Abstract
This review is devoted to the 100-year history of the investigation of peptide hormones and the creation of drugs on their basis, starting from the insulin discovery and its introduction into a medical practice in 1921. The basic groups of the peptide hormones are discussed: neurohypophyseal hormones, hypothalamic releasing hormones, incretins, insulin, adrenocorticotropic hormone (ACTH), and calcitonin. The first therapeutic agents based on the peptide hormones were created by a traditional approach that involved the isolation of peptides from animal tissues, their purification to individual compounds, determination of their primary structure, their chemical synthesis or their deep purification, and the creation of a pharmaceutical substance. A modern approach to creation of peptide hormone drugs is based on their consideration as ligands of the corresponding cellular receptors and the use of computer modeling, efficient synthesis methods, and high-throughput screening. The combination of these methods enabled the development of analogs which would be more active than the corresponding natural compounds, exhibit other activities in addition to the hormonal regulation, and be resistant to biodegradation. Such therapeutic agents have been designed on the basis of agonistic and antagonistic analogs of somatostatin and luliberin, and have found wide application in hormonal regulation and cancer treatment. Over the past two decades, the glucagon-like peptide (GLP-1) has been intensively investigated as a potential therapeutic agent. In our review, we describe modifications which resulted in the most highly effective long-acting drugs. Now, natural hormones and their analogs are widely present in the pharmaceutical market.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
TABLE OF CONTENTS
INTRODUCTION
CLASSICAL HORMONAL PEPTIDE DRUGS
HYPOTHALAMIC RELEASING HORMONES AND THEIR ANALOGS
ANALOGS OF THE GLUCAGON-LIKE PEPTIDE-1
CONCLUSIONS
REFERENCES
INTRODUCTION
Peptide drugs occupy an important place in the modern pharmaceutical industry. They are diverse, from the modified lisinopril dipeptide (the known hypotensive agent) to insulin (the irreplaceable medicine for a treatment of the type I diabetes). Peptides are important regulators of the functioning of nearly all living organisms, starting from protozoa. These compounds are signal molecules for many physiological functions, thus, they can correct a wide spectrum of biological processes of an organism. Earlier, peptides were generally used for hormonal replacement therapy that restored the peptide level in cases where natural production is reduced or discontinued. Nowadays, the extent of peptide application is much wider. Peptide hormones were initially used in medicine in the first half of the 20th century. The fundamental event was the isolation and purification of insulin in 1921.
The use of peptides as therapeutic agents has evolved with time and is developing along with progress in biochemistry, molecular biology, and medicine. Two main periods can be distinguished in the process of the discovery and development of peptide hormonal drugs [1–3]. The first one is associated with traditional approaches that involve isolation of peptides from animal tissues, their purification to individual compounds, determination of their primary structure, their chemical synthesis or deep purification, and, finally, creation of a pharmaceutical agent. The propagation of peptide therapy was limited by such properties of the natural peptides as their short half-life in blood plasma and low peroral bioavailability. The short half-life period of many peptide hormones is explained by the action of many peptidases and excretory processes which inactivate and remove the peptides. This property is responsible for a rapid modulation of the hormonal level in an organism to maintain homeostasis, but presents a serious problem in the development of therapeutic drugs.
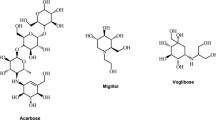
The modern approach to creation of the peptide drugs is associated with the development of molecular biology. Information on the genome provides a possibility of cloning genes which encode therapeutically important biological targets and express their protein products. This approach is based on a consideration of the ligand–receptor interaction as a universal method of the information transduction by cells and tissues of an organism. The structural correspondence necessary for the protein-target binding serves as the main criterion for a design of the peptides with therapeutic potential. This approach also involves modifications of the ligand structures to increase their resistance to biodegradation and their activity in comparison with the natural analogs. In addition, large combinatorial libraries of organic substances and highly efficient screening technologies allow the creation of small nonpeptide molecules which are targeted to peptide receptors [3, 4]. These compounds are usually more suitable for peroral administration and are more easily produced than peptides. However, such an approach does not displace the peptide compounds, their use in medicine is only expanding. Undoubtedly, the most important factor in progress in the field of therapeutic agents of the peptide nature is the introduction of new methods for peptide production, such as automated solid-phase peptide synthesis and gene-engineering technologies.
CLASSICAL HORMONAL PEPTIDE DRUGS
The first peptide on the basis of which the important therapeutic agent was created was insulin. It is a peptide hormone that consists of 51 amino acid residues. Insulin is produced by the β-cells of the islets of Langerhans, which are formations in the pancreas, and regulates biosynthesis and consumption of glucose by cells. This hormone was first isolated from pig pancreas 100 years ago by Banting et al. [5]. As soon as the capability of insulin isolated from animals to regulate glucose consumption was confirmed, the medicinal drug based on purified animal insulin was created, though the insulin structure remained unknown for more than 30 years. Sanger et al. determined the primary structure of insulin only in 1954 (Fig. 1) [6, 7]. Insulin consists of two polypeptide chains connected by two disulfide bridges. The third bridge is placed in the A-chain between Cys6 and Cys11. Generally, insulin serves as a good marker for the development of biochemistry. Many landmarks of insulin research are marked by Nobel Prizes. In 1923, F.G. Banting and J.J.R. Macleod received the Nobel Prize in the field of physiology and medicine. For the determination of the primary structure of insulin, F. Sanger was awarded the Nobel Prize in 1958, and D. Hodgkin received the Nobel Prize in 1964 for the development of crystallographic studies and the determination of the spatial structure of insulin [8].
The chemical structure of insulin [8].
