Abstract
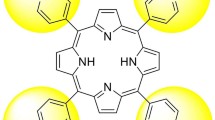
Hand hygiene is one of the most important interventions for reducing transmission of nosocomial life-threatening microorganisms, like methicillin resistant Staphylococcus aureus (MRSA), enterohemorrhagic Escherichia coli (EHEC) or Candida albicans. All three pathogens have become a leading cause of infections in hospitals. Especially EHEC is causing severe diarrhoea and, in a small percentage of cases, haemolytic-uremic syndrome (HUS) as reported for E. coli 104:H4 in Germany 2011. We revealed the possibility to inactivate very fast and efficiently MRSA, EHEC and C. albicans using the photodynamic approach. MRSA, EHEC and C. albicans were incubated in vitro with different concentrations of TMPyP for 10 s and illuminated with visible light (50 mW cm−2) for 10 and 60 s. 1 μmol l−1 of TMPyP and an applied radiant exposure of 0.5 J cm−2 achieved a photodynamic killing of ≥99.9% of MRSA and EHEC. Incubation with higher concentrations (up to 100 μmol l−1) of TMPyP caused bacteria killing of >5 log10 (≥99.999%) after illumination. Efficient Candida killing (≥99.999%) was achieved first at a higher light dose of 12 J cm−2. Different rise and decay times of singlet oxygen luminescence signals could be detected in Candida cell suspensions for the first time, indicating different oxygen concentrations in the surrounding for the photosensitizer and singlet oxygen, respectively. This confirms that TMPyP is not only found in the water-dominated cell surrounding, but also within the C. albicans cells. Applying a water-ethanol solution of TMPyP on ex vivo porcine skin, fluorescence microscopy of histology showed that the photosensitizer was exclusively localized in the stratum corneum regardless of the incubation time. TMPyP exhibited a fast and very effective killing rate of life-threatening pathogens within a couple of seconds that encourages further testing in an in vivo setting. Being fast and effective, antimicrobial photodynamic applications might become acceptable as a tool for hand hygiene procedures and also in other skin areas.
Similar content being viewed by others

References
J. Kluytmans, A. van Belkum, and H. Verbrugh, Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks, Clin. Microbiol. Rev., 1997, 10, 505–520.
R. Kock, A. Mellmann, F. Schaumburg, A. W. Friedrich, F. Kipp, and K. Becker, The epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) in Germany, Dtsch. Arztebl. Int., 2011, 108, 761–767.
Y. H. Samaranayake, B. P. Cheung, N. Parahitiyawa, C. J. Seneviratne, J. Y. Yau, K. W. Yeung, and L. P. Samaranayake, Synergistic activity of lysozyme and antifungal agents against Candida albicans biofilms on denture acrylic surfaces, Arch. Oral Biol., 2009, 54, 115–126.
D. M. Arana, C. Nombela, and J. Pla, Fluconazole at subinhibitory concentrations induces the oxidative- and nitrosative-responsive genes TRR1, GRE2 and YHB1, and enhances the resistance of Candida albicans to phagocytes, J. Antimicrob. Chemother., 2010, 65, 54–62.
S. Mathur, and R. Singh, Antibiotic resistance in food lactic acid bacteria–a review, Int. J. Food Microbiol., 2005, 105, 281–295.
J. R. Bower, Foodborne diseases: Shiga toxin producing E. coli (STEC), Pediatr. Infect Dis. J., 1999, 18, 909–910.
P. C. Appelbaum, The emergence of vancomycin-intermediate and vancomycin-resistant Staphylococcus aureus, Clin. Microbiol. Infect., 2006, 12 Suppl 1, 16–23.
J. Y. Ang, E. Ezike, and B. I. Asmar, Antibacterial resistance, Indian J. Pediatr., 2004, 71, 229–239.
R. M. Chapple, B. Inglis, and P. R. Stewart, Lethal and mutational effects of solar and UV radiation on Staphylococcus aureus, Arch. Microbiol., 1992, 157, 242–248.
W. M. Snellings, C. S. Weil, and R. R. Maronpot, A two-year inhalation study of the carcinogenic potential of ethylene oxide in Fischer 344 rats, Toxicol. Appl. Pharmacol., 1984, 75, 105–117.
