Abstract
Data sources
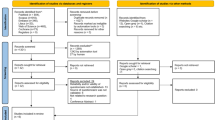
The search strategy focused on publications up to May 2015 in five electronic databases: PubMed, LILACS, Scopus, Web of Science and Science Direct. Furthermore, a partial grey literature search through Google Scholar and a hand-search of the references of the included studies were also performed.
Study selection
Those studies including patients with TMD associated with otologic signs and symptoms treated with conservative therapies, such as physiotherapy or cognitive behavioural therapy. These studies needed to describe whether the conservative treatments affected the associated otologic signs and symptoms. No language or time restrictions were applied.
Data extraction and synthesis
The search was completed in two stages. 1st stage: titles and abstracts were screened and included (or excluded) independently by two reviewers. 2nd stage: the same selection criteria were applied to the full text of the previously selected studies by the same reviewers. Disagreements were discussed, and a third author was involved, when required, to make a final decision. Study quality was assessed by the two reviewers using two risk of bias tools: ‘Quality Assessment of a Cohort Study’ and ‘Quality Assessment of a Randomised Clinical Trial’. Because of heterogeneity in the study designs only a narrative summary was presented.
Results
Eight studies were finally included in this review. Three of them were randomised clinical trials and five were cohort studies. All studies had an acceptable risk of bias, except one with high risk of bias. Seven of the eight studies showed total or partial resolution of otologic signs and/or symptoms after TMD therapy.
Conclusions
Insufficient evidence was identified to strongly support positive or negative changes in otologic signs and symptoms after conservative management therapies for TMD. Further studies with a higher level of evidence and more representative samples should be conducted to improve our understanding of the effect of TMD therapy on otologic complains.
Similar content being viewed by others
Commentary
The first description of temporo-mandibular disorders (TMD) was established by an ear, nose and throat specialist. He suggested a relationship between the temporomandibular joint (TMJ) and otologic problems.1 Hence, historically and due to its anatomical proximity, TMJ and ear pains have been associated.2 In addition, the proximity of the ear to the TMJ and muscles of mastication as well as their common trigeminal innervation frequently creates pain referral between these structures.3
Another common point is the fact that even if the prevalence of otologic symptoms in the general population may vary from 10% to 31%, it increases to 85% in patients with TMD.4 This is a significant increase even though we still cannot define precisely the pathophysiology of this portrayed association. It has been proposed that conservative therapies for TMD patients with otologic complaints may reduce secondary otalgia, ear fullness, earache and tinnitus.5
To investigate this SR a PICO question was established as:
-
Population: adults with TMD and related otologic complaints
-
Intervention: conservative TMD management therapies
-
Control: other forms of TMD management therapies or follow-up of an untreated sample.
-
Outcome: changes in otologic signs and symptoms.
This seems to be a well conducted systematic review. After applying the CEBM systematic-review appraisal tool6 it became clear that only one out of the six questions implied negative effects, but this conclusion was deemed questionable. Therefore, we can assume that this is a high quality systematic review. The questions that are part of this appraisal tool for systematic reviews are:
-
1
What question (PICO) did the systematic review address? Yes.
-
2
Is it unlikely that important, relevant studies were missed? Yes.
-
3
Were the criteria used to select articles for inclusion appropriate? Yes.
-
4
Were the included studies sufficiently valid for the type of question asked? No; ideally, randomised controlled trials are the gold standard to assess therapy.
-
5
Were the results similar from study to study? Yes.
-
6
How are the results presented? No meta-analysis was feasible.
On top of that, this systematic review followed PRISMA guidelines and was registered in PROSPERO.
A positive point is that a partial grey literature search and hand-search were performed. Another positive aspect is the incorporation of validated criteria for TMD diagnosis, RDC/TMD,7 as inclusion criteria. This likely reduced the chances of misdiagnosis.
Since using or not using a control group was not part of the inclusion criteria, the search results yielded three randomised controlled trials and five cohort studies. The gold standard to assess a therapeutic intervention is a randomised controlled trial. Nonetheless, this does not mean that other study designs cannot contribute to providing a certain amount of data to the bulk of evidence.
According to the authors of this systematic review, all the studies except one had an acceptable risk of bias. On top of that, seven out of the eight studies suggested an improvement in otologic signs and symptoms. Among these, it seems that tinnitus was the most mentioned. Nevertheless, the authors concluded that ‘insufficient evidence in favour or against the conservative therapies for TMD on changes in otologic signs and symptoms was identified’. This makes sense because even if the studies showed improvement in the otologic signs and symptoms, most of them are observational studies and one should not imply a relationship of cause-effect (TMD therapy-otalgic signs and symptoms relief) from them.
Practice points
-
Apparently, if we apply conservative therapies to patients with TMD and related otologic signs and symptoms, the otologic problems improve. Nevertheless, the level of evidence is not categorical enough to support conservative TMD management as an undisputable treatment option to manage otologic signs and symptoms. Having stated that, it is also unlikely that such conservative TMD management will worsen otologic signs and symptoms.
References
Costen JB . A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. 1934. Ann Otol Rhinol Laryngol 1997; 106:805–819.
Tuz HH, Onder EM, Kisnisci RS . Prevalence of otologic complaints in patients with temporomandibular disorder. Am JOrthod Dentofacial Orthop 2003; 123:620–623.
Okeson JP . Bell's Oral and Facial Pain. 7th ed. USA: Quintessence Pub Co; 2014:560pp.
Salvetti G, Manfredini D, Barsotti S, Bosco M . Otologic symptoms in temporomandibular disorders patients: is there evidence of an association-relationship? Minerva Stomatol 2006; 55:627–637.
Kuttila M, Le Bell Y, Savolainen-Niemi E, Kuttila S, Alanen P . Efficiency of occlusal appliance therapy in secondary otalgia and temporomandibular disorders. Acta Odontol Scand 2002; 60:248–254.
https://www.cebm.net/2014/06/critical-appraisal/ (accessed February 2018)
Schiffman EL, Ohrbach R, Truelove EL, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 2010; 24:63–78.
Author information
Authors and Affiliations
Additional information
Address for correspondence: André Luís Porporatti, Department of Prosthodontics, Bauru School of Dentistry, University of São Paulo, Al. Octávio Pinheiro Brizolla 9-75, CEP: 17012-901 Vila Universitária, Bauru, SP, Brazil. E-mail: andreporporatti@yahoo.com.br; andreporporatti@usp.br
Stechman-Neto J, Porporatti AL, Porto de Toledo I, Costa YM, Conti PC, De Luca. Canto G, Mezzomo LA. Effect of temporomandibular disorder therapy on otologic signs and symptoms: a systematic review. J Oral Rehabil 2016; 43: 468-479. doi: 10.1111/joor.12380. Epub 2016 Jan 8. Review. PubMed PMID: 26749516.
Rights and permissions
About this article
Cite this article
Morell, G. Insufficient evidence to support or reject effect of conservative TMD therapies on otologic signs and symptoms. Evid Based Dent 19, 26–27 (2018). https://doi.org/10.1038/sj.ebd.6401293
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401293
This article is cited by
-
Temporomandibular treatments are significantly efficient in improving otologic symptoms
BMC Oral Health (2023)