-
PDF
- Split View
-
Views
-
Cite
Cite
Carlo Basile, Christian Combe, Francesco Pizzarelli, Adrian Covic, Andrew Davenport, Mehmet Kanbay, Dimitrios Kirmizis, Daniel Schneditz, Frank van der Sande, Sandip Mitra, on behalf of the EUDIAL Working Group of ERA-EDTA, Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres, Nephrology Dialysis Transplantation, Volume 35, Issue 5, May 2020, Pages 737–741, https://doi.org/10.1093/ndt/gfaa069
Close - Share Icon Share
Abstract
COVID-19, a disease caused by a novel coronavirus, is a major global human threat that has turned into a pandemic. This novel coronavirus has specifically high morbidity in the elderly and in comorbid populations. Uraemic patients on dialysis combine an intrinsic fragility and a very frequent burden of comorbidities with a specific setting in which many patients are repeatedly treated in the same area (haemodialysis centres). Moreover, if infected, the intensity of dialysis requiring specialized resources and staff is further complicated by requirements for isolation, control and prevention, putting healthcare systems under exceptional additional strain. Therefore, all measures to slow if not to eradicate the pandemic and to control unmanageably high incidence rates must be taken very seriously. The aim of the present review of the European Dialysis (EUDIAL) Working Group of ERA-EDTA is to provide recommendations for the prevention, mitigation and containment in haemodialysis centres of the emerging COVID-19 pandemic. The management of patients on dialysis affected by COVID-19 must be carried out according to strict protocols to minimize the risk for other patients and personnel taking care of these patients. Measures of prevention, protection, screening, isolation and distribution have been shown to be efficient in similar settings. They are essential in the management of the pandemic and should be taken in the early stages of the disease.
INTRODUCTION
An epidemic of Severe Acute Respiratory Syndrome-Corona Virus-2 (SARS-CoV-2) (COVID-19), a new strand of the coronavirus family, originated from Wuhan (China) in December 2019, and was declared a pandemic by the World Health Organization as of 11 March 2020 (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). The global pandemic of SARS-CoV-2 (COVID-19) is quickly affecting the delivery of health care worldwide [1–4]. This novel coronavirus has specifically high morbidity in the elderly and in comorbid populations [1–4]. Chronic kidney disease constitutes a relevant co-morbidity, and dialysis centres pose a risk as potential vector in the spreading of this pandemic [1–4]. In previous epidemics or catastrophic situations, the case fatality rate has always been much higher in dialysis patients than in the general population.
In the first two decades of this century, three members of the coronavirus family, Severe Acute Respiratory Syndrome-Corona Virus (SARS-CoV), Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) and SARS-CoV-2, have caused three major pandemic outbreaks of infectious respiratory diseases. At the present time, it is believed that SARS-CoV-2 is more contagious, but with a lower case fatality rate than the other two viruses. Compared with the previous two outbreaks, the epidemic area of COVID-19 caused by SARS-CoV-2 is larger, the number of infected people and, consequently, the number of deaths higher, and the strain on the healthcare system, as well as the global economic loss, greater [1–4].
Uraemic patients on dialysis combine an intrinsic fragility and a very frequent burden of comorbidities with a specific setting in which many patients are repeatedly treated in the same area (haemodialysis centres). Dialysis patients constitute a susceptible population because of their older age and their less efficient immune system, and they are therefore more prone to develop severe infectious diseases than the general population [5, 6]. Dialysis patients are exposed and re-exposed to a higher contamination risk than the general population because their routine treatment usually requires three dialysis sessions per week. Moreover, if infected, the intensity of dialysis requiring specialized resources and staff is further complicated by requirements for isolation, control and prevention, putting healthcare systems under exceptional additional strain. Therefore, all measures to slow if not to eradicate the pandemic and to control unmanageably high incidence rates must be taken very seriously.
To the best of our knowledge, at the time of writing of this article (14 March 2020), only one series of cases from one haemodialysis centre in Wuhan has been published [7]. The authors reviewed the whole course of the outbreak emerging in the haemodialysis centre of Renmin Hospital, Wuhan University, from 14 January 2020, the day the first case was confirmed, to 17 February 2020, the day of the epidemic extinction. The authors reported that 37 cases in 230 haemodialysis patients (16.1%) and 4 cases out of 33 staff members (12.1%) were diagnosed with COVID-19. Dialysis patients with COVID-19 had less lymphopenia, lower serum levels of inflammatory cytokines and milder clinical disease than other patients affected by COVID-19 infection. During that epidemic, seven dialysis patients died, including six with COVID-19 and one without COVID-19. The presumed causes of death were not directly related to pneumonia, but due to cardiovascular and cerebrovascular diseases, and hyperkalaemia. The outcome of the four staff members was favourable [7].
