Key Points
-
Provides an overview of the philosophy and the management of the Radboud Tooth Wear Project from monitoring and counselling to a full rehabilitation.
-
Emphasises the need of counselling and monitoring to objectively evaluate the progression of tooth wear over time and determine the patients' commitment for a possible restorative rehabilitation.
-
Illustrates several minimally invasive and adhesive restorative strategies for the treatment of severe tooth wear patients.
Abstract
This paper explains a conservative, pragmatic and minimally invasive intervention concept for the treatment of severe tooth wear patients based on the Radboud Tooth Wear Project in the Netherlands. Guidelines and flowcharts for management of severe tooth wear patients and rehabilitation in increased vertical dimension of occlusion are presented. We concluded that: (a) Restorative treatment is not always indicated, even for patients with severe tooth wear. (b) If the patient has no complaints, counselling and monitoring is probably the best option. (c) Minimally invasive and adhesive restorative strategies are preferred when severe tooth wear patients are to be treated in increased vertical dimension, especially when young patients are involved. (d) Clinical evidence for a suitable restorative treatment protocol is limited to five-year follow up for direct composites. This material seems to be suitable for rehabilitation in increased vertical dimension on the middle long term. Clinical results for indirect techniques are not available yet. (e) Restorations, including those that are considered 'definitive' may prove to have a limited lifetime in patients with severe tooth wear due to bruxism and erosion. Explanation of the possible treatment options and expected complications should be included in the informed consent.
Similar content being viewed by others
Introduction
Especially among younger generations, more people are tending to keep their teeth for life, resulting in teeth having to function for 80 years and more. As a result, tooth wear may pose new challenges to the dental profession1 as it seems to become more and more common and is considered increasingly as a concern in oral health, especially among younger people.2,3,4 However, while prevalence of erosive tooth wear of permanent teeth in children and adolescents is reported to be 30%5,6 the consequences, and especially severe wear, for maintaining a dentition during lifetime is not yet clear. Therefore, in 2012 the 'Radboud Tooth Wear Project' was started at the dental school of the Radboud University Medical Center in Nijmegen, the Netherlands, aiming to answer several questions:
-
Is tooth wear a continuous or episodic process?
-
Is the stage of wear a predictor for future wear and related to quality of oral health problems?
-
Which aetiological factors are responsible for those cases of tooth wear that are threading for a lifelong maintenance of quality of oral health?
-
If tooth wear needs restorative intervention, which restorative strategies are optimal for these patients.
In this paper we will address these questions and explain the Radboud philosophy on the management of severe tooth wear from monitoring and counselling to a full rehabilitation based on principles of 'conservative, pragmatic and minimally invasive interventions'.
Guideline for the management of severe tooth wear
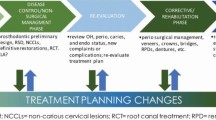
To help the general practitioner in the decision-making process on the management of severe wear cases, a decision flow chart was developed in a recent European Consensus Meeting (Fig. 1).7 The aim of this flowchart might help the clinician to make the appropriate decision and give treatment advice, from counselling and monitoring towards restorative treatment.
Diagnosis of severe tooth wear
Tooth wear is often mentioned as 'erosion', indicating that it is the main responsible factor. A more suitable term would be 'erosive tooth wear' or just 'tooth wear', meaning that also mechanical factors like attrition and abrasion are important aetiological factors contributing to tooth wear. Especially in cases of severe and pathological wear the aetiology will be multifactorial in most cases.8 For diagnosis, one has to realise that tooth wear is a physiological process, while caries is a pathological process in itself. As a result, a diversity of tooth wear stages may be observed in patients that can be considered as expressions of physiological wear. In individual cases, also among younger patients, tooth wear may become severe or pathological. 'Severe tooth wear' is defined as 'tooth wear with substantial loss of tooth structure, with dentin exposure and significant loss (≥1/3) of the clinical crown'.7 However, this does not imply that all cases of severe wear can be considered as pathological, especially among the highly aged where severe wear can be considered as normal in many cases. Meanwhile, pathological tooth wear is defined as 'tooth wear which is atypical to the age of the patient, causing pain or discomfort, functional problems, or deteriorations in aesthetic appearance, which, if progressing, may give rise to undesirable complications of increasing complexity'.7 As a consequence, painful occlusal cusps with exposed dentin due to active erosive wear among adolescents can be considered as pathological while such a state of wear is not severe per se. The diversity of stages of wear related to the age of the patient should always play a role in diagnosis.