The MarketsandMarkets analytical company priced the world market of human insulin drugs at about 25 billion US dollars in 2018, and a tendency of permanent growth is observed [9]. Now, three major producers of insulin (Eli Lilly, Novo Nordisk, and Sanofi) control 96% of the insulin world market. Nowadays, most of the insulin drugs are produced by the gene-engineering technologies using recombinant plasmids carrying the proinsulin synthetic gene, which are incorporated into bacterial or yeast producer strains. Proinsulin is expressed by bacteria or yeasts and is converted to insulin by enzymatic hydrolysis. The so-called semisynthetic insulin drugs, whose amino acid sequence has been changed to correspond to human insulin, are prepared from a hormone isolated from the pancreas of animals. Insulin structural analogs with different duration of action have been created along with natural insulin. Such insulin drugs are widely represented in the pharmaceutical market [10]. The importance of insulin research can scarcely be overestimated. Insulin is considered to have opened a new stage of targeted replacement therapy. The insulin discovery has signified the end of the so-called preinsulin era and paved the way for new therapeutic approaches [11].
The most important hormonal peptide therapeutic agents that were mainly created on the basis of the “classic” approaches are listed in Table 1 [2].
Several drugs were isolated and introduced into the clinical practice as a result of studies of a relationship of the hormonal and nervous systems and regulation of the synthesis and release of the adenohypophysis hormones by the central nervous system. The first of these drugs is adrenocorticotropic hormone (ACTH). ACTH consists of 39 amino acid residues and has the following amino acid sequence: Ser-Tyr-Ser-Met-Glu-His-Phe-Arg-Trp-Gly-Lys-Pro-Val-Gly-Lys-Lys-Arg-Arg-Pro-Val-Lys-Val-Tyr-Pro-Asn-Gly-Ala-Glu-Asp-Glu-Ser-Ala-Glu-Ala-Phe-Pro-Leu-Glu-Phe. It stimulates secretion of glucocorticoid hormones from the adrenal cortex. ACTH was isolated from the bovine hypophysis in 1942 [12], and the therapeutic agent based on it was created in 1950s [2, 13]. The biologically active 1–24 fragment of ACTH was synthesized in 1960s. Both natural and synthetic adrenocorticotropic hormones are applied to the treatment of rheumatism, polyarthritis, podagra, bronchial asthma, eczema, the hormonal disorders that are associated with insufficient ACTH production and the adrenal cortex dysfunction (Addison’s disease and Cushing’s syndrome), and other diseases [14]. This hormone is also used in diagnostic kits for a determination of the ACTH content by enzyme immunoassay methods. The ACTH level is a marker of not only hormonal disorders but the hormone-dependent cancers as well. Based on the ACTH structure, short peptides with an action spectrum radically distinct from that of the original hormone have been created. The Semax peptide (Met-Glu-His-Phe-Pro-Gly-Pro) should be first to be mentioned. Semax was a Russian drug that was introduced into medicine in 1997 [15]. Semax was created on the basis of the ACTH4–10 fragment, consisting of the 4–7 fragment of ACTH (Met-Glu-His-Phe) and the Pro-Gly-Pro sequence, which increased the Semax resistance to enzymatic hydrolysis and its nootropic activity tenfold in comparison with the natural ACTH4–10. This drug was completely deprived of hormonal activity, but exhibited a wide spectrum of nootropic and adaptive properties. Semax is used for the treatment of stroke, transient ischemic attack, memory and cognitive disorders, gastric ulcers, diseases of the optic nerve, and also for strengthening the immune system [16, 17].
At the beginning of the 1960s, the calcitonin 32‑member peptide hormone was isolated in a pure form [18]. Calcitonin is secreted by the parafollicular cells of the thyroid glands of humans and other animals. This hormone decreases the calcium content in blood, and this effect is opposite to that of the parathyroid hormone. Calcitonin has the following primary structure: Cys-Gly-Asn-Leu-Ser-Thr-Cys-Met-Leu-Gly-Thr-Tyr-Thr-Gln-Asp-Phe-Asn-Lys-Phe-His-Thr-Phe-Pro-Gln-Thr-Ala-Ile-Gly-Val-Gly-Ala-Pro(S–S1–7). It involves the 7-member cycle that is formed by the disulfide bond between Cys1 and Cys7. For the first time, the calcitonin drug was created on the basis of the hormone from salmon thyroid glands: Cys-Ser-Asn-Leu-Ser-Thr-Cys-Val-Leu-Gly-Lys-Leu-Ser-Gln-Glu-Leu-His-Lys-Leu-Gln-Thr-Tyr-Pro-Arg-Thr-Asn-Thr-Gly-Ser-Gly-Thr-Pro(S–S1–7). The salmon calcitonin more actively regulates the human calcium metabolism than the human calcitonin in spite of a considerable difference in their structures (16 amino acid residues of 32 are different).
Currently, only synthetic calcitonin serves as a substrate for the therapeutic agent. This calcitonin is prepared using recombinant DNA or by solid phase synthesis. Elcatonin is a calcitonin-relative drug, the analog of eel calcitonin which contains the stable C–N bond in its 7-member cycle instead of the S–S bond [19]. Calcitonin medicines are used for treatment of hypercalcemia and osteoporosis. They inhibit adsorption and autolysis of bones, and, thus, result in a decrease in the calcium content in blood, prevent the solution and transfer of bone salts, facilitate the excretion of calcium and phosphorus with urine, inhibit readsorption of calcium, phosphorus, and sodium in the renal tubules, and support the normal calcium level in blood.
A traditional approach to a design of the peptide drugs was continued by studies of oxytocin and vasopressin. These compounds are neurohypophyseal peptide hormones produced in the hypothalamus and are secreted into the neurohypophysis and, further, into the bloodstream. Du Vigneaud et al. were the first who isolated these compounds from the posterior lobe of the hypophysis and determined the structures of both hormones [20, 21]. The Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly-NH2(S–S1–6) oxytocin peptide and the Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2(S–S1–6) vasopressin peptide consist of nine amino acid residues and contain the 6-member cycle formed by the disulfide bond between Cys1 and Cys6. The content of these hormones in the brain tissues is insignificant, and, therefore, their preparative isolation is completely unprofitable. Therefore, oxytocin was the first synthetic peptide hormone and the first synthetic peptide substance of the peptide drug. Du Vigneaud et al. performed the chemical synthesis of oxytocin and vasopressin in 1953 [22, 23]. The oxytocin medicine was introduced into clinical practice in 1962 and, since that time, oxytocin was used in medicine as a stimulator of the smooth muscle contraction and an irreplaceable agent for obstetrics in gynecology and veterinary medicine. Vasopressin is known as a hormone that regulates the water–salt metabolism and blood pressure. Medicines for treatment of diabetes insipidus were also created based on the vasopressin substance.
