Abstract
Checkpoint inhibitors are being added to standard-of-care chemotherapy in multiple clinical trials. Success has been reported in non–small and small cell lung carcinomas and urothelial, head and neck, gastric, and esophageal cancers, and promising results are already available in triple-negative breast and pancreatic malignancies. The potential mechanisms of synergy include immunogenic tumor cell death, antiangiogenesis, selective depletion of myeloid immunosuppressive cells, and lymphopenia, which reduces regulatory T cells and makes room for proliferation of effector T cells. However, chemotherapy regimens have not been optimized for such combinations, perhaps explaining some recent clinical trial disappointments. Approaches to make the most of chemoimmunotherapy include neoadjuvant and adjuvant schemes.
Significance: Immunotherapy of cancer based on PD-1/PD-L1 blockade has prompted a revolution in cancer clinical management. Evidence in phase III clinical trials already supports combinations of immunotherapy with standard-of-care chemotherapy for a number of malignant diseases. This review focuses on such evidence and provides an overview of the potential synergistic mechanisms of action and the opportunities to optimize chemoimmunotherapy regimens.
Cancer Chemotherapy
Finding the Achilles' heel of metastatic cancer is a formidable task. The first pharmacologic answer comes from the search for chemicals that would selectively damage replicating cells. Compounds achieving such an effect mainly include DNA-damaging agents, those interfering with the DNA enzymatic replicative machinery, and those impairing nucleotide synthesis or mitotic mechanisms. The development of chemotherapy started in the 1950s with remarkable success for Hodgkin lymphoma (1), testicular cancer (2), and acute lymphoid leukemia (3). Curative effects against such diseases were discovered with the realization that synergistic combinations of several drugs were required, and that efficacy comes at the cost of significant toxicity. Over the years, cytotoxic compounds for cancer therapy have been developed in an empiric quest to attain survival advantage for patients in myriads of disease-by-disease clinical trial efforts.
Unfortunately, for the most prevalent epithelial solid malignancies at metastatic stages, chemotherapy at its best offers only modest prolongation of survival. Indeed, the best effects of chemotherapy are obtained when it is delivered in a complementary fashion to radical surgery, either before the operation (neoadjuvant treatment) or after surgery (adjuvant treatment).
Cellular biology observations indicate that most chemotherapy agents in the clinic ultimately trigger the proapoptotic suicidal machinery of cancer cells. However, resistance mechanisms are most often induced as a result of the expression of multidrug transporters that pump out the chemicals, and genetic and epigenetic adaptations to the selective Darwinian pharmacologic pressure.
The current state of the art is that aggressive and poorly tolerated chemotherapy schemes are instigated in induction and maintenance regimens until radiologic cancer progression involving tumor masses thriving or newly appearing in spite of treatment. Doses and intervals have been chosen under the maximal tolerated dose paradigm. More recently, therapies to attain selective chemotherapy by nano-formulated drugs such as albumin-conjugated taxanes (nab-paclitaxel) or the liposomal formulation of anthracyclines (liposomal doxorubicin), or antibody–drug conjugates (ADC; such as TDM-1) have been developed. In line with this, tumor selectivity of the ADC can be further attained by optimized linkers that release the chemotherapy moiety selectively in the tumor cell context, as in the case of trastuzumab-deruxtecan (4), or by protease activatable precursor forms of the antibodies (probodies) conjugated to chemotherapy agents (5).
Unfortunately, despite its potency, chemotherapy largely lacks a bystander tumor-killing effect, and escape and resistance are most frequently possible for the remaining malignant cells at tolerable doses. Paradoxically, full-dose chemotherapy is known to affect replicating immune system cells. Indeed, chemotherapy at high doses can cause immunosuppression (6), and drugs that were originally devised to treat cancer are currently mainly used for autoimmune disorders or to prevent allograft rejection. Nonetheless, a therapeutic window exists that contradicts the dogmatic interpretation that was taught until recently in medical school classrooms, stating that the mechanisms targeted by chemotherapy were exactly the same as those required for adaptive immune responses, which are dependent on clonal lymphocyte expansions.
Mechanisms
Following obscure years of intensive research to harness the power of the cytotoxic immune response against cancer, we are witnessing a revolution in cancer therapeutics exploiting the tumor recognition and destruction capabilities of the immune system. Two approaches have yielded unprecedented success: checkpoint inhibitors (7) and adoptive T-cell therapy with chimeric antigen receptors for B cell–derived malignancies (8). Importantly, the most striking therapeutic effects of checkpoint inhibitors have been observed upon combination with chemotherapy or antiangiogenic drugs, whereas adoptive T-cell therapy requires preconditioning regimens of non-myeloablative chemotherapy or total body irradiation (9, 10). A summary of the main mechanisms at the interface of chemotherapy and immunotherapy is shown graphically in Fig. 1.
Postulated mechanisms of synergy between chemotherapy and immunotherapy. In the upper part, the pros and cons mechanisms of chemotherapy with regard to the immune response are depicted with emphasis on the fact that the pros must outbalance the cons. In the lower part, the main invoked mechanisms of action are schematically represented with the main supportive literature references. MDSC, myeloid-derived suppressor cell; Treg, regulatory T cell.
Postulated mechanisms of synergy between chemotherapy and immunotherapy. In the upper part, the pros and cons mechanisms of chemotherapy with regard to the immune response are depicted with emphasis on the fact that the pros must outbalance the cons. In the lower part, the main invoked mechanisms of action are schematically represented with the main supportive literature references. MDSC, myeloid-derived suppressor cell; Treg, regulatory T cell.
Tumor Debulking by Chemotherapy
Tumor masses are active producers of immunosuppressive substances that inhibit immune responses systemically (11). Hence, any treatment that would cause tumor tissue debulking (surgery, chemotherapy, or radiotherapy) may have a beneficial impact on the overall antitumor immune response and its efficacy (12). Additionally, the bulk and numbers of tumor cells to be cleared by the immune system are likely to have limitations. Reducing tumor mass leaves fewer tumor cells to be cleared by the immune system, thereby also reducing the chances for immunoescape variants.
Immunogenic Cell Death: Chemotherapy Meets Immunology
Apoptosis was perceived as an immunologically silent form of cell death and turnover. However, the group of G. Kroemer realized that tumor cells apoptotically killed under the influence of certain chemotherapeutic drugs or ionizing radiation vaccinated mice against a subsequent lethal inoculi of viable tumor cells (13). Such ensuing immunity is mainly dependent on CD8 T lymphocytes (13). Incisive research on the mechanisms underlying these effects concluded that the immunogenicity of cell death is a function of premortem reticular stress (14) and release of tissue damaging–denoting substances (alarmins) that alert the immune system. Ultimately, tumor cell debris uptake by professional antigen-presenting dendritic cells and their activation/maturation state seem to determine the immune outcome (15). Several hallmarks of immunogenic cell death have been proposed, including exposure of calreticulin on the outer cell surface; release of ATP, Annexin-1, and HMGB1; autophagy; inflammasome activation; induction of type 1 IFN signaling, and release of mitochondrial formyl peptides (16). Interestingly, in vivo or in vitro measurements of such hallmark mechanisms allow drugs to be ranked as inducers of immunogenic cell death (17, 18). It must be acknowledged that most of the evidence corresponds to imperfect mouse models and to correlative studies in human cell line samples. Ultimately, the contribution of these mechanisms needs to be addressed in patient tissues under treatment. An excellent recent review summarizes specific knowledge on immunogenic cell death and immune mechanisms elicited in mouse models by anticancer agents, listing most conventional chemotherapy drugs (18).
The postulated train of events in immunogenic cell death includes release of antigens from the dying or dead cells that is taken up, processed, and presented by specialized antigen-presenting cells termed conventional type 1 dendritic cells (cDC1). Maturation/activation of such cDC1 cells is induced by factors released by the surrounding stressed cells under the influence of toxics. Such phenomena are collectively termed as cross-priming of tumor antigens (19), but it must be acknowledged that formal experimental proof for chemotherapy-enhanced tumor antigen cross-priming in humans remains to be published.
