-
PDF
- Split View
-
Views
-
Cite
Cite
Dan Song, Jie Zhou, Tianli Fan, Jing Chang, Yuzhen Qiu, Zexiang Zhuang, Juanjuan Ma, Li Zeng, Decision aids for shared decision-making and appropriate anticoagulation therapy in patients with atrial fibrillation: a systematic review and meta-analysis, European Journal of Cardiovascular Nursing, Volume 21, Issue 2, February 2022, Pages 97–106, https://doi.org/10.1093/eurjcn/zvab085
Close - Share Icon Share
Abstract
Underuse of oral anticoagulants (OACs) is commonly observed among patients with atrial fibrillation (AF), which hinders stroke prevention in AF. Shared decision-making (SDM) can help enhance adherence by minimizing patients’ misunderstanding of treatment and aligning care with their preferences. Decision aids (DAs) have been developed to facilitate the SDM process. This study aimed to: (i) evaluate the effects of DAs on AF patients’ knowledge, decisional conflict, OAC uptake, and adherence and on the incidence of stroke and bleeding; and (ii) explore characterizing factors associated with enhanced DA effectiveness.
Five databases were searched. Meta-analysis was conducted using RevMan 5.3 when data were available. Comparative analysis between effective and ineffective DAs was conducted to determine the DA designs associated with better effects. Ten studies were included. Pooling results indicated that DAs reduce decisional conflict related to warfarin use [mean difference = −0.10; 95% confidence interval (CI): −0.18 to −0.02; P = 0.01] and enhance OAC uptake [risk ratio: 1.03; 95% CI: 1.01–1.05; P = 0.004]. The effects of DAs on adherence and incidence of stroke and bleeding were unclear. Comparative analysis revealed that DAs with key elements of SDM (situation diagnosis, choice awareness, option clarification, benefits and disadvantages, and patient’s preference) and pre-consultation delivery are more likely to be effective in promoting SDM and OAC uptake.
DAs are promising in promoting SDM and OAC uptake in patients with AF. The evidence on adherence and incidence of stroke and bleeding remains uncertain. More trials with rigorous study design and longer follow-up are necessary to obtain evidence.
Patient decision aids (DAs) could be applied in clinical practice, as this study provides evidence that they are beneficial to reduce decisional conflict, improve patients’ knowledge level and anticoagulant uptake among patients with atrial fibrillation (AF).
Effective DAs should incorporate multiple key elements of shared decision-making (SDM) in line with the International Patient Decision Aid Standards (IPDAS) collaboration, and such tools should be delivered prior to the consultation rather than within the consultation, thereby better preparing the patients for SDM.
To facilitate the use of such effective tools in clinical practice, parallel efforts should be provided to training the healthcare professionals to obtain knowledge and skills of SDM.
Interprofessional SDM model is encouraged, and nurses should play a more active role in SDM to better support patients with AF in making tough decisions.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia; it affects 33.5 million people worldwide,1 with 5 million new cases identified annually.2 AF is a major risk factor of ischaemic stroke. When untreated, stroke risk may increase five-fold, and one in every five stroke incidences is caused by AF.3 Stroke in patients with AF has greater severity, higher mortality rates, and higher treatment costs than stroke due to other causes.4 Evidence suggests that the risk of stroke can be reduced by 60–70% with the use of oral anticoagulants (OACs).5 Professional guidelines on AF provide clear OAC recommendations.6,7 Despite the evidence, adherence to these guidelines remains poor. A review of 54 studies found that 50% of AF patients with high risk of stroke did not receive appropriate OAC therapy.8 Four out of five patients presenting stroke had inadequate therapeutic anticoagulation preceding the event,9 thereby further highlighting the importance of adequate OAC therapy.
The reasons for the underuse of OAC are many. First, the risk of bleeding is a predominant concern with OAC treatment, although bleeding events are estimated to be five to eight times less likely than stroke,10 and a clear net benefit is obtained. Second, traditional anticoagulants, such as warfarin, negatively interact with some medicines and food and require regular blood tests, thereby leading to adherence challenges. Non-vitamin K OACs (NOACs), which do not require as much blood monitoring and have few drug and food interactions, are now available. However, NOACs are not applicable to valvular AF.11 Therefore, anticoagulation treatment to reduce stroke risk is a complex and preference-sensitive decision that depends on a clear understanding of the value patients place on the trade-offs between the benefits and risks of the treatment options. For such decisions, shared decision-making (SDM) is an ideal approach that is characterized by cooperative communication between health professionals and patients, who work together to make clinical decisions by considering the best available evidence and the patients’ problems, preferences and contexts.12 Patients who are more active in making decisions about their health have better health outcomes and healthcare experiences.13,14
SDM is challenging because of time constraints, and specific skills are required. An SDM interaction between a patient and a healthcare provider has six key elements,15 namely, situation diagnosis, choice awareness, option clarification, discussion of harms and benefits, deliberation of patient preferences, and decision-making. Evidence-based decision aids (DAs) have been developed to facilitate the process. According to the International Patient Decision Aid Standards (IPDAS) collaboration, all six SDM key elements, except making the decision, should be handled by a tool regarded as a DA.16 DAs differ from general education materials and are used to obtain an explicit decision, thereby providing a detailed and personalized focus in the options and outcomes to prepare the people for decision-making. On the contrary, education materials help people understand their diagnosis and management in general terms and do not necessarily help them participate in SDM.17 DAs have received an increasing amount of attention, because they involve patients with AF into the decision-making regarding OAC treatment. Integrating such findings can provide important insights into the effects of DAs on the OAC treatment for this important clinical cohort.