Counselling and monitoring: the first option
If the amount of wear is physiological (typical for the age of the patient), no treatment will be needed. In cases where the wear is pathological, further diagnostics are needed to determine the best management of the tooth wear. Even if wear can be defined as pathological or severe, people may be functioning with their worn dentition to their satisfaction for years. The advice to start an, often complex, rehabilitation in patients that have no functional problems and have not made a request for help is high risk.Especially in these patients, who have shown to destruct their own dentition in the past, defects at restorations as wear and fractures are likely to occur. Moreover, compliance for a long, complex and expensive treatment will be limited among patients that have no demand for help. Therefore, a non-restorative intervention with counselling and monitoring is advised for patients with severe or pathological wear, but who have not requested treatment. 'Counselling' includes giving information to the patient about their tooth wear and establishes an individual preventive programme, whereas 'monitoring' includes the objective measurement of the amount of wear and its progression over time. Counselling starts with identifying risk factors; this being the basis for the assessment of preventive measurements that should be discussed with the patient, such as prescribing a night guard in case of bruxism, giving dietary advice, discussing drinking and eating habits, or referring the patient to a gastroenterologist in case of suspicion of gastro-oesophageal reflux disease (GORD). Dietary advice includes reducing the amount and frequency of intake of acidic drinks, changing drinking habits (such as 'swishing' or 'sipping') and advising safer food alternatives, such as calcium-enriched (sports) drinks and foods, or water and milk.3 However, there is limited evidence for the efficacy of intra oral splints (night guards) to reduce wear in case of bruxism or for changing diets for patients that suffer from erosion.9
Additionally, it is possible to use specific protective products or materials, such as toothpastes or mouth rinses containing stannous fluoride or stannous chloride which have the potential for slowing the progression of erosive tooth wear.10
Moreover, little evidence is available on the reduction of tooth wear when using proton pomp inhibitors (PPI) over a longer period of time.11 As severe tooth wear patients often suffer from multifactorial aetiological factors, preventive measurements can be increasingly complex as gastric acid may have a worsening effect when retained inside a night guard during the night. Therefore, in severe tooth wear cases, the prognosis of the treatment and effect of specific preventive measurements is often difficult to determine as diagnoses are often 'best guesses' and evidence for preventive measurements is still scarce or absent.
Monitoring has the aim to objectively determine the amount of tooth wear and evaluate the progression of wear over time. The severity of tooth wear can be determined by using an index score using, for example, Tooth Wear Index (TWI), Basic Erosive Wear Examination (BEWE), or the Tooth Wear Evaluation System (TWES).12,13,14 Together with the shared decision-making outcomes and the actions taken, it has to be added to the clinical records of the patient, otherwise, the general practitioner may be accused of supervised neglect. Monitoring can be performed by using a series of 'traditional' casts or digital 3D datasets/scans of teeth obtained over a period of several months or years. These casts or digital 3D datasets are also a valuable aid to elucidate the aetiology of the process and explain the nature and severity of the condition to the patients.7 When satisfied that wear is not progressive on a pathological level and that no functional or aesthetical problems are present, new registrations can be made at intervals of approximately three years. It is remarkable that even in younger patients with advanced stages of (pathological) tooth wear, often no progression of wear is found between those intervals. In Figure 2 a female patient (33 years old) is presented with moderate to severe tooth wear. As there were no aesthetical or functional problems, the patient consented to a counselling and monitoring programme. Over a period of 3.5 years no pathological wear was observed and it was decided to continue monitoring and recall at another three years (Fig. 2). In another case, a 50-year-old female patient presented with severe tooth wear at intake. No functional problems were present and the main aetiological factors could not be determined, although likely related to erosion. The patient consented to monitoring as the first treatment strategy. After a period of 1.5 years wear had progressed pathologically, and still no reason for the progression could be assessed, such as symptoms of reflux (for example, GORD) or abnormal dietary or drinking habits. Moreover, external staining was present due to smoking, which is not in accordance with progressive erosion. Despite the progressive wear, still no commitment was present for a restorative rehabilitation and it was decided to shorten the monitoring interval to one year (Fig. 3). These remarkable interindividual differences were also found in the study of Rodriguez et al.,15 in which 63 subjects with severe tooth wear were monitored, concluding that tooth wear may be cyclical and inactive in the majority of participants.
If the procedure of monitoring reveals that the wear process is progressive, it should signal the need for further preventive measures, such as a referral for investigating reflux disease. It may also help to motivate the patient and increase compliance for a more complex restorative treatment.