The most exploitable consequence of these immunogenic cell death phenomena is that chemotherapy may result in mechanisms that unleash immunity to tackle malignant cells that could be intrinsically resistant to the chemotherapeutic agent. Nonetheless, the most immunogenic form of cell death is probably far less immunogenic than the immunogenicity following detection of microbial presence (20). Microbial moieties detected by innate pathogen recognition receptors are the physiologic triggers of immunity. Therefore, further combination with locally given or systemically delivered TLR agonists, STING agonists, or virotherapy could be advisable to make the most of the proimmune effects of chemotherapy (21). Of note, off-target effects of chemotherapy may provide adjuvanticity to raise the immunogenicity of tumor antigens, for instance, the reported TLR4 agonist activity of paclitaxel (22).
Depletion of Myeloid-Derived Suppressor Cells, Cancer-Associated Neutrophils, and Macrophages
Not all cells of the immune system fight cancer. In fact, there are leukocyte populations that depress cytotoxic antitumor immunity. Tumors favor a form of leukocyte hematopoiesis that yields myeloid cells phenotypically similar to immature macrophages and neutrophils that in culture and in vivo dampen antitumor T-cell immunity (23, 24). Such myeloid-derived suppressor cells (MDSC) are known to be sensitive to chemotherapeutic agents in mice and humans, which include platinum compounds and DNA alkylating agents (25, 26). The mechanisms that such immunosuppressive myeloid cells deploy to impair T-cell function are multifarious, encompassing production of growth and proangiogenic factors, T-cell damaging enzymatic functions, and neutrophil extracellular trap formation, among others. For instance, cancer vaccines are more effective under the influence of cyclophosphamide or platinum-based regimens (25, 26), because of attenuation of MDSC. Of note, gemcitabine and 5-FU are also reported to effectively deplete MDSCs (27, 28). Intratumoral macrophages with transcriptomic features conceptualized as M2 are clearly protumoral, whereas those conceptualized as M1 may mediate antitumor function. Chemotherapy drugs such as cyclophosphamide and doxorubicin reportedly favor M1 differentiation (29). Another possible explanation is that by damaging or killing malignant cells, chemotherapeutic drugs downregulate or reduce factors derived from tumor cells that otherwise may favor M2 differentiation, thereby potentially acting through indirect effects.
Tumors promote the formation of tumor-supportive myeloid leukocytes with growth factors (i.e., GM-CSF, G-CSF, M-CSF, HGF, etc.) and attraction with chemokines (i.e., CXCL1, CXCL8, CCL2, etc.; refs. 24, 30). Ironically, the frequently prescribed recombinant G-CSF to treat or prevent chemotherapy-induced neutropenia is likely to be deleterious for the proimmune effects of chemotherapy.
Homeostatic Proliferation of Effector T Cells, and Treg Depletion
T lymphocytes enter the cell cycle as a result of two types of stimuli. On the one hand, cognate antigen recognition spurs rapid clonal expansion, while on the other hand, T-cell numbers are homeostatically maintained by a competition for promitotic growth factors such as IL7 and IL15. Accordingly, lymphopenia results in homeostatic proliferation of antigen-naïve and central memory T cells.
Hence, lymphotoxic chemotherapy might result in a paradoxical reshaping of the T-cell repertoire and the differentiation into tumor-attacking cytotoxic T cells. Of note, the window of doses and dose intervals becomes crucial, because too much chemotherapy would destroy lymphocytes undergoing expansion, but at optimal doses may foster specific immunity. This is best perceived in the context of adoptive T-cell therapy approaches, where chemotherapy drugs (usually cyclophosphamide and fludarabine) make room for homeostatic proliferation of adoptively infused cells (9). This mechanism is considered crucial, and efficacy has been correlated to the circulating levels of homeostatic cytokines and the achieved lymphopenia (9, 31).
Among T cells, a CD4+ subset is specialized at reducing the activation and expansion of effector T lymphocytes. Such a subset differentiates in the thymus and is driven by the transcription factor FOXP3. In cancer, such regulatory T cells (Treg) interfere with tumor immunity in mouse models, and their presence in the tumor microenvironment has been correlated with a poorer prognosis (32). Moreover, FOXP3+ Treg cell differentiation can be induced as a result of local factors in the tumor tissue microenvironment, such as TGFβ (33). Tregs are probably specific to self-antigens conferring a certain level of self-tolerance and are frequently engaged in the cell cycle. Interestingly, some chemotherapies such as cyclophosphamide seem to be selective to some extent at killing these FOXP3+ subpopulations (34). However, clinical studies have questioned whether cyclophosphamide could actually induce relevant levels of Treg depletion (35). Dosing and timing may be critical to the immunomodulatory effects of cyclophosphamide, and the concept of medium-dose intermittent chemotherapy has been suggested as optimal (36). In any case, cyclophosphamide is an imperfect Treg-depleting agent, and more precise and effective ways to target this immunosuppressive population are under clinical investigation.
All considered, predosing with low-dose cyclophosphamide is a common adjuvant procedure in experimental cancer vaccines (37). Treg depletion by chemotherapy is also likely to explain the favorable effects on lymphodepletion in TIL adoptive therapy. It must be remembered that efficient Treg depletion in tumor tissues is a pending issue in cancer immunotherapy. Of note, low-dose regimens of cyclophosphamide such as metronomic or oral schedules might derive their benefit from these immune-mediated mechanisms. Nonetheless, clinical proof for the efficacy of cyclophosphamide as an immunotherapy-potentiating tool remains to be established and is matter of debate.
Antiangiogenesis
Immunotherapy with PD-1/PD-L1–blocking checkpoint inhibitors induces striking clinical benefit upon combination with VEGF–VEGFR antagonists for metastatic renal cell carcinoma (RCC; refs. 38, 39) and hepatocellular carcinoma (HCC; ref. 40). Indeed, the multityrosine kinase inhibitor axitinib + pembrolizumab or avelumab and the combination of bevacizumab + atezolizumab are market-approved for first-line treatment of advanced RCC and HCC, respectively. These combined therapeutic mechanisms were originally translated to the clinic for melanoma by S. Hodi's team (41) and are related not only to angiogenesis inhibition, but also to the reshaping of myeloid populations and to VEGF effects on innate lymphocytes (42). Although VEGF–VEGFR-targeted inhibitors cannot be considered as chemotherapy, they illustrate the concept that antiangiogenesis in combination with immunotherapy may result in synergistic effects.
In this regard, proliferating vascular cells can be the prey of a variety of chemotherapeutic agents even at low metronomic doses (43) that thereby cause solid-tumor hypoxia and nutrient deprivation. This is a double-edged sword for cancer immunity. It is intriguing that a relative degree of hypoxia increases the activity of cytotoxic T cells (44) while it may also result in a more hostile myeloid cell environment (44). Furthermore, tissue penetration of T lymphocytes across endothelial barriers could be altered for the better or for the worse by chemotherapy pretreatment (42).
Disruption of the Gut Microbiome Barrier
The importance of the abundance and species composition of the gut microbiome for immunotherapy has been intensively studied and found to exert a significant effect on therapeutic outcomes in response to immunotherapies with potential for therapeutic interventions (45). Chemotherapy agents very actively destroying replicating enterocytes result in disruption of the gut mucosal barrier leading to bacilli and microbial biomolecules that reach otherwise sterile tissues (46). Such barrier disruption is also induced by total body irradiation and may exert important effects on cancer immunity, in part depending on the control of the maturation state of dendritic cells even if they are located distant from the gut (47).
It is worth mentioning that chemotherapy often causes febrile neutropenia as a side effect that is frequently treated with broad-spectrum antibiotics, which severely modify the gut microbiota. When considering the potential effects on concomitant immunotherapy, this could be deleterious, neutral, or favorable with regard to antitumor effects. These phenomena deserve attention in chemoimmunotherapy trials and will most probably be deleterious for patients' outcomes (48).
Recently, attention has focused on the presence of bacteria or their nucleic acids in tumor lesions, particularly in metastasis from digestive cancers (49, 50). It would not be surprising that such levels of microbial colonization could be increased by chemotherapy drugs, thereby exerting anticancer or procancer immune effects.
Deleterious Effects of Chemotherapy on Immunity
High-dose chemotherapy beyond a poorly understood threshold results in overall immune functional depression (51). This is presumably the result of elimination of anticancer effector components or the demise of stem-like T cells able to restore the antigen-recognition repertoire. Such an undesirable effect may come from dose levels and continuous dosing without intervals for immune recovery. Certainly, dose and schedules of chemotherapy have not been chosen for being immune system-friendly.