Nowadays, the role of oxytocin and vasopressin is not limited to hormonal regulation. These peptides are evolving components of the oxytocin–vasopressin integrated adaptive system. The more ancient vasopressin peptide supports individual survival and plays a role in defensive behavior, including mobilization and aggression. Oxytocin is associated with positive social behavior and can be considered as a biological metaphor of a social attachment and love [24]. The vasopressin influences human biorhythms has also been found; this peptide is directly involved in regulation of the circadian cycle of the suprachiasmatic nucleus of the hypothalamus [25].
The studies of vasopressin, oxytocin, and their antagonists and agonists have reached a new level after a discovery of their receptors and determination of the receptor structures. Oxytocin and vasopressin mediate their biological effects (hormonal and adaptive) through an interaction with the specific receptors like nearly all peptide hormones. Three types of the vasopressin receptors (V1aR, V1bR, and V2R) and one oxytocin receptor (OTR) are known [26, 27]. They belong to the G-protein-coupled receptor family and are found in many organs and tissues. The wide occurrence and variability of these receptors explain the multifunctionality of the neurohypophyseal hormones [28, 29]. Two other atypical receptors that exhibited an affinity to arginine-vasopressin and mediate intracellular responses to this hormone were discovered later: the angiotensin-vasopressin receptor (AngII/AVP) and the calcium immobilization receptor-1 (VACM-1) [30, 31]. It is interesting that the sequences of both receptors differ from those of the vasopressin receptor family, but their location is similar to that of V1aR and V1bR [30]. In addition, AngII/AVP has been found to have a high affinity to antagonists of the V1-receptors, and VACM-1 can distinguish vasopressin and oxytocin [30–32]. The discovery of the receptors and the determination of their structures gave rise to a novel approach to a design of analogs of the neurohypophyseal hormones and an appraisal of the previously synthesized analogs. To date, several thousand peptide and nonpeptide analogs (agonists and antagonists) of vasopressin and oxytocin were synthesized [33, 34]. Many of them are highly selective and effective. However, only seven peptides and two nonpeptide agonists are approved for medicinal use in the United States according to data of the Manning Laboratory, which is a leader in this area (data on 2012, Table 2) [34].
In Russia, vasopressin drugs of the natural structure are allowed and predominantly used for treatment of diabetes insipidus. Drugs based on desmopressin are also used. Desmopressin is the structural analog of vasopressin with the deaminated residue of Cys1 and the replacement of L-Arg by D-Arg in position 8. These modifications considerably increase the enzymatic resistance of the peptide and change its preceptor specificity. Desmopressin selectively activates the V2-receptors and has no influence on the V1-receptors of the smooth-muscle cells of vessels and internal organs. As a result, the ratio of the antidiuretic activity and the pressor action is 2000 : 1 in comparison with that of arginine-vasopressin (1 : 1) [35]. The enzymatic resistance of desmopressin allows its application in tablet form and as a nasal spray.
The injection forms of oxytocin of the natural structure and desaminooxytocin (the deaminated analog of oxytocin) are widely used in gynecology. The intranasal spray of oxytocin is also allowed for use in Russia [35]. At present, studies of the peptides of the oxytocin and vasopressin family are generally aimed at the creation of the compounds which have no hormonal activity but selectively affect the different CNS functions. The peptides which are structurally related to vasopressin and oxytocin are examined as potential therapeutic agents for the treatment of the autism and anxiety disorders, for stimulation of memory and teachability, and as the adaptive drugs in surgery [36–38]. Activation of the vasopressin system is considered to play an important role in the prophylaxis and treatment of cognitive disorders during the Alzheimer’s disease [39]. Systems of oxytocin and vasopressin are of interest as potential targets for the treatment of alcoholism [40].
HYPOTHALAMIC RELEASING HORMONES AND THEIR ANALOGS
The new stage of the medicinal application of peptide hormones began at the end of 1960s and at the beginning of 1970s. It has been associated with the isolation and determination of the chemical structure of hypothalamic regulators of biosynthesis and secretion of the adenohypophysis hormones. These compounds implement a connection between CNS and the endocrine system and occupy a key position in the hypothalamus-hypophysis-peripheral endocrine glands system. The structure of the thyrotropin-releasing hormone, TRH (the first discovered hypothalamic hormone) was determined in 1969 by two groups of scientists [41, 42]. TRH proved to be the pGlu-His-Pro-NH2 tripeptide. It stimulates biosynthesis and secretion of thyrotropin and prolactin adenotropic hormones, plays a key role in support of the homeostasis of the thyroid gland, and exhibits a pronounced neurotropic effect along with the hormonal action. This effect manifests itself as the activation of a number of CNS functions [43–47]. TRH exhibits anticonvulsant, anticataleptic, and antihypothermic effects and acts as an antagonist of many CNS inhibitors. TRH removes effects of reserpine, chlorpromazine, and haloperidol and exhibits analeptical properties, blocking the action of ethanol and barbiturates and several effects of morphine and opioid peptides. Biological studies of TRH and its analogs differentiate more than ten possible areas of their application as activators of the CNS functions (Fig. 2) [44].
Clinical application of TRH and its analogs [43]. * Can be particularly effective as a an adjuvant therapy.
