Abstract
To explore the parmacokinetics, safety and tolerability of paclitaxel after oral administration of SMEOF#3, a novel Self-Microemulsifying Oily Formulation, in combination with cyclosporin A (CsA) in patients with advanced cancer. Seven patients were enrolled and randomly assigned to receive oral paclitaxel (SMEOF#3) 160 mg+CsA 700 mg on day 1, followed by oral paclitaxel (Taxol®) 160 mg+CsA 700 mg on day 8 (group I) or vice versa (group II). Patients received paclitaxel (Taxol®) 160 mg as 3-h infusion on day 15. The median (range) area under the plasma concentration–time curve of paclitaxel was 2.06 (1.15–3.47) μg h ml−1 and 1.97 (0.58–3.22) μg h ml−1 after oral administration of SMEOF#3 and Taxol®, respectively, and 4.69 (3.90–6.09) μg h ml−1 after intravenous Taxol®. Oral SMEOF#3 resulted in a lower median Tmax of 2.0 (0.5–2.0) h than orally applied Taxol® (Tmax=4.0 (0.8–6.1) h, P=0.02). The median apparent bioavailability of paclitaxel was 40 (19–83)% and 55 (9–70)% for the oral SMEOF#3 and oral Taxol® formulation, respectively. Oral paclitaxel administered as SMEOF#3 or Taxol® was safe and well tolerated by the patients. Remarkably, the SMEOF#3 formulation resulted in a significantly lower Tmax than orally applied Taxol®, probably due to the excipients in the SMEOF#3 formulation resulting in a higher absorption rate of paclitaxel.
Similar content being viewed by others
Main
Currently, paclitaxel is only marketed as an intravenous (i.v.) formulation. Paclitaxel is poorly soluble in most pharmaceutical solvents, therefore, in the marketed i.v. formulation it is formulated in a 1:1 combination of the solubilising agent polyoxyethylated caster oil (Cremophor® EL (CrEL)) and dehydrated ethanol. CrEL has been reported to be responsible for severe hypersensitivity reactions (Webster et al, 1997) and the nonlinear pharmacokinetic behaviour of i.v. administered paclitaxel (Sparreboom et al, 1996; van Tellingen et al, 1999; van Zuylen et al, 2001a).
Oral administration of paclitaxel might be attractive because it is more convenient for patients than i.v. administration. Furthermore, oral paclitaxel administration may enable the development of treatment regimens resulting in plasma concentrations above a pharmacologically relevant level for more prolonged periods of time. However, oral treatment with paclitaxel is severely hampered because of its low bioavailability, which is caused by two main reasons. Firstly, paclitaxel is a high-affinity substrate for the efflux multidrug transporter P-glycoprotein (P-gp), which is highly expressed in the gastrointestinal tract (Sparreboom et al, 1997). Secondly, paclitaxel undergoes first-pass metabolism by the gut and liver cytochrome P450 (CYP) enzymes (CYP 2C8 and CYP 3A4).
Previous studies carried out at our Institute investigated the pharmacokinetics of the i.v. paclitaxel formulation after oral administration as a drinking solution diluted with water (Meerum Terwogt et al, 1999; Malingré et al, 2000a, 2000b; Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e) and revealed that coadministration of oral CsA resulted in an increased systemic exposure to oral paclitaxel (van Asperen et al, 1998; Meerum Terwogt et al, 1999). As CsA is an inhibitor of both P-gp and CYP3A4, both an increased absorption and a reduced first-pass effect may be responsible for the increased systemic exposure. We have shown previously that systemic exposure to paclitaxel did not increase with CsA doses higher than 10 mg kg−1 (Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e).
