Abstract
Study design:
Case report.
Objective:
To present and discuss the case of a patient who sustained a significant flexion compression injury of the cervical spine with resulting tetraplegia and development of cortical blindness.
Setting:
National Spinal Injuries Unit and Institute of Neurological Sciences, Southern General Hospital, Glasgow, Scotland, UK.
Methods:
Clinical and radiological follow-up of the patient.
Results:
Cortical blindness resulted from vertebral artery dissection associated with blunt cervical spine trauma. The patient is registered blind and is ventilator dependent.
Conclusion:
The potential complications of blunt vertebral artery injury remain poorly recognised. Screening is routinely not performed. Advances in noninvasive radiological techniques may result in recognition of asymptomatic disease and the potential for therapeutic intervention.
Similar content being viewed by others
Introduction
Cerebrovascular insults following blunt cervical spine trauma were previously felt to be rare and of little practical significance.1 Application of vascular imaging has unmasked a higher incidence than previously thought, with increased awareness of potentially severe neurological complications. We report the case of an adult male who developed cervical cord injury secondary to multiple cervical vertebrae fractures, resulting in tetraplegia. Cortical blindness subsequently developed as a result of occipital infarction secondary to bilateral vertebral artery dissections.
Case report
A 30-year-old male dived head first into a paddling pool and collapsed. He had a cardio-respiratory arrest and was resuscitated at the scene. On arrival at a local hospital, there was no movement in the upper or lower limbs, he was areflexic and hypotonic, priapism was present, there was absent anal tone. Computerised tomographic (CT) scan of the brain was normal. He was intubated and ventilated.
Imaging of his cervical vertebrae demonstrated multiple fractures involving the posterior C3 vertebral body, bilateral inferior articular facet fractures of C3; fracture through the anterior inferior C5 vertebral body and also through the anterior superior C7 vertebral body. He was transferred to the local neurosurgical team. Initially he required inotropic support and i.v. antibiotics for aspiration pneumonia. Additional imaging with spinal MRI demonstrated a haemorrhage in the cord at the level of C3/4 with adjacent oedema.
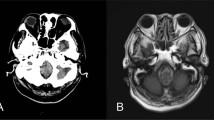
At 11 days post injury, he was transferred to the national spinal unit. Neurological examination of his limbs was limited due to heavy sedation. This was subsequently reduced and a nasal tube replaced the endotracheal tube before tracheostomy. His neck was maintained in a Philadelphia collar. Eye examination was documented as normal. Communication was difficult with no initial verbal response. His conscious state fluctuated but slowly improved. On day 28, he commented to nursing staff that he had difficulty focusing. Formal neuro-ophthamology assessment demonstrated bilateral visual loss. He was unable to perceive light with his right eye and had 6/60 vision with the left eye using the reduced Snellen chart at 1 m. There was no evidence of afferent pupillary defect. A diagnosis of cortical blindness was made. Repeated cranial CT scanning now showed a small infarct in the left thalamus (Figure 1a), with evidence of small areas of low density in the occipital lobes (Figure 1b). Poorly formed cortical responses to flash stimulation for both eyes on visually evoked responses (VER) were noted. CT angiogram demonstrated bilateral vertebral artery dissections, with a short segment of left vertebral artery occlusion between C3/4 and C4/5 (Figure 2). Anticoagulation with heparin was considered inappropriate on the basis of documented haemorrhage in the spinal cord and uncertain time of onset.
Repeated neuro-ophthamology assessment at 1 month showed failure of the patient to detect hand movements with either eye, but the ability to perceive light in all four quadrants. He has been registered blind and remains ventilator dependent.
Discussion
The path of the vertebral artery, as it courses the cervical vertebrae, makes it vulnerable to damage following injury to the cervical spine. The true incidence of vertebral artery injury following blunt trauma to the neck has been difficult to establish. Many patients are asymptomatic, while others have symptoms attributed to the traumatic injury before the onset of ischaemic sequelae. In a cohort of 38 patients with blunt vertebral artery injury (VAI), the incidence of posterior circulation stroke was 24% with an attributed death rate of 8%.2 A latent period of several weeks may separate the traumatic injury from the complications of ischaemia.3 Distal embolisation from established thrombosis at the site of injury is felt to be the causative factor and provides a potential window for stroke prevention. Awareness of the severe complications and the possibility of therapeutic intervention have led to the introduction of aggressive screening protocols in some centres. Two recently published series using digital subtraction arteriography (DSA) as part of an established screening protocol describe the incidence of VAI in 0.73 and 0.71% of all blunt traumatic admissions. In total, 605 (4.8%) and 216 (3.5%) patients admitted to their respective centres underwent DSA, detecting VAI in 15 and 20% of cases.4, 5 Cervical spine fractures were present in more than 70% of patients. Screening protocols used in both centres advised angiography in all cervical spine fractures. In a number of smaller studies, specific fracture types have been used to identify patients at a heightened risk of VAI. Nine out of 12 patients (75%) with facet joint dislocations were found to have vertebral artery occlusion.6 In eight patients with fractures involving the foramen transversarium of the cervical spine, seven (88%) had VAI.7 Combination of both these fracture types in a screening angiography protocol identified VAI in 12/26 patients (46%).8 Although accepted as the gold standard for the diagnosis of VAI, angiography is invasive and carries a risk of renal failure or stroke. In an attempt to limit the need for unnecessary DSA, it has recently been proposed that the screening criteria be redefined to include those patients with subluxation, extension into the foramen transversarium or upper C1–C3 fractures.4