For instance, in an attempt to deal with these immunosuppressive side effects, strategies of extraction, expansion, preservation, and reinfusion of polyclonal peripheral blood T cells have been clinically tested in patients undergoing chemotherapy to improve overall immunocompetence and tumor immune responsiveness (52). These approaches might be especially suitable for combination with checkpoint inhibitors.
In addition, it must be considered that the approach of combining chemotherapy and immunotherapy also leads to increased toxicity, as observed with most combination therapies. For example, in the lung cancer KEYNOTE-189 trial, despite a similar overall rate of adverse events, the discontinuation rate for all treatments or any treatment component was higher in the chemoimmunotherapy combination arm (53).
Disease-by-Disease Experience
Examples of already available phase III evidence supporting the notion of chemoimmunotherapy combinations can be found and have been published or recently released in congresses in multiple oncology conditions [Table 1, including HR and P data evidence for overall survival (OS) or progression-free survival (PFS)]. Moreover, hundreds of clinical trials are ongoing or are in the plan/preparation phases in which immunotherapy agents are combined with chemotherapy regimens again across multiple malignant indications (Supplementary Table). Furthermore, many studies on neoadjuvant settings are ongoing with evidence for enhanced pathologic responses on chemoimmunotherapy that remain to be validated in terms of OS consequences. A general appraisal of these types of combinations is quite favorable, and they will likely expand to numerous diseases and disease stages. However, benefit is not universally found, and there are trials failing to report superiority of chemoimmunotherapy over standard-of-care options.
Chemoimmunotherapy clinical phase III trials with disclosed efficacy results
| Indication . | Stage . | Chemotherapy agent . | Immunotherapy agent . | NCT . | Ref. . | Clinical efficacy (ChtIO/Cht) . | Statistical evidence . | FDA approval . | Clinical benefit . |
|---|---|---|---|---|---|---|---|---|---|
| NSCLC | MTS 1L | Platinum/Pem | Pembrolizumab | KEYNOTE-189 (NCT02578680) | 53 | ORR 47.6 vs. 18.9%; PFS: 8.8 m vs. 4.9 m; OS at 12 months 69.2% vs. 49.4% | OS: HR 0.49 (CI 0.38–0.64); P < 0.001 | Yes | Yes |
| NSCLC | MTS 1L | Platinum-based + Pem | Atezolizumab | IMpower 132 (NCT02657434) | 59 | ORR 47% vs. 32%; PFS 7.6 m vs. 5.2 m; OS 18.1 m vs. 13.6 m | PFS: HR 0.596 (CI 0.494–0.719); P < 0.0001 | No | Yes |
| NSCLC | MTS 1L | Histology-based ChT | Nivolumab | CheckMate 227 (NCT02477826) | 57 | ORR 48.1 vs. 29.3%; PFS 8.7 vs. 5.8 m; OS 18.8 vs. 15.6 m | OS: HR 0.86 (CI 0.69–1.08); P = 0.1859 | No | No |
| NSCLC | MTS 1L | Histology-based ChT | Nivolumab + ipilimumab | CheckMate 9LA (NCT03215706) | 61 | ORR 38 vs. 25%; PFS 6.7 vs. 5 m; OS 15.6 vs. 10.9 m; OS at 1-year 63% vs. 47% | OS: HR 0.69 (CI 0.55–0.87); P = 0.0006 | Yes | Yes |
| NSCLC | MTS 1L | Carb + Pacl + Bev | Nivolumab | TASUKI-52 (ONO-4538-52) | 58 | PFS 12.12 vs. 8.11 m; OS not mature | PFS: HR 0.56 (CI 0.43–0.71); P = 0.0001 | No | Yes |
| NSCLC | MTS 1L | Carb + Pacl + Bev | Atezolizumab | IMpower150 (NCT02366143) | 63 | ORR 63.5 vs. 48%; PFS 8.3 vs. 8.6 m; OS 19.2 vs. 14.7 m | OS: HR 0.78 (CI: 0.64–0.96); P = 0.02 | Yes | Yes |
| NSCLCsq | MTS 1L | Carb + Nab-Pacl/Pacl | Pembrolizumab | KEYNOTE-407 (NCT02775435) | 56 | ORR 57.9 vs. 38.4%; PFS 6.4 vs. 4.8 m; OS 15.9 vs. 11.3 m | OS: HR 0.64 (CI 0.49–0.85); P < 0.001 | Yes | Yes |
| NSCLCsq | MTS 1L | Carb + Pacl/Nab-Pacl | Atezolizumab | IMpower131 (NCT02367794) | 60 | ORR 49 vs. 41%; PFS 6.3 m vs. 5.6 m; OS 14.2 m vs. 13.5 m | PFS: HR 0.71 (CI 0.60–0.85); P = 0.0001 | No | No |
| SCLC | MTS 1L | Carb + Etop | Atezolizumab | IMpower133 (NCT02763579) | 65 | ORR 60.2 vs. 64.4%; PFS 5.2 vs. 4.3 m; OS 12.3 vs. 10.3 m | OS: HR 0.70 (CI 0.54–0.91); P = 0.007 | Yes | Yes |
| SCLC | MTS 1L | Carb + Etop | Durvalumab | CASPIAN (NCT03043872) | 66 | ORR 68 vs. 58%; OS 13 vs. 10.3 m | OS: HR 0.73 (CI 0.59–0.91); P = 0.0047 | Yes | Yes |
| SCLC | MTS 1L | Carb/Cis + Etop | Pembrolizumab | KEYNOTE-604 (NCT03066778) | 67 | ORR 70.6 vs. 61.8%; PFS 4.5 vs. 4.3 m; OS 10.8 vs. 9.7 m | PFS: HR 0.75 (CI 0.61–0.91); P = 0.0023. OS: HR 0.80 (0.64–0.98); P = 0.0164 | No | Yes? |
| Breast TN | MTS 1L | Nab-Pacl | Atezolizumab | IMpassion 130 (NCT02425891) | 68, 69, 70 | PFS: 7.2 vs. 5.5 m; OS (ITT): 21 vs. 18.7 m; OS (PD-L1>1%): 25.4 vs. 17.9 m | PFS: HR 0.80 (CI 0.69–0.92); P = 0.002 OS (ITT): HR 0.87 (CI 0.72–1.02); P = 0.078 OS (PD-L>1%): HR 0.67 (CI 0.53–0.86) | Yes, PD-L1 (+) | No |
| Breast TN | MTS 1L | Pacl | Atezolizumab | IMpassion 131 (NCT03125902) | 71 | ORR 54 vs. 47%; PFS 5.7 vs. 5.6 m; OS 19.2 vs. 22.8 m | OS: HR 1.12 (CI 0.76–1.65) PFS: HR 0.82 (CI 0.60–1.12) | No | No |
| Breast TN | MTS 1L | Nab-Pacl or Pacl or Carb + Gem | Pembrolizumab | KEYNOTE-355 (NCT02819518) | 72 | PFS (CPS>10) 9.7 vs. 5.6 m; PFS (CPS>1) 7.6 vs. 5.6 m | PFS (CPS>10): HR 0.65 (CI 0.49–0.86) P = 0.00411 | Yes (PD-L1 CPS>10) | Yes |
