Abstract
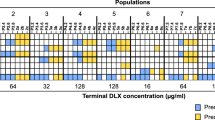
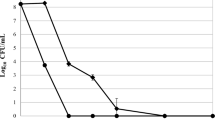
Daptomycin is an antibiotic used to treat infections caused by multidrug-resistant gram-positive pathogens. With increasing resistance to other antibiotics, an increase in daptomycin consumption is expected, which poses a potential threat of emergence of antibiotic resistance. These facts explain the need to study possible mechanisms for resistance emergence. In vitro selection of resistance to daptomycin in methicillin-resistant Staphylococcus aureus SA0420 of the ST239 genetic line was carried out. After 40 passages, the derivative strain was characterized by an increase in daptomycin minimum inhibitory concentration (MIC) from 1 to 64 µg/mL and a decrease in the doubling time and growth rate, while the induced autolytic activity did not change. During the selection and assessment of population diversity by the whole genome sequencing, both homo-mutations (nucleotide substitutions in 96–100% of reads after the alignment with the control genome at the particular position) and hetero-mutations (5‒95% of alternative reads) were revealed. After the fifth passage, the mutation in the S295L codon of the mprF gene was identified. The 40th passage revealed an additional mutation in the R50C codon; this mutation was not previously described. A new variant of the A214T mutation was detected in the Cls2 protein. The hetero-mutation in the Q493K codon of the walK regulatory gene associated with the cell wall was identified during the fifth passage and was not detected during further passaging. Hetero-mutations were also found in the ktrA and ntpA genes encoding the potassium uptake protein and phosphate transport protein, respectively. By the 40th passage of the selection, stop codons in the hypothetical gene yhfP (SACOL1927) were identified. Therefore, daptomycin resistance arises through the development of hetero-populations. After the 5th, 20th, and 40th passages, homo- and hetero-mutations in the genes with the proved role in the emergence of daptomycin resistance (mprF, cls2, and walK), as well as in the potential candidates (ktrA, ntpA, and yhfP), were revealed.


Similar content being viewed by others
REFERENCES
Turner, N.A., Sharma-Kuinkel, B.K., Maskarinec, S.A., et al., Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research, Nat. Rev. Microbiol., 2019, vol. 17, no. 4, pp. 203—218. https://doi.org/10.1038/s41579-018-0147-4
Steenbergen, J.N., Alder, J., Thorne, G.M., and Tally, F.P., Daptomycin: a lipopeptide antibiotic for the treatment of serious gram-positive infections, J. Antimicrob. Chemother., 2005, vol. 55, no. 3, pp. 283—291. https://doi.org/10.1093/jac/dkh546
Stefani, S., Campanile, F., Santagati, M., et al., Insights and clinical perspectives of daptomycin resistance in Staphylococcus aureus: a review of the available evidence, Int. J. Antimicrob. Agents, 2015, vol. 46, no. 3, pp. 278—289. https://doi.org/10.1016/j.ijantimicag.2015.05.008
Streit, J.M., Jones, R.N., and Sader, H.S., Daptomycin activity and spectrum: a worldwide sample of 6737 clinical Gram-positive organisms, J. Antimicrob. Chemother., 2004, vol. 53, no. 4, pp. 669—674. https://doi.org/10.1093/jac/dkh143
Duah, M., Daptomycin for methicillin-resistant Staphylococcus epidermidis native-valve endocarditis: a case report, Ann. Clin. Microbiol. Antimicrob., 2010, vol. 9. https://doi.org/10.1186/1476-0711-9-9
Hagiya, H., Sugawara, Y., Kimura, K., et al., Emergence of daptomycin non-susceptible coagulase-negative staphylococci in patients with cardiovascular device infections: two cases report investigated by whole genome analysis, Medicine (Baltimore), 2018, vol. 97, no. 49. https://doi.org/10.1097/MD.0000000000013487