Drugs based on the native TRH structure have been created and are present in the pharmaceutical market, but a wide spectrum of activities of this compound, its fast biodegradation, and low bioavailability limit its use. TRH is generally applied to diagnostics of the thyroid function. TRH administration is used for an evaluation of the hypophysis’ ability to secrete the thyrotrophic hormone (TSH). The TSH level before and after the TRH stimulation is determined in this test. The direct determination of TRH by the enzyme immunoassay is more rarely used. To date, several hundred TRH analogs with different action profiles have been synthesized [43, 48–51]. Active research into novel synthetic analogs of TRH is still ongoing [52, 53], but few of them have successfully passed all the three phases of clinical trials. Only taltirelin, developed in Japan, is used as a drug [50]. Taltirelin is the TRH analog with a substitution of 2,4-dioxo-3-methylpyrimidinic acid for Glp. It is used for treatment of various neurodegenerative disorders [54]. Taltirelin’s ability to increase the dopamine level during the Parkinson’s disease seems especially promising [55].
The structure of one more releasing-hormone, luliberin (releasing-hormone of gonadotrophic hormones, GnRH) was determined in 1971. Luliberin proved to be the ten-member peptide: pGlu-His-Trp-Ser-Tyr-Gly-Leu-Arg-Pro-Gly-NH2 [56, 57]. This hormone is a regulator of the reproductive sphere. It stimulates secretion and biosynthesis of luteinizing and follicular-stimulating hormones. Rapid development of the peptide synthesis was observed in the 1970s. Along with the multistage time-consuming conventional peptide synthesis, the solid phase peptide synthesis was put to use. This method allowed automation and acceleration of the peptide preparation and removed restrictions on the length of a peptide chain. Several thousand luliberin analogs (agonists and antagonists) had been prepared using conventional and solid phase methods of peptide synthesis by the mid-1980s [58, 59]. The super active agonists that were several hundred times more active than the natural hormone were designed. The Gly residue in position 6 was replaced by a residue of a D‑amino acid in these analogs. Several of these peptides additionally involved ethyl amide instead of glycyl amide. The ovulation-stimulating therapeutic agents that provided a preparation of ova for extracorporeal fertilization were prepared based on these agonists. Tryptorelin (pGlu-His-Trp-Ser-Tyr-D-Trp-Leu-Arg-Pro-Gly-NH2) with the D-tryptophan residue in position 6, leuprolide (H-Pyr-His-Trp-Ser-Tyr-D-Leu-Leu-Arg-Pro-NHEt), buserilin (D-Ser(tBu)6EA10-LHRH), and other peptides belonged to such agents. Leuprolide and other super agonists of GnRH are also used for treatment of the hormone-dependent tumors, such as prostate and breast cancers, hysteromyomas, and endometriosis. The treatment of cancers and hormonal disorders is based on the paradoxical inhibitory effect of the super agonists [60, 61]. They cause an initial intensive stimulation of the hypophysis, but, later, exhibit an inhibitory effect if the agonist concentration in blood is constant. The inhibition occurs due to resistance of the GnRH super agonists to degradation by the hypophyseal enzymes. The super agonists block the gonadotrophic receptors in the hypophysis and make them insensitive after the initial stimulation, i.e., receptor desensitization occurs, resulting in the dramatic decrease in the gonadotropin level in blood. Correspondingly, the level of the sex hormones is also decreased, and hormonal blockage occurs. The inhibitory effects of the agonists are completely reversible.
The structure of the GnRH antagonists differs from that of the natural molecule in a larger degree than the agonist structures. The antagonists often contain residues of unnatural amino acids. The N-terminal region of all the antagonists is changed in comparison with the natural GnRH. The GnRH antagonists preserve the ability to be bound to the GnRH receptors, compete for the receptor binding sites with the natural hormone, but do not cause the generation of a cellular signal and a release of the luteinizing and follicle-stimulating hormones. Thus, the action of the natural GnRH is blocked. The antagonists stabilize the receptors in their inactive conformation, and the stimulation phase is absent distinct from the super agonists. The effect is prolonged due to the high resistance of the antagonists to the action of peptidases. Effective antitumor drugs and regulators of the hormonal disorders were also created based on the superactive antagonists. Degarelix, cetrorelix, abarelix, ganirelix, and ozarelix are the best known drugs [62, 63]. These peptides involve the Ac-D-Nal-D-Cpa-D-Pal sequence (where Nal is 3-(2-naphthyl)alanine, Pal is 3-(2-pyridyl)alanine, and Cpa is β-cyclopropylalanine) in the amino terminal area, different derivatives of D-amino acids in position 6, and D-Ala in the C‑terminal region. The primary structures of the best known antagonists of GnRH are listed in Table 3. Both super agonists and super antagonists were introduced into clinical practice in the mid-1980s and are currently widely used.
Somatostatin, also known as a growth hormone-inhibiting hormone (GHIH), was isolated in 1970s. Somatostatin is a 14-member cyclic peptide (Ala-Gly-Cys-Lys-Asn-Phe-Phe-Trp-Lys-Thr-Phe-Thr-Ser-Cys(S–S3–14)) [64]. This compound is a multifunctional regulator and is produced not only in the hypothalamus, but in the stomach, bowels, and pancreas as well. Somatostatin inhibits the secretion of the somatotropic and thyrotrophic pituitary hormones, peptides that are produced in the stomach, bowels, liver, and pancreas, and serotonin. Somatostatin inhibits the secretion of insulin, glucagon, gastrin, cholecystokinin, vasoactive intestinal polypeptide, the insulin-like growth factor-1, and other compounds. Somatostatin is used for therapy of hormonal disorders that are associated with hyperproduction of the somatotropin growth hormone and various diseases of the gastrointestinal tract and pancreas [65]. The modustatin and stilamin drugs that have the natural structure of somatostatin were developed and introduced into medicinal practice at the end of 1980s.
