Abstract
The development of specific drugs against SARS-CoV-2 infection is a major challenge facing global science and healthcare. Despite numerous attempts, there are still no truly effective drugs. Currently, the main approach in the creation of drugs against COVID-19 is repurposing, i.e., re-profiling existing drugs approved for medical use, for example, the use of a drug for the treatment of Ebola—Remdesivir, and the use of a drug for the treatment of influenza—Favipiravir. However, it is already obvious that these drugs are not specific enough nor effective enough. Another promising approach is the creation of new molecules, but it should be noted immediately that implementation requires much more time and costs. However, the search for new SARS-CoV-2 specific antiviral agents continues. The aim of our work was the creation of new 5-substituted uridine derivatives as potential inhibitors of coronavirus RNA-dependent RNA polymerase. The substances were obtained in high yields by the Suzuki‒Miyaura reaction and characterized using modern physicochemical methods. However, testing of their antiviral activity against SARS-CoV-2 did not reveal a significant inhibitory effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
COVID-19 is a highly contagious respiratory disease caused by SARS-CoV-2 betacoronavirus. After the first cases of the disease were reported in China at the end of December 2019, SARS-CoV-2 quickly spread around the world, which led to the development of a pandemic, as a result of which the death toll is approaching 5 million people [1]. Despite numerous studies that have led to a better understanding of the mechanisms of SARS-CoV-2 pathogenesis, this virus remains a worldwide problem. New outbreaks of this disease are observed due to the emergence and spread of mutant variants.
The structure and life cycle of SARS-CoV-2 are well studied [2, 3]. The major enzyme of viral replication—RNA-dependent RNA polymerase (RdRp, nsp12) functions as part of the replicase-transcriptase complex (RTC), which controls the synthesis of viral RNA [3]. The key role of RdRp in SARS-CoV-2 replication makes this enzyme an attractive therapeutic target, and the absence of its analogues in mammalian cells suggests potential high selectivity of inhibition. Currently, RdRp inhibitors that potentially have a pronounced antiviral activity are being intensively developed. The currently existing RdRp inhibitors fall into two main classes—nucleoside (NI) and non-nucleoside inhibitors (NNIs) binding at the active site and allosteric site, respectively [4].
The creation of NI is considered a promising strategy aimed at stopping viral RNA replication, due to the high degree of conservatism of active RdRp sites and the relatively low mutation rate in these regions, which should provide broad antiviral activity and a high threshold of resistance. The main mechanism of action of nucleoside analogs involves their intracellular conversion to the corresponding triphosphates, which, competing with the triphosphates of natural nucleosides, become terminator substrates for viral polymerases. For effective inhibition of viral RNA replication, the nucleotide analog inserted into the growing chain must not be cleaved due to the corrective activity characteristic of a significant proportion of polymerases, or the rate of its inclusion must be many times greater than the rate of cleavage. Antiviral NIs are divided into three types: obligate chain terminators, non-obligate chain terminators, and mutagenic. Obligate chain terminators do not contain a 3'-hydroxyl group in the riboside part of the molecule, which makes further elongation of the nucleotide chain impossible. Non-obligate chain terminators contain a natural base and a 3'-hydroxyl on the sugar residue, but they have an additional substituent at the C-1' or C-2' positions of the ribose ring, blocking the subsequent formation of a phosphodiester bond with the appropriate nucleoside triphosphate [5]. The mechanism of lethal mutagenesis is the inability to recognize nucleoside analogues as normal nucleotide bases, which causes mismatches in base pairing and an increase in the number of mutations, and ultimately leads to non-viable genomes.