In cases where tooth wear has progressed so far that retention of possible restorations will become a risk, like when crown height is reduced more than two thirds, we advise the patient to start with rehabilitation even when the patient is satisfied with the situation. However, one should realise that a predictable and successful restorative intervention is always dependent on full commitment and informed consent. Patients with extreme levels of tooth wear might have a particularly high risk of restoration failure due to certain destructive habits. In Figure 4 a male (52 years old) is presented with severe erosive tooth wear, without any functional problems, but complaining about his aesthetic appearance. He consumed many acidic beverages during the day and was aware of bruxism (heavy grinding and clenching during day and night). Furthermore, his working environment was highly abrasive due to (fine) dust from demolition work. From the intake pictures it is obvious that retention of restorations was reduced on his lower and upper anterior teeth. Despite this complicating factor, a full rehabilitation with direct composite restorations was performed. After 2.5 years most posterior restorations were performing well, but pathological wear was found on the lower anterior teeth and several fractures had occurred on the upper anterior teeth illustrating the high risk profile of this patient (Fig. 4). A recent study by Bartlett et al.16 also addresses the need for maintenance and repair in severe tooth wear rehabilitations with composite resin.
At intake almost no retention for the restorations was available. A full rehabilitation with direct composite restorations was performed. After 5.5 years most restorations were performing well, however, a pathological wear was found at the lower anterior teeth and several fractures are seen at the upper anterior teeth. Despite the high risk of fracture, patient did not want to wear a night guard
Restorative intervention
To postpone the start of the restorative cycle,17 the process of counselling and monitoring wear can be continued as long as possible. However, it seems realistic that at a certain moment in time restorative rehabilitation has to start. At the moment patient and dentist come to the consensus that a restorative treatment has to be started; a treatment plan including all possible options and informed consent on the chosen option has to be established.
A diversity of techniques is available for rehabilitation of patients suffering from severe wear. A recent systematic review on the treatment of severe tooth wear was inconclusive regarding whether direct or indirect techniques are to be preferred for these rehabilitations,18 but consensus exists on the recommendation to use minimally invasive treatment options when possible.7 Therefore, the Radboud Tooth Wear Project includes preferably minimally invasive techniques, as tooth wear patients are in need of additive restorations to compensate for tooth substance loss. However, it has to be emphasised that this approach tends to be as complex and demanding as conventional treatments.
The limited available evidence from clinical studies shows that direct composite resin restorations perform adequately in rehabilitation of patients with severe tooth wear,19,20,21,22 although one study showed high failure rates for composite restorations.23 Indirect techniques are also recommended for treatment of severe tooth wear cases, but clinical trials are limited to a study on indirect composites (with unfavourable outcome),23 while no information is available on crowns or onlays. Therefore, we included these techniques in the Radboud Tooth Wear Project including indirect composites and 3D CAD-CAM fabricated resin nanoceramics.
Determination of increased vertical dimension of occlusion
In advance, the optimal intermaxillary position (habitual occlusion or centric relation) in which the patient is going to be rehabilitated has to be determined. In the Radboud Tooth Wear Project patients are treated in centric relation unless clear signs indicate that a predictable and stable intermaxillary position can only be achieved in habitual relation. To obtain space for the restorations the new desired vertical dimension of occlusion (VDO) has to be determined at the start of the rehabilitation. A flowchart is used in the Radboud Tooth Wear Project which starts with the analysis of cast models (Fig. 5).
Using cast models (mounted either in habitual occlusion or centric relation) and based on original anatomical form, the loss of vertical tooth substance at location of the first molar can be estimated, related to the original anatomic form of teeth. The first molar often presents the most wear,15 but in case other posterior or anterior teeth present more wear, the estimation of lost vertical tooth height may be adjusted. Moreover, as a rehabilitation preferably includes a fully supported occlusion and cuspal guidance, it must be decided if and how lower and/or upper anterior teeth need to be lengthened, which is also determined by the preferred aesthetic appearance (smile design). Complicating factors such as overbite, open bite and end-to-end relation tend to limit possibilities and can force the clinician to certain compromises. For example an Angle Class II/1 relation in increased VDO can make it impossible to create anterior contact. Also in the situation of an end-to-end anterior contact or a vertical open bite, one must realise that an increase of VDO in the posterior area will either lead to loss of anterior contact or increased open bite unless compensated by (probably aesthetically undesired) lengthening of anterior teeth. When a necessary increase of VDO is not possible to obtain, orthodontic pre-treatment may be considered before rehabilitation starts.
