboriginal and Torres Strait Islander workforce [58, 71, 73]. Our findings highlight the need to develop the overall chronic disease workforce, with a specific focus for recruitment and retention of Aboriginal and Torres Strait Islander Health Workers and Practitioners and providing cultural safety training for all non-Indigenous staff. Alongside this, mechanisms for recognising the value and load of cultural mentorship/education should be developed. This reflects a recent research findings that showed 39% of Aboriginal and/or Torres Strait Islander workers (n = 1033) across Australia experienced high cultural load in terms of extra work demands and their engagement in educating others [74].
Chronic disease management requires multidisciplinary team input for effective care delivery [75]. When optimally resourced, primary care can serve a coordinating role in patient care, and effectively ensure patients have access to all allied health and specialist care they need [76]. Therefore, in order to engage Aboriginal and Torres Strait Islander people with chronic disease care and maintain continuity of care, there needs to be established, streamlined, and practitioner and patient friendly systems in place [76, 77]. Existing evidence also documented inadequate number of general practitioners and lack of specialists in rural and remote settings of Australia compared to urban or city areas which hinders individuals, particularly Aboriginal and Torres Strait Islander people, to receive timely treatment for their co-occurring conditions in an integrated care approach [78, 79]. A lack of integrated IT systems, poor infrastructure, and poor communication between primary care team members were found in this review to impede provision of such care. It is evident that strategies like GP care plans and tertiary care follow up are important sources of information for primary care providers, hospitals and patients which are supported by IT infrastructure [80]. Previous research highlighted the feasibility of system integration through utilising continuous quality improvement processes and community co-design [81]. Infrastructure investment such as internet access, in-house IT support and automated systems for follow-up care, is urgently required to ensure that patients who do present or engage with primary care in regional or remote settings, are retained in the system to enable coordinated access to the multidisciplinary care required for chronic disease management. Moreover, rapidly evolving technology such as tele-health, videoconferencing and Point-of-Care Testing may can facilitate access to the Aboriginal and Torres Strait Islander people in remote and rural areas. However, implementing these tools should be part of broader strategy rather than a substitute for solving problems faced by PHC such as workforce retention, undersupply or maldistribution issues [82]. Therefore, when implementing an integrated team care program [83] or any other integrated model of care, both barriers and facilitators identified herein should be applied to improve the continuity of care with considering the context.
Effective engagement of Aboriginal and Torres Strait Islander communities and their leadership in program design, delivery and evaluation of chronic disease programs is integral to improving Aboriginal and Torres Strait Islander health and increasing access to primary care services [84, 85]. Previous studies have identified the following factors that enable engagement with Aboriginal and Torres Strait Islander communities: employment of local Aboriginal health workforce; trust and relationships; Aboriginal and Torres Strait Islander leadership; availability of flexible services to address holistic needs of local communities; benefits of engagement in service design and delivery; cost of participation and recognition of local Aboriginal knowledge and cultural traditions on study design implementation and dissemination [84, 86,87,88]. These enablers align with those reported in health service research that engaged with Indigenous and marginalised communities in an international context [89]. Similarly, this review identified a range of impeding factors to engagement of Aboriginal and Torres Strait Islander people with primary health care. Key factors included: a fear or lack of trust on mainstream health facilities, lack of respect from health care providers, experiences of interpersonal and structural racism, lack of understanding of cultural differences to initiate an open discussion and a narrow concept of health that fails to consider the Aboriginal definition of health which is more comprehensive than the Western biomedical perspective of health that focuses on treating health conditions [90,91,92]. Evidence also shows that Aboriginal and Torres Strait Islander people in rural and remote communities do not have equitable access to PHC services, including lack of local available services to meet their holistic needs, inadequate infrastructure, high costs, long travel distance and insufficient workforce [59, 93]. Therefore, trustful, and culturally safe engagement of Aboriginal and Torres Strait Islander communities through all aspects of the program design, implementation and evaluation is essential to program success, and where possible, the Aboriginal Health Workforce and ACCHOs should be utilised.
Policy and practice recommendations: This study identified several policy and practice recommendations (Table 3) that need to be considered for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care. Our recommendations align with Australia’s Primary Health Care 10 Year Plan 2022–2032 ($632.8 million new investment) that has identified three streams of work: future focused health care; person-centred primary health care supported by funding reform; and integrated care, locally delivered [94].