J. A. Imlay, S. M. Chin, and S. Linn, Toxic DNA damage by hydrogen peroxide through the Fenton reaction in vivoin vitro, Science, 1988, 240, 640–642.
B. V. Krishna, and A. P. Gibb, Use of octenidine dihydrochloride in methicillin-resistant Staphylococcus aureus decolonisation regimens: a literature review, J. Hosp. Infect., 2010, 74, 199–203.
G. Judah, P. Donachie, E. Cobb, W. Schmidt, M. Holland, and V. Curtis, Dirty hands: bacteria of faecal origin on commuters’ hands, Epidemiol. Infect., 2010, 138, 409–414.
F. Gad, T. Zahra, K. P. Francis, T. Hasan, and M. R. Hamblin, Targeted photodynamic therapy of established soft-tissue infections in mice, Photochem. Photobiol. Sci., 2004, 3, 451–458.
N. Komerik, H. Nakanishi, A. J. MacRobert, B. Henderson, P. Speight, and M. Wilson, In vivo killing of Porphyromonas gingivalis by toluidine blue-mediated photosensitization in an animal model, Antimicrob Agents Chemother., 2003, 47, 932–940.
T. Maisch, J. Wagner, V. Papastamou, H. J. Nerl, K. A. Hiller, R. M. Szeimies, and G. Schmalz, Combination of 10% EDTA, Photosan, and a blue light hand-held photopolymerizer to inactivate leading oral bacteria in dentistry in vitro, J. Appl. Microbiol., 2009, 107, 1569–1578.
A. S. Garcez, S. C. Nunez, M. R. Hamblin, and M. S. Ribeiro, Antimicrobial effects of photodynamic therapy on patients with necrotic pulps and periapical lesion, J. Endod., 2008, 34, 138–142.
A. S. Garcez, S. C. Nunez, J. L. Lage-Marques, M. R. Hamblin, and M. S. Ribeiro, Photonic real-time monitoring of bacterial reduction in root canals by genetically engineered bacteria after chemomechanical endodontic therapy, Braz Dent. J., 2007, 18, 202–207.
X. Ragas, T. Dai, G. P. Tegos, M. Agut, S. Nonell, and M. R. Hamblin, Photodynamic inactivation of Acinetobacter baumannii using phenothiazinium dyes: in vitroin vivo studies, Lasers Surg. Med., 2011, 42, 384–390.
Y. Nitzan, R. Dror, H. Ladan, Z. Malik, S. Kimel, and V. Gottfried, Structure–activity relationship of porphines for photoinactivation of bacteria, Photochem. Photobiol., 1995, 62, 342–347.
E. Alves, L. Costa, C. M. Carvalho, J. P. Tome, M. A. Faustino, M. G. Neves, A. C. Tome, J. A. Cavaleiro, A. Cunha, and A. Almeida, Charge effect on the photoinactivation of Gram-negative and Gram-positive bacteria by cationic meso-substituted porphyrins, BMC Microbiol., 2009, 9, 70.
T. Maisch, J. Baier, B. Franz, M. Maier, M. Landthaler, R. M. Szeimies, and W. Baumler, The role of singlet oxygen and oxygen concentration in photodynamic inactivation of bacteria, Proc. Natl. Acad. Sci. U. S. A., 2007, 104, 7223–7228.
M. Merchat, G. Bertolini, P. Giacomini, A. Villanueva, and G. Jori, Meso-substituted cationic porphyrins as efficient photosensitizers of gram-positive and gram-negative bacteria, J. Photochem. Photobiol., B., 1996, 32, 153–157.
M. Salmon-Divon, Y. Nitzan, and Z. Malik, Mechanistic aspects of Escherichia coli photodynamic inactivation by cationic tetra-meso(N-methylpyridyl)porphine, Photochem. Photobiol. Sci., 2004, 3, 423–429.
L. Brancaleon, and H. Moseley, Laser and non-laser light sources for photodynamic therapy, Lasers Med. Sci., 2002, 17, 173–186.
J. Regensburger, T. Maisch, A. Felgentrager, F. Santarelli, and W. Baumler, A helpful technology–the luminescence detection of singlet oxygen to investigate photodynamic inactivation of bacteria (PDIB), J. Biophotonics., 2010, 3, 319–327.