Isolation practices can be effective for preventing secondary transmission of viruses closely related to COVID-19. For instance, during the 2015 MERS-CoV outbreak in Korea, although 116 participants in three haemodialysis units were incidentally exposed to the virus, strict patient surveillance and proper isolation practice prevented secondary transmissions [8].
COVID-19 infection in patients treated in dialysis centres presents a particular challenge as the risk of transmission to the medical staff, facility workers, other patients and to family members is significantly increased.
The Chinese Society of Nephrology [9], the Taiwan Society of Nephrology [10] and the Centers for Disease Control and Prevention (https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/dialysis.html) have recently developed guidelines for dialysis units during the COVID-19 outbreak. The aim of the present review of the EUDIAL Working Group of ERA-EDTA is to provide recommendations for the prevention, mitigation and containment in haemodialysis centres of the emerging SARS-CoV-2 (COVID-19) pandemic. In doing so, we have held in high consideration the suggestions of our Asian colleagues, given their significant experience in dealing with COVID-19 [9, 10], the interim additional guidance released by the Centers for Disease Control and Prevention on 10 March 2020 [11] and the World Health Organization recommendation for the rational use of personal protective equipment for COVID-19 [12]. The EUDIAL Working Group will update its recommendations any time new data and evidences become available. The ERA-EDTA has also launched a dedicated webpage that is regularly updated at https://www.era-edta.org/en/covid-19-news-and-information/.
RECOMMENDATIONS
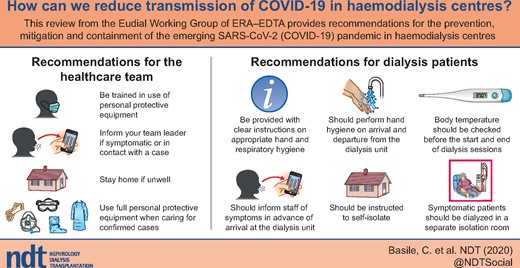
Healthcare team
A working team consisting of dialysis physicians, nursing staff and technicians should receive training in updated clinical knowledge of the COVID-19 epidemic, epidemic prevention tools and guidelines from the government, scientific societies and hospital authorities. Instructions should include how to use the different types of facemasks, how to use tissues to cover the nose and mouth when coughing or sneezing, how to dispose of tissues and contaminated items in waste receptacles, and how and when to perform hand hygiene. Training can be done peer to peer or online.
Latest care recommendations and epidemic information should be updated and delivered to all medical care personnel as needed.
Staff members should self-monitor their symptoms (if any) and should inform the team leader in case they or their family members develop symptom(s) suggestive of COVID-19 infection. Sick members of the team should stay at home, and in any case should not be in contact with patients or other team members.
Nurses should be trained to take nasopharynx swabs for COVID-19 polymerase chain reaction, with appropriate dressing using a filtering face piece 2 (FFP2) mask (filtering 95% of particulate matter and aerosols in inhaled air), goggles, mobcap, disposable surgical blouse and gloves.
Dialysis patients and dialysis facilities
Dialysis patients should be instructed to stay at home while off dialysis and on their non-dialysis days, to use individual transport to and from dialysis facilities, to avoid public transportation, to abstain from travelling around the country, to avoid personal contact, and to abstain from public, private or religious events (family reunions, marriages, funerals, etc.). Parents and grandparents on dialysis may want to abstain from personal contact especially with their children and grandchildren, because the younger population serves as a vector of the disease often without showing symptoms.
Dialysis facilities should provide patients with instructions (in appropriate languages) about hand hygiene, respiratory hygiene and cough etiquette. Instructions should include how to use facemasks, how to use tissues to cover the nose and mouth when coughing or sneezing, how to dispose of, preferably disposable paper, tissues and contaminated items in waste receptacles, and how and when to perform hand hygiene. Dispensers of hydroalcoholic solutions should be installed in waiting rooms. Patients must be educated and encouraged to perform hand hygiene at least on arrival and at the time of departure from the unit and if in contact with respiratory secretions. Dialysis facilities should have space in waiting areas for ill patients to sit separated from other patients by at least 2 m. Medically stable patients might opt to wait in a personal vehicle or outside the healthcare facility. Two metres separation between dialysis stations is advisable.