| Breast TN | NeoAd | Pacl + Cycloph + Doxor/Epi | Pembrolizumab | KEYNOTE-522 (NCT03036488) | 75 | pCR 64.8% vs. 51.2% | pCR: Inc. 13.6%; CI 5.4 to 21.8; P < 0.001 | No | Yes |
| Breast TN | NeoAd | Carb + Nab-Pacl | Atezolizumab | NeoTRIPaPDL1 (NCT02620280) | 76 | pCR 43.5% vs. 40.8% | Not available | No | No |
| Breast TN early | NeoAd | Pacl + Cycloph + Doxor | Atezolizumab | IMpassion031 (NCT03197935) | 77 | pCR 57.6% vs. 41.1% | pCR: Inc. 16.5% (5.9, 27.1); 1-sided P = 0.0044 | No | Yes |
| Bladder | MTS 1L | Gem + Cis/Carb | Avelumab (maintenance) | JAVELIN Bladder 100 (NCT02603432) | 87 | OS 21.4 m vs. 14.3 m | OS: HR 0.69 (CI 0.56–0.86); 1-sided P = 0.0005 | Yes | Yes |
| Bladder | MTS 1L | Gem + Cis/Carb | Pembrolizumab | KEYNOTE-361 (NCT02853305) | 89 | ORR 54.7 vs. 44.9%; PFS 8.3 vs. 7.1 m; OS 17 vs. 14.3 m | PFS: HR 0.78 (IC 0.65–0.93); P = 0.0033. OS: HR 0.86 (IC 0.72–1.02); P = 0.0407 | No | No |
| HNC | MTS 1L | Carb/Cis + 5-FU or Carb/Cis + 5-FU + Cetux | Pembrolizumab | KEYNOTE-048 (NCT02358031) | 92 | ORR 35 vs. 19%; OS (ITT): 13 vs. 10.7 m. OS (CPS≥1): 13.6 vs. 10.4 m. OS (CPS≥20): 14.7 vs. 11 m | OS (ITT): HR 0.77 (CI 0.63–0.93); P = 0.0034. OS (CPS≥1): HR 0.65 (CI 0.53–0.80); P < 0.0001. OS (CPS≥20): 0.60 (CI 0.45–0.82); P = 0.0004 | Yes CPS≥1 | Yes |
| Gastric | MTS 1L | Cis + 5-FU/Cape | Pembrolizumab | KEYNOTE-062 (NCT02494583) | 101 | ORR 52.5% vs. 36.7%; PFS (CPS≥1) 6.9 m vs. 6.4 m; OS (CPS≥1) 12.5 vs. 11.1 m OS (CPS≥10) 12.3 vs. 10.8 m | OS (CPS≥1): HR, 0.85 (CI 0.70–1.03); P = 0.05. OS (CPS≥10): HR, 0.85 (CI 0.62–1.17); P = 0.16 | No | No |
| Gastric/Esophageal | MTS 1L | Cape + Oxali/5-FU + Oxali | Nivolumab | CheckMate-649 (NCT02872116) | 102 | PFS (PD-L1 CPS≥5) 7.6 vs. 6.1 m; OS (all) 13.8 vs. 11.6 m | OS (all): HR 0.80 (CI 0.68–0.94); P = 0.0002.PFS (CPS≥5): HR 0.68 (CI 0.56–0.81); P < 0.0001 | No | Yes |
| Indication | Stage | Chemotherapy agent | Immunotherapy agent | NCT | Ref. | Clinical efficacy (ChtIO/Cht) | Statistical evidence | FDA approval | Clinical benefit |
| Gastric | MTS 1L | S-1 + Oxali/Cape + Oxali | Nivolumab | ATTRACTION (ONO-4538–37) | 103 | ORR 57.5 vs. 47.8%; PFS 10.5 vs. 8.3 m; OS 17.5 vs. 17.2 m | PFS: HR 0.68 (CI 0.51–0.90); P = 0.0007 OS: HR 0.90 (CI 0.75–1.08); P = 0.257 | No | Yes |
| Esophageal | Adjuvant | CRT | Nivolumab | CheckMate 577 (NCT02743494) | 104 | DFS 22.4 vs. 11 m | DFS: HR 0.69 (CI 0.56–0.86); P = 0.0003 | No | Yes |
| Esophageal | MTS 1L | Cis + 5-FU | Pembrolizumab | KEYNOTE-590 (NCT03189719) | 105 | ORR (all) 45 vs. 29.3%; PFS (all) 6.3 vs. 5.8 m; OS (all) 12.4 vs. 9.8 m | PFS (all): HR 0.65 (CI, 0.55–0.76); P < 0.0001. OS (all): HR, 0.73 (CI 0.62–0.86); P < 0.0001 | No | Yes |
| Glioblastoma | MTS 1L | Temoz + RT | Nivolumab | CheckMate-548 (NCT02667587) | [press release]. Princeton, NJ: BMS; May 9, 2019 | PFS not improved, OS not mature | Results not published | No | No |
| Ovarian | NeoAd/Ad | Carb + Pacl + Bev | Atezolizumab | IMagyn050 (NCT03038100) | Ann Oncol. 2020;31:S1161–S1162. | PFS (ITT) 19.5 vs. 18.6 m; PFS (PD-L1+) 20.8 vs. 18.5 m; OS not mature | PFS (ITT): HR 0.92 (CI 0.79–1.07). PFS (PD-L1+): HR 0.80 (CI 0.65–0.99) | No | No |
| Indication . | Stage . | Chemotherapy agent . | Immunotherapy agent . | NCT . | Ref. . | Clinical efficacy (ChtIO/Cht) . | Statistical evidence . | FDA approval . | Clinical benefit . |
|---|---|---|---|---|---|---|---|---|---|
| NSCLC | MTS 1L | Platinum/Pem | Pembrolizumab | KEYNOTE-189 (NCT02578680) | 53 | ORR 47.6 vs. 18.9%; PFS: 8.8 m vs. 4.9 m; OS at 12 months 69.2% vs. 49.4% | OS: HR 0.49 (CI 0.38–0.64); P < 0.001 | Yes | Yes |
| NSCLC | MTS 1L | Platinum-based + Pem | Atezolizumab | IMpower 132 (NCT02657434) | 59 | ORR 47% vs. 32%; PFS 7.6 m vs. 5.2 m; OS 18.1 m vs. 13.6 m | PFS: HR 0.596 (CI 0.494–0.719); P < 0.0001 | No | Yes |
| NSCLC | MTS 1L | Histology-based ChT | Nivolumab | CheckMate 227 (NCT02477826) | 57 | ORR 48.1 vs. 29.3%; PFS 8.7 vs. 5.8 m; OS 18.8 vs. 15.6 m | OS: HR 0.86 (CI 0.69–1.08); P = 0.1859 | No | No |
| NSCLC | MTS 1L | Histology-based ChT | Nivolumab + ipilimumab | CheckMate 9LA (NCT03215706) | 61 | ORR 38 vs. 25%; PFS 6.7 vs. 5 m; OS 15.6 vs. 10.9 m; OS at 1-year 63% vs. 47% | OS: HR 0.69 (CI 0.55–0.87); P = 0.0006 | Yes | Yes |
| NSCLC | MTS 1L | Carb + Pacl + Bev | Nivolumab | TASUKI-52 (ONO-4538-52) | 58 | PFS 12.12 vs. 8.11 m; OS not mature | PFS: HR 0.56 (CI 0.43–0.71); P = 0.0001 | No | Yes |
| NSCLC | MTS 1L | Carb + Pacl + Bev | Atezolizumab | IMpower150 (NCT02366143) | 63 | ORR 63.5 vs. 48%; PFS 8.3 vs. 8.6 m; OS 19.2 vs. 14.7 m | OS: HR 0.78 (CI: 0.64–0.96); P = 0.02 | Yes | Yes |
| NSCLCsq | MTS 1L | Carb + Nab-Pacl/Pacl | Pembrolizumab | KEYNOTE-407 (NCT02775435) | 56 | ORR 57.9 vs. 38.4%; PFS 6.4 vs. 4.8 m; OS 15.9 vs. 11.3 m | OS: HR 0.64 (CI 0.49–0.85); P < 0.001 | Yes | Yes |
| NSCLCsq | MTS 1L | Carb + Pacl/Nab-Pacl | Atezolizumab | IMpower131 (NCT02367794) | 60 | ORR 49 vs. 41%; PFS 6.3 m vs. 5.6 m; OS 14.2 m vs. 13.5 m | PFS: HR 0.71 (CI 0.60–0.85); P = 0.0001 | No | No |
| SCLC | MTS 1L | Carb + Etop | Atezolizumab | IMpower133 (NCT02763579) | 65 | ORR 60.2 vs. 64.4%; PFS 5.2 vs. 4.3 m; OS 12.3 vs. 10.3 m | OS: HR 0.70 (CI 0.54–0.91); P = 0.007 | Yes | Yes |