Although CrEL was reported to exhibit no oral absorption (Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e) it affects paclitaxel pharmacokinetics by limiting the absorption of paclitaxel from the intestine after oral administration, probably by entrapment of paclitaxel in micelles, thereby reducing the availability of paclitaxel for uptake (Sparreboom et al, 1996; Sparreboom et al, 1999; Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e; van Zuylen et al, 2001b; Bardelmeijer et al, 2002). Thus far, a favourable oral formulation with paclitaxel has not been found yet.
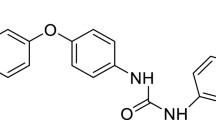
Self-Microemulsifying Oily Formulation (SMEOF)#3 is a novel oral SMEOF of paclitaxel. The formulation consists of an isotropic mixture of oils and surfactants, which solubilise paclitaxel and spontaneously forms a microemulsion upon contact with water. Previous in vivo studies in wild-type mice and mdr1a/b (−/−) knockout mice, which lack functional P-gp activity, showed that SMEOF#3 was a suitable delivery vehicle for oral administration of paclitaxel in combination with oral CsA (data on file). The choice of the excipients was motivated by a previous study exploring particle size, physical and chemical stability as well as cytotoxic activity in vitro of different formulations of paclitaxel (Gursoy et al, 2003). Furthermore, the physical stability was assessed of emulsions of different SMEOFs of paclitaxel after dilution in simulated gastric fluid (SGF). It was shown that after dilution of the i.v. paclitaxel (Taxol®) formulation in SGF, major part of the micelles was destabilised and a massive precipitation immediately occurred (data on file). This phenomenon was thought to be due to diffusion of ethanol in the SGF after which the remaining CrEL was not capable to maintain all paclitaxel in solution. SMEOF#3, however, showed a good stability for about 6 h after dilution in SGF. In SMEOF#3, tyloxapol and TPGS (d-alpha-tocopheryl polyethylene glycol 1000 succinate) have been selected for their ability to solubilise paclitaxel. Tyloxapol is a nonionic surfactant used in the product Exosurf® (GlaxoSmithKline, UK). Upon contact with water, tyloxapol was shown to form lyotropic liquid crystals, which are are thought to contribute to the formation of microemulsions (Gershanik and Benita, 2000). Furthermore, it was shown that tyloxapol can be used as a cosolvent by increasing the solubility of paclitaxel in ethanol (Gursoy et al, 2003). TPGS is a derivative of vitamin E with amphiphillic properties and it is used as excipient in Agenerase® (amprenavir, GlaxoSmithKline, UK). TPGS has been shown to increase the bioavailability of poorly absorbed lipophilic drugs (Chang et al, 1996), probably by its solubilising effect through improved micelle formation (Boudreaux et al, 1993). As compared to the commercial paclitaxel (Taxol®) formulation tested orally, the main advantages of SMEOF#3 are the absence of CrEL and the significantly lower ethanol/paclitaxel ratio, which allows reducing the amount of ethanol to be administered.
The purpose of this study was to investigate the pharmacokinetics, safety and tolerability of this novel oral formulation of paclitaxel (SMEOF#3).
Patients and methods
Patient population
Patients with a histological or cytological diagnosis of advanced nonhaematological cancer for whom no curative therapy existed and for whom treatment with single agent paclitaxel was considered of potential benefit were eligible for the study. Patients had to be recovered from any toxicities of prior treatment. Previous chemotherapy was allowed as long as the last treatment was at least 4 weeks prior to study entry and at least 3 weeks should have elapsed since receiving radiotherapy.
