Abstract
BACKGROUND: Inappropriate use of antimicrobials to treat acute upper respiratory tract infections (URIs), which usually have a viral etiology, contributes to emergence and spread of antimicrobial resistance in Streptococcus pneumoniae and other human bacterial pathogens.
OBJECTIVE: To reduce antimicrobial use for management of acute URIs in adult and pediatric patients.
DESIGN: Prospective, nonrandomized, controlled trial.
SETTING: Four primary care clinics within a staff model HMO in Detroit, Mich.
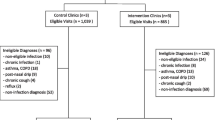
PARTICIPANTS: Twenty-one primary care physicians at clinics where the educational intervention was implemented, and 9 primary care physicians at control clinics where no educational programs were implemented.
MEASUREMENTS: Antibiotic prescribing for acute URIs during the baseline and study years among the intervention and control groups.
RESULTS: A generalized linear mixed-effects model was used and showed that antimicrobial prescribing among the intervention group physicians decreased 24.6% from the baseline to the postintervention period (P<.0001) for both pediatric and adult medicine physicians. From the baseline to the study period, there was no significant decline in rates of antimicrobial prescribing by the control group of physicians (pediatricians, P=.35; internists, P=.42). The rates of decline in antimicrobial prescribing differed significantly between the intervention and control groups (P<.0003 for pediatricians and P<.01 for Internists).
CONCLUSIONS: An interactive, case-based educational program for physicians and their staff proved effective for reducing unwarranted prescribing of antibiotics in the treatment of URIs by primary care physicians in a Medicaid HMO setting.
Similar content being viewed by others
References
Whitney CG, Farley MM, Hadler J, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343:1917–24.
Baquero F, Negri MC, Mirosini MI, Blasquez J. Antibiotic selective environments. Clin Infect Dis. 1998;27(suppl 1):S5–11.
Centers for Disease Control and Prevention. Streptococcus pneumoniae disease. Available at: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/streppneumo.htm. Accessed August 20, 2001.
Michigan Department of Community Health. Antimicrobial resistance trends. Penicillin resistant study-site isolates of Streptococcus pneumoniae and vancomycin resistant sterile-site isolates of Enterococcus spp. Michigan Sentinel Hospital Laboratory Survey, Fourth Quarter, 1995 through First Quarter, August 2000.
McCaig LF, Hughes JM. Trends in antimicrobial prescribing among office-based physicians in the United States. JAMA. 1995;273:214–9.
Gonzales R, Steiner JF, Lum A, Barrett PH, Jr. Decreasing antibiotic use in ambulatory practice. JAMA. 1999;281:1512–9.
McCaig LM, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002;287:3096–102.
Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 1999. Emerging infectious diseases: A strategy for the 21st century. Available at: http://www.cdc.gov/ncidod/emergplan. Accessed August 10, 2000.
McCaig LM, Besser RE, Hughes JM. Antimicrobial drug prescriptions in ambulatory care settings, United States, 1992–2000. Emerg Inf Dis. 2003;9:432–6.
Centers for Disease Control and Prevention. Vancomycin resistant Staphylococcus aureus—Michigan, June 2002. MMWR 2002. Available at: http://www.cdc.gov/od/oc/media/mmwrnews/n020705.htm#mmwr4. Accessed July 5, 2002.
Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA. 1996;275:175.
Stewart J, Pilla J, Dunn L. Pilot study for appropriate anti-infective community therapy: effect of a guideline-based strategy to optimize use of antibiotics. Can Fam Phys. 2000;46:851–9.
Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA. 2002;287:3103–9.
Juzych NS, Thompson S. Antibiotics: What You Should Know. A patient brochure produced for the Michigan Antibiotic Resistance Reduction Coalition, 2001.
Centers for Disease Control and Prevention. Viral Disease Prescription Pad. Available at: http://www.cdc.gov/drugresistance/community/files/Viral_Prescription_Pad.pdf. Accessed February 8, 2002.
Centers for Disease Control and Prevention. Letter for Daycare Providers. Available at: http://www.cdc.gov/drugresistance/community/files/MD_letter_4c.pdf. Accessed February 8, 2002.
The Anti-Infective Review Panel. Anti-Infective Guidelines for Community-Acquired Infections. 2nd ed. PAACT: Toronto, ON, Canada; 1997.
McCullagh P, Nelder JA. Generalized Linear Models. New York, NY: Chapman & Hall; 1992.
Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Institute Inc.; 1996.
Orr PH, Scherer K, MacDonald A, Moffatt MEK. Randomized placebo-controlled trials of antibiotics for acute bronchitis: a critical review of the literature. J Fam Pract. 1993;36:507–12.
Gonzales R, Sande M. What will it take to stop physicians from prescribing antibiotics in acute bronchitis? Lancet. 1995;1345:665–6.
MacKay DN. Treatment of acute bronchitis in adults without underlying lung disease. J Gen Intern Med. 1996;11:557–62.
American Academy of Pediatrics. Principles of judicious use of antimicrobial agents: a compendium for the health care professional. Pediatrics. 1998;101(suppl):163–184.
American College of Physicians. Guidelines for appropriate antibiotic use for treatment of acute respiratory tract infections in adults. Ann Intern Med. 2001;134:479–529.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no conflicts of interest to declare for this article or this research.
Financial support for the printing of educational brochures and posters was provided by General Motors Foundation, and cold kifs were provided by Glaxo SmithKline and Pfizer Corporation.
Rights and permissions
About this article
Cite this article
Juzych, N.S., Banerjee, M., Essenmacher, L. et al. Improvements in antimicrobial prescribing for treatment of upper respiratory tract infections through provider education. J GEN INTERN MED 20, 901–905 (2005). https://doi.org/10.1111/j.1525-1497.2005.0198.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2005.0198.x