Strengths and limitations
Strengths of the present study include (i) the generation of an evidence summary required to guide policy and practice is a short time frame, (ii) the application of iterative process from the design to completion of review with engagement of Aboriginal and Torres Strait Islander researchers and Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members, (iii) a quality appraisal of the included studies using Aboriginal and Torres Strait Islander Quality Appraisal Tool that privileges Aboriginal and Torres Strait Islander people’s ways of knowing, being, doing and (iv) interpretation of findings validated by Aboriginal and Torres Strait Islander knowledge champions.
One limitation of this review was that search was restricted to only two databases as the decision makers seek the evidence is a short period of time and were based on peer reviewed articles published in English language. We also acknowledge that the findings might not be comprehensive as the review was conducted in short timeframe, limitations in key words used and subjected to publication bias, as we omitted published program reports, grey literature, and policy guidelines from our inclusion criteria. Moreover, our search was limited to specific databases and terms, which could result in overlooking articles present in other databases or identified through alternate search terms. Despite these limitations, this review is Aboriginal and Torres Strait Islander researchers led that allowed Indigenous perspectives and knowledge to be integrated in the evidence synthesis; ensuring findings are meaningful for the broader sector.
Conclusion
This rapid review synthesises the barriers and enablers to designing and implementing chronic disease prevention and management programs for Aboriginal and Torres Strait Islander communities. While there is no one-size-fits-all approach to the heterogeneous Aboriginal and Torres Strait Islander communities, several policy and practice recommendations are broadly applicable to service providers. These include addressing social and cultural determinants of health, developing the Aboriginal and Torres Strait Islander and non-Indigenous chronic disease workforce, supporting multidisciplinary teams through strengthening clinical care pathways, and engaging Aboriginal and Torres Strait Islander communities in design and delivery of chronic disease prevention and management programs. This requires funding mechanisms and models of care that are flexible enough to account for local and individual context through policy and practice reforms. Moreover, enabling place-based partnerships to develop local and population-based strategies that align with community priories and aspiration is crucial for tackling increasing burden of chronic disease.
Availability of data and materials
All available materials are available as Additional material.
Change history
26 April 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12961-024-01140-8
Abbreviations
- ACCHOs:
-
Aboriginal Community Controlled Health Organisations
- MBS:
-
Medicare Benefits Schedule
- CVD:
-
Cardiovascular Disease
- CKD:
-
Chronic Kidney Disease
- PRISMA-P:
-
Preferred Reporting Items for Systematic Review and Meta-analysis Protocols
- STARR:
-
SelecTing Approaches for Rapid Reviews
References
Kairuz CA, Casanelia LM, Bennett-Brook K, Coombes J, Yadav UN. Impact of racism and discrimination on physical and mental health among Aboriginal and Torres Strait islander peoples living in Australia: a systematic scoping review. BMC Public Health. 2021;21(1):1302.
Penm, E., Cardiovascular disease and its associated risk factors in Aboriginal and Torres Strait Islander peoples 2004–05, 2008, Australian Institute of Health and Welfare: Canberra.
Cardiovascular disease, diabetes and chronic kidney disease-Australian facts: Aboriginal and Torres Strait Islander people 2015 [https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/cardiovascular-diabetes-chronic-kidney-indigenous/summary]
Australian Burden of Disease Study 2018-Key findings [https://www.aihw.gov.au/reports/burden-of-disease/burden-of-disease-study-2018-key-findings]
Swerissen H, Duckett S, Moran G. Mapping primary care in Australia. 2018. Grattan Institute. Available from: https://grattan.edu.au/wp-content/uploads/2018/07/906-Mapping-primary-care.pdf.
Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, race, and mortality in US states. Soc Sci Med. 2005;61(1):65–75.
Lavoie JG, Forget EL, Prakash T, Dahl M, Martens P, O’Neil JD. Have investments in on-reserve health services and initiatives promoting community control improved First Nations’ health in Manitoba? Soc Sci Med. 2010;71(4):717–24.
Thomas SL, Zhao Y, Guthridge SL, Wakerman J. The cost-effectiveness of primary care for Indigenous Australians with diabetes living in remote Northern Territory communities. Med J Aust. 2014;200(11):658–62.