| SCLC | MTS 1L | Carb + Etop | Durvalumab | CASPIAN (NCT03043872) | 66 | ORR 68 vs. 58%; OS 13 vs. 10.3 m | OS: HR 0.73 (CI 0.59–0.91); P = 0.0047 | Yes | Yes |
| SCLC | MTS 1L | Carb/Cis + Etop | Pembrolizumab | KEYNOTE-604 (NCT03066778) | 67 | ORR 70.6 vs. 61.8%; PFS 4.5 vs. 4.3 m; OS 10.8 vs. 9.7 m | PFS: HR 0.75 (CI 0.61–0.91); P = 0.0023. OS: HR 0.80 (0.64–0.98); P = 0.0164 | No | Yes? |
| Breast TN | MTS 1L | Nab-Pacl | Atezolizumab | IMpassion 130 (NCT02425891) | 68, 69, 70 | PFS: 7.2 vs. 5.5 m; OS (ITT): 21 vs. 18.7 m; OS (PD-L1>1%): 25.4 vs. 17.9 m | PFS: HR 0.80 (CI 0.69–0.92); P = 0.002 OS (ITT): HR 0.87 (CI 0.72–1.02); P = 0.078 OS (PD-L>1%): HR 0.67 (CI 0.53–0.86) | Yes, PD-L1 (+) | No |
| Breast TN | MTS 1L | Pacl | Atezolizumab | IMpassion 131 (NCT03125902) | 71 | ORR 54 vs. 47%; PFS 5.7 vs. 5.6 m; OS 19.2 vs. 22.8 m | OS: HR 1.12 (CI 0.76–1.65) PFS: HR 0.82 (CI 0.60–1.12) | No | No |
| Breast TN | MTS 1L | Nab-Pacl or Pacl or Carb + Gem | Pembrolizumab | KEYNOTE-355 (NCT02819518) | 72 | PFS (CPS>10) 9.7 vs. 5.6 m; PFS (CPS>1) 7.6 vs. 5.6 m | PFS (CPS>10): HR 0.65 (CI 0.49–0.86) P = 0.00411 | Yes (PD-L1 CPS>10) | Yes |
| Breast TN | NeoAd | Pacl + Cycloph + Doxor/Epi | Pembrolizumab | KEYNOTE-522 (NCT03036488) | 75 | pCR 64.8% vs. 51.2% | pCR: Inc. 13.6%; CI 5.4 to 21.8; P < 0.001 | No | Yes |
| Breast TN | NeoAd | Carb + Nab-Pacl | Atezolizumab | NeoTRIPaPDL1 (NCT02620280) | 76 | pCR 43.5% vs. 40.8% | Not available | No | No |
| Breast TN early | NeoAd | Pacl + Cycloph + Doxor | Atezolizumab | IMpassion031 (NCT03197935) | 77 | pCR 57.6% vs. 41.1% | pCR: Inc. 16.5% (5.9, 27.1); 1-sided P = 0.0044 | No | Yes |
| Bladder | MTS 1L | Gem + Cis/Carb | Avelumab (maintenance) | JAVELIN Bladder 100 (NCT02603432) | 87 | OS 21.4 m vs. 14.3 m | OS: HR 0.69 (CI 0.56–0.86); 1-sided P = 0.0005 | Yes | Yes |
| Bladder | MTS 1L | Gem + Cis/Carb | Pembrolizumab | KEYNOTE-361 (NCT02853305) | 89 | ORR 54.7 vs. 44.9%; PFS 8.3 vs. 7.1 m; OS 17 vs. 14.3 m | PFS: HR 0.78 (IC 0.65–0.93); P = 0.0033. OS: HR 0.86 (IC 0.72–1.02); P = 0.0407 | No | No |
| HNC | MTS 1L | Carb/Cis + 5-FU or Carb/Cis + 5-FU + Cetux | Pembrolizumab | KEYNOTE-048 (NCT02358031) | 92 | ORR 35 vs. 19%; OS (ITT): 13 vs. 10.7 m. OS (CPS≥1): 13.6 vs. 10.4 m. OS (CPS≥20): 14.7 vs. 11 m | OS (ITT): HR 0.77 (CI 0.63–0.93); P = 0.0034. OS (CPS≥1): HR 0.65 (CI 0.53–0.80); P < 0.0001. OS (CPS≥20): 0.60 (CI 0.45–0.82); P = 0.0004 | Yes CPS≥1 | Yes |
| Gastric | MTS 1L | Cis + 5-FU/Cape | Pembrolizumab | KEYNOTE-062 (NCT02494583) | 101 | ORR 52.5% vs. 36.7%; PFS (CPS≥1) 6.9 m vs. 6.4 m; OS (CPS≥1) 12.5 vs. 11.1 m OS (CPS≥10) 12.3 vs. 10.8 m | OS (CPS≥1): HR, 0.85 (CI 0.70–1.03); P = 0.05. OS (CPS≥10): HR, 0.85 (CI 0.62–1.17); P = 0.16 | No | No |
| Gastric/Esophageal | MTS 1L | Cape + Oxali/5-FU + Oxali | Nivolumab | CheckMate-649 (NCT02872116) | 102 | PFS (PD-L1 CPS≥5) 7.6 vs. 6.1 m; OS (all) 13.8 vs. 11.6 m | OS (all): HR 0.80 (CI 0.68–0.94); P = 0.0002.PFS (CPS≥5): HR 0.68 (CI 0.56–0.81); P < 0.0001 | No | Yes |
| Indication | Stage | Chemotherapy agent | Immunotherapy agent | NCT | Ref. | Clinical efficacy (ChtIO/Cht) | Statistical evidence | FDA approval | Clinical benefit |
| Gastric | MTS 1L | S-1 + Oxali/Cape + Oxali | Nivolumab | ATTRACTION (ONO-4538–37) | 103 | ORR 57.5 vs. 47.8%; PFS 10.5 vs. 8.3 m; OS 17.5 vs. 17.2 m | PFS: HR 0.68 (CI 0.51–0.90); P = 0.0007 OS: HR 0.90 (CI 0.75–1.08); P = 0.257 | No | Yes |
| Esophageal | Adjuvant | CRT | Nivolumab | CheckMate 577 (NCT02743494) | 104 | DFS 22.4 vs. 11 m | DFS: HR 0.69 (CI 0.56–0.86); P = 0.0003 | No | Yes |
| Esophageal | MTS 1L | Cis + 5-FU | Pembrolizumab | KEYNOTE-590 (NCT03189719) | 105 | ORR (all) 45 vs. 29.3%; PFS (all) 6.3 vs. 5.8 m; OS (all) 12.4 vs. 9.8 m | PFS (all): HR 0.65 (CI, 0.55–0.76); P < 0.0001. OS (all): HR, 0.73 (CI 0.62–0.86); P < 0.0001 | No | Yes |
| Glioblastoma | MTS 1L | Temoz + RT | Nivolumab | CheckMate-548 (NCT02667587) | [press release]. Princeton, NJ: BMS; May 9, 2019 | PFS not improved, OS not mature | Results not published | No | No |
| Ovarian | NeoAd/Ad | Carb + Pacl + Bev | Atezolizumab | IMagyn050 (NCT03038100) | Ann Oncol. 2020;31:S1161–S1162. | PFS (ITT) 19.5 vs. 18.6 m; PFS (PD-L1+) 20.8 vs. 18.5 m; OS not mature | PFS (ITT): HR 0.92 (CI 0.79–1.07). PFS (PD-L1+): HR 0.80 (CI 0.65–0.99) | No | No |
NOTE: Each clinical trial is referred to according to text bibliography. Abbreviations: 5-FU, 5-Fluorouracile; Bev, bevacizumab; Cape, capecitabine; Carb, carboplatin; Cetux, cetuximab; ChT, chemotherapy; Cis, cisplatin; CPS, PD-L1 combined positive score; CRT, chemoradiotherapy; Cycloph, cyclophosphamide; Doxor, doxorubicin; DFS, disease-free survival; Epi, epirubicin; Etop, etoposide; Gem, gemcitabine; ITT, intention-to-treat; HNC, head and neck cancer; MTS, metastatic; Nab-Pacl, nab-paclitaxel; NeoAd, neoadjuvant; NeoAd/Ad, neoadjuvant and/or adjuvant; NSCLC, non–small cell lung cancer squamous and non-squamous; NSCLCsq, squamous non–small cell lung cancer; ORR, objective response rate; OS, overall survival; Oxali, oxaliplatin; Pacl, paclitaxel; Pem, pemetrexed; PFS, progression-free survival; pCR, pathologic complete response; RT, radiotherapy; Temoz, temozolamide; TN, triple negative.
