Abstract
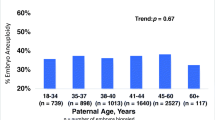
Although controversial, increasing paternal age has been shown to negatively affect assisted reproductive technology (ART) outcomes and success rates. Most studies investigating the effect of paternal age on ART outcomes use a donor oocyte model to minimize maternal aneuploidy contribution. This study sought to determine whether increasing paternal age is associated with adverse in vitro fertilization (IVF) outcomes when aneuploidy is minimized using preimplantation genetic screening. There were 573 single thawed euploid embryo transfers from 473 patients undergoing oocyte donor and autologous IVF cycles. Cycles were categorized according to paternal age at oocyte retrieval, and an age adjustment was performed for maternal age in order to evaluate for an isolated paternal age effect. Fertilization rate was found to decrease significantly with increasing paternal age (P =.04). After controlling for oocyte age, there was no significant difference in pregnancy outcomes across all paternal age categories after euploid embryo transfer, including implantation rate (P =.23), clinical pregnancy rate (P =.51), and spontaneous abortion rate (P =.55). Therefore, if a couple is able to produce and transfer a single thawed euploid embryo, no difference in IVF pregnancy outcomes is identified with increasing paternal age.
Similar content being viewed by others
References
Bellver J, Garrido N, Remohi J, Pellicer A, Meseguer M. Influence of paternal age on assisted reproduction outcome. Reprod Biomed Online. 2008;17(5):595–604. doi:10.1016/S1472-6483(10)60305-7.
Paulson RJ, Milligan RC, Sokol RZ. The lack of influence of age on male fertility. Am J Obstet Gynecol. 2001;184(5):818–822. doi: 10.1067/mob.2001.113852.
de la Rochebrochard E, de Mouzon J, Thepot F, Thonneau P. French National IVFRA. Fathers over 40 and increased failure to conceive: the lessons of in vitro fertilization in France. Fertil Steril. 2006;85(5):1420–1424. doi:10.1016/j.fertnstert.2005.11. 040.
Robertshaw I, Khoury J. Abdallah ME, Warikoo P, Hofmann GE. The effect of paternal age on outcome in assisted reproductive technology using the ovum donation model. Reprod Sci. 2014; 21(5):590–593. doi:10.1177/1933719113506497.
Frattarelli JL, Miller K, Miller BT, Elkind-Hirsch K, Scott R. Jr. Male age negatively impacts embryo development and reproductive outcome in donor oocyte assisted reproductive technologies. Fertil Steril. 2008;90(1):97–103. doi:10.1016/j.fertnstert. 2007.06.009.
Agarwal A, Said TM. Role of sperm chromatin abnormalitie, and DNA damage in male infertility. Hum Reprod Update. 2003;(9): 331–345. doi:10.1093/humupd/dmg027.
Moskovtsev SI, Willis J, Mullen BM. Age-related decline in sperm deoxyribonucleic acid integrity in patients evaluated for male infertility. Fertil Steril. 2006;85(2):496–499. doi:10.1016/j.fertnstert.2005.05.075.
Brahem S, Mehdi M, Elghezal H, Saad A. The effects of male aging on semen quality, sperm DNA. fragmentation and chromosomal abnormalities in an infertile population. J Assist Reprod Genet. 2011;28:425–432. doi:10.1007/s10815-011-9537-5.
Rosenbusch BE. Cytogenetics of human spermatozoa: what about the reproductive relevance of structural chromosome aberrations? J Assist Reprod Genet. 1995;12(6):375–383. doi:10.1007/BF02215729.
Sartorelli EM, Mazzucatto LF, de Pina-Neto JM. Effect of paternal age on human sperm chromosomes. Fertil Steril. 2001;76(6):1119–1123. doi:http://dx.doi.org/10.1016/S0015-0282(01)02894-1.
Garcia-Ferrayra J, Luna D, Villegas L, et al. High aneuploidy rates observed in embryos derived from donated oocytes are related to male aging and high percentages of sperm DNA. fragmentation. Clin Med Insights Reprod Health. 2015;9:21–27. doi:10.4137/CMRH.S32769.
Vagnini L, Baruffi RL, Mauri AL, et al. The effects of male age of sperm DNA damage in an infertile population. Reprod Biomed Online. 2007;15:514–519. doi:10.1016/S1472-6483(10)60382-3.
Lopes S, Jurisicova A, Sun JG, Casper RF. Reactive oxygen species: potential caus, for DNA fragmentation in human spermatozoa. Hum Reprod. 1998;13:896–900. PMID: 9619544.
Morris ID, Ilott S, Dixon L, Brison DR. The spectru, of DNA damage in human sperm assessed by single cell gel electro-phoresis (Comet assay) and its relationship to fertilization and embryo development. Hum Reprod. 2002;17:990–998. PMID: 11925396.