Commonwealth of Australia, Department of the Prime Minister and Cabinet. Closing the Gap Prime Minister’s report 2017. Canberra: Department of the Prime Minister and Cabinet, 2017. Available at www.niaa.gov.au/sites/default/files/publications/ctg-report-2017.pdf.
Australian Institute of Health and Welfare 2023. Aboriginal and Torres Strait Islander Health Performance Framework: summary report July 2023. Canberra: AIHW. Viewed:17/07/2023.
The Royal Australian College of General Practitioners. Vision for general practice and a sustainable healthcare system. East Melbourne, Vic: RACGP, 2019. Available at www.racgp.org.au/advocacy/advocacy-resources/the-vision-for-general-practice/the-vision.
TOWARDS A NATIONAL PRIMARY HEALTH CARE STRATEGY: FULFILLING ABORIGINAL PEOPLES ASPIRATIONS TO CLOSE THE GAP.National Aboriginal Community Controlled Health Organisation, February 2009. https://www.naccho.org.au/publications-resources/.
Gibson O, Lisy K, Davy C, Aromataris E, Kite E, Lockwood C, Riitano D, McBride K, Brown A. Enablers and barriers to the implementation of primary health care interventions for Indigenous people with chronic diseases: a systematic review. Implement Sci. 2015;10:71.
Yadav UN, Smith M, Agostino J, Sinka V, Williamson L, Wyber R, Butler DC, Belfrage M, Freeman K, Passey M, et al. Understanding the implementation of health checks in the prevention and early detection of chronic diseases among Aboriginal and Torres Strait Islander people in Australia: a realist review protocol. BMJ Open. 2023;13(6): e071234.
Australian Institute of Health and Welfare. Indigenous-specific health checks during the COVID-19 pandemic. https://www.aihw.gov.au/reports/indigenous-australians/indigenous-health-checks-during-the-covid-pandemic/contents/about
Follent D, Paulson C, Orcher P, O’Neill B, Lee D, Briscoe K, Dimopoulos-Bick TL. The indirect impacts of COVID-19 on Aboriginal communities across New South Wales. Med J Aust. 2021;214(5):199-200.e191.
Plüddemann A, Aronson JK, Onakpoya I, Heneghan C, Mahtani KR. Redefining rapid reviews: a flexible framework for restricted systematic reviews. BMJ Evid Based Med. 2018;23(6):201–3.
Pandor A, Kaltenthaler E, Martyn-St James M, Wong R, Cooper K, Dimairo M, O’Cathain A, Campbell F, Booth A. Delphi consensus reached to produce a decision tool for SelecTing approaches for rapid reviews (STARR). J Clin Epidemiol. 2019;114:22–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Lutschini M. Engaging with holism in Australian Aboriginal health policy–a review. Aust New Zealand Health Policy. 2005;2:15.
Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, Beaton A, Ehau T. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Glob Health. 2017;13(1):69.
National Indigenous Australians agency. Priority Reform One: Formal partnerships and shared decision-making. 2023 Commonwealth Closing the Gap Implementation Plan. [https://www.niaa.gov.au/2023-commonwealth-closing-gap-implementation-plan].
Naylor C, Charles A. Place-based partnerships explained. The King's Fund. 2022 [https://www.kingsfund.org.uk/publications/place-based-partnerships-explained].
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org.
Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, Beaton A, Ehau T. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Global Health. 2017;13(1):69.
Davy C, Harfield S, McArthur A, Munn Z, Brown A. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health. 2016;15(1):163.
Harfield S, Pearson O, Morey K, Kite E, Canuto K, Glover K, Gomersall JS, Carter D, Davy C, Aromataris E, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol. 2020;20(1):79.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Martin K, Mirraboopa B. Ways of knowing, being and doing: A theoretical framework and methods for indigenous and indigenist re‐search. J Aus Stud. 2003;27(76):203–214.
Askew DA, Togni SJ, Schluter PJ, Rogers L, Egert S, Potter N, Hayman NE, Cass A, Brown ADH. Investigating the feasibility, acceptability and appropriateness of outreach case management in an urban Aboriginal and Torres strait Islander primary health care service: a mixed methods exploratory study. BMC Health Serv Res. 2016;16:178.