Using the increased VDO as assessed from the mounted castings, a clinical try-in session is performed to test the VDO clinically, and for making a mock-up for testing the aesthetic appearance by unbonded direct composite build-ups on teeth 13 to 23. The aesthetics of length and width of teeth is evaluated using lip-generated smile design in rest and during speaking and laughing.24 After approval of the patient, this 'analogue' smile design is recorded with intra-oral photographs or, in case CAD-CAM restorations are made, by a digital 3D scan. Additionally, two silicon stops are made in the posterior area in the mounted castings which are transferred to test the desired increased VDO intra-orally, after which the mock-up is removed. Alternatively, a wax-up can be made and a try-in can be applied using a mould. When the patient has given informed consent, the restorative procedure can start.
In the minimally invasive treatment protocols used in the Radboud Tooth Wear Project the use of direct composite resin restorations is preferred. The applied technique for building up follows a protocol starting with lower anterior teeth, followed by upper anterior teeth, lower posterior teeth and upper posterior teeth in which the increase of VDO is transferred intra-orally using the silicon stops made at the mock-up procedure. The technique preferably used for this is the DSO technique (direct shaping by occlusion) which is described elsewhere.25,26 A typical case in which this technique was used is shown in Figure 6. The preoperative situation as well as the situation directly after placement and at five years is shown. No interventions were needed during this follow-up interval and the patient is functioning well and satisfied with the result.
Also indirect restorations made of ceramic, resin ceramics or composite, can be used to rehabilitate worn dentitions. In the Radboud Tooth Wear Project, these restorations are designed as an additive 'uplay or tabletop' and can be fabricated manually by the dental technician or can be digitally designed and manufactured (for example, 3D CAD-CAM). If this indirect technique is only used on a selected amount of teeth, the remaining teeth are restored with a direct composite restoration (so called hybrid technique). Accordingly, already existing direct restorations are either left in place or replaced if necessary, and comparable to the 'deep margin elevation' technique,27,28 proximal surfaces have direct composite at the surface.
In Figure 7 an example is shown of a patient fully treated with 3D CAD-CAM restorations of nanoceramics (LAVA Ultimate, 3M) at intake, directly after placement and at one year recall (Fig. 7). All posterior teeth and the palatal side of the upper and lower anterior teeth were made of indirect manufactured restorations, the buccal veneer restorations on the upper and lower teeth were made of direct composite resin restorations.
The rehabilitation was performed based on 3D CAD-CAM technology using nanoceramic restorations (LAVA Ultimate, 3M). Placement procedure was divided into 2 sessions: first all restorations of session 1 are placed, then in session 2 a new 3D scan and CAD-CAM-design was made after which the final restorations were cemented
Clinical performance of restorations
First preliminary findings show that rehabilitations after a mean observation time of 3.5 years with direct composite show acceptable clinical performance with annual failure rate of approximately 3%.8 In this study no exclusions were made on aetiological factors (for example, presence of bruxism or erosive challenges). Compared to other studies investigating restorative rehabilitation of severe tooth wear patients, the first results of the Radboud Tooth Wear Project on restoration survival are comparable to studies by Hamburger et al.,20 reporting an annual failure rate of 1.5% and Attin et al.19 reporting an annual failure rate 0.3% survival at 5.5 years. Compared to the only randomised clinical trial treating this high-risk patient group, which was published in 2006 by Bartlett and Sundaram,23 our results are much better then in that study that showed 50% failure after three years of molars restored in increased VDO with direct or indirect composite, resulting in an annual failure rate of 16.5%. Types of failures are mostly related to fracture, as can be explained by the inclusion of many severe bruxing patients in our studies. Despite the relatively low failure rate of the composite restorations, a factor which may be of interest is the amount of wear over time, whereas indirect composite restorations tend to show less wear but more fracture. However, we have to wait on further results to confirm these preliminary impressions.
Nevertheless, it can be expected that rehabilitations in increased VDO have to be retreated in the long term. In Figure 8 a case is shown of a 22-year-old male patient that suffered from severe and pathological tooth wear. Aetiology was established as multifactorial: clenching and high frequency of soft drinks as well as reflux symptoms appeared in the dental history at intake. The first rehabilitation using direct composite (Clearfil AP-X) in increased VDO as shown lasted 15 years when increased failure occurred due to wear and fracture. Then a second rehabilitation with a new increased VDO was done. After six years, this rehabilitation is still in function, but increased levels of wear can be observed and it is expected that within five years a new retreatment in increased VDO will be necessary. However, the applied minimal invasive additive adhesive technique allows for repeated rehabilitations without increased risk for complications. It will take several years until these long term data will become available for the large amount of patients included in the Radboud Tooth Wear Project. Meanwhile there is increasing evidence that for severe tooth wear a pragmatic, conservative and minimally invasive approach might the best choice and individual management strategies based on individual diagnosis are probably the most suitable way to go.