The structure-functional studies of somatostatin resulted in the creation of its highly active agonistic analogs, octreotide and lanreotide [65–68]. Octreotide is a cyclic octapeptide of the following primary structure: D-Phe-Cys-Phe-D-Trp-Lys-Thr-Cys-Thr-Ol(S–S2–7). It pharmacologically imitates the natural somatostatin, but much more effectively inhibits the growth hormone, glucagon, and insulin in comparison with the natural hormone. An important advantage of octreotide is its high resistance to enzymatic degradation due to such structural modifications as the introduction of the D-amino acid residues and changes in the N-terminus and С-terminus of the natural molecule. Octreotide is widely used for treatment of hormone-depended tumors. Lanreotide (Naphtyl-D-Ala-Cys-Tyr-D-Trp-Lys-Val-Cys-Thr-NH2(S–S2–7)) is also stable to degradation but differs from somatostatin and lanreotide in its spectrum of action. Lanreotide exhibits the more pronounced affinity to the peripheral somatostatin receptors (hypophysial and pancreatic) than that to the central receptors [68]. This property is responsible for the lanreotide selectivity towards a secretion of somatotropin and the exocrine secretion by pancreas and the intestinal glands.
Several drugs which are applied to the treatment of many diseases are created on the basis of octreotide and lanreotide. Four Russian companies produce octreotide: Ellara, Farm-Sintez, Farmkompaniya, and FarmFirma Soteks. Major world manufacturers of octreotide are Novartis Pharma (Switzerland), Fresenius KABI Deutschland (Germany), and Sun Pharmaceutical Industries (India) [69]. The production volume of lanreotide is smaller. This drug is produced by the Ipsen Pharma Biotech (France) under the names of Somatuline and Somatuline Autogel [70].
ANALOGS OF THE GLUCAGON-LIKE PEPTIDE-1
It has become evident in the last quarter of the 20th century that peptide hormones are multifunctional bioregulators, and there are a majority of receptors for these hormones in an organism. The peptide hormones have been found to be produced not only in the system of hypothalamus-hypophysis-endocrine glands, but in other organs and tissues as well. Incretins that are secreted by the gastrointestinal tract occupy an important place among these “nonclassic” hormones [71]. These compounds regulate the carbohydrate metabolism and a number of the gastrointestinal functions and serve as an initial material for the creation of novel therapeutic agents. The glucagon-like peptide-1 (GLP-1) has attracted the special attention of scientists among the other incretins. GLP-1 is the 36-member peptide whose receptors are widely distributed in many organs and tissues. The activity spectrum of this universal bioregulator is very wide. Its action extends to important organs and tissues along with its stimulation effect on biosynthesis and excretion of insulin (Table 4) [72]. The shortened GLP-1(7–37) and GLP-1(7–36)-NH2 peptides also exhibit biological activity.
The main obstacle for the application of the GLP-1 peptide as the drug substance is its short half-life (2 min). To date, this disadvantage has been eliminated, and several drugs based on stable GLP-1 analogs have been developed [73–76]. This strategy for a design of these therapeutic agents is a good example of the use of modern approaches to the creation of peptide drugs with the desired properties and involves several steps. The purpose of the modifications was to make the hormone molecule stable, increase its half-life, while maintaining its high level of activity. The analogs should have a high structural correspondence to the cellular GLP-1 receptor, resistance to the dipeptidylpeptidase-4 (DPP4), and the ability to reversibly bind to albumin. These desired properties would prevent rapid degradation of the analogs. Liraglutide and semaglutide were created using this approach [73].
A long-chain fatty acid was chosen and attached to the hormone molecule, taking into account the high albumin affinity to hydrophobic compounds. Positions which modification with a fatty acid residue has little influence on conformational peculiarities of GLP-1 and its high affinity to the receptor were determined. As a result, the Lys26 residue was chosen. The derivatives with the С12–С18 fatty acid chains and with or without a carboxyl on the free terminus were prepared. In general, 36 compounds were synthesized in order to choose the most suitable position of the modification and structures of the linker and the fatty acid. An examination of their binding to the GLP 1(7–37) receptor revealed liraglutide as the most active and long-lived compound. Its structure is given in Fig. 3.
Chemical structure of liraglutide and semaglutide [70].
The structure of GLP-1(7–37) was further changed by an introduction of the aminoisobutyric acid residue in position 2, which significantly increased the resistance of the peptide to DPP4 without a significant decrease in the activity. The Lys26 position was modified by bis-aminodiethoxyacetyl linker and the residue of the C18 fatty diacyl acid [74]. All these modifications resulted in the highly active and stable semaglutide analog of GLP-1. It is administered once a week, used for treatment of the type II diabetes, and improves functioning of the cardiovascular system. The ability of semaglutide to decrease the body weight of obese individuals without any side effects is of the greatest interest. The therapeutic analogs of GLP-1 are evidently commercially very successful owing to a widespread prevalence of diabetes and obesity, and the pace of development and adoption of these drugs is very rapid. The peptide hormone drugs that have the highest sales volumes are given in Table 5.
CONCLUSIONS
Within the span of 100 years after the isolation of insulin and its introduction into medical practice, the peptide hormones, their analogs, and their mimetics have become an important element of the pharmaceutical industry. Dozens of medicinal drugs have been created, and the insulin therapeutics stably occupy the first place. The leading companies of the United States and Europe produced the insulin drugs in the total amount of 25 billion dollars in 2019. Approximately one and a half dozen other peptide therapeutic agents also have high cost parameters (Table 5) [1]. The GLP-1 and GLP-2 analogs (dulaglutide, liraglutide, semaglutide, exenatide, and teduglutide) have leading positions. Two analogs of GnRH (leuprolide and goserelin) are also represented on the pharmaceutical market. Teriparatide (the drug based on the recombinant human parathyroid hormone) has high volumes of sales. The classical drugs of ACTH and vasopressin also hold their positions in the market.