The ability of many drugs initially targeting the RdRp of other RNA viruses such as Remdesivir (Ebola virus), Favipiravir (influenza virus), NHD EIDD-2801 (broad spectrum), and Sofosbuvir (hepatitis C virus) to inhibit SARS-CoV-2 has been evaluated [6]. Sofosbuvir is a highly active uridine nucleotide that specifically inhibits hepatitis C virus replication. The similarity of the hepatitis C virus and coronavirus replication cycles suggested that Sofosbuvir could be used in the treatment of COVID-19 [7]. Remdesivir was the first specific antiviral drug approved by the Association of European Universities for the treatment of patients with severe COVID-19. One of the main disadvantages of Remdesivir is the need for intravenous administration, which limits the widespread use of this drug and forces it to be used in a hospital setting. To change the situation, an inhaled form has been created, which is currently undergoing phase 1 clinical trials. A number of clinical studies have shown the effectiveness of Favipiravir in the treatment of COVID-19, however, animal experiments have revealed potential teratogenic activity of this drug [8]. However, Favipiravir is approved for use in a number of countries. Molnupiravir (EIDD-2801) is an oral, bioavailable prodrug, it is a nucleoside analogue of β-D-N4-hydroxycytidine, acting by the mechanism of lethal mutagenesis with a wide spectrum of action. N4-hydroxycytidine is more than 100 times more active than Ribavirin or Favipiravir against the SARS-CoV-2 coronavirus, and its antiviral activity correlates with the level of mutagenesis in viral RNA. Molnupiravir has been shown to be safe in phase 1 clinical trials and clinical trials are ongoing. However, the ability of N4-hydroxycytidine cause genomic mutations in human cells in vitro has been shown [9].
Thus, at the moment there is no highly effective and specific drug against SARS-CoV-2, therefore, the immediate creation of new agents aimed at inhibiting the activity of RdRp coronavirus is extremely important. Our work describes the synthesis and determination of the antiviral activity of six 5-substituted uridine derivatives.
EXPERIMENTAL
In the study we used 5-bromouridine (Sigma, United States), high purity boronic acids and solvents (Acros, Belgium). Column chromatography was carried out on reverse-phase LiChroprep media RP-18, eluted with water. NMR spectra were recorded on an AMX III-400 spectrometer (Bruker, USA) with an operating frequency of 400 MHz for 1H (Me4Si as an internal standard for organic solvents and sodium 3‑(trimethylsilyl)-1-propanesulfonate (DSS) for D2O) and 100.6 MHz for 13C NMR (with suppression of carbon-proton interaction). The reaction progress was monitored by TLC on Kieselgel 60 F254 plates (Merck, Germany), eluted with dioxane-25% aqueous NH3 (4 : 1).
General procedure for the preparation of compounds 1a–g. A solution of boronate (1 eq.) in THF (4 mL) was added to 5-bromouridine dissolved in a mixture of water (4 mL) and methanol (2 mL) and purged with argon. Tetraxy(triphenylphosphine)palladium catalyst (0.1 eq.) and sodium hydroxide (10 eq.) were added. The reaction mass was boiled for 7 h, then evaporated, dissolved in chloroform (15 mL) and was extracted with water (15 mL). The aqueous fraction was washed with chloroform (2 × 5 mL), concentrated, and the target substance was isolated by column chromatography on RP-18, eluted with water. Product output of 1a–g amounted to 37–59%.
1-((2R,3R,4S,5R)-3,4-Dihydroxy-5-(hydroxymethyl) tetrahydrofuran-2-yl)-5-(pyridin-2-yl)pyrimidin-2,4(1H,3H)-dione (1a) light yellow crystals, 41% 1H NMR (CD3OD): 3.76–3.95 (2H, m, H'5), 4.06–4.08 (1H, m, H4′), 4.25–4.28 (2H, m, H3′, H2'), 5.98–5.99 (1H, d, H1′), 7.43–7.47 (1H, m, H5 Py), 8.06–8.10 (1H, m, H4 Py), 8.44–8.46 (1H, d, H6 Py), 8.49 (1H, s, H6), 8.77–8.78 (1H, d, H2 Py). 13C NMR (D2O): 60.13, 68.90, 74.08, 83.73, 90.03, 112.46, 123.94, 130.12, 137.44, 139.19, 147.62, 147.98, 155.05, 169.10.
