Abstract
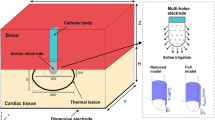
A mathematical model for epicardial radiofrequency ablation using an electrode irrigated by saline is proposed. Saline flow profiles are derived using thin film theory, and heat convection due to blood flow is also included in the model. Results from a computer implementation of the model using a finite element method suggest that transmural ablation lesions can be made in 4-mm-thick tissue. Effects of parameters such as tissue and saline layer thickness, irrigation rate, blood flow rate, and applied power are investigated. Saline is found to irrigate as well as ablate. Rise in saline temperature and consequent ablation by saline is more pronounced as saline layer becomes thicker. Electrode tip temperatures as much as 40 °C lower than maximum tissue temperature were found in simulations. © 2002 Biomedical Engineering Society.
PAC2002: 8754Br, 8719Pp, 0270Dh, 8710+e
Similar content being viewed by others
REFERENCES
Acheson, D. J. Elementary Fluid Dynamics. Oxford: Clarendon, 1990.
Bennet, C. O., and J. E. Myers. Momentum, Heat and Mass Transfer, 2nd ed. New York: McGraw Hill, 1974.
Cox, J. L., J. P. Boineau, R. B. Schuessler, K. M. Kater, and D. G. Lappas. Five-year experience with the maze procedure for atrial fibrillation. Ann. Thorac. Surg. 56:814-824, 1993.
Duck, F. A. Physical Properties of Tissue: A Comprehensive Reference Book. San Diego: Academic, 1990.
Gabriel, C. Compilation of the Dielectric Properties of Body Tissues at RF and Microwave Frequencies. Tech. Rep. AL/OE-TR-1996-0037, Armstrong Laboratory, Brooks Airforce Base, TX 78235-5102, 1996.
Haines, D. E., and D. D. Watson. Tissue heating during radiofrequency catheter ablation: a thermodynamic model and observations in isolated perfused and superfused canine right ventricular free wall. Pacing. Clin. Electrophysiol. 12:962-976, 1989.
Hestenes, M. R., and E. Stiefel. Methods of conjugate gradi-ents for solving linear systems. J. Res. Natl. Bur. Stand. 49:409-436, 1952.
Huppert, H. E. The propagation of two-dimensional and axisymmetric viscous gravity currents over a rigid horizontal surface. J. Fluid Mech. 121:43-58, 1982.
Jain, M. K., R. Richman, J. Crowe, P. D. Wolf, and B. Pless. Effect of fat layer on epicardial radiofrequency lesions. Pacing. Clin. Electrophysiol. 2000.
Jain, M. K., and P. D. Wolf. Temperature-controlled and constant-power radio-frequency ablation: what affects lesion growth. IEEE Trans. Biomed. Eng. 46:405-412, 1999.
Jain, M. K., and P. D. Wolf. A three-dimensional finite element model of radiofrequency ablation with blood flow and its experimental validation. Ann. Biomed. Eng. 28:1075-1084, 2000.
Johnson, C. Numerical Solution of Partial Differential Equations by the Finite Element Method. Cambridge: Cambridge University Press, 1995.
Kharge, K., T. Deneke, H. Haardt, B. Lemke, P. Grewe, K.-M. Müller, and A. Laczkovics. Saline-irrigated, cooled-tip radiofrequency ablation is an effective technique to perform the Maze procedure. Ann. Thorac. Surg. 72:S0190-1095, 2001.
Labonte, S. A. A computer simulation of radio-frequency ablation of the endocardium. IEEE Trans. Biomed. Eng. 41:883-890, 1994.
Labonte, S. Numerical model for radio-frequency ablation of the endocardium and its experimental validation. IEEE Trans. Biomed. Eng. 41:108-115, 1994.
Lin, A. C., and D. Wilbur. Complications associated with radiofrequency catheter ablation. In: Radiofrequency Catheter Ablation of Cardiac Arrhythmias: Basic Concepts and Clinical Applications. New York: Future, 2000, pp. 737-746.
McRury, I. D., D. Panescu, M. A. Mitchell, and D. E. Haines. Nonuniform heating during radiofrequency catheter ablation with long electrodes: monitoring the edge effect. Circulation 11:4057-4064, 1996.
Min, X., and R. Mehra. Analysis of the variables that affect electrode and tissue temperature during RF ablation in a finite element analysis model. In: Computers in Cardiology New York: IEEE, 1999, pp. 205-208.
Nakagawa, H., W. S. Yamanashi, J. V. Pitha, M. Arruda, X. Wang, K. Ohtomo, K. J. Beckman, J. H. McClelland, R. Lazzara, and W. M. Jackman. Arrhythmias/radiofrequency ablation: Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with a salineirrigated electrode versus temperature control in a canine thigh muscle preparation. Circulation 91:2264-73, 1995.
Panescu, D., J. G. Whayne, S. D. Fleischman, M. S. Mirotznik, D. K. Swanson, and J. G. Webster. Three-Dimensional Finite Element Analysis of Current Density and Temperature Distributions During Radio-Frequency Ablation. IEEE Trans. Biomed. Eng. 42:879-890, 1995.
Petersen, H. H., J. H. Svendsen, S. Haunsø, and D. L. Packer. Irrigated tip radiofrequency ablation: Is there a virtual electrode effect? Pacing Chin. Electrophysiol. 821.
Saad, Y., and M. H. Schultz. GMRES: A generalized minimal residual algorithm for solving nonsymmetric linear systems. SIAM (Soc. Ind. Appl. Math.) J. Sci. Stat. Comput. 7:856-869, 1986.
Schöberl, J. An advancing front 2D/3D-mesh generator based on abstract rules. Comput. Visual Sci. 1:41-52, 1997.
Schwan, H. P., and K. R. Foster. RF-Field Interactions with Biological Systems: Electrical Properties and Biophysical Mechanisms. Proc. IEEE 68:104-113, 1980.
Skrumeda, L. L., and R. Mehra. Comparison of standard and irrigated radiofrequency ablations in the canine ventricle. J. Cardiovasc. Electrophysiol. 9:1196-205, 1998.
Sosa, E., M. Scanavacca, A. D'Avila, J. Piccioni, O. Sanchez, J. L. Velarde, M. Silva, and B. Reolão. Endocardial and epicardial ablation guided by nonsurgical transthoracic epicardial mapping to treat recurrent ventricular tachycardia. J. Cardiovasc. Electrophysiol. 9:229-239, 1998.
Surowiec, A., S. S. Stuchly, L. Eidus, and A. Swarup. In vitro dielectric properties of human tissues at radiofrequencies. Phys. Med. Biol. 32:615-621, 1987.
Tungjitkusolmun, S., V. R. Vorperian, N. Bhavaraju, H. Cao, J.-Z. Tsai, and J. G. Webster. Guidelines for predicting lesion size at common endocardial locations during radio-frequency ablation. IEEE Trans. Biomed. Eng. 48:194-201, 2001.
Wong, W. S., B. A. Wanderbrink, R. E. Riley, M. Pomeranz, M. S. Link, M. K. Homoud, N. A. Mark Estes, III, and P. J. Wang. Effect of saline irrigation flow rate on temperature profile during cooled radiofrequency ablation. J. Interv. Card. Electrophysiol. 4:321-326, 2000.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gopalakrishnan, J. A Mathematical Model for Irrigated Epicardial Radiofrequency Ablation. Annals of Biomedical Engineering 30, 884–893 (2002). https://doi.org/10.1114/1.1507845
Issue Date:
DOI: https://doi.org/10.1114/1.1507845