Patients had to have acceptable haematological parameters (white blood cells (WBC) ⩾3.0 × 109 l−1, and platelets ⩾100 × 109 l−1)), hepatic function (serum bilirubin ⩽20 μmol l−1; AST and ALT⩽1.5 × upper limit of normal (ULN) or ⩽3 × ULN in case of liver metastases) and renal function (serum creatinine ⩽160 μmol l−1 or creatinine clearance ⩾50 ml min−1 as calculated by Cockcroft Gault formula), and a World Health Organization (WHO) performance status (PS) ⩽2. Patients were excluded if they had experienced severe toxicities on prior taxane treatment, suffered from uncontrolled infectious disease, heart disease, bowel obstruction or motility disorders that could have influenced the resorption of drugs. Further exclusion criteria were concomitant use of known P-gp and CYP 3A modulating drugs and chronic use of H2-receptor antagonists or proton pump inhibitors. Female patients were excluded when breast-feeding or pregnant (confirmed by a pregnancy test before study entry). Patients had to be willing and able to follow the protocol requirements. The Medical Ethics Committee of the Institute approved the study protocol and all patients gave written informed consent.
Study design
Initially six patients were planned to be enrolled in the study and were randomly assigned to two groups of treatment. Group I received a combination of oral paclitaxel (SMEOF#3) 160 mg and CsA 700 mg on day 1, followed by oral paclitaxel (Taxol®) 160 mg in combination with CsA 700 mg on day 8, and group II received oral paclitaxel (Taxol®) 160 mg in combination with CsA 700 mg on day 1, followed by oral paclitaxel (SMEOF#3) 160 mg and CsA 700 mg on day 8. CsA was administered orally at a fixed dose of 700 mg (approximately equivalent to 10 mg kg−1 CsA) 30 min prior to oral administration of paclitaxel. The patients in both groups received a single i.v. administration of paclitaxel (Taxol®) 160 mg as a 3-h infusion on day 15.
Drug composition and administration
The composition of SMEOF#3 (Novagali Pharma SA, Evry cedex, France) is presented in Table 1. SMEOF#3 (160 mg in 10 ml) was administered orally to the patients via a syringe within 30 min after 1:3 dilution with tap water to 40 ml resulting in a final paclitaxel concentration of 4 mg ml−1. The commercially available i.v. paclitaxel (Taxol®) formulation (Bristol-Myers Squibb, Syracuse, NY, USA) containing paclitaxel 6 mg ml−1, ethanol 396 mg ml−1, and CrEL 527 mg ml−1 was administered orally after dilution of 26.7 ml (160 mg) with water to 40 ml (4 mg ml−1). The i.v. paclitaxel (Taxol®) formulation was administered i.v. at a fixed dose of 160 mg as 3-h infusion to all patients on day 15. CsA was administered as seven capsules of 100 mg each (Neoral®, Novartis, Basel, Switzerland).
To prevent possible nausea and vomiting during both the treatment with oral SMEOF#3 and oral Taxol®, patients were premedicated with oral granisetron (Kytril®) 1 mg approximately 2 h before the intake of paclitaxel. In addition, patients received a light standard breakfast (two crackers and a cup of tea) at least 2 h prior to each paclitaxel administration. Intake of food was not allowed until 2 h following the intake of oral paclitaxel. Patients were premedicated with dexamethasone 20 mg p.o. 8–10 h prior to, and ranitidine 50 mg i.v., clemastine 2 mg i.v. and dexamethasone 20 mg i.v., 30–60 min before i.v. paclitaxel dosing, to prevent infusion-related hypersensitivity reactions. If considered in their best interest, patients continued on a 3-weekly schedule of i.v. paclitaxel at a dose of 175 mg m−2.
Sample collection and analysis
Blood samples for pharmacokinetic analysis of paclitaxel were collected via an indwelling catheter in 5 ml heparinised tubes after both p.o. and i.v. administration. Following oral administration samples were obtained prior to administration, immediately after administration, and 15, 30, 45 min, and 1, 2, 4, 6, 8, 24, 48, and 72 h after paclitaxel administration. Following i.v. administration samples were obtained prior to administration, 60, 120, and 165 min after start of infusion, at the end of infusion, and 15, 30, 45 min, and 1, 2, 4, 6, 8, 24, 48, and 72 h after infusion. Blood samples were centrifuged, and plasma was separated and immediately transferred into polypropylene tubes and stored at −20°C until analysis. Paclitaxel concentrations in plasma were determined using a validated high performance liquid chromatographic (HPLC) tandem mass spectrometric (MS/MS) method (Vainchtein et al, 2006).