5-(3-Aminophenyl)-1-((2R,3R,4S,5R)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)pyrimidin-2,4(1H,3H)-dione (1b) gray crystals, 37% 1H NMR (CD3OD): 3.77–3.87 (2H, m, H5′), 4.02–4.04 (1H, m, H4′), 4.19–4.27 (2H, m, H3′, H2′), 5.96–5.98 (1H, d, H1′), 6.63–6.67 (1H, m, Ph), 6.89–6.96 (2H, m, Ph), 7.06–7.11 (1H, d, Ph), 7.92 (1H, s, H6). 13C NMR (D2O): 60.52, 69.24, 73.91, 83.65, 89.93, 115.55, 116.35, 116.54, 129.41, 135.44, 138.07, 146.09, 157.63, 172.64.
5-(4-Aminophenyl)-1-((2R,3R,4S,5R)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)pyrimidin-2,4(1H,3H)-dione (1c) beige crystals, 39% 1H NMR (CD3OD): 3.71–3.90 (2H, m, H5′), 4.00–4.02 (1H, m, H4′), 4.18–4.27 (2H, m, H3′, H2′), 5.95–5.97 (1H, d, H1′) , 6.72–6.75 (2H, m, Ph), 7.28–7.33 (2H, m, Ph), 7.82 (1H, s, H6). 13C NMR (CD3OD): 60.38, 69.26, 74.00, 83.81, 90.15, 114.39 × 2, 122.53, 128.55 × 2, 130.78, 135.88, 148.32, 150.88, 165.91.
4-(1-((2R,3R,4S,5R)-3,4-Dihydroxy-5-(hydro-xymethyl)tetrahydrofuran-2-yl)-2,4-dioxo-1,2,3,4-tetrahydropyrimidine- 5-yl)benzamide (1d) yellow crystals, 53% 1H NMR (D2O): 3.72–3.91 (2H, m, H5′), 4.06–4.10 (1H, m, H4′), 4.20–4.24 (1H, t, H3′), 4.30–4.33 (1H, t, H2′), 5.93–5.94 (1H, d, H1′), 7.52–7.56 (2H, m, Ph), 7.77–7.80 (2H, m, Ph), 7.92 (1H, s, H6). 13C NMR (D2O): 56.95, 59.84, 66.08, 73.54, 83.07, 89.60, 114.88, 127.01, 128.33, 130.84 × 2, 138.32, 138.45, 157.62, 163.24, 172.51.
N-(4-(1-((2R,3R,4S,5R)-3,4-Dihydroxy-5-(hydro-xymethyl)tetrahydrofuran-2-yl)-2,4-dioxo-1,2,3,4-tetrahydropyrimidin-5-yl)phenyl)acetamide (1e) white crystals, 57% 1H NMR (D2O): 2.13 (3H, s, CH3), 3.71–3.88 (2H, m, H5′), 4.04–4.08 (1H, m, H4′), 4.18–4.22 (1H, t, H3′), 4.29–4.32 (1H, t, H2′), 5.92–5.94 (1H, d, H1′), 7.39 (4H, s, Ph), 7.78 (1H, s, H6). 13C NMR (D2O): 22.34, 56.93, 60.00, 68.70, 73.40, 83.08, 89.46, 115.41, 121.28, 128.25, 128.87, 129.25, 135.52, 137.57, 158.13, 165.77, 172.49.
4-(1-((2R,3R,4S,5R)-3,4-dihydroxy-5-(hydro-xymethyl)tetrahydrofuran-2-yl)-2,4-dioxo-1,2,3,4-tetrahydropyrimidine-5-yl)-N-methylbenzamide (1g) white crystals, 54% 1H NMR (D2O): 2.91 (3H, s, CH3), 3.73–3.92 (2H, m, H5′), 4.06–4.11 (1H, m, H4′), 4.21–4.25 (1H, t, H3′), 4.31–4.34 (1H, t, H2′), 5.94–5.95 (1H, d, H1′), 7.51–7.55 (2H, m, Ph), 7.71–7.73 (2H, m, Ph), 7.91 (1H, s, H6). 3C NMR (D2O): 26.39, 48.90, 60.31, 69.05, 74.05, 83.57, 90.08, 115.38, 127.01, 127.52, 128.84, 138.25, 138.79, 157.81, 163.24, 171.13, 172.67.