Gandini L, Lombardo F, Paoli D, et al. Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod. 2004;19:1409–1417. doi:10.1093/humrep/ deh233.
Luna M, Finkler E, Barritt J, et al. Paternal age and assisted reproductive technology outcome in ovum recipients. Fertil Steril. 2009; 92:1772–1775. doi:10.1016/j.fertnstert.2009.05.036.
Braude P, Bolton V, Moore S. Human gene expression first occurs between the four- and eight-cell stages of preimplanta-tion development. Nature. 1988;332:459–461. doi:10.1038/ 332459a0.
Duncan FE, Hornick JE, Lampson MA, Schultz RM, Shea LD, Woodruff TK. Chromosome cohesion decreases in human eggs with advanced maternal age. Aging Cell. 2012;11:1121–1124. doi:10.1111/j.1474-9726.2012.00866.x.
Palermo G, Munné S, Cohen J. The human zygote inherits its mitotic potential from the male gamete. Hum Reprod. 1994;9: 1220–1225. PMID: 7962421.
Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012; 488:471–475. doi:10.1038/nature11396.
Jenkins TG, Aston KI, Meyer T, Carrell DT. The sperm epigenome, male aging, and potential effects on the embryo. Adv Exp Med Biol. 2015:81–93. doi:10.1007/978-3-319-18881-2_4.
Sagi-Dain L, Sagi S, Dirnfeld M. Effect of paternal age on reproductive outcomes in oocyte donation model: a systematic review. Fertil Steril. 2015;104(4):857–865. doi:10.1016/j.fertnstert.2015. 06.036.
Harton GL, Munne S, Surrey M, et al; PGD Practitioners Group. Diminished effect of maternal age on implantation after preim-plantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100(6):1695–1703. doi:10. 1016/j.fertnstert.2013.07.2002.
Grifo JA, Hodes-Wertz B, Lee HL, Amperloquio E, Clarke-Williams M, Adler A. Single thawed euploid embryo transfe, improves IV pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J Assist Reprod Genet. 2013;30(2):259–264. doi:10.1007/ s10815-012-9929-1.
Gutiérrez-Mateo C, Colls P. Sánchez-Garcia J, et al. Validation of microarray comparative genomic hybridization for comprehensive chromosome analysis of embryos. Fertil Steril. 2011;95: 953–958. doi:10.1016/j.fertnstert.2010.09.010.
Haddad G, Deng M, Wang CT. et al. Assessment of aneuploidy formation in human blastocysts resulting from donated eggs and the necessity of the embryos for aneuploidy screening. J Assist Reprod Genet. 2015;31(6):999–1006. doi:10.1007/s10815-015-0492-4.
Garcia-Velasco JA, Isaza V, Caligara C, Pellicer A, Remohi J, Simon C. Factors that determine discordant outcome from shared oocytes. Fertil Steril. 2003;80(1):54–60. doi:http://dx.doi.org/10.1016/S0015-0282(03)00545-4.
Reig-Viader R, Capilla L, Vila-Cejudo M, et al. Telomere homeostasis is compromised in spermatocytes from patients with idio-pathic infertility. Fertil Steril. 2014;102(3):728–738. doi:10.1016/j.fertnstert.2014.06.005.
Allsopp RC, Vaziri H, Patterson C, et al. Telomere length predicts replicative capacity of human fibroblasts. Proc Natl Acad Sci USA. 1992;89:10114–10118. PMID: 1438199.
Aston KI, Hunt SC, Susser E, et al. Divergence of sperm and leukocyte age-dependent telomere dynamics: implications for male-driven evolution of telomere length in humans. Mol Hum Reprod. 2012;18:517–522. doi:10.1093/molehr/gas028.
Baird DM, Britt-Compton B, Rowson J. Amso NN, Gregory L, Kipling D. Telomere instability in the male germline. Hum Mol Genet. 2006;15:45–51. doi:10.1093/hmg/ddi424.
Atunes DMF, Kalmback KH, Wang F, et al. A single-cell assay for telomere DNA content shows increasing telomere length heterogeneity, as well as increasing mean telomere length in human spermatozoa with advancing age. J Assist Reprod Genet. 2015;32: 1685–1690. doi:10.1007/s10815-015-0574-3.
Franasiak JM, Forman EJ, Hong KH, et al. The nature of aneu-ploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101(3):656–663. doi:10.1016/j.fertnstert.2013.11.004.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tiegs, A.W., Sachdev, N.M., Grifo, J.A. et al. Paternal Age Is Not Associated With Pregnancy Outcomes After Single Thawed Euploid Blastocyst Transfer. Reprod. Sci. 24, 1319–1324 (2017). https://doi.org/10.1177/1933719116687660
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719116687660