Two narrative reviews on the benefits of DAs in patients with AF have been published in 2017.18,19 Both reviews concluded the positive effects of DAs on patient knowledge and decisional conflict, given that majority of the studies showed favourable findings on these outcomes. Nevertheless, these reviews have two major limitations. Firstly, both reviews included observational studies, which may compromise the synthesized evidence quality. Updating the review and strengthening the evidence quality by including randomized controlled trials (RCTs) exclusively are necessary, because several new RCTs are published recently. Secondly, the lack of evaluation of the association between the characteristics of DAs and study outcomes in both reviews limits their potential in making precise implications in practice. Therefore, this study addresses these gaps in the literature.
The objectives of the present systematic review are as follows: (i) to identify the effects of DAs on AF patients’ knowledge, decisional conflict, OAC uptake and adherence, as well as the incidence of stroke and bleeding; and (ii) to examine the association, if any, between elements of SDM present and the effects of these DAs.
Methods
Search strategy
We followed the PRISMA guideline.20 We comprehensively searched four English databases, namely, CINAHL, EMBASE, Medline, and PsycINFO. The China National Knowledge Infrastructure (CNKI) was also included in the search. All the databases were searched from inception to 31 January 2021. Search terms included ‘atrial fibrillation’, ‘shared decision making’, ‘decision making’, ‘decision aid’, ‘decision support’, and ‘decision tool’. D.S. and J.Z. independently performed the literature search. The full search strategies for Medline are presented in Supplementary materialonline,FileS1.
Inclusion criteria
Only RCTs published as full-length articles were included. The included studies met the following inclusion criteria listed in a population, intervention, comparison, and outcome format. The participants were adults with AF who were aged 18 years old or above. Studies that considered DAs as the intervention were included. DAs, in this review, were defined according to the IPDAS Collaboration’s description, as follows: ‘tools designed to help people participate in decision-making about health care options’.16 All types of control were considered as eligible. For outcome measures, we collected decisional conflict, knowledge, OAC uptake and adherence, and incidence of stroke and bleeding.
Methodological quality appraisal
D.S. and J.Z. independently assessed the risk of bias of each study using the Cochrane collaboration risk of bias tool for RCTs,21 and disagreements were resolved by consensus. If one or more of the five other domains was at a high risk of bias, then the summary assessment of the risk of bias was ‘high’. If one or more domains was ‘unclear’, and all others were ‘low risk’, then we summarized the risk of bias as ‘unclear’. If all domains were ‘low risk’, then the summary assessment of the risk of bias was ‘low’.
Data collection
For each eligible study, data about study and DA characteristics, outcome measures and the main results were extracted using a self-designed standardized form. For the three studies that did not report raw data, the authors of such studies were contacted to retrieve the raw data; however, no one replied. We used the definitions in Table 1 to determine the key SDM components present in each DA. D.S. and J.Z. independently performed the data collection.
Definitions for the key elements of SDM in DAs
| Key element of SDM . | Definitions for this study15 . |
|---|---|
| Situation diagnosis | The DA explicitly describes the patient’s problem. |
| Choice awareness | The DA explicitly acknowledges that the patient’s situation is mutable, that there is more than one option to address this situation, and that patient input matters in deciding how to proceed. |
| Option clarification | The DA explicitly describes the available options. |
| Harms and benefits discussion | The DA explicitly explains the harms and benefits of the available options. |
| Patient preferences deliberation | The DA explicitly elicits the patient’s preferences. |
| Making the decision | The DA explicitly elicits the patient’s wish to make or defer a decision, asks for or describes the patient’s choice. |
| Key element of SDM . | Definitions for this study15 . |
|---|---|
| Situation diagnosis | The DA explicitly describes the patient’s problem. |
| Choice awareness | The DA explicitly acknowledges that the patient’s situation is mutable, that there is more than one option to address this situation, and that patient input matters in deciding how to proceed. |
| Option clarification | The DA explicitly describes the available options. |
| Harms and benefits discussion | The DA explicitly explains the harms and benefits of the available options. |
| Patient preferences deliberation | The DA explicitly elicits the patient’s preferences. |
| Making the decision | The DA explicitly elicits the patient’s wish to make or defer a decision, asks for or describes the patient’s choice. |
DA, decision aids; SDM, shared decision-making.
Definitions for the key elements of SDM in DAs
| Key element of SDM . | Definitions for this study15 . |
|---|---|
| Situation diagnosis | The DA explicitly describes the patient’s problem. |
| Choice awareness | The DA explicitly acknowledges that the patient’s situation is mutable, that there is more than one option to address this situation, and that patient input matters in deciding how to proceed. |
| Option clarification | The DA explicitly describes the available options. |
| Harms and benefits discussion | The DA explicitly explains the harms and benefits of the available options. |
| Patient preferences deliberation | The DA explicitly elicits the patient’s preferences. |
| Making the decision | The DA explicitly elicits the patient’s wish to make or defer a decision, asks for or describes the patient’s choice. |
| Key element of SDM . | Definitions for this study15 . |
|---|---|
| Situation diagnosis | The DA explicitly describes the patient’s problem. |
| Choice awareness | The DA explicitly acknowledges that the patient’s situation is mutable, that there is more than one option to address this situation, and that patient input matters in deciding how to proceed. |
| Option clarification | The DA explicitly describes the available options. |
| Harms and benefits discussion | The DA explicitly explains the harms and benefits of the available options. |
| Patient preferences deliberation | The DA explicitly elicits the patient’s preferences. |
| Making the decision | The DA explicitly elicits the patient’s wish to make or defer a decision, asks for or describes the patient’s choice. |
DA, decision aids; SDM, shared decision-making.