For the pharmacokinetic analysis of CsA, blood samples were collected in 5 ml EDTA tubes at the same time points as for paclitaxel after the oral SMEOF#3 and oral Taxol® administrations. Whole blood samples were stored at 4°C until analysis using a specific fluorescence polarisation immunoassay (FPIA) (Malingré, 2001).
Urine samples were collected prior to paclitaxel administration and at the intervals: 0–24, 24–48, and 48–72 h after oral SMEOF#3 and oral Taxol® and after i.v. Taxol® administration. A volume of 19 ml of each urine sample was mixed with 1 ml of a mixture of 5% CrEL (Sigma, Prague, Czech Republic) – ethanol (Merck, Darmstadt, Germany) 1:1 v v−1 to prevent paclitaxel precipitation. Subsequently, 5 ml was transferred into a 10 ml polypropylene tube and stored at −20°C until analysis. Paclitaxel concentrations in urine were determined using a validated HPLC method with ultraviolet (UV) detection (Huizing et al, 1995).
Pharmacokinetics
The pharmacokinetic parameters of paclitaxel and CsA were determined by noncompartmental analysis, using WinNonLin™ (version 5.0, Pharsight Corporation, Mountain View, CA, USA). The area under the plasma concentration time curve (AUC) was determined using the linear logarithmic trapezoidal method up to the last measured concentration-time point and extrapolated to infinity (AUC0−∞) using the slope of the terminal part of the logarithmic concentration vs time curve (λz). Furthermore, the terminal half-life (t1/2) was determined. The maximal observed drug concentration (Cmax) and time to maximal observed drug concentration (Tmax) were obtained directly from the experimental data.
The apparent bioavailability (F) of paclitaxel was calculated by the ratio of the AUC0−∞ after oral administration and AUC0−∞ after i.v. administration of paclitaxel. Furthermore, the fraction of the paclitaxel dose that was excreted unchanged in urine was calculated.
Statistics
The software package Statistical Product and Service Solutions (version 12.1. 1 for Windows, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The priori level of significance was P=0.05. The paired t-test was applied on logarithmic-transformed values to make a comparison between the pharmacokinetic parameters of paclitaxel after the different study treatments.
Safety
All toxicities observed were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 3.0, 2003 (http://ctep.cancer.gov/forms/CTCAEv3.pdf).
Results
Patient characteristics
As one patient was not fully evaluable for pharmacokinetic analysis, one additional patient was included and in total seven patients were entered into the study. Patient characteristics are specified in Table 2. Patients 1, 4, 5, and 7 were assigned to group I and patients 2, 3, and 6 were assigned to group II. Four patients and three patients had a PS of 1 and 2, respectively. Age, height, and weight appeared to be equally distributed over the two treatment groups.
Drug administration and extent of exposure
All patients received all three treatments (day 1, 8, and 15) at the single flat dose of 160 mg per formulation. The i.v. administration of Taxol® during day 15 was temporally interrupted in patient 1 due to infusion leakage. Patient 4, a 54 years old female, developed rash and dyspnoea 15 min following i.v. paclitaxel administration. The paclitaxel infusion was terminated and 2 mg clemastine i.v. was given, which resolved the hypersensitivity reaction. Therefore, blood sampling for pharmacokinetics could not be performed and this patient was not fully eligible. Intravenous paclitaxel administration was restarted after one hour at a lower infusion rate, which did not cause any adverse reactions.
Pharmacokinetic and statistical analysis
Figure 1 depicts the plasma pharmacokinetic profiles of paclitaxel after treatment with p.o. paclitaxel (SMEOF#3), p.o. paclitaxel (Taxol®) (n=7), and i.v. paclitaxel (Taxol®) 160 mg as 3 h infusion (n=6). Interpatient variability in paclitaxel plasma concentrations was comparable between p.o. SMEOF#3 and p.o. Taxol®, both coadministered with CsA, but was lower after i.v. administered Taxol®.