Treatment and waiting areas should have good air conditioning and ventilation to remove particles and aerosol droplets from the air.
Body temperature should be systematically measured before the start and at the end of the dialysis session in all patients.
Early recognition and isolation of individuals with respiratory infection are mandatory: (i) dialysis facilities should identify patients with signs and symptoms of fever, cough, upper airway involvement or conjunctivitis before they enter the waiting room and treatment area; (ii) patients must inform staff of fever or respiratory symptoms before arrival at the facility by phone or appropriate electronic means; thus, the facility can be prepared for their arrival (preferably they should be seen in a first aid department and not in a dialysis department) or triage them to a more appropriate setting such as an acute care hospital; (iii) patients with respiratory symptoms should be brought to an appropriate treatment area as soon as possible to minimize the time in waiting areas; (iv) all patients who have fever, cough, upper airway involvement or conjunctivitis should be screened for novel COVID-19 infection. For sampling, patients should be either in a single-patient room or in a room dedicated to sampling. Disinfection of the room after sampling is mandatory.
Ideally, symptomatic patients should be dialysed in a separate isolation room (if available), in which a negative pressure atmosphere can be established, with the door closed. Otherwise, they should wait in a separate isolation room and receive dialysis in the last shift of the day until infection is excluded. He/she should wear a proper (surgical or N95) mask filtering 95% of the particulate matter <2.5 µm in the aerosol of exhaled air.
Patients with confirmed COVID-19 infection should be admitted to an airborne infection isolation room and should not receive dialysis in an outpatient dialysis facility, unless an airborne infection isolation room is available. All personnel involved in the direct care of patients affected by COVID-19 must undertake full protection, including long-sleeved waterproof isolation clothing, hair caps, goggles, gloves and medical masks (FFP2 or FFP3 mask if available) filtering 95–99% of particulate matter and aerosols in inhaled air. Hand hygiene must be strictly implemented, carefully washing hands with soap and water and systematically using alcoholic solutions and disposable gloves.
Consideration should be given to cohorting more than one patient with suspected or confirmed COVID-19 and the healthcare team caring for them in the same section of the unit and/or on the same shift (e.g. consider the last shift of the day). Avoid, however, mixing of suspected and confirmed cases.
Manpower should be cohorted in separate teams for the management of high-risk and low-risk patients. Only the assigned healthcare team should enter the isolation room/cohort area, all non-scheduled team-mates should be excluded at all times.
If a newly confirmed or highly suspected case of novel coronavirus infection in dialysis centres is identified, disinfection must be carried out immediately. Areas in close contact with these patients must not be used for other patients until cleared.
The medical waste from confirmed or suspected patients with novel coronavirus infection must be considered as infectious medical waste and disposed of accordingly.
Duration of isolation precautions for patients under investigation for or with confirmed COVID-19
Discontinuation of isolation precautions should be determined on a case-by-case basis, in conjunction with local, state and federal health authorities, until the information is available regarding viral shedding after clinical improvement.
Factors to be considered include presence of symptoms related to COVID-19 infection, date when symptoms resolved, other conditions that require specific precautions (e.g., tuberculosis, Clostridium difficile), other laboratory information reflecting clinical status and alternatives to inpatient isolation, such as the possibility of safe recovery at home.
Surgical operations
Patients who need vascular access surgery should be screened for COVID-19. Operations on patients with confirmed or suspected COVID-19 infection must be carried out in a designated room with necessary protection for medical staff.
Operational strategies for family members and caregivers
All family members living with dialysis patients must follow all precautions and regulations given to patients to prevent person-to-person and within-family transmission of the COVID-19, which include body temperature measurement, good personal hygiene, handwashing and prompt reporting of potentially infected individuals.
Dialysis patients who have a family member or caregiver subject to quarantine (precautionary isolation—basically for 14 days—because of a potential exposition to the coronavirus but not showing any signs of infection) [13], can have dialysis as usual during the 14-day period of quarantine of the family members or caregivers.
Once family members or caregivers of dialysis patients have been converted to a confirmed case, the patient’s identity must be upgraded and treated in accordance with the above-mentioned conditions.
Home haemodialysis and peritoneal dialysis
These patients should be assisted at home as far as is possible, using telereporting assistance or other electronic systems for clinical management and to supplement home visits by healthcare staff, as deemed necessary.