Data synthesis
Meta-analysis was performed using Review Manager 5.3. For each outcome of interest, the intervention effect of continuous data was expressed as the mean difference (MD) with 95% confidence interval (CI) of post-intervention results between groups. Risk ratios (RRs) were used for dichotomous outcomes using the Mantel–Haenszel method. Statistical heterogeneity between studies was quantified by using the I2 statistic. A randomized effect model was used for I2 > 50%. Subgroup analysis was impossible for a limited number of studies. Thus, comparative analysis was used to determine the potential DA design that might lead to more significant effects on outcomes.
Results
Search process
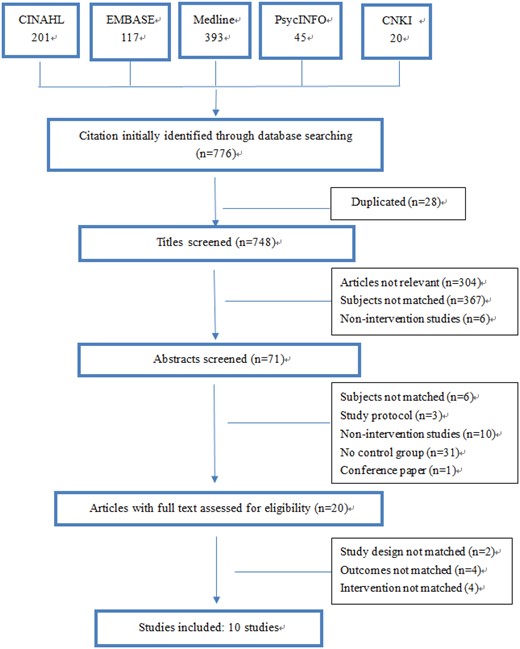
The results of the search process are presented in Figure 1. A total of 776 citations were identified. Among these, 28 citations were removed because of duplication. After screening the titles and abstracts, 728 studies were excluded, and 20 papers with full texts were checked for eligibility. Finally, 10 eligible studies were included in this review.
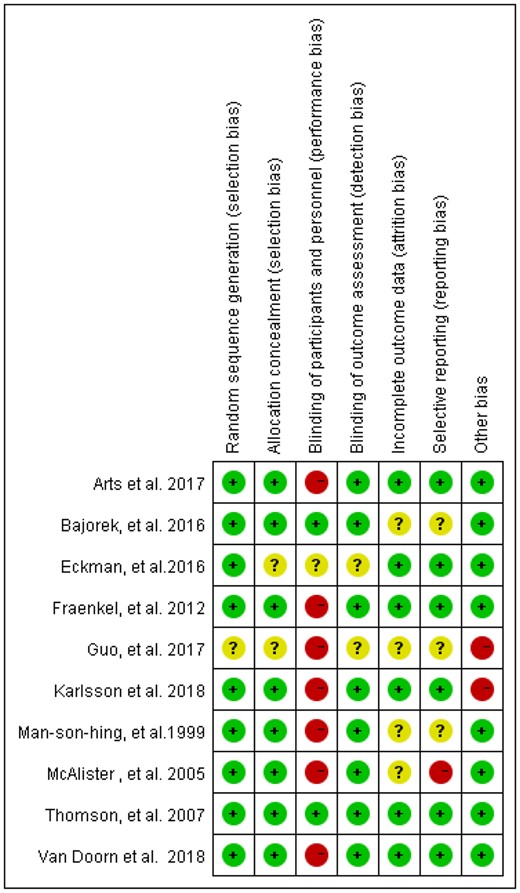
Risk of bias
Risk of bias is presented in Figure 2. In nine studies, the allocation sequence was adequately generated. In eight studies, allocation was adequately called. The participants and interveners were not blinded in the eight studies. In nine studies, data collectors were blinded. Incomplete outcome data were judged as low risk of bias in six studies. Selective reporting was judged as low risk of bias in seven studies. Two studies on the potential of other bias were judged as high risk, because clustering was unaccounted for in the analysis.
Study and intervention characteristics
Table 2 summarizes the characteristics of the studies. Table 3 summarizes the characteristics of the DAs. The DAs varied in terms of the format, delivery and content. Most studies (7/10) used the computer-based format. One study used a mobile-based format, whereas two studies used booklet and video formats. For delivery, five DAs were delivered within the clinical consultation; four DAs were delivered prior to the clinical consultation; and one DA was delivered after the clinical consultation. The situation diagnosis (n = 9) and option clarification (n = 10) were the elements that were most commonly included in the DAs. A clarification of the benefits and disadvantages of alternative options was present in six DAs. Choice awareness and patient preference were present in five DAs. All elements were supported in only two DAs.