Earlier comparisons of DSA with the noninvasive techniques of magnetic resonance angiography (MRA) and computerised tomographic angiography (CTA) have been disappointing. In an analysis of the three methods, CTA and MRA demonstrated sensitivities of 53 and 47% for blunt VAI compared to the accepted gold standard of DSA.5 Further advances in noninvasive radiological imaging, specifically CTA, now pose exciting alternatives for screening. Multisection CTA provides high-resolution and high-contrast images of the arterial lumen and wall. When compared to cerebral angiography in 19 patients with vertebral artery dissection and 49 controls, it gave 100% sensitivity and 98% specificity.9 Access to CTA and the suitability of patients for this method of noninvasive screening is very attractive. Contraindications and difficulties associated with MRA in ventilated spinal injury patients make CTA a more practical method of noninvasive screening. Improvements in ultrasound techniques have improved detection of features consistent with dissection, namely intimal flaps and fissures. The use of B-Flow, a method using ultrasound to detect blood flow was 98% sensitive for both carotid artery and vertebral artery dissection as compared to the 82 and 67%, respectively, using colour-coded Doppler in 11 patients with carotid artery and nine patients with vertebral artery dissections confirmed using MRA.10 The use of ultrasonographic techniques in the initial assessment of patients with suspected dissection has invariably required confirmatory testing with additional angiography, either invasively or noninvasively. The technique is dependent on the accessibility of the region to screening and although helpful for proximal dissections, the detection of more distal disease is limited11, 12
Controversy continues as to the optimal management of patients with asymptomatic vertebral artery injury. Guidelines published in 2002 indicated that there was insufficient evidence to support anticoagulation in asymptomatic patients, specifically relating to a 14% risk of complications from anticoagulant use.13 More recent evidence using a refined heparin regimen (target APTT of 40–50 s, no bolus) or anti-platelet agents in 39/50 patients with blunt VAI before the onset of ischaemia found a stroke rate of 2.6% compared to 54% in the untreated group.14 In patients with vertebral artery injury and evidence of posterior circulation stroke, anticoagulation with heparin results in better outcomes and is recommended as treatment.13
Current guidelines do not recommend screening of patients with cervical spine injuries for evidence of blunt vertebral or carotid artery injuries. The current case illustrates the devastating potential of vertebral artery dissection. Cortical blindness is characterised by loss of vision with preservation of pupillary responses and normal fundoscopy. Following vertebral artery injury, distal clot embolisation from a dissection or local thrombotic vessel occlusion resulted in posterior circulation ischaemia and resulting occipital lobe damage. Application of designated centres screening criteria to this patient would have warranted imaging for vascular injury. Cerebral angiography is invasive and not always readily available. Exposure of traumatised patients to invasive cerebral angiography and the paucity of evidence-based treatment has prevented universal acceptance of such an aggressive screening policy. We propose that when logistically possible, CTA should be considered at the time of cervical vertebrae assessment. Although controversy exists as to the best management of these patients, knowledge of vascular injury before the onset of discrete symptoms or acute ischaemia may assist in patient management.
References
Reid JD, Weigelt JA . Forty-three cases of vertebral artery trauma. J Trauma 1988; 28: 1007–1012.
Biffl WL et al. The devastating potential of blunt vertebral arterial injuries. Ann Surg 2000; 231: 672–681.
Nazir FS, Muir KW . Prolonged interval between vertebral artery dissection and ischemic stroke. Neurology 2004; 62: 1646–1647.
Cothren CC et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma 2003; 55: 811–813.
Miller PR et al. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann Surg 2002; 236: 386–393.
Louw JA, Mafoyane NA, Small B, Neser CP . Occlusion of the vertebral artery in cervical spine dislocations. J Bone Joint Surg Br 1990; 72: 679–681.
Woodring JH, Lee C, Duncan V . Transverse process fractures of the cervical vertebrae: are they insignificant? J Trauma 1993; 34: 797–802.
Willis BK, Greiner F, Orrison WW, Benzel EC . The incidence of vertebral artery injury after midcervical spine fracture or subluxation. Neurosurgery 1994; 34: 435–441.
Chen CJ, Tseng YC, Lee TH, Hsu HL, See LC . Multisection CT angiography compared with catheter angiography in diagnosing vertebral artery dissection. AJNR Am J Neuroradiol 2004; 25: 769–774.
Clevert DA, Rupp N, Reiser M, Jung EM . Improved diagnosis of vascular dissection by ultrasound B-flow: a comparison with color-coded Doppler and power Doppler sonography. Eur Radiol 2005; 15: 342–347.
Bartels E, Flugel KA . Evaluation of extracranial vertebral artery dissection with duplex color-flow imaging. Stroke 1996; 27: 290–295.
de Bray JM, Penisson-Besnier I, Dubas F, Emile J . Extracranial and intracranial vertebrobasilar dissections: diagnosis and prognosis. J Neurol Neurosurg Psychiatry 1997; 63: 46–51.
Guidelines for the management of acute cervical spine and spinal cord injury (section on disorders of the spine and peripheral nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons): management of vertebral artery injuries after nonpenetrating cervical trauma. Neurosurgery 2002; 50: S173–S178.
Miller PR et al. Blunt cerebrovascular injuries: diagnosis and treatment. J Trauma 2001; 51: 279–285.
Acknowledgements
We acknowledge Dr C Santosh for his help with image selection and preparation.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
McCormick, M., Robinson, H., Bone, I. et al. Blunt cervical spine trauma as a cause of spinal cord injury and delayed cortical blindness. Spinal Cord 45, 687–689 (2007). https://doi.org/10.1038/sj.sc.3101995
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101995