In 1995 (intake) a rehabilitation in increased VDO was performed with direct composite restorations (Clearfil AP-X), without involving lower anterior teeth. In 2011 the patient complained of multiple fractures and wear of the lower anterior teeth, and it was decided to do a second rehabilitation with direct composite in increased VDO (Clearfil AP-X) also including lower anterior teeth. In 2017, the result was still satisfying although progressive wear, especially in lower anterior teeth is observed. The patient has no protective night guard. Remarkable observations in this 22-year follow up case are the satisfying performance of direct composite for more than a decade where a second minimally invasive rehabilitation could be done
Conclusions
Restorative treatment is not always indicated for patients with tooth wear. Preventive measures should be advised and arrangements made for counselling and monitoring, irrespective of the severity of the tooth wear.
If tooth wear is considered to be progressive, with a rate giving cause for concern, engage the patient in establishing the main aetiological factors and instituting a mutually agreed-upon programme of preventive measures:
-
If the patient has no complaints: counselling and monitoring is probably the best option to test the efficacy of the preventive measures, preferably relying on (stone or digital) casts
-
If the patient is concerned about her/his appearance or has complaints: (minimally invasive) restorative options should be critically reviewed with the patient.
Minimally invasive and adhesive restorative strategies are preferred when severe tooth wear patients are to be treated in increased vertical dimension, especially when young patients are involved.
Clinical evidence for suitable restorative treatment protocol is limited to five-year follow up for direct composites. This material seems to be suitable for rehabilitation in increased vertical dimension on the middle long term.
Restorations, including composites and full veneer crowns, do not prevent wear processes; they merely modify the rate, location, and nature of the wear. Moreover, most restorations that are considered 'definitive' may prove to have a limited lifetime in patients with severe tooth wear due to bruxism and erosion. Explanation of the possible treatment options and expected complications should be included in the informed consent.
References
Lussi A, Carvalho T S . Erosive tooth wear: a multifactorial condition of growing concern and increasing knowledge. Monogr Oral Sci 2014; 25: 1–15.
El Aidi H, Bronkhorst E M, Huysmans M C, Truin G J . Dynamics of tooth erosion in adolescents: a 3-year longitudinal study. J Dent 2010; 38: 131–137.
Carvalho T S, Lussi A, Jaeggi T, Gambon D L . Erosive tooth wear in children. Monogr Oral Sci 2014; 25: 262–278.
Wetselaar P, Vermaire J H, Visscher C M, Lobbezoo F, Schuller A A . The Prevalence of Tooth Wear in the Dutch Adult Population. Caries Res 2016; 50: 543–550.
Bartlett D W, Lussi A, West N X, Bouchard P, Sanz M, Bourgeois D . Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013; 41: 1007–1013.
Salas M M, Nascimento G G, Huysmans M C, Demarco F F . Estimated prevalence of erosive tooth wear in permanent teeth of children and adolescents: an epidemiological systematic review and meta-regression analysis. J Dent 2015; 43: 42–50.
Loomans B, Opdam N, Attin T et al. Severe Tooth Wear: European Consensus Statement on Management Guidelines. J Adhes Dent 2017; 19: 111–119.
Loomans BAC, Kreulen CM, Huijs-Visser HECE, Sterenborg BAMM, Bronkhorst EM, Huysmans MCDNJM, Opdam NJM . Clinical performance of full rehabilitations with direct composite in severe tooth wear patients: 3.5 Years results. J Dent. 2018 Jan 12. pii: S0300-5712(18)30001-0. 10.1016/j.jdent.2018.01.001. [Epub ahead of print] PubMed PMID: 29339203.
Johansson A, Omar R, Carlsson G E . Bruxism and prosthetic treatment: a critical review. J Prosthodont Res 2011; 55: 127–136.
West N X, He T, Macdonald E L, Seong J, Hellin N, Barker M L, Eversole S L . Erosion protection benefits of stabilized SnF2 dentifrice versus an arginine-sodium monofluorophosphate dentifrice: results from in vitro and in situ clinical studies. Clin Oral Investig 2017; 21: 533–540.