Characteristics of the included studies
| Authors, year/country . | Participants . | Intervention . | Control . | Risk of bias . | ||||
|---|---|---|---|---|---|---|---|---|
| Type of intervention . | Age (mean) . | Female (%) . | Type of control . | Age (mean) . | Female (%) . | |||
| Van Doorn et al., 2018/The Netherlands | Adults with AF in general practice Exp: n = 1129 Con: n = 1226 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 77 | 49.4% | Usual care | 77 | 46.2% | Low |
| Arts et al., 2017/The Netherlands | Adults with AF in general practice Exp: n = 496 Con: n = 235 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 74.61 | / | Usual care | 72.61 | / | Low |
| Karlsson et al., 2018/Sweden | Adults with AF in general practice Exp: n = 8292 Con: n = 6508 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | / | 43% | Usual care | / | 43% | High |
| Fraenkel et al., 2012/USA | Adults with AF in general practice Exp: n = 69 Con: n = 66 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | / | 1% | Usual care | / | 2% | Low |
| Eckman et al., 2016/UK | Adults with AF in general practice Exp: n = 801 Con: n = 692 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 70.2 | 44% | Disseminations of didactic materials | 69.8 | 48% | Unclear |
| Thomson et al., 2007/UK | Adults with AF in general practice Exp: n = 69 Con: n = 67 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | 73.7 | 44.6% | Evidence-based paper guidelines | 73.1 | 43.4% | Low |
| McAlister et al., 2005/Canada | Adults with AF in general practice Exp: n = 228 Con: n = 218 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 73 | 43% | Usual care | 71 | 34% | High |
| Man-Son-Hing et al., 1999/Canada | Adults with AF in AF centres Exp: n = 148 Con: n = 139 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 65 | 24% | Usual care | 67 | 24% | Unclear |
| Guo et al., 2017/China | Adults with AF in hospitals Exp: n = 113 Con: n = 96 | mobile-based DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 67.4 | 42.5% | Usual care | 70.9 | 44.8% | High |
| Bajorek et al., 2016/Australia | Adults with AF in general practices Exp: n = 250 Con: n = 250 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 78.2 | 45.1% | Usual care | 77.7 | 46% | Unclear |
| Authors, year/country . | Participants . | Intervention . | Control . | Risk of bias . | ||||
|---|---|---|---|---|---|---|---|---|
| Type of intervention . | Age (mean) . | Female (%) . | Type of control . | Age (mean) . | Female (%) . | |||
| Van Doorn et al., 2018/The Netherlands | Adults with AF in general practice Exp: n = 1129 Con: n = 1226 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 77 | 49.4% | Usual care | 77 | 46.2% | Low |
| Arts et al., 2017/The Netherlands | Adults with AF in general practice Exp: n = 496 Con: n = 235 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 74.61 | / | Usual care | 72.61 | / | Low |
| Karlsson et al., 2018/Sweden | Adults with AF in general practice Exp: n = 8292 Con: n = 6508 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | / | 43% | Usual care | / | 43% | High |
| Fraenkel et al., 2012/USA | Adults with AF in general practice Exp: n = 69 Con: n = 66 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | / | 1% | Usual care | / | 2% | Low |
| Eckman et al., 2016/UK | Adults with AF in general practice Exp: n = 801 Con: n = 692 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 70.2 | 44% | Disseminations of didactic materials | 69.8 | 48% | Unclear |
| Thomson et al., 2007/UK | Adults with AF in general practice Exp: n = 69 Con: n = 67 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | 73.7 | 44.6% | Evidence-based paper guidelines | 73.1 | 43.4% | Low |
| McAlister et al., 2005/Canada | Adults with AF in general practice Exp: n = 228 Con: n = 218 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 73 | 43% | Usual care | 71 | 34% | High |
| Man-Son-Hing et al., 1999/Canada | Adults with AF in AF centres Exp: n = 148 Con: n = 139 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 65 | 24% | Usual care | 67 | 24% | Unclear |
| Guo et al., 2017/China | Adults with AF in hospitals Exp: n = 113 Con: n = 96 | mobile-based DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 67.4 | 42.5% | Usual care | 70.9 | 44.8% | High |
| Bajorek et al., 2016/Australia | Adults with AF in general practices Exp: n = 250 Con: n = 250 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 78.2 | 45.1% | Usual care | 77.7 | 46% | Unclear |
/, not reported; Con, control group; DA, decision aids; Exp, experimental group; NOAC, direct oral anticoagulant; SDM, shared decision-making.
Characteristics of the included studies
| Authors, year/country . | Participants . | Intervention . | Control . | Risk of bias . | ||||
|---|---|---|---|---|---|---|---|---|
| Type of intervention . | Age (mean) . | Female (%) . | Type of control . | Age (mean) . | Female (%) . | |||
| Van Doorn et al., 2018/The Netherlands | Adults with AF in general practice Exp: n = 1129 Con: n = 1226 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 77 | 49.4% | Usual care | 77 | 46.2% | Low |
| Arts et al., 2017/The Netherlands | Adults with AF in general practice Exp: n = 496 Con: n = 235 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 74.61 | / | Usual care | 72.61 | / | Low |
| Karlsson et al., 2018/Sweden | Adults with AF in general practice Exp: n = 8292 Con: n = 6508 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | / | 43% | Usual care | / | 43% | High |
| Fraenkel et al., 2012/USA | Adults with AF in general practice Exp: n = 69 Con: n = 66 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | / | 1% | Usual care | / | 2% | Low |
| Eckman et al., 2016/UK | Adults with AF in general practice Exp: n = 801 Con: n = 692 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 70.2 | 44% | Disseminations of didactic materials | 69.8 | 48% | Unclear |
| Thomson et al., 2007/UK | Adults with AF in general practice Exp: n = 69 Con: n = 67 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | 73.7 | 44.6% | Evidence-based paper guidelines | 73.1 | 43.4% | Low |
| McAlister et al., 2005/Canada | Adults with AF in general practice Exp: n = 228 Con: n = 218 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 73 | 43% | Usual care | 71 | 34% | High |
| Man-Son-Hing et al., 1999/Canada | Adults with AF in AF centres Exp: n = 148 Con: n = 139 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 65 | 24% | Usual care | 67 | 24% | Unclear |
| Guo et al., 2017/China | Adults with AF in hospitals Exp: n = 113 Con: n = 96 | mobile-based DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 67.4 | 42.5% | Usual care | 70.9 | 44.8% | High |