Bailie J, Schierhout G, Laycock A, Kelaher M, Percival N, O’Donoghue L, McNeair T, Bailie R. Determinants of access to chronic illness care: a mixed-methods evaluation of a national multifaceted chronic disease package for Indigenous Australians. BMJ Open. 2015;5(11): e008103.
Canuto K, Wittert G, Harfield S, Brown A. “I feel more comfortable speaking to a male”: Aboriginal and Torres Strait Islander men’s discourse on utilizing primary health care services. Int J Equity Health. 2018;17(1):185.
Deshmukh T, Abbott P, Reath J. 'It’s got to be another approach’: an Aboriginal health worker perspective on cardiovascular risk screening and education. Aust Fam Physician. 2014;43(7):475–8.
Bailie J, Laycock A, Matthews V, Bailie R. System-level action required for wide-scale improvement in quality of primary health care: synthesis of feedback from an interactive process to promote dissemination and use of aggregated quality of care data. Front Public Health. 2016;4:86.
Barrett E, Salem L, Wilson S, O’Neill C, Davis K, Bagnulo S. Chronic kidney disease in an Aboriginal population: a nurse practitioner-led approach to management. Aust J Rural Health. 2015;23(6):318–21.
Reeve C, Humphreys J, Wakerman J, Carroll V, Carter M, O’Brien T, Erlank C, Mansour R, Smith B. Community participation in health service reform: the development of an innovative remote Aboriginal primary health-care service. Aust J Prim Health. 2015;21(4):409–16.
Davy C, Kite E, Sivak L, Brown A, Ahmat T, Brahim G, Dowling A, Jacobson S, Kelly T, Kemp K, et al. Towards the development of a wellbeing model for aboriginal and Torres Strait islander peoples living with chronic disease. BMC Health Serv Res. 2017;17(1):659.
Blignault I, Norsa L, Blackburn R, Bloomfield G, Beetson K, Jalaludin B, Jones N. “You Can’t Work with My People If You Don’t Know How to”: Enhancing Transfer of Care from Hospital to Primary Care for Aboriginal Australians with Chronic Disease. Int J Environ Res Public Health. 2021;18(14):7233.
Bailie J, Matthews V, Laycock A, Schultz R, Burgess CP, Peiris D, Larkins S, Bailie R. Improving preventive health care in Aboriginal and Torres Strait Islander primary care settings. Global Health. 2017;13(1):48.
Seear KH, Atkinson DN, Henderson-Yates LM, Lelievre MP, Marley JV. Maboo wirriya, be healthy: community-directed development of an evidence-based diabetes prevention program for young Aboriginal people in a remote Australian town. Eval Program Plann. 2020;81: 101818.
Seear KH, Atkinson DN, Lelievre MP, Henderson-Yates LM, Marley JV. Piloting a culturally appropriate, localised diabetes prevention program for young Aboriginal people in a remote town. Aust J Prim Health. 2019;25(5):495–500.
Spurling GK, Bond CJ, Schluter PJ, Kirk CI, Askew DA. 'I’m not sure it paints an honest picture of where my health’s at’—identifying community health and research priorities based on health assessments within an Aboriginal and Torres Strait Islander community: a qualitative study. Aust J Prim Health. 2017;23(6):549–53.
Stoneman A, Atkinson D, Davey M, Marley JV. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal community controlled health services. BMC Health Serv Res. 2014;14:481.
Webster E, Johnson C, Kemp B, Smith V, Johnson M, Townsend B. Theory that explains an Aboriginal perspective of learning to understand and manage diabetes. Aust N Z J Public Health. 2017;41(1):27–31.
Wood AJ, Graham S, Boyle JA, Marcusson-Rababi B, Anderson S, Connors C, McIntyre HD, Maple-Brown L, Kirkham R. Incorporating Aboriginal women’s voices in improving care and reducing risk for women with diabetes in pregnancy—a phenomenological study. BMC Pregnancy Childbirth. 2021;21(1):624.
Woods C, Carlisle K, Larkins S, Thompson SC, Tsey K, Matthews V, Bailie R. Exploring systems that support good clinical care in indigenous primary health-care services: a retrospective analysis of longitudinal systems assessment tool data from high-improving services. Front Public Health. 2017;5:45.