Figure 2 presents the AUC0−∞ (μg h ml−1), Cmax (μg ml−1), and Tmax (h) of paclitaxel after p.o. SMEOF#3, p.o. Taxol® and after i.v. Taxol® given as 3 h infusion. Tmax after oral SMEOF#3 was substantially lower compared to p.o. paclitaxel (Taxol®) (P=0.021).
The plasma pharmacokinetic parameters of paclitaxel after the three study treatments are depicted in Table 3. The median (range) AUC0−∞ of the SMEOF#3 formulation was 2.06 (1.15–3.47) μg h ml−1, which was not significantly higher than the AUC0−∞ of 1.97 (0.58–3.22) μg h ml−1 after oral Taxol® (P=0.74). The interpatient variability in AUC0−∞ was relatively high after both p.o. SMEOF#3 (%CV=42) and p.o. Taxol® (%CV=45). Furthermore, oral SMEOF#3 resulted in a not significantly higher median Cmax of 0.21 (0.15–0.35) μg ml−1 compared to a Cmax of 0.16 (0.10–0.29) μg ml−1 after oral Taxol® (P=0.15). Remarkably, oral SMEOF#3 showed a significantly lower Tmax of 2.0 (0.5–2.0) h than p.o. Taxol®, which had a Tmax of 4.0 (0.8–6.1) h (P=0.021). The median apparent bioavailability was 40% (19–83%) and 55% (9–70%) for the oral SMEOF#3 and oral Taxol® formulation, respectively. After both i.v. and oral administration excretion of paclitaxel in the urine was low and more than 70% of the total urinary excretion occurred within 24 h.
Figure 3 depicts the mean pharmacokinetic profiles of CsA after oral administration of CsA 700 mg in combination with p.o. SMEOF3# 160 mg and p.o. Taxol® 160 mg (n=7). The pharmacokinetic parameters of CsA of all three study treatments are summarised in Table 4.
Figure 3 and Table 4 clearly show that CsA pharmacokinetics were not influenced by coadministration of either paclitaxel formulations.
Safety evaluation
Nonhaematological toxicities were CTCAE grade 1–2, except for two grade 3 events: one hypersensitivity reaction in patient 4 after i.v. paclitaxel administration, and muscular weakness in patient 1, that was considered to be probably related to SMEOF#3. No life threatening adverse events (grade 4) and deaths (grade 5) were reported in the study. Overall, the most frequently reported drug-related adverse events were gastrointestinal disorders with the most common symptoms of nausea occurring in three patients after oral administration of paclitaxel. Furthermore, abdominal pain, diarrhoea, and stomatitis were reported in two patients. No clinical relevant haematological toxicities occurred after the three treatments. Furthermore, no abnormal blood chemistry values were reported.
Discussion
In the present clinical study, we tested the pharmacokinetics, safety and tolerability of SMEOF#3, a new micro-emulsifying formulation for oral administration of paclitaxel in combination with CsA.
The apparent bioavailability of paclitaxel after oral administration of SMEOF#3 coadministered with CsA was estimated at 40% (19–83%) and was comparable to the apparent bioavailability of orally administered Taxol®. These data were in line with studies that showed that the apparent bioavailability of orally administered Taxol® in combination with CsA was approximately 47% (Huizing et al, 1997; Meerum Terwogt et al, 1999).