Bertsche, U., Weidenmaier, C., Kuehner, D., et al., Correlation of daptomycin resistance in a clinical Staphylococcus aureus strain with increased cell wall teichoic acid production and D-alanylation, Antimicrob. Agents Chemother., 2011, vol. 55, no. 8, pp. 3922—3930. https://doi.org/10.1128/AAC.01226-10
Cafiso, V., Bertuccio, T., Purrello, S., et al., dltA overexpression: a strain-independent keystone of daptomycin resistance in methicillin-resistant Staphylococcus aureus,Int. J. Antimicrob. Agents, 2014, vol. 43, no. 1, pp. 26—31. https://doi.org/10.1016/j.ijantimicag.2013.10.001
Tran, T.T., Munita, J.M., and Arias, C.A., Mechanisms of drug resistance: daptomycin resistance, Ann. N.Y. Acad. Sci., 2015, vol. 1354, pp. 32—53. https://doi.org/10.1111/nyas.12948
Bayer, A.S., Schneider, T., and Sahl, H.G., Mechanisms of daptomycin resistance in Staphylococcus aureus: role of the cell membrane and cell wall, Ann. N.Y. Acad. Sci., 2013, vol. 1277, pp. 139—158. https://doi.org/10.1111/j.1749-6632.2012.06819.x
Jiang, J.H., Dexter, C., Cameron, D.R., et al., Evolution of daptomycin resistance in coagulase-negative staphylococci involves mutations of the essential two-component regulator WalKR, Antimicrob. Agents Chemother., 2019, vol. 63, no. 3. https://doi.org/10.1128/AAC.01926-18
Kang, K.M., Mishra, N.N., Park, K.T., et al., Phenotypic and genotypic correlates of daptomycin-resistant methicillin-susceptible Staphylococcus aureus clinical isolates, J. Microbiol., 2017, vol. 55, no. 2, pp. 153—159. https://doi.org/10.1007/s12275-017-6509-1
Cui, L., Isii, T., Fukuda, M., et al., An RpoB mutation confers dual heteroresistance to daptomycin and vancomycin in Staphylococcus aureus,Antimicrob. Agents Chemother., 2010, vol. 54, no. 12, pp. 5222—5233. https://doi.org/10.1128/AAC.00437-10
Hall, B.G., Acar, H., Nandipati, A., and Barlow, M., Growth rates made easy, Mol. Biol. Evol., 2014, vol. 31, no. 1, pp. 232—238. https://doi.org/10.1093/molbev/mst187
Gustafson, J.E., Berger-Bachi, B., Strassle, A., and Wilkinson, B.J., Autolysis of methicillin-resistant and -susceptible Staphylococcus aureus,Antimicrob. Agents Chemother., 1992, vol. 36, no. 3, pp. 566—572. https://doi.org/10.1128/aac.36.3.566
Brown, J., Pirrung, M., and McCue, L.A., FQC Dashboard: integrates FastQC results into a web-based, interactive, and extensible FASTQ quality control tool, Bioinformatics, 2017, vol. 33, no. 19, pp. 3137—3139 https://doi.org/10.1093/bioinformatics/btx373
Bolger, A.M., Lohse, M., and Usadel, B., Trimmomatic: a flexible trimmer for Illumina sequence data, Bioinformatics, 2014, vol. 30, no. 15, pp. 2114—2134. https://doi.org/10.1093/bioinformatics/btu170
Bankevich, A., Nurk, S., Antipov, D., et al., SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing, J. Comput. Biol., 2012, vol. 19, no. 5, pp. 455—477. https://doi.org/10.1089/cmb.2012.0021
Langdon, W.B., Performance of genetic programming optimized Bowtie2 on genome comparison and analytic testing (GCAT) benchmarks, BioData Min., 2015, vol. 8, no. 1. [pii]https://doi.org/10.1186/s13040-014-0034-034
Li, H., Handsaker, B., Wysoker, A., et al., The sequence alignment/map format and SAMtools, Bioinformatics, 2009, vol. 25, no. 16, pp. 2078—2087. https://doi.org/10.1093/bioinformatics/btp352
Barrick, J.E., Colburn, G., Deatherage, D.E., et al., Identifying structural variation in haploid microbial genomes from short-read resequencing data using breseq, BMC Genomics, 2014, vol. 15. https://doi.org/10.1186/1471-2164-15-1039
UniProt: a worldwide hub of protein knowledge, Nucleic Acids. Res., 2019, vol. 47, no. D1, pp. D506—D515. https://doi.org/10.1093/nar/gky1049
Roch, M., Gagetti, P., Davis, J., et al., Daptomycin resistance in clinical MRSA strains is associated with a high biological fitness cost, Front. Microbiol., 2017, vol. 8. https://doi.org/10.3389/fmicb.2017.02303