Sebastian S, Thomas DP, Brimblecombe J, Arley B, Cunningham FC. Perceived impact of the characteristics of the Indigenous Queensland B.strong brief intervention training program on uptake and implementation. Health Promot J Austr. 2022;33(1):245–56.
Kirkham R, Trap-Jensen N, Boyle JA, Barzi F, Barr ELM, Whitbread C, Van Dokkum P, Kirkwood M, Connors C, Moore E, et al. Diabetes care in remote Australia: the antenatal, postpartum and inter-pregnancy period. BMC Pregnancy Childbirth. 2019;19(1):389.
Cuesta-Briand B, Saggers S, McManus A. “It still leaves me sixty dollars out of pocket”: experiences of diabetes medical care among low-income earners in Perth. Aust J Prim Health. 2014;20(2):143–50.
Govil D, Lin I, Dodd T, Cox R, Moss P, Thompson S, Maiorana A. Identifying culturally appropriate strategies for coronary heart disease secondary prevention in a regional Aboriginal Medical Service. Aust J Prim Health. 2014;20(3):266–72.
Kirkham R, Boyle JA, Whitbread C, Dowden M, Connors C, Corpus S, McCarthy L, Oats J, McIntyre HD, Moore E, et al. Health service changes to address diabetes in pregnancy in a complex setting: perspectives of health professionals. BMC Health Serv Res. 2017;17(1):524.
Macniven R, Gwynn J, Fujimoto H, Hamilton S, Thompson SC, Taylor K, Lawrence M, Finlayson H, Bolton G, Dulvari N, et al. Feasibility and acceptability of opportunistic screening to detect atrial fibrillation in Aboriginal adults. Aust N Z J Public Health. 2019;43(4):313–8.
Conway J, Tsourtos G, Lawn S. The barriers and facilitators that indigenous health workers experience in their workplace and communities in providing self-management support: a multiple case study. BMC Health Serv Res. 2017;17(1):319.
Schmidt B, Campbell S, McDermott R. Community health workers as chronic care coordinators: evaluation of an Australian Indigenous primary health care program. Aust N Z J Public Health. 2016;40(Suppl 1):S107-114.
Campbell S, Roux N, Preece C, Rafter E, Davis B, Mein J, Boyle J, Fredericks B, Chamberlain C. Paths to improving care of Australian Aboriginal and Torres Strait Islander women following gestational diabetes. Prim Health Care Res Dev. 2017;18(6):549–62.
Saurman E. Improving access: modifying Penchansky and Thomas’s theory of access. J Health Serv Res Policy. 2016;21(1):36–9.
Davy C, Cass A, Brady J, DeVries J, Fewquandie B, Ingram S, Mentha R, Simon P, Rickards B, Togni S, et al. Facilitating engagement through strong relationships between primary healthcare and Aboriginal and Torres Strait Islander peoples. Aust N Z J Public Health. 2016;40(6):535–41.
Jongen C, McCalman J, Campbell S, Fagan R. Working well: strategies to strengthen the workforce of the Indigenous primary healthcare sector. BMC Health Serv Res. 2019;19(1):910.
Nolan-Isles D, Macniven R, Hunter K, Gwynn J, Lincoln M, Moir R, Dimitropoulos Y, Taylor D, Agius T, Finlayson H, et al. Enablers and Barriers to Accessing Healthcare Services for Aboriginal People in New South Wales, Australia. Int J Environ Res Public Health. 2021;18(6):3014.
Christidis R, Lock M, Walker T, Egan M, Browne J. Concerns and priorities of Aboriginal and Torres Strait Islander peoples regarding food and nutrition: a systematic review of qualitative evidence. Int J Equity Health. 2021;20(1):220.
Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18):E474-e483.
Markwick A, Ansari Z, Sullivan M, Parsons L, McNeil J. Inequalities in the social determinants of health of Aboriginal and Torres Strait Islander People: a cross-sectional population-based study in the Australian state of Victoria. Int J Equity Health. 2014;13(1):91.
Australian Institute of Health and Welfare (2022). Australia’s health 2022: in brief, catalogue number AUS 241. Australia’s health series number 18, AIHW, Australian Government. https://www.aihw.gov.au/reports/australias-health/australias-health-2022-in-brief/summary.