Wilder-Smith C H, Wilder-Smith P, Kawakami-Wong H, Voronets J, Osann K, Lussi A . Quantification of dental erosions in patients with GERD using optical coherence tomography before and after double-blind, randomized treatment with esomeprazole or placebo. Am J Gastroenterol 2009; 104: 2788–2795.
Smith B G N, Knight J K . An index for measuring the wear of teeth. Br Dent J 1984; 156: 435–438.
Bartlett D, Ganss C, Lussi A . Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig 2008; 12 (Suppl 1): S65–S68.
Wetselaar P, Lobbezoo F . The tooth wear evaluation system: a modular clinical guideline for the diagnosis and management planning of worn dentitions. J Oral Rehabil 2016; 43: 69–80.
Rodriguez J M, Austin R S, Bartlett DW . In vivo measurements of tooth wear over 12 months. Caries Res 2012; 46: 9–15.
Bartlett D, Varma S . A retrospective audit of the outcome of composites used to restore worn teeth. Br Dent J 2017; 223: 33–36.
Elderton R J . Clinical studies concerning re-restoration of teeth. Adv Dent Res 1990; 4: 4–9.
Mesko M E, Sarkis-Onofre R, Cenci M S, Opdam N J, Loomans B, Pereira-Cenci T . Rehabilitation of severely worn teeth: A systematic review. J Dent 2016; 48: 9–15.
Attin T, Filli T, Imfeld C, Schmidlin P R . Composite vertical bite reconstructions in eroded dentitions after 5.5 years: a case series. J Oral Rehabil 2012; 39: 73–79.
Hamburger J T, Opdam N J, Bronkhorst E M, Kreulen C M, Roeters J J, Huysmans M C . Clinical performance of direct composite restorations for treatment of severe tooth wear. J Adhes Dent 2011; 13: 585–593.
Poyser N J, Briggs P F, Chana H S, Kelleher M G, Porter R W, Patel M M . The evaluation of direct composite restorations for the worn mandibular anterior dentition – clinical performance and patient satisfaction. J Oral Rehabil 2007; 34: 361–376.
Milosevic A, Burnside G . The survival of direct composite restorations in the management of severe tooth wear including attrition and erosion: A prospective 8-year study. J Dent 2016; 44: 13–19.
Bartlett D, Sundaram G . An up to 3-year randomised clinical study comparing indirect and direct resin composites used to restore worn posterior teeth. Int J Prosthodont 2006; 19: 613–617.
Morley J, Eubank J . Macroesthetic elements of smile design. J Am Dent Assoc 2001; 132: 39–45.
Opdam N, Skupien J A, Kreulen C M, Roeters J, Loomans B, Huysmans M D . Case report: A predictable technique to establish occlusal contact in extensive direct composite resin restorations: The DSO-technique. Oper Dent 2016; 41 (Suppl 7): S96–S108.
Hamburger J, Opdam N, Loomans B . Direct posterior esthetics: a management protocol for the treatment of severe tooth wear with resin composite (chapter 6); Direct posterior esthetics: clinical case (chapter 7). In Banerjee A (ed) Minimally invasive esthetics: essentials in esthetic dentistry series. Amsterdam: Elsevier Health Sciences, 2015.
Magne P, Spreafico R C . Deep margin elevation: A paradigm shift. Am J Esthet Dent 2012; 2: 86–96.
Opdam N, Frankenberger R, Magne P . From 'direct versus indirect' toward an integrated restorative concept in the posterior dentition. Oper Dent 2016; 41 (Suppl 7): S27–S34.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loomans, B., Opdam, N. A guide to managing tooth wear: the Radboud philosophy. Br Dent J 224, 348–356 (2018). https://doi.org/10.1038/sj.bdj.2018.164
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.164
This article is cited by
-
Managing tooth wear with respect to quality of life: an evidence-based decision on when to intervene
British Dental Journal (2023)
-
Effects of in vitro erosion on surface texture, microhardness, and color stability of resin composite with S-PRG fillers
Clinical Oral Investigations (2023)
-
S-PRG-based composites erosive wear resistance and the effect on surrounding enamel
Scientific Reports (2022)
-
Deterioration of anterior resin composite restorations in moderate to severe tooth wear patients: 3-year results
Clinical Oral Investigations (2022)
-
Speech changes in patients with a full rehabilitation for severe tooth wear, a first evaluation study
Clinical Oral Investigations (2020)