Study of antiviral activity. Stock solutions of test compounds at a concentration of 5 μM were prepared in 100% DMSO.
Antiviral activity was evaluated on the SARS-CoV-2 strain PIK35 (GISAID ID EPI_ISL_428851). The vero green monkey kidney cell line was obtained from Biologicals, WHO, Switzerland (RCB 10-87). Cells were cultured in DMEM medium (Chumakov Federal Scientific Center for Research and Development of Immune-and-Biological Products, RAN, Russia) with fetal bovine serum (Gibco, United States, 5%), streptomycin (0.1 mg/mL), and penicillin (100 U/mL) (PanEco, Russia).
The technique for assessing antiviral activity was described earlier [10]. Eight twofold dilutions of stock solutions of compounds in DMEM medium (Chumakov Federal Scientific Center for Research and Development of Immune-and-Biological Products, RAN, Russia), were mixed with equal volumes of a viral suspension containing 50–200 TCD50 per well, and incubated for 1 h at 37°C. Next, virus–compound mixtures were added to Vero cell monolayers in duplicate. The cytopathic effect (CPE) was assessed microscopically after 5 days of incubation at 37°C. EU50 values calculated by the Kerber method. The experiment was repeated at least 2 times with each compound. N4-hydroscycytidine was used as the positive control, DMSO was used as the negative control, and the virus dose was regulated by titration.
RESULTS AND DISCUSSION
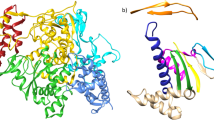
Earlier, a group of scientists led by K. Seley-Radtke developed a new type of modified nucleosides bearing flexible or “cleaved” analogues of purine bases, called fleximers [10]. The heterocyclic bases of fleximers consist of imidazole and pyrimidine rings linked by a single carbon-carbon bond, rather than being fused, as in conventional purines (Fig. 1). As a result, the nitrogenous base retains the necessary hydrogen bonds and aromatic properties that are required for recognition, while gaining the flexibility to adapt to the enzyme binding site and potential mutations. It has been shown that such compounds are able to inhibit the replication of HCoV-NL63 and MERS-CoV coronaviruses in cell culture [11, 12]. The idea of fleximer compounds was developed further in the form of the synthesis of “reverse” fleximers (Fig. 1), in which the backbone of the purine base is connected to the sugar moiety at N-3 of the pyrimidine ring, rather than N-9 of the imidazole ring. This changes the conformation of the fleximer base, which can also be considered as a C5-substituted pyrimidine [13]. In continuation of these works, we decided to synthesize a series of 5‑substituted uridine derivatives (1a–g), which can be considered as reverse fleximers, in the hope of obtaining substances with antiviral activity against SARS-Cov-2. To obtain target compounds, we considered various modern methods for creating C-C bonds.
Palladium catalysis plays a key role in the synthesis of complex organic molecules using cross-coupling reactions. The longstanding interest in this area is due to two main reasons. First, such catalytic systems make it easy to create carbon–carbon and carbon–nitrogen bonds under stable conditions with excellent yields. Second, the mild reaction conditions make it possible to carry out synthesis requiring selective binding of molecules in certain positions without affecting other functional groups [14].