The term bioavailability, however, should be interpreted with caution due to the nonlinear pharmacokinetics of i.v. paclitaxel caused by the presence of CrEL (van Tellingen et al, 1999). Entrapment of paclitaxel in CrEL micelles in the central compartment causes a more than proportional increase in plasma paclitaxel concentrations with increasing doses. Studies in mice showed that these higher total drug levels in plasma did not result in higher drug levels in tissues (Sparreboom et al, 1996). Previous studies showed that CrEL is not absorbed after oral administration. This pseudo-nonlinearity of i.v. paclitaxel has two important implications for the pharmacology of oral paclitaxel. Firstly, the oral bioavailability of paclitaxel, calculated by comparing the AUC values after oral and i.v. administration, will be underestimated as the affinity of paclitaxel for the plasma compartment is increased after i.v. administration due to the presence of CrEL in the central circulation. Secondly, the pseudo-nonlinearity of i.v. paclitaxel implies that after oral administration, when CrEL is not present, plasma levels of paclitaxel represent a higher fraction of free drug, which will result in enhancement of the availability of paclitaxel for the (tumour) tissues (van Tellingen et al, 1999). Consequently, threshold values for the paclitaxel concentration established for i.v. paclitaxel (Gianni et al, 1995; Huizing et al, 1997) cannot be used for oral administration of paclitaxel.
The pharmacokinetic parameters of CsA after coadministration with oral SMEOF#3 and orally administered Taxol® were comparable. Furthermore, pharmacokinetic parameters of CsA were in line with those obtained before (Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e). It has been demonstrated that 10 mg kg−1 CsA was sufficient for maximal enhancement of paclitaxel bioavailability (Malingré et al, 2001a, 2001b, 2001c, 2001d, 2001e). In combination, these facts suggest that a dose of 700 mg CsA as used in this study was sufficient.
Remarkably, the Tmax of paclitaxel after oral administration of the SMEOF#3 formulation was lower compared to oral Taxol®. It was previously described by us that CrEL limits the absorption rate of paclitaxel due to encapsulation in CrEL micelles. As the concentration of CrEL in the gastrointestinal tract decreases with time due to distribution, breakdown and elimination of CrEL, more unbound paclitaxel becomes available for absorption in the systemic circulation with time and consequently the absorption rate increases (de Jonge et al, 2005). The lower Tmax after oral SMEOF#3 is probably due to the ability of the SMEOF#3 formulation to remain stable in the gastrointestinal tract avoiding precipitation of paclitaxel leading to a major fraction of paclitaxel in solution, which is available for absorption. However, in the case of oral paclitaxel administered as Taxol®, probably a significant amount of paclitaxel precipitates due to quick diffusion and resorption of ethanol and the precipitated fraction of paclitaxel is slowly re-dissolved in the gastrointestinal fluids before being absorbed. Furthermore, a lower amount of ethanol was administered after SMEOF#3 160 mg compared to the orally applied i.v. paclitaxel (Taxol®) formulation 160 mg; the amount of administered ethanol was approximately 3.3 g and 10.6 g after SMEOF#3 and the orally applied i.v. paclitaxel (Taxol®) formulation, respectively.
An extensive pharmacokinetic analysis demonstrated an increase in the systemic exposure to paclitaxel and a prolonged time of a paclitaxel concentration above a pharmacological relevant level with increasing doses of SMEOF#3 (data not shown).