Hayman N. Strategies to improve indigenous access for urban and regional populations to health services. Heart Lung Circ. 2010;19(5–6):367–71.
Purdie P., Dudgeon P., Walker R. Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. 2nd ed. Australian Government Department of the Prime Minister and Cabinet. ACT; Canberra, Australia: 2014.
Kelly J, Dwyer J, Willis E, Pekarsky B. Travelling to the city for hospital care: access factors in country Aboriginal patient journeys. Aust J Rural Health. 2014;22(3):109–13.
Moore L, Britten N, Lydahl D, Naldemirci Ö, Elam M, Wolf A. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand J Caring Sci. 2017;31(4):662–73.
McGrath PD, Patton MA, Ogilvie KF, Rayner RD, McGrath ZM, Holewa HA. The case for Aboriginal health workers in palliative care. Aust Health Rev. 2007;31(3):430–9.
Lahn J., Puszka S., Lawton P., Dinku Y., Nichols N. and Markham F. (2020) Beyond Parity in Aboriginal and Torres Strait Islander Health Workforce Planning: Achieving Equity through Needs-Based and Strengths-Based Approaches, Commissioned Report No. 6, Centre for Aboriginal Economic Policy Research, Australian National University. https://doi.org/10.25911/5f88175975c5b
Lai GC, Taylor EV, Haigh MM, Thompson SC. Factors Affecting the retention of indigenous Australians in the health workforce: a systematic review. Int J Environ Res Public Health. 2018;15(5):914.
Gwynne K, Lincoln M. Developing the rural health workforce to improve Australian Aboriginal and Torres Strait Islander health outcomes: a systematic review. Aust Health Rev. 2017;41(2):234–8.
Australian Government Department of Health . National Aboriginal and Torres Strait Islander Health Workforce Strategic Framework and Implementation Plan 2021–2031. Available from: https://www.health.gov.au/sites/default/files/documents/2022/03/national-aboriginal-and-torres-strait-islander-health-workforce-strategic-framework-and-implementation-plan-2021-2031.pdf. In.
McCalman J, Campbell S, Jongen C, Langham E, Pearson K, Fagan R, Martin-Sardesai A, Bainbridge R. Working well: a systematic scoping review of the Indigenous primary healthcare workforce development literature. BMC Health Serv Res. 2019;19(1):767.
Diversity Council Australia/Jumbunna Institute (Brown, C., D’Almada-Remedios, R., Gilbert, J. O’Leary, J. and Young, N.) Gari Yala (Speak the Truth): Centreing the Work Experiences of Aboriginal and/or Torres Strait Islander Australians, Sydney, Diversity Council Australia/Jumbunna Institute, 2020.
Harris MF, Jayasinghe UW, Taggart JR, Christl B, Proudfoot JG, Crookes PA, Beilby JJ, Davies GP. Multidisciplinary team care arrangements in the management of patients with chronic disease in Australian general practice. Med J Aust. 2011;194(5):236–9.
Digital technologies and chronic disease management. Australian Journal for General Practitioners 2014, 43:842-846.
Michielsen L, Bischoff EWMA, Schermer T, Laurant M. Primary healthcare competencies needed in the management of person-centred integrated care for chronic illness and multimorbidity: results of a scoping review. BMC Primary Care. 2023;24(1):98.
Street TD, Somoray K, Richards GC, Lacey SJ. Continuity of care for patients with chronic conditions from rural or remote Australia: a systematic review. Aust J Rural Health. 2019;27(3):196–202.
Comorbidity Guidelines. Rural and remote populations [https://comorbidityguidelines.org.au/part-c-specific-population-groups/rural-and-remote-populations#:~:text=The%20lack%20of%20specialists%20in%20rural%20and%20remote,of%20employed%20medical%20practitioners%20decreasing%20according%20to%20remoteness.]
Trankle SA, Usherwood T, Abbott P, Roberts M, Crampton M, Girgis CM, Riskallah J, Chang Y, Saini J, Reath J. Integrating health care in Australia: a qualitative evaluation. BMC Health Serv Res. 2019;19(1):954.
McCalman J, Bainbridge R, James YC, Bailie R, Tsey K, Matthews V, Ungar M, Askew D, Fagan R, Visser H, et al. Systems integration to promote the mental health of Aboriginal and Torres Strait Islander children: protocol for a community-driven continuous quality improvement approach. BMC Public Health. 2020;20(1):1810.