| Bajorek et al., 2016/Australia | Adults with AF in general practices Exp: n = 250 Con: n = 250 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 78.2 | 45.1% | Usual care | 77.7 | 46% | Unclear |
| Authors, year/country . | Participants . | Intervention . | Control . | Risk of bias . | ||||
|---|---|---|---|---|---|---|---|---|
| Type of intervention . | Age (mean) . | Female (%) . | Type of control . | Age (mean) . | Female (%) . | |||
| Van Doorn et al., 2018/The Netherlands | Adults with AF in general practice Exp: n = 1129 Con: n = 1226 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 77 | 49.4% | Usual care | 77 | 46.2% | Low |
| Arts et al., 2017/The Netherlands | Adults with AF in general practice Exp: n = 496 Con: n = 235 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 74.61 | / | Usual care | 72.61 | / | Low |
| Karlsson et al., 2018/Sweden | Adults with AF in general practice Exp: n = 8292 Con: n = 6508 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | / | 43% | Usual care | / | 43% | High |
| Fraenkel et al., 2012/USA | Adults with AF in general practice Exp: n = 69 Con: n = 66 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | / | 1% | Usual care | / | 2% | Low |
| Eckman et al., 2016/UK | Adults with AF in general practice Exp: n = 801 Con: n = 692 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 70.2 | 44% | Disseminations of didactic materials | 69.8 | 48% | Unclear |
| Thomson et al., 2007/UK | Adults with AF in general practice Exp: n = 69 Con: n = 67 | Computerized DA to facilitate decision-making in OAC therapy (warfarin) | 73.7 | 44.6% | Evidence-based paper guidelines | 73.1 | 43.4% | Low |
| McAlister et al., 2005/Canada | Adults with AF in general practice Exp: n = 228 Con: n = 218 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 73 | 43% | Usual care | 71 | 34% | High |
| Man-Son-Hing et al., 1999/Canada | Adults with AF in AF centres Exp: n = 148 Con: n = 139 | Booklet and audiotape DA to facilitate decision-making in OAC therapy (warfarin) | 65 | 24% | Usual care | 67 | 24% | Unclear |
| Guo et al., 2017/China | Adults with AF in hospitals Exp: n = 113 Con: n = 96 | mobile-based DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 67.4 | 42.5% | Usual care | 70.9 | 44.8% | High |
| Bajorek et al., 2016/Australia | Adults with AF in general practices Exp: n = 250 Con: n = 250 | Computerized DA to facilitate decision-making in OAC therapy (warfarin/NOACs) | 78.2 | 45.1% | Usual care | 77.7 | 46% | Unclear |
/, not reported; Con, control group; DA, decision aids; Exp, experimental group; NOAC, direct oral anticoagulant; SDM, shared decision-making.
Characteristics of the reviewed decision aids
| Study . | Format . | Delivery . | Contents (SDM elements in DA) . | SDM outcomes . | Health outcome . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Situation diagnosis . | Choice awareness . | Option clarification . | Harms and benefits . | Patient preference . | Making decision . | Knowledge . | Decisional conflict . | Proportion of OAC uptake . | Adherence to OAC therapy . | Incidence of stroke . | Incidence of bleeding . |
| Van Doorn et al., 2018 | Computerized DA | Within the consultation | √ | • | √ | ? | ? | ? | • | • | ↔ | • | ↔ | ↔ |
| Arts et al., 2017 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Karlsson et al., 2018 | Computerized DA | Within the consultation | √ | ? | √ | • | • | • | • | • | • | ↔ | ||
| Fraenkel et al., 2012 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | • | Accuracy of treatment options | Decisional conflict scale | • | • | • | • |
| Eckman et al., 2016 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Thomson et al., 2007 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Knowledge score on warfarin ↔ | Decisional conflict scale | • | • | • | • |
| McAlister et al., 2005 | Booklet and audiotape DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Accuracy of stroke risk without OAC | Decisional conflict scale | Proportion of adherent participants at 3-month follow-up | • | • | |
| Man-Son-Hing, et al., 1999 | Booklet and audiotape DA | Prior to the consultation | ? | √ | √ | √ | √ | √ | Self-designed scale on AF and OAC therapy | Decisional conflict scale | ↔ | Proportion of adherent participants at 6-month follow-up ↔ | • | • |
| Guo et al., 2017 | Mobile-based DA | After the consultation/discharge | √ | √ | √ | √ | √ | • | The AF knowledge scale (evaluating AF symptoms and OAC therapy) | • | • | Pharmacy quality alliance adherence scale Measured at 3-month follow-up | • | • |
| Bajorek et al., 2016 | Computerized DA | Within the consultation | √ | ? | √ | √ | • | • | • | • | • | • | • | |
| Study . | Format . | Delivery . | Contents (SDM elements in DA) . | SDM outcomes . | Health outcome . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Situation diagnosis . | Choice awareness . | Option clarification . | Harms and benefits . | Patient preference . | Making decision . | Knowledge . | Decisional conflict . | Proportion of OAC uptake . | Adherence to OAC therapy . | Incidence of stroke . | Incidence of bleeding . |
| Van Doorn et al., 2018 | Computerized DA | Within the consultation | √ | • | √ | ? | ? | ? | • | • | ↔ | • | ↔ | ↔ |
| Arts et al., 2017 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Karlsson et al., 2018 | Computerized DA | Within the consultation | √ | ? | √ | • | • | • | • | • | • | ↔ | ||
| Fraenkel et al., 2012 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | • | Accuracy of treatment options | Decisional conflict scale | • | • | • | • |
| Eckman et al., 2016 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Thomson et al., 2007 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Knowledge score on warfarin ↔ | Decisional conflict scale | • | • | • | • |
| McAlister et al., 2005 | Booklet and audiotape DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Accuracy of stroke risk without OAC | Decisional conflict scale | Proportion of adherent participants at 3-month follow-up | • | • | |
| Man-Son-Hing, et al., 1999 | Booklet and audiotape DA | Prior to the consultation | ? | √ | √ | √ | √ | √ | Self-designed scale on AF and OAC therapy | Decisional conflict scale | ↔ | Proportion of adherent participants at 6-month follow-up ↔ | • | • |
| Guo et al., 2017 | Mobile-based DA | After the consultation/discharge | √ | √ | √ | √ | √ | • | The AF knowledge scale (evaluating AF symptoms and OAC therapy) | • | • | Pharmacy quality alliance adherence scale Measured at 3-month follow-up | • | • |
| Bajorek et al., 2016 | Computerized DA | Within the consultation | √ | ? | √ | √ | • | • | • | • | • | • | • | |
?, unclear; ↑, favoured DA; ↔, no statistically significant effect; √, present; DA, decision aids; Elements: •, not present; OAC, oral anticoagulant; Outcomes: •, not reported; SDM, shared decision-making.