In summary, we demonstrated that the novel SMEOF#3 formulation was well tolerated after oral administration at the given dose of 160 mg when coadministered with CsA, without induction of relevant gastrointestinal or haematological toxicity. Regarding the nearly uneventful oral administration of the 160 mg dose together with the relatively low AUC0−∞ after CsA coadministration, we suggest that new studies should be initiated with this novel SMEOF#3 formulation to explore once daily administration of paclitaxel at higher dose levels in order to increase systemic exposure and to prolong exposure at therapeutic levels.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bardelmeijer HA, Ouwehand M, Malingré MM, Schellens JHM, Beijnen JH, van Tellingen O (2002) Entrapment by Cremophor EL decreases the absorption of paclitaxel from the gut. Cancer Chemother Pharmacol 49: 119–125
Boudreaux JP, Hayes DH, Mizrahi S, Maggiore P, Blazek J, Dick D (1993) Use of water-soluble liquid vitamin E to enhance cyclosporine absorption in children after liver transplant. Transplant Proc 25: 1875
Chang T, Benet LZ, Hebert MF (1996) The effect of water-soluble vitamin E on cyclosporine pharmacokinetics in healthy volunteers. Clin Pharmacol Ther 59: 297–303
de Jonge ME, Huitema ADR, Schellens JHM, Rodenhuis S, Beijnen JH (2005) Population pharmacokinetics of orally administered paclitaxel formulated in Cremophor EL. Br J Clin Pharmacol 59: 325–334
Gershanik T, Benita S (2000) Self-dispersing lipid formulations for improving oral absorption of lipophilic drugs. Eur J Pharm Biopharm 50: 179–188
Gianni L, Kearns CM, Giani A, Capri G, Vigano L, Lacatelli A, Bonadonna G, Egorin MJ (1995) Nonlinear pharmacokinetics and metabolism of paclitaxel and its pharmacokinetic/pharmacodynamic relationships in humans. J Clin Oncol 13: 180–190
Gursoy N, Garrigue JS, Razafindratsita A, Lambert G, Benita S (2003) Excipient effects on in vitro cytotoxicity of a novel paclitaxel self-emulsifying drug delivery system. J Pharm Sci 92: 2411–2418
Huizing MT, Giaccone G, van Warmerdam LJ, Rosing H, Bakker PJ, Vermorken JB, Postmus PE, van Zandwijk N, Koolen MG, ten Bokkel Huinink WW, van der Vijgh WJ, Bierhorst FJ, Lai A, Dalesio O, Pinedo HM, Veenhof CH, Beijnen JH (1997) Pharmacokinetics of paclitaxel and carboplatin in a dose-escalating and dose-sequencing study in patients with non-small-cell lung cancer. The European Cancer Centre. J Clin Oncol 15: 317–329
Huizing MT, Rosing H, Koopman F, Keung AC, Pinedo HM, Beijnen JH (1995) High-performance liquid chromatographic procedures for the quantitative determination of paclitaxel (Taxol) in human urine. J Chromatogr B Biomed Appl 664: 373–382
Malingré MM (2001) Performance of the analytical assays of paclitaxel, docetaxel and cyclosporin in a routine hospital laboratory setting. J Liq Chrom Rel Technol 24: 2697–2717
Malingré MM, Beijnen JH, Rosing H, Koopman FJ, van Tellingen O, Duchin K, ten Bokkel Huinink WW, Swart M, Lieverst J, Schellens JHM (2001a) A phase I and pharmacokinetic study of bi-daily dosing of oral paclitaxel in combination with cyclosporin A. Cancer Chemother Pharmacol 47: 347–354
Malingré MM, Beijnen JH, Rosing H, Koopman FJ, van Tellingen O, Duchin K, ten Bokkel Huinink WW, Swart M, Lieverst J, Schellens JHM (2001b) The effect of different doses of cyclosporin A on the systemic exposure of orally administered paclitaxel. Anticancer Drugs 12: 351–358
Malingré MM, Beijnen JH, Schellens JHM (2001c) Oral delivery of taxanes. Invest New Drugs 19: 155–162