For this approach, the accepted standard-of-care chemotherapy regimen has been chosen as such in most cases. We have elected not to present a catalog of immune-related effects of chemotherapy agents as published by Galluzzi and colleagues (18), because in the best of cases it would be incomplete and probably inaccurate. Indeed, the immune-effect profile of chemotherapy drugs commonly used in the clinic needs to be investigated in mouse models and in humans over a broad range of doses.
Chemoimmunotherapy of Lung Cancer
The first and foremost success of chemotherapy being combined with immunotherapy came in the field of non–small cell lung cancer (NSCLC). Following approval of PD-1 and PD-L1 antagonists in second-line metastatic or locally advanced NSCLC, a race for approvals as the first line of treatment with immunotherapy agents began. Single-agent immunotherapy found efficacy in first-line therapy against tumors with high (>50%) PD-L1 expression versus platinum-based chemotherapy doublets (54, 55). In this scenario, an obvious approach was to add immunotherapy to the standard chemotherapy regimens and maintenance with anti–PD-1/PD-L1 immunotherapy as suggested by phase II trials. Amazing unprecedented efficacy in terms of OS as compared with chemotherapy was observed for a pembrolizumab + chemotherapy combination either for adenocarcinoma (HR 0.49; P < 0.001; ref. 53) or for squamous histologies (HR 0.64; P < 0.001; ref. 56). Intriguingly, a parallel trial of chemotherapy with nivolumab failed in its primary endpoint of OS to beat chemotherapy with the chemoimmunotherapy combination in the first-line setting (HR 0.86; P = 0.1859; ref. 57). Nonetheless, results from a randomized phase III clinical trial comparing the addition or not of nivolumab to carboplatin + paclitaxel + bevacizumab for first-line nonsquamous NSCLChave recently disclosed superiority for the nivolumab-containing arm in terms of PFS (HR 0.56; P = 0.0001), while the study is yet immature for OS (58).
The anti–PD-L1 monoclonal antibody atezolizumab combined with carboplatin/cisplatin and pemetrexed for first-line metastatic nonsquamous NSCLC improved PFS compared with chemotherapy alone (HR 0.596; P < 0.0001; ref. 59). Similar benefit in PFS for a chemoimmunotherapy combination with atezolizumab in squamous NSCLC came from another phase III trial (HR 0.71; P = 0.0001), but OS was no longer in the chemoimmunotherapy arm (60). Most recently, ipilimumab + nivolumab combined with chemotherapy surpassed chemotherapy alone as a first-line treatment (HR 0.69; P = 0.0006; ref. 61).
Frequent crossover from chemotherapy to immunotherapy did not prevent improved survival, thus supporting the notion that sequencing both approaches is less beneficial. Importantly, benefit extended to patients with tumors presenting low or no expression of PD-L1. Safety profiles of the combination were tolerable, and >grade 3 adverse events were similar in percentages to chemotherapy + placebo (53, 56). However, as mentioned, the discontinuation rate was higher in the chemoimmunotherapy arm in the Keynote-189 trial (53).
Other PD-1/PD-L1–blocking-based combinations, including those with anti-CTLA4 antibodies and VEGF blockade, have also recently obtained FDA approval for first-line treatment of NSCLC. In this regard, the field has widened with the use of ipilimumab + nivolumab that surpasses chemotherapy, especially in those patients with a high tumor mutational burden (62), and atezolizumab + bevacizumab + chemotherapy, which is better than bevacizumab + chemotherapy (HR 0.78; P = 0.02; ref. 63). As mentioned above, nivolumab in combination with chemotherapy + bevacizumab also rendered benefit over standard chemotherapy + bevacizumab (58).
The most astonishing results of immunotherapy in lung cancer have been observed in the neoadjuvant setting, where nivolumab achieved pathologic complete responses in 45% of cases (64). Several phase III clinical trials are evaluating the added benefit of combining immunotherapy and chemotherapy in the neoadjuvant setting (Supplementary Table).
In small cell lung cancer (SCLC), recent results have also documented in first-line treatment that the addition of PD-L1 blockade with atezolizumab (65) or durvalumab (66) to standard platinum + etoposide yields better results than chemotherapy alone (HR 0.70, P = 0.007; HR 0.73, P = 0.0047, respectively, for atezolizumab or durvalumab). The benefit for pembrolizumab with etoposide + carboplatin over chemotherapy alone has been reported in a phase III trial in terms of PFS (HR 0.75; P = 0.0023), but with a final analysis for OS that did not reach the significance boundary, even if a favorable tendency was observed (HR 0.80; P = 0.0164; ref. 67).
The clinical success of these combinations in the NSCLC and SCLC arenas has not been followed by deep mechanistic insight or the identification of predictive or pharmacodynamic biomarkers. The discovery and validation of such markers is crucial and the focus of ongoing efforts.
Chemoimmunotherapy of Breast Cancer
From the different types of carcinoma of the breast, HER2-negative hormone receptor–negative [triple-negative breast cancer (TNBC)] remains a formidable clinical challenge. In the absence of targeted therapy, the standard of care includes several lines of chemotherapy.
Much enthusiasm and expectation were originally raised by the published results of a clinical trial testing first-line treatment of metastatic TNBC using a combination of nab-paclitaxel + atezolizumab that conferred a better PFS for the combination arm over chemotherapy alone (HR 0.80; P = 0.002), which was higher in the PD-L1–positive tumors (68). However, the final results for OS were negative for the intention-to-treat population (HR 0.87; P = 0.078; refs. 69, 70). The clinical benefit has been described to be almost restricted to patients with PD-L1 > 1% (HR 0.67; refs. 69, 70). Given these results, the field underwent a significant degree of confusion, and the FDA issued an alert regarding the marketing approval. Furthermore, a trial that tested paclitaxel in combination with atezolizumab versus paclitaxel in monotherapy also for first-line TNBC has rendered negative results [HR (OS) 1.12; HR (PFS) 0.82; ref. 71]. In this case, the need for immunosuppressive steroids to permit administration of the weekly taxane might have been involved in the lack of superiority for the chemoimmunotherapy.
A phase III clinical trial comparing pembrolizumab in combination with chemotherapy (paclitaxel, nab-paclitaxel, or carboplatin/gemcitabine) versus chemotherapy alone has shown a significant benefit for the chemoimmunotherapy combination in those patients with combined positive score (CPS) ≥ 10 (HR 0.65; P = 0.00411), leading to FDA approval, but results were not statistically significant for patients with CPS ≤ 1 (72). Of important note, numerous phase I–II clinical trials are exploiting chemoimmunotherapy combinations in patients with metastatic TNBC (Supplementary Table).
In early-stage TNBC following diagnostic biopsy, neoadjuvant chemotherapy regimens have been shown to be highly beneficial to avoid relapse (73). Recently, combination results with pembrolizumab added to the neoadjuvant chemotherapy regimens in two randomized phase II–III trials enhanced the percentage of pathologic complete responses. In this phase II trial (I-SPY2), the pathologic complete response rate in the combination arm was 60% compared with 20% in the chemotherapy-alone arm (74). In the phase III clinical trial, the pathologic complete response rate was 64.8% in the pembrolizumab + chemotherapy arm and 51.2% in the chemotherapy arm (estimated treatment difference 13.6%; P < 0.001; ref. 75) and will be probably conducive to a survival benefit. A randomized study with atezolizumab + chemotherapy in a similar neoadjuvant setting was, however, negative (from 40.8% to 43.5%), even in the PD-L1–positive population (76). Nonetheless, a phase III clinical trial of atezolizumab + chemotherapy in early-stage TNBC has concluded benefit for chemoimmunotherapy, with pathologic complete responses seen in 57.6% versus 41.1% (P = 0.0044; ref. 77). Whether these findings translate into OS and PFS benefit needs longer follow-up.