J. Baier, T. Fuß, C. Pöllmann, C. Wiesmann, K. Pindl, R. Engl, D. Baumer, M. Maier, M. Landthaler, W. Bäumler, Theoretical and experimental analysis of the luminescence signal of singlet oxygen for different photosensitizers, J. Photochem. Photobiol. B: Biol., 2007, 87, 163–173.
A. A. Miles, S. S. Misra, and J. O. Irwin, The estimation of the bactericidal power of the blood, J. Hyg. (Lond)., 1938, 38, 732–749.
T. Mosmann, Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays, J. Immunol. Methods., 1983, 65, 55–63.
J. M. Boyce, and D. Pittet, Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force, Am. J. Infect. Control., 2002, 30, S1–S46.
S. B. al-Masaudi, M. J. Day, and A. D. Russell, Antimicrobial resistance and gene transfer in Staphylococcus aureus, J. Appl. Bacteriol., 1991, 70, 279–290.
F. Baquero, J. F. Barrett, P. Courvalin, I. Morrissey, L. Piddock, and W. J. Novick, Epidemiology and mechanisms of resistance among respiratory tract pathogens, Clin. Microbiol. Infect., 1998, 4 Suppl 2, S19–S26.
L. Birosova, and M. Mikulasova, Development of triclosan and antibiotic resistance in Salmonella enterica serovar Typhimurium, J. Med. Microbiol., 2009, 58, 436–441.
K. Komagoe, H. Kato, T. Inoue, and T. Katsu, Continuous real-time monitoring of cationic porphyrin-induced photodynamic inactivation of bacterial membrane functions using electrochemical sensors, Photochem. Photobiol. Sci., 2011, 10, 1181–1188.
T. Maisch, C. Bosl, R. M. Szeimies, N. Lehn, and C. Abels, Photodynamic effects of novel XF porphyrin derivatives on prokaryotic and eukaryotic cells, Antimicrob. Agents Chemother., 2005, 49, 1542–1552.
T. Breitenbach, M. K. Kuimova, P. Gbur, S. Hatz, N. B. Schack, B. W. Pedersen, J. D. Lambert, L. Poulsen, and P. R. Ogilby, Photosensitized production of singlet oxygen: spatially-resolved optical studies in single cells, Photochem. Photobiol. Sci., 2009, 8, 442–452.
R. F. Pfeltz, V. K. Singh, J. L. Schmidt, M. A. Batten, C. S. Baranyk, M. J. Nadakavukaren, R. K. Jayaswal, and B. J. Wilkinson, Characterization of passage-selected vancomycin-resistant Staphylococcus aureus strains of diverse parental backgrounds, Antimicrob. Agents Chemother., 2000, 44, 294–303.
V. Gottfried, D. Peled, J. W. Winkelman, and S. Kimel, Photosensitizers in organized media: singlet oxygen production and spectral properties, Photochem. Photobiol., 1988, 48, 157–163.
Y. Usui, Determination of quantum yield of Singlet Oxygen Formation by Photosensitization, Chem. Lett., 1973, 7, 743–744.
R. Pottier, A. Lachaine, M. Pierre, and J. C. Kennedy, A new electronic absorbance band in concentrated aqueous solutions of hematoporphyrin IX detected by photoacoustic spectroscopy, Photochem. Photobiol., 1988, 47, 669–674.
I. J. Davis, H. Richards, and P. Mullany, Isolation of silver- and antibiotic-resistant Enterobacter cloacae from teeth, Oral Microbiol. Immunol., 2005, 20, 191–194.
J. T. Trevors, Copper resistance in bacteria, Microbiol. Sci., 1987, 4, 29–31.
S. Silver, Bacterial resistances to toxic metal ions–a review, Gene, 1996, 179, 9–19.
M. M. Huycke, D. F. Sahm, and M. S. Gilmore, Multiple-drug resistant enterococci: the nature of the problem and an agenda for the future, Emerg. Infect. Dis., 1998, 4, 239–249.
M. Grinholc, B. Szramka, K. Olender, and A. Graczyk, Bactericidal effect of photodynamic therapy against methicillin-resistant Staphylococcus aureus strain with the use of various porphyrin photosensitizers, Acta Biochim. Pol., 2007, 54, 665–670.