Characteristics of the reviewed decision aids
| Study . | Format . | Delivery . | Contents (SDM elements in DA) . | SDM outcomes . | Health outcome . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Situation diagnosis . | Choice awareness . | Option clarification . | Harms and benefits . | Patient preference . | Making decision . | Knowledge . | Decisional conflict . | Proportion of OAC uptake . | Adherence to OAC therapy . | Incidence of stroke . | Incidence of bleeding . |
| Van Doorn et al., 2018 | Computerized DA | Within the consultation | √ | • | √ | ? | ? | ? | • | • | ↔ | • | ↔ | ↔ |
| Arts et al., 2017 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Karlsson et al., 2018 | Computerized DA | Within the consultation | √ | ? | √ | • | • | • | • | • | • | ↔ | ||
| Fraenkel et al., 2012 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | • | Accuracy of treatment options | Decisional conflict scale | • | • | • | • |
| Eckman et al., 2016 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Thomson et al., 2007 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Knowledge score on warfarin ↔ | Decisional conflict scale | • | • | • | • |
| McAlister et al., 2005 | Booklet and audiotape DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Accuracy of stroke risk without OAC | Decisional conflict scale | Proportion of adherent participants at 3-month follow-up | • | • | |
| Man-Son-Hing, et al., 1999 | Booklet and audiotape DA | Prior to the consultation | ? | √ | √ | √ | √ | √ | Self-designed scale on AF and OAC therapy | Decisional conflict scale | ↔ | Proportion of adherent participants at 6-month follow-up ↔ | • | • |
| Guo et al., 2017 | Mobile-based DA | After the consultation/discharge | √ | √ | √ | √ | √ | • | The AF knowledge scale (evaluating AF symptoms and OAC therapy) | • | • | Pharmacy quality alliance adherence scale Measured at 3-month follow-up | • | • |
| Bajorek et al., 2016 | Computerized DA | Within the consultation | √ | ? | √ | √ | • | • | • | • | • | • | • | |
| Study . | Format . | Delivery . | Contents (SDM elements in DA) . | SDM outcomes . | Health outcome . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Situation diagnosis . | Choice awareness . | Option clarification . | Harms and benefits . | Patient preference . | Making decision . | Knowledge . | Decisional conflict . | Proportion of OAC uptake . | Adherence to OAC therapy . | Incidence of stroke . | Incidence of bleeding . |
| Van Doorn et al., 2018 | Computerized DA | Within the consultation | √ | • | √ | ? | ? | ? | • | • | ↔ | • | ↔ | ↔ |
| Arts et al., 2017 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Karlsson et al., 2018 | Computerized DA | Within the consultation | √ | ? | √ | • | • | • | • | • | • | ↔ | ||
| Fraenkel et al., 2012 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | • | Accuracy of treatment options | Decisional conflict scale | • | • | • | • |
| Eckman et al., 2016 | Computerized DA | Within the consultation | √ | • | √ | • | • | • | • | • | ↔ | • | • | • |
| Thomson et al., 2007 | Computerized DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Knowledge score on warfarin ↔ | Decisional conflict scale | • | • | • | • |
| McAlister et al., 2005 | Booklet and audiotape DA | Prior to the consultation | √ | √ | √ | √ | √ | √ | Accuracy of stroke risk without OAC | Decisional conflict scale | Proportion of adherent participants at 3-month follow-up | • | • | |
| Man-Son-Hing, et al., 1999 | Booklet and audiotape DA | Prior to the consultation | ? | √ | √ | √ | √ | √ | Self-designed scale on AF and OAC therapy | Decisional conflict scale | ↔ | Proportion of adherent participants at 6-month follow-up ↔ | • | • |
| Guo et al., 2017 | Mobile-based DA | After the consultation/discharge | √ | √ | √ | √ | √ | • | The AF knowledge scale (evaluating AF symptoms and OAC therapy) | • | • | Pharmacy quality alliance adherence scale Measured at 3-month follow-up | • | • |
| Bajorek et al., 2016 | Computerized DA | Within the consultation | √ | ? | √ | √ | • | • | • | • | • | • | • | |
?, unclear; ↑, favoured DA; ↔, no statistically significant effect; √, present; DA, decision aids; Elements: •, not present; OAC, oral anticoagulant; Outcomes: •, not reported; SDM, shared decision-making.