The creation of drugs on the basis of the peptide hormones is a dynamically developing industry with clearly defined aims and a number of trends. The creation of highly active and selective analogs of the “classic” hormones is still a topical problem. The therapeutics based on hormones whose structures have comparatively recently been determined are being actively introduced into medicine. For example, the tesamorelin analog of the somatotropic hormone was approved for medicinal use in 2010. Determination of the structure of the peptide hormone receptors gives an opportunity to search for their ligands on the basis of a structural correspondence using modern computer technologies and databases, resulting in novel agonists and antagonists of both peptide and nonpeptide natures. Problems of an increase in the stability and bioavailability of the peptide drugs are being successfully solved. Old ways of delivery of hormones to an organism are improved and new delivery methods are being developed. Investigations in the area of technologies of a preparation of the peptide hormones and their analogs are of undiminished interest. New breakthrough synthetic methods are being developed. Undoubtedly, our knowledge of the peptide hormones will be expanded in the future, and, hence, novel and more ideal drugs will be designed and will find an application to not only hormonal therapy, but to other areas of medicine, such as oncology, neurology, treatment of the cardiovascular diseases, and metabolic imbalances.
REFERNCES
Muttenthaler, M., King, G.F., Adams, D.J., and Alewood, P.F., Nat. Rev. Drug Discov., 2021, vol. 20, pp. 309–325. https://doi.org/10.1038/s41573-020-00135-8
Lau, J.L. and Dunn, M.K., Bioorg. Med. Chem., 2018, vol. 26, pp. 2700–2707. https://doi.org/10.1016/j.bmc.2017.06.052
Fosgerau, K. and Hoffmann, T., Drug Discov. Today, 2014, vol. 20, pp. 122–128. https://doi.org/10.1016/j.drudis.2014.10.003
Filimonov, D.A., Druzhilovskiy, D.S., Lagunin, A.A., Gloriozova, T.A., Rudik, A.V., Dmitriev, A.V., and Poroikov, V.V., Biomed. Chem.: Res. Methods, 2018, vol. 1, pp. 1–21. https://doi.org/10.18097/bmcrm00004
Banting, F.G., Best, C.H., Collip, J.B., Campbell, W.R., and Fletcher, A.A., Can. Med. Assoc. J., 1922, vol. 12, pp. 141–146.
Sanger, F. and Tuppy, H., Biochem. J., 1951, vol. 49, pp. 463–481. https://doi.org/10.1042/bj0490463
Sanger, F. and Thompson, E.O., Biochem. J., 1953, vol. 53, pp. 353–366. https://doi.org/10.1042/bj0530366
Candido, R., Wyne, K., and Romoli, E., Diabetes Ther., 2018, vol. 9, pp. 927–949. https://doi.org/10.1007/s13300-018-0422-4
Infoholic Research LLP, Global Human Insulin Market 2018–2024, Research and Markets, ID 4470733, 2018. www.researchandmarkets.com/reports/4470733/ global-human-insulin-market-2018-2024.
Hirsch, I.B., N. Engl. J. Med., 2005, vol. 352, pp. 174–183. https://doi.org/10.1056/NEJMra040832
Vecchio, I., Tornali, C., Bragazzi, N.L., and Martini, M., Front. Endocrinol., 2018, vol. 9, p. 613. https://doi.org/10.3389/fendo.2018.00613
Li, C.H., Simpson, M.E., and Evans, H.M., Science, 1942, vol. 96, p. 450. https://doi.org/10.1126/science.96.2498.450
Elkinton, J.R., Hunt, A.D., Godfrey, L., McCrory, W.W., Rogerson, A.G., and Stokes, J., J. Am. Med. Assoc., 1949, vol. 141, pp. 1273–1279. https://doi.org/10.1001/jama.1949.02910180001001
Gallo-Payet, N., Martinez, A., and Lacroix, D., Front. Endocrinol., 2017, vol. 8, p. 101. https://doi.org/10.3389/fendo.2017.00101
Ashmarin, I.P., Nezavibat’ko, V.N., Myasoedov, N.F., Kamenskii, A.A., Grivennikov, I.A., Ponomareva-Stepnaya, M.A., and Ryasina, T.V., Zh. Vyssh. Nerv. Deyat., 1997, vol. 47, pp. 419–425.
Levitskaya, N.G., Glazova, N.Yu., Sebentsova, E.A., Manchenko, D.M., Vilenskii, D.A., Andreeva, L.A., Kamenskii, A.A., and Myasoedov, N.F., Neirokhimiya, 2008, vol. 25, pp. 111–118.
Manchenko, D.M., Glazova, N.Yu., Levitskaya, N.G., Andreeva, L.A., Kamenskii, A.A., and Myasoedov, N.F., Ross. Fiziol. Zh., 2010, vol. 96, pp. 1014–1023.
Copp, D.H. and Cheney, B., Nature, 1962, vol. 193, pp. 381–382. https://doi.org/10.1038/193381a0
Inzerillo, A.M., Zaidi, M., and Huang, C.L.H., J. Pediatr. Endocrinol. Metab., 2004, vol. 17, pp. 931–940. https://doi.org/10.1515/JPEM.2004.17.7.931
Vigneaud, V., Ressler, C., and Trippett, S., J. Biol. Chem., 1953, vol. 205, pp. 949–957. https://doi.org/10.1016/S0021-9258(18)49238-1
Vigneaud, V., Lawler, H.C., and Popenoe, E.A., J. Am. Chem. Soc., 1953, vol. 75, pp. 4880–4881. https://doi.org/10.1021/ja01115a554
Vigneaud, V., Ressler, C., Swan, J.M., Roberts, C.W., and Katsoyannis, P.G., J. Am. Chem. Soc., 1954, vol. 76, pp. 3115–3121. https://doi.org/10.1021/ja01641a004
Vigneaud, V., Gish, D.T., and Katsoyannis, P.G., J. Am. Chem. Soc., 1954, vol. 76, pp. 4751–4752. https://doi.org/10.1021/ja01647a089
Carter, C.S., Front. Endocrinol., 2017, vol. 22, p. 356. /https://doi.org/10.3389/fendo.2017.00356
Tkacheva, M.A., Inyushkina, E.M., Karyan, S.D., and Inyushkin, A.N., Ul’yan. Med.-Biol. Zh., 2018, no. 1, pp. 145–158.