A phase II randomized clinical trial in the neoadjuvant setting that combines durvalumab versus placebo plus chemotherapy (nab-paclitaxel sequenced to epirubicine + cyclophosphamide) did not show a significant improvement in pCR, although those patients who had received durvalumab alone two weeks before starting chemotherapy had a better and significant pCR advantage versus those who did not receive durvalumab (61.0% vs. 41.4%; OR 2.22; 95% CI 1.06–4.64; P = 0.035; ref. 78). These results stress again the importance of an adequate treatment sequencing of chemo and immunotherapy to achieve the best from such combinations.
At present, the field of TNBC awaits clarification on whether there is a benefit of chemoimmunotherapy versus chemotherapy alone. It could be that the type of chemotherapy, the level of expression of PD-L1, and the vast genetic/transcriptomic heterogeneity of TNBC subtypes matter (79). In this regard, taxanes are considered weak inducers of immunogenic cell death, whereas anthracyclines and alkylating agents are considered to be more proimmunogenic (16). Only further translational research will be able to clarify these points.
Chemoimmunotherapy of Genitourinary Tumors
PD-1/PD-L1 immunotherapy is standard therapy in RCC (80). Prior to the advent of checkpoint blockade, the standard of care for first-line clear cell RCC (ccRCC) treatment was not chemotherapy, but rather antiangiogenic tyrosine kinase inhibitors (TKI). Following the usual paradigm of adding immunotherapy to standard-of-care therapy, first-line treatment of metastatic ccRCC now includes combinations of anti–PD-1 with antiangiogenic agents such as axitinib + pembrolizumab (38), avelumab + axitinib (39), and nivolumab + ipilimumab (81), which in all cases outperformed sunitinib. In this disease, further addition of chemotherapy would be complicated because of its lack of efficacy on its own and the potential for increased toxicity.
In contrast, metastatic urothelial carcinoma has clearly benefited to some extent from platinum-based chemotherapy (82). Pembrolizumab and atezolizumab are approved for second-line treatment of metastatic urothelial carcinoma (83, 84, 85) and as first-line treatment for patients who are ineligible for cisplatin (86). Recently, a phase III clinical trial comparing avelumab as maintenance after an induction phase of chemotherapy versus best supportive care resulted in overwhelmingly better results for the immunotherapy over placebo (HR 0.69; one-sided P = 0.0005), thus leading to FDA approval (87). More recently, exploratory biomarkers in biopsies indicated that those patients with indicators of lymphocyte activity benefited the most with avelumab maintenance, whereas benefit was negatively associated with markers of chronic inflammation (88). By contrast, recently released results from a phase III clinical trial in first line failed to meet the statistical thresholds for the benefit of pembrolizumab combined with chemotherapy as compared with chemotherapy alone, even though there was a clear tendency in favor of chemoimmunotherapy [HR (PFS) 0.78; P = 0.0033; HR (OS) 0.86; P = 0.0407; ref. 89]. This trial (KEYNOTE 361) is very interesting in its three-arm design because it compares chemotherapy alone with chemoimmunotherapy and includes a third immunotherapy-alone arm. However, the comparison with the pembrolizumab single-treatment arm is not available yet.
In castration-resistant metastatic prostate cancer, a beneficial effect of checkpoint inhibitors remains to be seen, although taxane chemotherapy is indicated following hormonal therapy failure. Perhaps subgroups of patients such as those with microsatellite-unstable or BRCA-mutant prostate cancer may benefit from the addition of checkpoint inhibitors to chemotherapy, as is being tested in clinical trials (NCT03834506). As mentioned, one of the potential problems for taxanes is the need for them to be accompanied by steroids, which in pharmacodynamics terms may be at odds with checkpoint inhibitors.
Chemoimmunotherapy of Squamous Head and Neck Cancer
Nivolumab and pembrolizumab are approved for second-line treatment of head and neck cancers (90, 91). Conventional first-line treatment involves the use of chemotherapy and anti-EGFR (cetuximab). Pembrolizumab monotherapy is also approved for first-line treatment of patients whose tumors are CPS > 20 (92). In the same trial (KEYNOTE-048), chemotherapy + pembrolizumab was found to be superior to cetuximab + chemotherapy in the intention-to-treat, in CPS > 1, and in CPS > 20 populations in OS (HR 0.77, 0.65, and 0.60, respectively; P = 0.0034, P < 0.0001, P = 0.0004, respectively), although chemoimmunotherapy did not show superior PFS (92). In this regard, it is worth mentioning that immunotherapy seems to enable more durable objective responses in this setting. The nature of this disease offers many opportunities for neoadjuvant or adjuvant chemoimmunotherapy treatments that are already under intensive investigation in early stages of the disease (Supplementary Table).
Chemoimmunotherapy for Gastrointestinal Tumors
Immunotherapy with checkpoint inhibitors has demonstrated clinical benefit in patients with metastatic microsatellite-unstable colorectal cancer (93), gastric cancer (94), and HCC (95). PD-1/PD-L1 immunotherapy alone minimally affects disease response in patients with pancreatic ductal adenocarcinoma (PDAC; ref. 96); even in microsatellite instability–high (MSI-H) cases the response rate is below 20% (97). Chemotherapy regimens are considered first-line standard of care for colorectal cancer (in combination with cetuximab or bevacizumab), gastric cancer, esophageal cancer, and PDAC.
Colorectal Cancer
In metastatic microsatellite-stable (MSS) colorectal cancer, the use of checkpoint inhibitors thus far offers only anecdotal evidence of clinical activity, despite the fact that T-cell infiltration of primary tumors very much determines prognosis (98). However, recent evidence shows that PD-1 blockade in neoadjuvant regimens prior to removal of resectable primary MSS tumors achieves frequent pathologic responses (99). This disease arena might become fertile for combination regimens including novel immunotherapy agents that are postulated to synergize with chemotherapy regimens. As mentioned, for MSI-H metastatic colorectal cancer, pembrolizumab monotherapy has demonstrated improved PFS over standard of care (chemotherapy plus bevacizumab or cetuximab), supporting recent FDA approval for the indication (100).
Gastric and Esophageal Cancer
Recent data released at the European Society for Medical Oncology (ESMO) Virtual Congress 2020 regarding gastroesophageal junction (GEJ) and gastric cancer provide evidence for chemoimmunotherapy in the first-line setting of these diseases. Publication of such evidence in metastatic or advanced gastric cancer is eagerly awaited because communications in congresses seem to be conflicting to some extent with previous observations. A randomized phase III trial (101) concluded that the addition of chemotherapy to pembrolizumab apparently worsens survival over pembrolizumab or chemotherapy as single treatments (ref. 101; Table 1). Although there may be issues in this trial of patient selection, these results alert us to the fact that chemoimmunotherapy will not be universally beneficial. In line with this, it is possible that agents such as 5-fluorouracile, commonly used in digestive tumor regimens, might be deleterious for anticancer immune responses (51), even more so when used as an add-on rather than in sequential strategies. In striking contrast, recent results from another phase III trial evaluating chemoimmunotherapy combination in first line for advanced cancer of the GEJ/gastric cancer with nivolumab have shown benefit in PFS and OS in the prespecified interim analysis in those patients who received the combination and expressed PD-L1 CPS ≥ 5 [HR (OS) 0.80; P = 0.0002, and HR (PFS CPS ≥ 5) 0.68; P < 0.0001; ref. 102], leading to FDA marketing approval. In the same regard, another study in Asian patients comparing nivolumab + chemotherapy versus chemotherapy for first-line advanced GEJ/gastric cancer showed benefit for chemoimmunotherapy in PFS (HR 0.68; P = 0.0007; ref. 103).
In the localized setting of GEJ/gastric cancer following neoadjuvant chemoradiation and post-resection, adjuvant treatment with nivolumab resulted in a disease-free survival benefit as compared with placebo (HR 0.69; P = 0.003; ref. 104).
In advanced esophageal cancer, more specifically in squamous with PD-L1 CPS > 10, there was a very clear benefit for chemoimmunotherapy over chemotherapy alone (HR 0.57; P < 0.0001), although these positive outcomes favoring chemoimmunotherapy are also expanded to the intention-to-treat population (HR 0.73; P < 0.0001; ref. 105). It would have been very interesting to have an immunotherapy-alone arm in this study.