M. Grinholc, B. Szramka, J. Kurlenda, A. Graczyk, and K. P. Bielawski, Bactericidal effect of photodynamic inactivation against methicillin-resistant and methicillin-susceptible Staphylococcus aureus is strain-dependent, J. Photochem. Photobiol., B, 2008, 90, 57–63.
M. Grinholc, M. Richter, J. Nakonieczna, G. Fila, and K. P. Bielawski, The connection between agr and SCCmec elements of Staphylococcus aureus strains and their response to photodynamic inactivation, Photomed. Laser Surg., 2011, 29, 413–419.
G. Jori, C. Fabris, M. Soncin, S. Ferro, O. Coppellotti, D. Dei, L. Fantetti, G. Chiti, and G. Roncucci, Photodynamic therapy in the treatment of microbial infections: basic principles and perspective applications, Lasers Surg. Med., 2006, 38, 468–481.
S. Viazis, M. Akhtar, J. Feirtag, F. Diez-Gonzalez, Reduction of Escherichia coli O157:H7 viability on hard surfaces by treatment with a bacteriophage mixture, Int. J. Food Microbiol., 2011, 145, 37–42.
D. Goode, V. M. Allen, and P. A. Barrow, Reduction of experimental Salmonella and Campylobacter contamination of chicken skin by application of lytic bacteriophages, Appl. Environ. Microbiol., 2003, 69, 5032–5036.
M. Cislo, M. Dabrowski, B. Weber-Dabrowska, and A. Woyton, Bacteriophage treatment of suppurative skin infections, Arch. Immunol. Ther. Exp. (Warsz), 1987, 35, 175–183.
S. Guenther, D. Huwyler, S. Richard, and M. J. Loessner, Virulent bacteriophage for efficient biocontrol of Listeria monocytogenes in ready-to-eat foods, Appl. Environ. Microbiol., 2009, 75, 93–100.
R. Modi, Y. Hirvi, A. Hill, and M. W. Griffiths, Effect of phage on survival of Salmonella enteritidis during manufacture and storage of cheddar cheese made from raw and pasteurized milk, J. Food Prot., 2001, 64, 927–933.
B. Leverentz, W. S. Conway, Z. Alavidze, W. J. Janisiewicz, Y. Fuchs, M. J. Camp, E. Chighladze, and A. Sulakvelidze, Examination of bacteriophage as a biocontrol method for salmonella on fresh-cut fruit: a model study, J. Food Prot., 2001, 64, 1116–1121.
J. P. Nataro, C. A. Bopp, P. I. Fields, J. B. Kaper, and N. A. Strockbine, Escherichia, Shigella, and Salmonella, ASM Press, Washington, DC, USA, 9th edn., 2007.
F. Gad, T. Zahra, T. Hasan, and M. R. Hamblin, Effects of growth phase and extracellular slime on photodynamic inactivation of gram-positive pathogenic bacteria, Antimicrob. Agents Chemother., 2004, 48, 2173–2178.
T. N. Demidova, and M. R. Hamblin, Effect of cell-photosensitizer binding and cell density on microbial photoinactivation, Antimicrob. Agents Chemother., 2005, 49, 2329–2335.
B. Zeina, J. Greenman, W. M. Purcell, and B. Das, Killing of cutaneous microbial species by photodynamic therapy, Br. J. Dermatol., 2001, 144, 274–278.
W. Meyer, R. Schwarz, and K. Neurand, The skin of domestic mammals as a model for the human skin, with special reference to the domestic pig, Curr. Probl. Dermatol., 1978, 7, 39–52.
G. A. Simon, and H. I. Maibach, The pig as an experimental animal model of percutaneous permeation in man: qualitative and quantitative observations–an overview, Skin Pharmacol. Appl. Skin Physiol., 2000, 13, 229–234.
M. Whitby, M. L. McLaws, and M. W. Ross, Why healthcare workers don‘t wash their hands: a behavioral explanation, Infect Control Hosp. Epidemiol., 2006, 27, 484–492.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of a themed issue on current topics in photodermatology.
Rights and permissions
About this article
Cite this article
Eichner, A., Gonzales, F.P., Felgenträger, A. et al. Dirty hands: photodynamic killing of human pathogens like EHEC, MRSA and Candida within seconds. Photochem Photobiol Sci 12, 135–147 (2013). https://doi.org/10.1039/c2pp25164g
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1039/c2pp25164g