Malingré MM, Meerum Terwogt JM, Beijnen JH, Rosing H, Koopman FJ, van Tellingen O, Duchin K, ten Bokkel Huinink WW, Swart M, Lieverst J, Schellens JHM (2000b) Phase I and pharmacokinetic study of oral paclitaxel. J Clin Oncol 18: 2468–2475
Malingré MM, Schellens JHM, van Tellingen O, Ouwehand M, Bardelmeijer HA, Rosing H, Koopman FJ, Schot ME, ten Bokkel Huinink WW, Beijnen JH (2001d) The co-solvent Cremophor EL limits absorption of orally administered paclitaxel in cancer patients. Br J Cancer 85: 1472–1477
Malingré MM, Schellens JHM, van Tellingen O, Rosing H, Koopman FJ, Duchin K, ten Bokkel Huinink WW, Swart M, Beijnen JH (2000a) Metabolism and excretion of paclitaxel after oral administration in combination with cyclosporin A and after i.v. administration. Anticancer Drugs 11: 813–820
Malingré MM, ten Bokkel Huinink WW, Duchin K, Schellens JHM, Beijnen JH (2001e) Pharmacokinetics of oral cyclosporin A when co-administered to enhance the oral absorption of paclitaxel. Anticancer Drugs 12: 591–593
Meerum Terwogt JM, Malingré MM, Beijnen JH, ten Bokkel Huinink WW, Rosing H, Koopman FJ, van Tellingen O, Swart M, Schellens JHM (1999) Coadministration of oral cyclosporin A enables oral therapy with paclitaxel. Clin Cancer Res 5: 3379–3384
Sparreboom A, van Asperen J, Mayer U, Schinkel AH, Smit JW, Meijer DK, Borst P, Nooijen WJ, Beijnen JH, van Tellingen O (1997) Limited oral bioavailability and active epithelial excretion of paclitaxel (Taxol) caused by P-glycoprotein in the intestine. Proc Natl Acad Sci USA 94: 2031–2035
Sparreboom A, van Tellingen O, Nooijen WJ, Beijnen JH (1996) Nonlinear pharmacokinetics of paclitaxel in mice results from the pharmaceutical vehicle Cremophor EL. Cancer Res 56: 2112–2115
Sparreboom A, van Zuylen L, Brouwer E, Loos WJ, de Bruijn P, Gelderblom H, Pillay M, Nooter K, Stoter G, Verweij J (1999) Cremophor EL-mediated alteration of paclitaxel distribution in human blood: clinical pharmacokinetic implications. Cancer Res 59: 1454–1457
Vainchtein LD, Thijssen B, Stokvis E, Rosing H, Schellens JHM, Beijnen JH (2006) A simple and sensitive assay for the quantitative analysis of paclitaxel and metabolites in human plasma using liquid chromatography/tandem mass spectrometry. Biomed Chromatogr 20: 139–148
van Asperen J, van Tellingen O, van der Valk MA, Rozenhart M, Beijnen JH (1998) Enhanced oral absorption and decreased elimination of paclitaxel in mice cotreated with cyclosporin A. Clin Cancer Res 4: 2293–2297
van Tellingen O, Huizing MT, Panday VR, Schellens JHM, Nooijen WJ, Beijnen JH (1999) Cremophor EL causes (pseudo-) non-linear pharmacokinetics of paclitaxel in patients. Br J Cancer 81: 330–335
van Zuylen L, Karlsson MO, Verweij J, Brouwer E, de Bruijn P, Nooter K, Stoter G, Sparreboom A (2001a) Pharmacokinetic modeling of paclitaxel encapsulation in Cremophor EL micelles. Cancer Chemother Pharmacol 47: 309–318
van Zuylen L, Verweij J, Sparreboom A (2001b) Role of formulation vehicles in taxane pharmacology. Invest New Drugs 19: 125–141
Webster LK, Linsenmeyer ME, Rischin D, Urch ME, Woodcock DM, Millward MJ (1997) Plasma concentrations of polysorbate 80 measured in patients following administration of docetaxel or etoposide. Cancer Chemother Pharmacol 39: 557–560
Acknowledgements
We thank Ms Ciska Koopman for her analytical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Veltkamp, S., Thijssen, B., Garrigue, J. et al. A novel self-microemulsifying formulation of paclitaxel for oral administration to patients with advanced cancer. Br J Cancer 95, 729–734 (2006). https://doi.org/10.1038/sj.bjc.6603312
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603312