CONCLUSIONS
COVID-19, a disease caused by a novel coronavirus, is a major global human threat that has turned into a pandemic. The only study so far reporting an outbreak of COVID-19 in a dialysis centre indicates that dialysis patients are a highly susceptible population and haemodialysis centres are a high-risk area in the outbreak of a COVID-19 epidemic [7]. The management of patients on dialysis affected by COVID-19 must be carried out according to strict protocols to minimize the risk for other patients and personnel taking care of these patients. Measures of prevention, protection, screening, isolation and distribution have been shown to be efficient in similar settings [8]. Prevention plays a key role; the other measures are essential in the mitigation and containment of the COVID-19 pandemic in haemodialysis centres.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Chinese Society of Nephrology.
Centers for Disease Control and Prevention. Interim Additional Guidance for Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed COVID-19 in Outpatient Hemodialysis Facilities,
World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19): Interim Guidance,




Comments
Sir— We read the article by Basile C et al with a great interest (1). The authors described essential recommendations for prevention, mitigation and containment of the emerging SARS-CoV-2 pandemic in haemodialysis centres (1). They advised wearing a mask for symptomatic patients, whether surgical or N95 while receiving dialysis session (1). We have concerns about this advice of propagating N95 usage.
N95 is not classified as mask, but a respirator. It has two types: Surgical N95 and standard N95. Standard N95s usually have an exhalation valve, and it is not recommended for symptomatic patients, because there is a possibility that exhaled particles may leave the respirator via the valve and enter the surrounding environment (2). Many symptomatic patients wear a valved respirator, and unfortunately they even don’t recognize their riskfull act. Both US Centers for Disease Control and Prevention (CDC) and WHO agree that symptomatic SARS-CoV-2 infected patients should wear surgical facemasks. This advice is valid for dialysis patients, too (3). According to CDC recommendations, the patients with symptoms of respiratory infections should be put on a facemask at check-in until they leave the dialysis facility (3).
Ma Y et al from Wuhan reported that the dialysis patients with COVID-19 should be isolated, and all medical staff (not the symptomatic patient) be asked to upgrade their personal protective equipment (PPE), and wear N95 respirator (4). Cozzolino M shared Milano experience on coronavirus management in dialysis centers patients, and reported that patients must wear a surgical mask when they arrive until they leave the dialysis facility during COVID-19 epidemic (5). During crisis situations, CDC recommends N95 respirators be used only during aerosol-generating procedures by healthcare workers (HCW).
The lack of adequate PPE during COVID-19 pandemic, including N95 respirators, for frontline HCWs is worrisome. Logical sourcing of PPE is an issue widely discussed in the literature (6). Project N95 ie, is a national COVID-19 medical equipment clearinghouse for PPE for medical workers, especially the N95 respirators (7). They identify high-need regions, and distribute any kind of equipments where it is needed most. Many inventory ideas (ie coffee filter masks, air conditioner filter masks) have been offered to create supply for critical shortages (6). Within this context, please do not propagate N95 usage by especially symptomatic patients within hospital wards, including dialysis facilities.
1- Basile C, Combe C, Pizzarelli F, et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres [published online ahead of print, 2020 Mar 20]. Nephrol Dial Transplant. 2020;gfaa069. doi:10.1093/ndt/gfaa069
2- https://multimedia.3m.com/mws/media/1792732O/respiratory-protection-faq-healthcare.pdf
3- Centers for Disease Control and Prevention. Interim Additional Guidance for Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed COVID-19 in Outpatient Hemodialysis Facilities, 2020. https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/dialysis.html (March 19, 2020, date last accessed)
4- Ma Y, Diao B, Lv Xet al. 2019 Novel Coronavirus Disease in Hemodialysis (HD) Patients: Report from One HD Center in Wuhan, China. https://www.medrxiv.org/content/10.1101/2020.02.24.20027201v2 (April 4, 2020, date last accessed)
5- https://www.era-edta.org/en/wp content/uploads/2020/03/200310_Milano_Experience_Covid19_dialysis.pdf (April 3, 2020 date last accessed)
6- Livingston E, Desai A, Berkwits M. Sourcing Personal Protective Equipment During the COVID-19 Pandemic [published online ahead of print, 2020 Mar 28]. JAMA. 2020;10.1001/jama.2020.5317.doi:10.1001/jama.2020.5317
7- Project N95. The national COVID-19 medical equipment clearinghouse. Accessed March 31, 2020. https://www.projectn95.org/ (April 3, 2020, date last accessed)