HCC
In the case of HCC, chemotherapy has never been first-line standard of care, whereas TKIs (sorafenib and lenvatinib) still are. However, chemoembolization is often used for localized disease. In advanced stages, PD-L1 blockade has shown remarkable results in combination with VEGF blockade with bevacizumab over sorafenib (40), changing standard of care. In this disease scenario, considered to be off-limits for chemotherapy, the incorporation of moderate doses of chemotherapy to instigate anticancer immunity is to be explored to further increase efficacy.
PDAC
Metastatic and locally advanced PDAC remains a daunting challenge for clinical oncology. As mentioned, immunotherapy with checkpoint inhibitors has not yielded any valuable results, even in MSI-H cases (96, 97). Chemotherapy of different kinds offers very limited OS benefit (106). In the context of chemoimmunotherapy, a phase II clinical trial combining gemcitabine + nab-paclitaxel with or without durvalumab + tremelimumab has recently disclosed no PFS or OS benefit (107). However, there are reasons for hope because radiologic responses were achieved in 32% of 23 metastatic patients given a regimen encompassing pembrolizumab + 5-FU/leucovorin + Onyvide (liposomal pegylated irinotecan) chemotherapy together with an antagonist of the CXCR4 chemokine receptor (108). Further development of this strategy is warranted and should advance to earlier localized stages of this deadly disease.
Critical Perspective
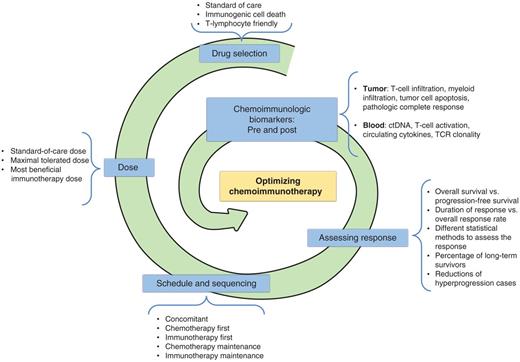
Chemoimmunotherapy combinations are changing several paradigms in clinical practice. This approach has been simple and consisted merely of standard-of-care chemotherapy regimens being added to immunotherapy and then being compared with chemotherapy plus placebo. Although this is the most feasible and convenient way to clinically develop this approach, we must remember that the elements in the combination have not been optimized at all. This means that doses, sequence of agents, drugs, and schedules are most likely suboptimal with much potential for improvement (Fig. 2). Knowing that chemotherapy was developed on the basis of a maximal tolerated dosing philosophy, it is likely that at such levels chemotherapy agents are causing some degree of immune cell toxicity. This could be affecting the long-term effects of immunotherapy working against the plateau of the tail in the survival curve, which is so dear to patients and physicians. Whenever possible, an immunotherapy-alone arm should be considered as an additional comparator in clinical trials to really ascertain the benefit of chemoimmunotherapy combinations.
Road map with the main points of improvement in chemotherapy approaches. Schematic representation of the main criteria and elements to further improve the efficacy of chemoimmunotherapy combinations. TCR, T-cell receptor.
Road map with the main points of improvement in chemotherapy approaches. Schematic representation of the main criteria and elements to further improve the efficacy of chemoimmunotherapy combinations. TCR, T-cell receptor.
To move forward, these issues should be reexamined in preclinical models testing the concept that, at least in certain cases, less chemotherapy in combination with immunotherapy might be conducive to better efficacy. Considering the mechanisms of synergy between chemotherapy and immunotherapy (Fig. 1), sequential approaches might be useful, and these need to be empirically developed in animal models and subsequently in clinical trials. In this regard, a detailed characterization in preclinical models of the profile of immune effects exerted by each chemotherapy agent should be undertaken as has been done for immunogenic cell death (18), but also considering direct or indirect effects on immune system cells.
Unconventional exploratory clinical trial designs can be undertaken, as has been done in the TONIC trial for metastatic TNBC, in which preconditioning chemotherapy and radiotherapy regimens were compared, followed by PD-1 blockade with nivolumab. This trial recruited small randomized cohorts of about 10 to 15 patients. Interestingly, doxorubicin showed better objective response rate (ORR) than cisplatin, radiotherapy, or cyclophosphamide (109). Furthermore, presurgical treatments will allow using pathologic responses and time-to-progression as potential surrogate endpoints to eventually determine patient survival benefit.
This issue of sequencing becomes further complicated by the advent of new immunotherapy agents that will be tested in the arena of the new chemoimmunotherapy standards of care. Nonetheless, concomitancy of treatments may allow chemotherapy to prevent cases of hyperprogression upon exposure to checkpoint inhibitors. This is particularly relevant considering that single-agent immunotherapy has been consistently associated with hyperprogressive disease in certain solid malignancies (110).
The role of surgery remains to be reexamined in the context of chemoimmunotherapy (111), because, contrary to general beliefs, debulking in metastatic stages may be beneficial for immunotherapy as a consequence of removing immunosuppressive factors dependent on tumor mass and reducing the amount of disease to be prey of the immune system.
In our opinion, chemoimmunotherapy regimens should advance to first-line treatment in a number of diseases at metastatic stages. The safety profile of chemoimmunotherapy will probably allow the development of combinations in neoadjuvant settings, in which reductions in chemotherapy intensity might be tested. Importantly, it should not be forgotten that improvements in ORR and PFS do not necessarily lead to longer OS, and ultimately the long-term tail under the Kaplan–Meier curve is the most striking value of immunotherapy, and unfortunately the one that potentially can be curtailed by chemotherapeutics.
It is of note that there are abundant reports from experience outside clinical trials that speak of the unexpected objective responses that do occur upon use of subsequent lines of chemotherapy in patients who had recently progressed to checkpoint inhibitors (68).
In chemoimmunotherapy trials, biomarker studies are to be encouraged, even as substudies in larger randomized studies. In our quest to make the most of chemoimmunotherapy, we need to exploit biomarkers in sequential blood and tumor samples. This should provide suitable pharmacodynamic parameters for optimization of dose, schedule, and drug regimens. For instance, benefit of nab-paclitaxel + atezolizumab in TNBC seemed to depend on PD-L1 expression in the tumor microenvironment (69). However, in NSCLC such a correlation is much weaker, and nonexistent for the combination of chemotherapy with pembrolizumab (53) and the combination of ipilimumab + nivolumab + chemotherapy (61). The room for future treatment individualization of chemoimmunotherapies is therefore huge.
All things considered, chemoimmunotherapy has arrived in the clinical setting and will stay for years to come. However, the field is to be considered in its infancy with regard to understanding mechanisms as well as to optimizing/individualizing treatments. Because of our imperfect knowledge, there will be mixtures of successes and failures in large randomized clinical trials. This overall strategy deserves attention back on the laboratory bench and in translational research-oriented clinical trials, because efficacy could most likely be further improved in a meaningful fashion.
Authors' Disclosures
D. Salas-Benito reports being employed at the clinical trial unit of Clínica Universidad de Navarra. J.L. Pérez-Gracia reports grants, personal fees, and non-financial support from Roche, BMS, MSD, and Seattle Genetics, grants and personal fees from Ipsen, grants from Eisai, Incyte, and Janssen outside the submitted work. M. Ponz-Sarvisé reports grants and personal fees from BMS and Roche and personal fees from Incyte outside the submitted work. I. Martínez-Forero reports personal fees from MSD during the conduct of the study. E. Castañón reports personal fees from AstraZeneca, Roche, BMS, and MSD outside the submitted work. M.F. Sanmamed reports grants from Roche outside the submitted work. I. Melero reports grants and personal fees from Roche, Alligator, AstraZeneca, Genmab, and Bristol Myers and personal fees from F-Star, Numab, Pharmamar, Gossamer, and Merck Serono outside the submitted work. No disclosures were reported by the other authors.
Acknowledgments
This work was supported by Miniserio de ciencia e innovación (SAF2017-83267-C2-1-R), Asociación Española contra el cáncer GCB15152947MELE, and PROCROP European commission HORIZON 2020. We are grateful for healthy discussion with Dr. Jesús San Miguel, Dr. Antonio González, Dr. Ignacio Gil Bazo, and Dr. Carlos de Andrea. Professional English editing by Dr. Paul Miller is also acknowledged.