Li, S., Yin, Y., Chen, H., et al., Fitness cost of daptomycin-resistant Staphylococcus aureus obtained from in vitro daptomycin selection pressure, Front. Microbiol., 2017, vol. 8. https://doi.org/10.3389/fmicb.2017.02199
Ernst, C.M., Slavetinsky, C.J., Kuhn, S., et al., Gain-of-function mutations in the phospholipid flippase MprF confer specific daptomycin resistance, MBio, 2018, vol. 9, no. 6. https://doi.org/10.1128/mBio.01659-18
Peleg, A.Y., Miyakis, S., Ward, D.V., et al., Whole genome characterization of the mechanisms of daptomycin resistance in clinical and laboratory derived isolates of Staphylococcus aureus,PLoS One, 2012, vol. 7, no. 1. https://doi.org/10.1371/journal.pone.0028316
Bayer, A.S., Mishra, N.N., Chen, L., et al., Frequency and distribution of single-nucleotide polymorphisms within mprF in methicillin-resistant Staphylococcus aureus clinical isolates and their role in cross-resistance to daptomycin and host defense antimicrobial peptides, Antimicrob. Agents Chemother., 2015, vol. 59, no. 8, pp. 4930—4937. https://doi.org/10.1128/AAC.00970-15
Zhang, T., Muraih, J.K., Tishbi, N., et al., Cardiolipin prevents membrane translocation and permeabilization by daptomycin, J. Biol. Chem., 2014, vol. 289, no. 17, pp. 11584—11591. https://doi.org/10.1074/jbc.M114.554444
Howden, B.P., McEvoy, C.R., Allen, D.L., et al., Evolution of multidrug resistance during Staphylococcus aureus infection involves mutation of the essential two component regulator WalKR, PLoS Pathog., 2011, vol. 7, no. 11. https://doi.org/10.1371/journal.ppat.1002359
Gries, C.M., Bose, J.L., Nuxoll, A.S., et al., The Ktr potassium transport system in Staphylococcus aureus and its role in cell physiology, antimicrobial resistance and pathogenesis, Mol. Microbiol., 2013, vol. 89, no. 4, pp. 760—773. https://doi.org/10.1111/mmi.12312
Fahmi, T., Port, G.C., and Cho, K.H., c-di-AMP: an essential molecule in the signaling pathways that regulate the viability and virulence of gram-positive bacteria, Genes (Basel), 2017, vol. 8, no. 8. https://doi.org/10.3390/genes8080197
Kelliher, J.L., Radin, J.N., Grim, K.P., et al., Acquisition of the phosphate transporter NptA enhances Staphylococcus aureus pathogenesis by improving phosphate uptake in divergent environments, Infect. Immun., 2018, vol. 86, no. 1. https://doi.org/10.1128/IAI.00631-17
Cameron, D.R., Mortin, L.I., Rubio, A., et al., Impact of daptomycin resistance on Staphylococcus aureus virulence, Virulence, 2015, vol. 6, no. 2, pp. 127—131. https://doi.org/10.1080/21505594.2015.1011532
Muller, A., Grein, F., Otto, A., et al., Differential daptomycin resistance development in Staphylococcus aureus strains with active and mutated gra regulatory systems, Int. J. Med. Microbiol., 2018, vol. 308, no. 3, pp. 335—348. https://doi.org/10.1016/j.ijmm.2017.12.002
Good, B.H., McDonald, M.J., Barrick, J.E., et al., The dynamics of molecular evolution over 60000 generations, Nature, 2017, vol. 551, no. 7678, pp. 45–50. https://doi.org/10.1038/nature24287
Funding
This study was supported by the Russian Science Foundation, project no. 18-75-10114 (New Mechanisms of Resistance of Staphylococcus aureus to Beta-Lactam and Glycopeptide Antibiotics, Associated with Intracellular c‑di-AMP Messengers and Hetero-Resistance).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest. This article does not contain any studies involving animals or human participants performed by any of the authors.
Additional information
Translated by A. Panyushkina
Rights and permissions
About this article
Cite this article
Gostev, V.V., Sopova, Y.V., Kalinogorskaya, O.S. et al. Selection of Resistance to Daptomycin in Methicillin-Resistant Staphylococcus aureus: Role of Homo- and Hetero-Mutations. Russ J Genet 56, 289–297 (2020). https://doi.org/10.1134/S1022795420030060
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1022795420030060