-
PDF
- Split View
-
Views
-
Cite
Cite
A. Zegard, F. Umar, R.J. Taylor, E. Acquaye, C. Gubran, S. Chalil, K. Patel, J. Panting, H. Marshall, T. Qiu, F. Leyva, 43
Long-term clinical outcomes of cardiac resynchronization therapy with or without defibrillation: impact of the etiology of cardiomyopathy, EP Europace, Volume 19, Issue suppl_1, October 2017, Page i20, https://doi.org/10.1093/europace/eux283Close - Share Icon Share
Background: There is a continuing debate as to whether cardiac resynchronization therapy-defibrillation (CRT-D) is superior to CRT-pacing (CRT-P), particularly in patients with non-ischemic cardiomyopathy (NICM).
Objective: We sought to quantify clinical outcomes after primary prevention CRT-D and CRT-P and whether clinical outcomes differ according to the etiology of cardiomyopathy.
Methods: Clinical events were quantified in patients undergoing CRT-D (n = 551) or CRT-P (n = 999). Analyses were undertaken in the total study population and in propensity-matched samples. Device choice was governed by clinical guidelines in the United Kingdom.
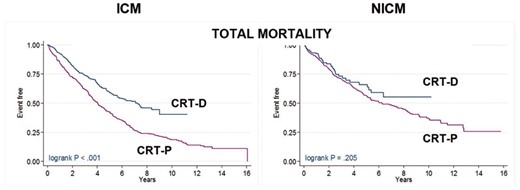
Results: In univariable analyses of the total study population, (maximum follow-up: 16 years; median of 4.7 years (interquartile range [IQR]: 2.4-7.1), CRT-D was associated with a lower total mortality (HR:0.71) and the composite endpoints of total mortality or HF hospitalization (HR:0.72) and total mortality or hospitalization for major adverse cardiac events (MACE; HR:0.71) (all p < 0.001). After propensity-matching (n = 796), CRT-D was associated with a lower total mortality (HR:0.72) and the composite endpoints (all p < 0.01). When further stratified according to etiology, CRT-D was associated with a lower total mortality (HR:0.62), total mortality or HF hospitalization (HR: 0.63) and total mortality or hospitalization for MACE (HR:0.59) (all p < 0.001) in patients with ischaemic cardiomyopathy (ICM). No difference in outcomes between CRT-D and CRT-P emerged in patients with NICM.
Conclusions: In this study of real-world clinical practice, CRT-D was superior to CRT-P with respect to total mortality and composite endpoints, independent of known confounders. The benefit of CRT-D was evident in ICM, but not in NICM.