Data synthesis for outcome measures
Decisional conflict
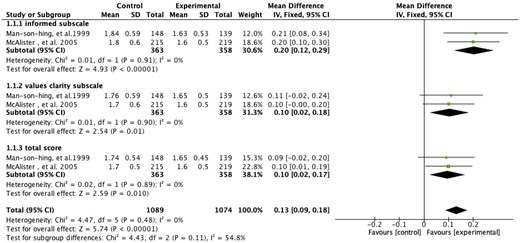
Four studies examined the effects of DAs on decisional conflict related to warfarin use. All studies measured decisional conflict by the decisional conflict scale (DCS), which consisted of the informed subscale and value clarity subscale. Pooling analysis was conducted for two studies,22,23 and the result showed significant differences in DCS total score (MD: −0.10, 95% CI: −0.18 to −0.02, P = 0.01; I2 = 0%), DCS informed subscale score (MD: −0.20, 95% CI: −0.29 to −0.12, P < 0.001; I2 = 0%), and DCS value clarity subscale score (MD: −0.10, 95% CI: −0.18 to −0.02, P = 0.01; I2 = 0%) (Figure 3). The other two studies were not available for pooling. One study24 reported significant effects of DAs on DCS total score (MD = 0.18, 95% CI: −0.34 to −0.01, P < 0.05); the other25 reported significant effects on DCS informed subscale and value clarity subscale with effect sizes being 0.3 and 0.5, respectively.
Forest plot of the effect of decision aids on decisional conflict.
Knowledge
Five studies examined the effects of DAs on patients’ AF knowledge. Pooling analysis was not available, as the questions posed to participants across the studies varied. The study by Fraenkel et al.24 reported that participants in the intervention group were significantly more likely to be able to name the medications for reducing stroke risk (odds ratio = 3.5, 95% CI: 1.6–7.7, P < 0.05). The study by McAlister et al.23 reported that participants in the intervention group were significantly more knowledgeable in estimating their personal stroke risk without treatment (MD = 12%, P < 0.05). In the study conducted by Thomson et al.,25 no significant difference was found in the level of knowledge on warfarin therapy between groups after the intervention (P > 0.05). The study by Man-Son-Hing et al.22 reported significant effects of DAs on improving the accurate response rate of self-designed OAC therapy questions between groups (MD = 14.9%, P < 0.05). The study by Guo et al.26 used the AF knowledge scale to evaluate participants’ knowledge, significant effects were observed (P < 0.05).
Proportion of OAC uptake
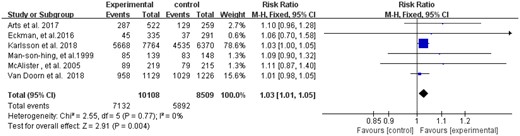
Seven studies examined the effects of DAs on the proportion of OAC uptake. Data from six studies22,23,27,–30 were available for pooling, and the results showed a significant difference (RR: 1.03, 95% CI: 1.01–1.05, P = 0.004; I2 = 0%) (Figure 4). The unpooled study31 found that patients in the intervention group are 2.8 times more likely to receive an anticoagulant therapy than those in the control group (P = 0.02).
Forest plot of the effect of decision aids on the proportion of anticoagulant therapy.
Adherence to OAC therapy
Three studies examined the effects of DAs on patients’ adherence to their OAC therapy decision during the follow-up. One study22 reported no significant difference in the self-report adherence between groups in the six-month follow-up period (P > 0.05). The study by McAlister et al.23 reported significant effects of DAs on improving the self-report adherence rate between groups at 3-month follow-up (MD = 11.9%, P < 0.05). The study by Guo et al.26 used the 3-item pharmacy quality alliance adherence measure and reported a significant increase in adherence to OAC therapy in the intervention group at 3-month follow-up (P < 0.05).
Incidence of stroke
Two studies followed up the effects of DAs on patients’ stroke incidence. Both studies did not find any significant differences between groups in the incidence rate of stroke at either 1-year follow-up29 or 2.7-year follow-up period.30
Incidence of bleeding
Two studies followed up the effects of DAs on patients’ major bleeding incidence. One study29 reported that the intervention group had a significantly lower incidence of major bleeding at 1-year follow-up with events in 12 (95% CI: 9–15) per 1000 patients in the intervention group compared to 16 (95% CI: 12–20) per 1000 patients in the control group (P = 0.04). The other study reported no significant differences between groups in the incidence rate of major bleeding at 2.7-year follow-up.30
Comparative analysis of DA characteristics on the outcomes
A comparative analysis was conducted to explore how the differences in intervention design were related to the study outcomes (Table 3). Three DAs (30%) were ineffective on neither direct outcomes of SDM (i.e. knowledge, decisional conflict, OAC uptake and adherence) nor long-term health effects (incidence of stroke and bleeding). The intervention design of these ineffective DAs was compared with those of seven DAs (70%) that were effective on at least one of the outcomes. The ineffective DAs were delivered within the consultation, and five of the seven effective DAs (71%) were delivered before the consultation. In addition to DA delivery, the key SDM elements covered varied greatly between effective and ineffective DAs. These ineffective DAs omitted the SDM element other than situation diagnosis and option clarification. However, six of the seven effective DAs (85%) covered the discussion on benefits and disadvantages and/or choice awareness/patient preference/making decision.
Discussion
Summary of findings
This systematic review evaluated the effects of DAs on SDM and health outcomes regarding anticoagulant use in patients with AF and further explored any differential benefits among different DA designs. Moderate quality evidence suggests that the DAs are associated with significant effects on reducing the decisional conflict related to warfarin use, which stems from the feeling of being uninformed and the lack of clarity regarding their values. Low-quality evidence suggests that the DAs are associated with significant effects on improving disease-related knowledge. The effects of DAs on the reduction of the incidence rate of stroke or bleeding remain unknown. Further comparative analysis indicated that the designs of the DAs may also exert influence on SDM outcomes. Specifically, DAs delivered prior to consultation may be more effective than those delivered within the consultation. The DAs that only included situation diagnosis and option clarification may not be sufficient to achieve beneficial effects on patients with AF.