Thomas SL, Wakerman J, Humphreys JS. Ensuring equity of access to primary health care in rural and remote Australia—what core services should be locally available? Int J Equity Health. 2015;14(1):111.
Australian Government Department of Health and Aged Care. Integrated Team Care Program.
Durey A, McEvoy S, Swift-Otero V, Taylor K, Katzenellenbogen J, Bessarab D. Improving healthcare for Aboriginal Australians through effective engagement between community and health services. BMC Health Serv Res. 2016;16(1):224.
Banks E, Haynes A, Lovett R, Yadav UN, Agostino J. Output-orientated policy engagement: a model for advancing the use of epidemiological evidence in health policy. Health Res Policy Syst. 2023;21(1):6.
O’Brien P, Prehn R, Rind N, Lin I, Choong PFM, Bessarab D, Coffin J, Mason T, Dowsey MM, Bunzli S. Laying the foundations of community engagement in Aboriginal health research: establishing a community reference group and terms of reference in a novel research field. Res Involve Engage. 2022;8(1):40.
Barnett L, Kendall E. Culturally appropriate methods for enhancing the participation of Aboriginal Australians in health-promoting programs. Health Promot J Austr. 2011;22(1):27–32.
Bessarab D, Durey A, Christou A, Katzenellenbogen JM, Taylor K, Brankovich J. Evaluation of the South Metropolitan Health Service Community Engagement Process Perth: Curtin University. 2014.
Yadav UN, Lloyd J, Baral KP, Bhatta N, Mehata S, Harris M. Evaluating the feasibility and acceptability of a co-design approach to developing an integrated model of care for people with multi-morbid COPD in rural Nepal: a qualitative study. BMJ Open. 2021;11(1): e045175.
Kaihlanen A-M, Hietapakka L, Heponiemi T. Increasing cultural awareness: qualitative study of nurses’ perceptions about cultural competence training. BMC Nurs. 2019;18(1):38.
Askew DA, Foley W, Kirk C, Williamson D. “I’m outta here!”: a qualitative investigation into why Aboriginal and non-Aboriginal people self-discharge from hospital. BMC Health Serv Res. 2021;21(1):907.
Gee G, Dudgeon P, Schultz C, Hart A, Kelly K. Aboriginal and Torres Strait Islander Social and Emotional Wellbeing. In: Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2014.
Bywood P, Katterl R, Lunnay B. Disparities in primary health care utilisation: Who are the disadvantaged groups? How are they disadvantaged? What interventions work? Adelaide: Primary Health Care Research and Information Service (PHCRIS), Policy Issue Review; 2011.
Australian Government Department of Health. Future focused primary health care: Australia’s Primary Health Care 10 Year Plan 2022–2032. 2022.Canberra ACT 2601.
Acknowledgements
We are grateful for the support of Chelsea Liu assisted with the use of the Quality Appraisal Tool and the support of Dr. Deborah Wong (Research Coordinator- Chronic Disease | Cervical Cancer) in designing Fig. 2. We would also like to acknowledge Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members at the National Centre for Aboriginal and Torres Strait Islander Wellbeing Research at the Australian National University for their continuous feedback without which this research piece wouldn’t have been completed.
Disclaimer
The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of their affiliated institutions.
Funding
This work was supported by funding from the Australian Government Department of Health-—First Nations Health Division. The funding body had no role in the writing of this article.
Author information
Authors and Affiliations
Contributions
Conceptualization & original draft: Uday Narayan Yadav and Rosemary Wyber. Data curation: Uday Narayan Yadav, Jasmine Meredith Davis and Rosemary Wyber. Review, edits and revision: Uday Narayan Yadav, Jasmine Meredith Davis, Keziah Bennett-Brook, Julieann Coombes, Rosemary Wyber and Odette Pearson.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: an incorrectly inserted phrase during proofing was modified
Supplementary Information
Additional file 1.
Study characteristics.
Additional file 2.
Meta aggregated study findings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yadav, U.N., Davis, J.M., Bennett-Brook, K. et al. A rapid review to inform the policy and practice for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care. Health Res Policy Sys 22, 34 (2024). https://doi.org/10.1186/s12961-024-01121-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12961-024-01121-x