Although palladium-catalyzed cross-coupling reactions are well known for a wide range of compounds, a number of difficulties arise in the case of nucleosides. In addition to the problems caused by cross-linking of multifunctional heterocyclic substrates, the polar nature of nucleoside derivatives often leads to their poor solubility in typical organic solvents [15]. One of the common approaches to eliminate this drawback is the protection of the hydroxyl groups of the carbohydrate moiety in order to obtain a more hydrophobic substrate. This method includes two additional synthesis steps, resulting in a lower yield. A more attractive approach is the use of unprotected nucleoside, nucleotide or oligonucleotide derivatives in cross-coupling reactions. This can be achieved with polar organic solvents. Nucleosides and nucleotide derivatives dissolve efficiently in water or in combination with organic solvents, which makes it possible to carry out reactions under homogeneous conditions without the need for protective groups [15].
Variants of the Suzuki–Miyaura reaction with unprotected nucleoside halides in various systems of water and cosolvents have been described. E.C. Western et al. [16] arylated 5-iodo-2-deoxyuridine in the presence of catalysts (tri-(4,6-dimethyl-3-sulfonatophenyl)phosphine and palladium acetate) in a 2 : 1 water–acetonitrile solvent system. The first stage of the synthesis of a uridine derivative using the Suzuki cross-coupling reaction between 5-iodo-2-deoxyuridine and 4-formylphenylboronic acid in a 5:1 methanol–water mixture was also described in the presence of tetrakis (triphenylphosphine)palladium catalyst [17]. Despite the insolubility of triphenylphosphine in water, it was shown [18] that the reaction between arylboronic acids and 5-iodo-2-deoxyuridine in water as the only solvent is successfully catalyzed by Pd(OAc)2/PPh3 at 120°C using microwave radiation.

Scheme 1. Synthesis of the 5-substituted uridine derivatives 1a–1g.
Based on the analysis of published data for the Suzuki–Miyaura reaction between 5-bromouridine and various boronates (Scheme 1), the solvent system H2O/MeOH / THF = 2: 1 : 2. After isolation and purification by ion-exchange chromatography, the biological activity and cytotoxicity of the synthesized substances were evaluated. Antiviral activity was determined by the ability of the test compounds to inhibit the death of Vero cells infected with the SARS-CoV-2 strain PIK35. N4-hydroxycytidine (EC50 > 5 µM) was used as the positive control. However, compounds 1a–g did not show the expected inhibitory effect (EC50 > 100 µM). Obviously, for effective suppression of SARS-CoV-2, a modification of the structure of the compounds is required. The activity of compounds 1a–g against other viral pathogens is currently being studied.
REFERENCES
Cascella M., Rajnik M., Aleem A., Dulebohn S., Di Napoli R. 2021. Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls.
Santos I.A., Grosche V.R., Bergamini F.R.G., Sabino-Silva R., Jardim A.C.G. 2020. Antivirals against coronaviruses: Candidate drugs for SARS-CoV-2 treatment? Front. Microbiol. 11, 1818.
Lei T., Qiang T., Liang C., Ren X., Jia M., Zhang J., Li J., Wan M., YuWen X., Li H., Cao W., Liu H. 2021. RNA-dependent RNA polymerase (RdRp) inhibitors: The current landscape and repurposing for the COVID-19 pandemic. Eur. J. Med. Chem. 213, 113201.
Cannalire R., Cerchia C., Beccari A.R., Di Leva F.S., Summa V. 2020. Targeting SARS-CoV-2 proteases and polymerase for COVID-19 treatment: State of the art and future opportunities. J. Med. Chemi. acs.jmedchem.0c01140. https://doi.org/10.1021/acs.jmedchem.0c01140
De Clercq E., Neyts J. 2009. Antiviral agents acting as DNA or RNA chain terminators. Antiviral Strategies. 189, 53‒84.
Buonaguro L., Tagliamonte M., Tornesello M.L., Buonaguro F.M. 2020. SARS-CoV-2 RNA polymerase as target for antiviral therapy. J. Transl. Med. 18 (1), 185. https://doi.org/10.1186/s12967-020-02355-3
Ju J., Li X., Kumar S., Jockusch S., Chien M., Tao C., Morozova I., Kalachikov S., Kirchdoerfer R.N., Russo J.J. 2020. Nucleotide analogues as inhibitors of SARS-CoV polymerase. Pharmacol. Res. Perspect. 8 (6), e00674.