Gimpl, G. and Fahrenholz, F., Physiol. Rev., 2001, vol. 81, pp. 629–683. https://doi.org/10.1152/physrev.2001.81.2.629
Hoyle, C.H., Brain Res., 1999, vol. 848, pp. 1–25. https://doi.org/10.1016/S0006-8993(99)01975-7
Neumann, I.D. and Landgraf, R., Trends Neurosci., 2012, vol. 35, pp. 649–659. https://doi.org/10.1016/j.tins.2012.08.004
Manning, M., Stoev, S., Chini, B., Durroux, T., Mouillac, B., and Guillon, G., Prog. Brain Res., 2008, vol. 170, pp. 473–512. https://doi.org/10.1016/S0079-6123(08)00437-8
Hurbin, A., Orcel, H., Ferraz, C., Moos, F.C., and Rabie, A., J. Neuroendocrinol., vol. 12, pp. 677–684. https://doi.org/10.1046/j.1365-2826.2000.00499.x
Herrera, V.L.M., Bagamasbad, P., Decano, J.L., and Ruiz-Opazo, N., Physiol. Genomics, 2011, vol. 43, pp. 32–42. https://doi.org/10.1152/physiolgenomics.00154.2010
Burnatowska-Hledin, M., Lazdins, I.B., Listenberger, L., Zhao, P., Sharangpani, A., and Folta, V., Am. J. Physiol. Renal. Physiol., 1999, vol. 276, pp. 199–209. https://doi.org/10.1152/ajprenal.1999.276.2.F199
Manning, M., Stoev, S., and Bankowski, K., J. Peptide Sci., 2010, vol. 16, pp. 366–367.
Manning, M., Misicka, A., Olma, A., Bankowski, K., Stoev, S., Chini, B., Durroux, T., Mouillac, B., Corbani, M., and Guillon, G., J. Neuroendocrinol., 2012, vol. 24, pp. 609–628. https://doi.org/10.1111/j.1365-2826.2012.02303.x
Biryukova, E.V., Ozhirenie Metab., 2017, vol. 14, no. 4, pp. 23–30. https://doi.org/10.14341/OMET2017423-30
Hammock, E.A., Neuropsychopharmacology, 2015, vol. 40, pp. 24–42. https://doi.org/10.1038/npp.2014.120
Belyakova, F.S., Sinjushin, A.A., Voskresenskaya, O.G., Kamensky, A.A., and Golubovich, V.P., Neurochem. J., 2015, vol. 9, pp. 201–205. https://doi.org/10.1134/S1819712415030034
Altura, B.M., Gebrewold, A., Carella, A., and Altura, B.T., Int. J. Surg. Res., 2017, vol. 4, pp. 1–3. https://doi.org/10.19070/2379-156X-170002e
Pan, Y.F., Jia, X.T., Wang, X.H., Chen, X.R., Li, Q.S., Gao, X.P., and Qi, J.S., Regul. Pept., 2013, vol. 183, pp. 7–12. https://doi.org/10.1016/j.regpep.2013.03.003
Harper, K.M., Knapp, D.J., Criswell, H.E., and Breese, G.R., Psychopharmacology (Berl.), 2018, vol. 235, pp. 3363–3379. https://doi.org/10.1007/s00213-018-5099-x
Burgus, R., Dunn, T.F., Desidero, D., and Guillemin, R., C.R. Hebd. Seances Acad. Sci., Ser. D, Sci. Nat., 1969, vol. 269, pp. 1870–1873.
Boler, J., Enzmann, F., Folkers, K., Bowser, C.Y., and Schally, A.V., Biochem. Biophys. Res. Commun., 1969, vol. 37, pp. 705–710. https://doi.org/10.1016/0006-291X(69)90868-7
Monga, V., Meena, C.L., Kaur, N., and Jain, R., Curr. Med. Chem., 2008, vol. 15, pp. 2718–2733.
Jantas, D., Adv. Cell Biol., 2010, vol. 2, pp. 139–154.
Pierpaoli, W., Curr. Aging Sci., 2013, vol. 6, pp. 92–98.
Yarbrough, G.G., Trends Pharmacol. Sci., 2003, vol. 24, pp. 617–618. https://doi.org/10.1016/j.tips.2003.10.001
Prokai, L., Prog. Drug Res., 2002, vol. 59, pp. 134–169. https://doi.org/10.1021/jm1012984
Faden, A.I., Saksen, I., and Noble, L.J., Brain Res., 1988, vol. 448, pp. 287–293. https://doi.org/10.1016/0006-8993(88)91265-6
Kaur, N., Monga, V., Lu, X., Gershengorn, M.C., and Jain, R., Bioorg. Med. Chem., 2007, vol. 15, pp. 433–443. https://doi.org/10.1016/j.bmc.2006.09.045
Yamamura, M., Kinoshita, K., Nakagawa, H., Tanaka, T., Maeda, K., and Ishida, R., Jpn. J. Pharmacol., 1990, vol. 53, pp. 451–461. https://doi.org/10.1254/jjp.53.451
Khomane, K.S., Meena, C.L., Jain, R., and Bansal, A.K., Expert Opin. Ther. Pat., 2011, vol. 21, pp. 1673–1691. https://doi.org/10.1517/13543776.2011.623127
Meena, C.L., Thakur, A., Nandekar, P.P., Sangamwar, A.T., Sharma, S.S., and Jain, R., Bioorg. Med. Chem., 2015, vol. 23, pp. 5641–5653. https://doi.org/10.1016/j.bmc.2015.07.022
Kobayashi, K., Abe, Y., Kawai, A., Furihata, T., Endo, T., and Takeda, H., Clin. Pharmacol., 2020, vol. 60, pp. 1314–1323. https://doi.org/10.1002/jcph.1628
Kinoshita, K., Yamamura, M., Sugihara, J., Suzuki, M., and Matsuoka, Y., CNS Drug Rev., 1998, vol. 4, pp. 25–41. https://doi.org/10.1111/j.1527-3458.1998.tb00039.x
Zheng, C., Chen, G., Tan, Y., Zeng, W., Peng, Q., Wang, J., Cheng, C., Yang, X., Nie, S., Xu, Y., Zhang, Z., Papa, S.M., Ye, K., and Cao, X., Front. Cell. Neurosci., 2018, vol. 12, pp. 1–16. https://doi.org/10.3389/fncel.2018.00417