The results supported the favourable effects of DAs on patient knowledge and decisional conflict observed in previous narrative reviews conducted by O’Neill et al.18 and Sheibani et al.19 These observations suggested that when informing people about this complex and value-sensitive decision, DAs may help people feel more informed and more comfortable with their choices than the usual care. Furthermore, the present review provided new evidence on DA’s effect on the increase in the OAC uptake by data pooling. This observation was clinically important, because it suggested that the beneficial effects of DAs on patients’ knowledge and decisional conflict can translate to actual reasonable decision-making.
Although the limited number of studies did not allow subgroup data synthesis, the systematic comparison analysis provided further insights, which explained how DAs support SDM with regards to OAC treatment in AF. Whether the DA is in computer-based or paper-based format, no difference was found in SDM outcomes. However, the DAs delivered prior to consultation may be more effective than those delivered within the consultation. This may be due to the fact that the former allows the patients to have more time to digest the information and be prepared for making the decision. Moreover, the comparative analysis of the key SDM elements covered in different DAs provides important implications. DAs that only contain situation diagnosis and option clarification may not empower patients to make informed decisions regarding anticoagulant treatment. To communicate the personal values they place on the benefits versus the disadvantages of achieving SDM to healthcare professionals, people need to comprehend the risks and benefits of the different preferences. This finding is supported by the results of the comparative analysis, which indicated that six out of seven effective DAs included the clarification of disadvantages and benefits of choices other than situation diagnosis and option clarification. Most of the effective studies (5/7) were designed according to the IPDAS collaboration and included all five SDM key elements to facilitate SDM, except for two effective DAs, which did not incorporate the preference awareness and deliberation of patient preferences. We are unable to delineate the additional effects of the two elements on SDM due to limited studies and lack of sensitive outcomes.
The effects of DAs on the reduction of the incidence rate of stroke or bleeding in patients with AF were unclear, because only two studies followed up these outcomes and obtained negative findings. The negative findings may be related to the fact that the two DAs only included situation diagnosis and option clarification, which were insufficient to empower the patients to make informed decisions. In both studies, OAC uptake did not increase immediately after the intervention. To obtain a more comprehensive understanding on the benefits of DAs, further research with well-designed DAs and longer follow-up are required to investigate the influence of DAs on the prevention of stroke or bleeding, which is among the most important management goals for patients with AF.
Implications for practice
Suboptimal OAC uptake is highly prevalent in patients with AF. The findings of this review showed that the DAs are effective in facilitating the OAC uptake in AF by improving patients’ knowledge and reducing decisional conflict. A qualified DA should cover five SDM key elements, namely, situation diagnosis, choice awareness, option clarification, discussion of harms, and benefits and deliberation of patient preferences, in line with the IPDAS collaboration. Such DAs should be delivered prior to the consultation rather than during the consultation to better prepare the patients for the SDM. In fact, although DAs have been evaluated in studies involving patients with AF, they are still not widely available for clinical use,16 thereby limiting their applicability. To facilitate the use of effective DAs in clinical practice, parallel efforts should be made to train the healthcare professionals for them to obtain SDM knowledge and skills. Furthermore, the interprofessional SDM model, which builds on the strengths of each profession, could be adopted to optimize the care delivery. A good example is the study by Fraenkel et al.,24 who confirmed the effectiveness of an interprofessional SDM model, in which the nurses and physicians collaborated with the patient to reach a decision. The nurses used the DA to support patient engagement in SDM and provided individualized patient education on the connection between AF and stroke and their risk of stroke, as well as a list of options and the disadvantages and benefits of each option. Meanwhile, the participants were encouraged to discuss their preference and reasons. Subsequently, the clinicians guided the patients through deliberation and communication and worked together to reach an agreed-upon decision. Nurses are influential in the SDM process when patients face complex and preference-sensitive decisions.32 Nurses need to play a more active role in SDM to better support patients with AF in making tough decisions.
Limitations
Firstly, this study was not prospectively registered. Secondly, only a limited number of studies were included in this review. Thus, the subgroup effect of different intervention designs on the effects size was not analysed. Thirdly, although the pooling results for decisional conflict demonstrated positive results, the studies pooled were undertaken in the pre-NOAC era. Therefore, further investigation is warranted before the application of such results in the current clinical practice. Finally, the results of the comparative analysis between effective and ineffective DAs should be interpreted with caution, as other participant factors (e.g. general and health literacy), staff training variations and DA quality that were not reported by the included studies may confound the results.
Conclusion
DAs are associated with reduced decisional conflict, improved knowledge, and OAC uptake in AF. Designing DAs according to the IPDAS collaboration and delivering them before consultation are recommended in future studies. However, given the limitations of the reviewed studies, the effects of such DAs on the prevention of stroke and major bleeding in AF remain inconclusive. Investigations with rigorous study design and long follow-up are required to provide the evidence.
Supplementary material
Supplementary material is available at European Journal of Cardiovascular Nursing online.
Funding
This research received external funding from the Humanities and Social Sciences Grants from the Ministry of Education of the People Republics of China (20YJCZH132) and the Shenzhen Science and Technology Innovation Committee (JCYJ20190812152401678).
Conflict of Interest: none declared.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
January CT, Wann LS, Calkins H, Field ME, Chen LY, Furie KL, Cigarroa JE, Heidenreich PA, Cleveland JC, Murray KT, Ellinor PT, Shea, JB, Ezekowitz MD; Tracy CM; Yancy CW.



Comments