Al-Horani R.A., Kar S. 2020. Potential anti-SARS-CoV-2 therapeutics that target the post-entry stages of the viral life cycle: A comprehensive review. Viruses. 12 (10), 1092‒1134.
Zhou S., Hill C.S., Sarkar S., Tse L.V., Woodburn B.M.D., Schinazi R.F., Sheahan T.P., Baric R.S., Heise M.T., Swanstrom R. 2021. β-DN 4-hydroxycytidine (NHC) inhibits SARS-CoV-2 through lethal mutagenesis but is also mutagenic to mammalian cells. J. Infect. Dis. 224 (3), 415‒419.
Seley-Radtke K. 2018. Flexibility—not just for yoga anymore! Antivir. Chem. Chemother. 26, 2040206618756788.
Matyugina E.S., Novikov M.S., Kozlovskaya L.I., Volok V.P., Shustova E.Yu., Ishmukhametov A.A., Kochetkov S.N., Khandazhinskaya A.L. 2021. Assessment of the antiviral potential of modified heterocyclic bases and 5′-norcarbocyclic nucleoside analogs with respect to SARS-CoV-2. Acta Naturae, 13 (4), 51‒54.
Peters H.L., Jochmans D., de Wilde A.H., Posthuma C.C., Snijder E.J., Neyts J., Seley-Radtke K.L. 2015. Design, synthesis and evaluation of a series of acyclic fleximer nucleoside analogues with anti-coronavirus activity. Bioorg. Med. Chem. Lett. 25 (15), 2923‒2926.
Zimmermann S.C., Sadler J.M., O’Daniel P.I., Kim N.T., Seley-Radtke K.L. 2013. “Reverse” carbocyclic fleximers: Synthesis of a new class of adenosine deaminase inhibitors. Nucleosides, Nucleotides Nucl. Acids. 32 (3), 137‒154.
Polshettiwar V., Decottignies A., Len C., Fihri A. 2010. Suzuki–Miyaura cross-coupling reactions in aqueous media: Green and sustainable syntheses of biaryls. ChemSusChem. 3 (5), 502–522.
Shaughnessy K.H. 2015. Palladium-catalyzed modification of unprotected nucleosides, nucleotides, and oligonucleotides. Molecules. 20 (5), 9419–9454.
Western E.C., Daft J.R., Johnson E.M. 2nd, Gannett P.M., Shaughnessy K.H. 2003. Efficient one-step Suzuki arylation of unprotected halonucleosides, using water-soluble palladium catalysts. J. Org. Chem. 68 (17), 6767–6774.
Okamoto A., Inasaki T., Saito I. 2005. Synthesis and ESR studies of nitronyl nitroxide-tethered oligodeoxynucleotides. Tetrahedron Lett. 46 (5), 791–795.
Fresneau N., Hiebel M.A., Agrofoglio L.A., Berteina-Raboin S. 2012. Efficient synthesis of unprotected C-5-aryl/heteroaryl-2'-deoxyuridine via a Suzuki–Miyaura reaction in aqueous media. Molecules. 17 (12), 14409–14417.
Funding
The study was financially supported by the Russian Foundation for Basic Research within project No. 20-04-60414 and the Ministry of Science and Higher Education of the Russian Federation (state assignment on the topic “Analogues of Nucleic Acid Components as Potential Inhibitors of Coronaviruses”). The study of the physicochemical properties of the products was carried out with the support of the Russian Science Foundation no. 19-74-10048.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests. The authors declare they have no conflicts of interest.
This study does not contain any research involving humans or animals as research objects.
Rights and permissions
About this article
Cite this article
Maslova, A.A., Matyugina, E.C., Shustova, E.Y. et al. New Analogues of Uridine as Possible Anti-Viral Agents Specific to SARS-CoV-2. Mol Biol 56, 469–473 (2022). https://doi.org/10.1134/S0026893322030098
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0026893322030098