Matsuo, H., Baba, Y., Nair, R.M.G., Arimura, A., and Schally, A.V., Biochem. Biophys. Res. Commun., 1971, vol. 43, pp. 1334–1341. https://doi.org/10.1016/S0006-291X(71)80019-0
Burgus, R., Butcher, M., Amoss, M., Ling, N., Monahan, M.W., Rivier, J., Fellows, R., Blackwell, R., Vale, W., and Guillemin, R., Proc. Natl. Acad. Sci. U. S. A., 1972, vol. 69, pp. 278–284. https://doi.org/10.1073/pnas.69.1.278
Karter, M.J. and Rivier, J.E., Endocrine Rev., 1986, vol. 7, pp. 44–66. https://doi.org/10.1210/edrv-7-1-44
Schally, A.V., Gynecol. Endocrinol., 1999, vol. 13, pp. 401–409. https://doi.org/10.3109/09513599909167587
Walker, L.M., Tran, S., and Robinson, J.W., Clin. Genitourin. Cancer, 2013, vol. 11, pp. 375–384. https://doi.org/10.1016/j.clgc.2013.05.004
Schultze-Mosgau, A., Griesinger, G., Altgassen, C., von Otte, S., Hornug, D., and Diedrich, K., Expert Opin. Investig. Drugs, 2005, vol. 14, pp. 1085–1097. https://doi.org/10.1517/13543784.14.9.1085
Van Poppel, H. and Klotz, L., Int. J. Urol., 2012, vol. 19, pp. 594–601. https://doi.org/10.1111/j.1442-2042.2012.02997.x
Kumar, P. and Sharma, A., J. Hum. Reprod. Sci., 2014, vol. 7, pp. 170–174. https://doi.org/10.4103/0974-1208.142476
Brazeau, P., Vale, W., Burgus, R., Ling, N., Butcher, M., Rivier, J., and Guillemin, R., Science, 1973, vol. 179, pp. 77–79. https://doi.org/10.1126/science.179.4068.77
Rai, U., Thrimawithana, T.R., Valery, C., and Young, S.A., Pharmacol. Ther., 2015, vol. 152, pp. 98–110. https://doi.org/10.1016/j.pharmthera.2015.05.007
Grozinsky-Glasberg, S., Shimon, I., Korbonits, M., and Grossman, A.B., Endocr. Relat. Cancer, 2008, vol. 15, pp. 701–720. https://doi.org/10.1677/ERC-07-0288
Gomes-Porras, M., Jersy Cárdenas-Salas J., and Álvarez-Escolá, C., Int. J. Mol. Sci., 2020, vol. 21, pp. 1682–1689. https://doi.org/10.3390/ijms21051682
Günther, T., Tulipano, G., Dournaud, P., Bousquet, C., Csaba, Z., Kreienkamp, H.J., Lupp, A., Korbonits, M., Castaño, J.P., Wester, H.J., Culler, M., Melmed, S., and Schulz, S., Pharmacol. Rev., 2018, vol. 70, pp. 763–835. https://doi.org/10.1124/pr.117.015388
Debnath, D. and Cheriyath, P., StatPearls, 2021. www.ncbi.nlm.nih.gov/books/NBK544333/.
Lanreotide. https://go.drugbank.com/drugs/DB06791.
Nauck, M.A. and Meier, J.J., Diabetes Obes. Metab., 2018, vol. 20, pp. 5–21. https://doi.org/10.1111/dom.13129
Ametov, A.S., Russ. Med. Zh., 2006, vol. 14, no. 26, pp. 11–16. https://doi.org/10.14341/2072-0351-5860
Knudsen, L.B. and Lau, J., Front. Endocrinol., 2019, vol. 10, p. 155. https://doi.org/10.3389/fendo.2019.00155
Lau, J., Bloch, P., Schaäffer, L., Pettersson, I., Spetzler, J., Kofoed, J., Madsen, K., Knudsen, L.B., McGuire, J., Steensgaard, B.D., Strauss, H.M., Gram, D., Knudsen, S.M., Nielsen, F.S., Thygesen, P., Reedtz-Runge, S., and Kruse, T., J. Med. Chem., 2015, vol. 58, pp. 7370–7380. https://doi.org/10.1021/acs.jmedchem.5b00726
St, OngeE.L. and Miller, S.A., Expert. Opin. Biol. Ther., 2010, vol. 10, pp. 801–806. https://doi.org/10.1517/14712598.2010.481281
Rosenstock, J., Balas, B., Charbonnel, B., Bolli, G.B., Boldrin, M., Ratner, R., and Balena, R., Diabetes Care, 2013, vol. 36, pp. 498–504. https://doi.org/10.2337/dc12-0709
Funding
This study was supported by the State Research Program of Belarus, “Chemical Processes, Reagents, and Technologies, Bioregulators and Bioorganic Chemistry” 2021–2025.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
This article does not contain any studies involving human participants and animals performed by any of the authors.
Conflict of Interst
The authors declare that they have no conflicts of interest.
Additional information
Translated by L. Onoprienko
Abbreviations: GIT, gastrointestinal tract; ACTH, adrenocorticotropic hormone; DPP4, dipeptidyl dipeptidase-4; GnRH, releasing hormone of gonadotropic hormones; GLP-1, Glucagon-like peptide-1; TRH, thyrotropin-releasing hormone; TSH, thyrotropic hormone.
Corresponding author: phone: +375(44)777-40-36.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martinovich, V.P., Baradzina, K.U. Peptide Hormones in Medicine: A 100-Year History. Russ J Bioorg Chem 48, 221–232 (2022). https://doi.org/10.1134/S1068162022020157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1068162022020157