Key Points
-
Suggests the tibial intraosseous access is an alternative to the venous access.
-
Explains that the tibial intraosseous access may serve as a rescue procedure available for dentists when treating a medical emergency and a venous access is not possible.
-
Highlights that the method offers the application of medication in cases when fluid has to be given.
Abstract
Background The anterior tibia has been recommended as emergency vascular access site if the intravenous route cannot be used.
Objective This study aims to evaluate the peripheral venous and anterior tibial intraosseous puncture as alternatives for dentists, using a human and a cadaver model.
Method One group of dental students performed a venipuncture by using a standard catheter device (n = 21) on other students. Another group (n = 24) used the Vidacare EZ-IO intraosseous kit on a cadaver tibia with india ink as a tracer. Success rates as well as the time needed for a successful puncture were recorded.
Results 28.5% of venous and 83.3% of intraosseous punctures were successful. The relative risk of venous cannulation failure was 3.4 (95% CI 1.6–7.2; p = 0.0005). A successful venous access could be performed within 163 ± 23.2 seconds (mean ± SD), a tibial intraosseous access within 30 ± 27.8 seconds (p = 0.0003).
Conclusions Within the limitation of this study, it can be demonstrated that the chances to perform a successful vascular access for inexperienced dentists may be higher when using the tibial intraosseous route for emergency intravascular medication.
Similar content being viewed by others
Introduction
Emergency situations requiring intravascular medication are assumed to happen rarely in dental facilities.1 If possible, emergencies should be treated using easy strategies such as intraoral, inhalational or intramuscular applications.2 In severe anaphylaxis, intramuscular adrenaline application is recommended.3 Intramuscular puncture may be much easier for dentists, compared to intravenous cannulation. However, a second line measure in severe anaphylaxis is intravascular fluid support.3 In student education it has been demonstrated, that up to 46 venous cannulations were required to prove competency.4 As dentists' daily work does not cover venous cannulation, this route may not be available for treatment.
Even experienced emergency physicians may encounter challenging situations when a venous access is not possible. Recently, the tibial intraosseous access has been recommended also for the experienced healthcare provider in the emergency medical service in cases of difficult venous access.5
The anterior tibia,6 the humerus,7 the radius,8 as well as the manubrium sterni9,10 have been scientifically evaluated and used pre-clinically as well as in hospital as sites for an intraosseous access.
The purpose of the present study was to compare the capabilities of dental students to establish either an intravenous access at the forearm or the hand of healthy volunteers versus a tibial intraosseous access in a cadaver.
Two null hypotheses were tested:
-
There would be no differences in success rates comparing both procedures
-
There would be no differences in times needed to perform each procedure.
Methods
The study participants were dental students of the first clinical year of two universities and had been educated in emergency medical procedures by the same instructor (T. S. M.). None of the test persons had ever performed a venous or intraosseous vascular access procedure before the test. To avoid carry over effects as well as preparedness of individual participants to perform the respective procedure, no cross over design was chosen.
A sample size estimate had been performed using G*Power (version 3.1.7). It had been assumed that venous punctures would be performed with a higher rate of failure, approximately 25% of punctures being successful, compared to the intraosseous tibial punctures, approximately 75% being successful. At α <0.05 and a power of 0.95, 28 individuals, and at α <0.05 and a power of 0.8, 18 individuals performing each procedure would have been needed per group. The available participant numbers or body donors, respectively, allowed more conservative planning exceeding the minimum power level.
The venous puncture study group participants performed the punctures on each other within a training course of their clinical education. The punctures were performed under close supervision to avoid injury or complications. The intraosseous puncture study group participants performed the tibial punctures on cadavers scheduled for the gross anatomy dissection course. The cadavers had undergone a fixation process involving perfusion of isopropyl alcohol, Lysoformin, formaldehyde and glycerol via the femoral artery
Each student group received a five minute video introduction on how to perform the respective procedure. Only the individuals involved in the immediate procedure were allowed to enter the test room. Blinding individuals regarding failure or success of other participants was achieved by permitting only test persons involved in the respective procedure to enter the test room. The success rates as well as the times needed to perform a successful puncture were recorded. After the test persons had performed the punctures, data were analysed.
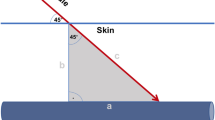
Venous punctures were performed on forearm or dorsal hand veins using venous catheters type Venflon II 1.2 × 45 mm. The intraosseous puncture kit consisted of a Vidacare battery powered motor driven EZ-IO system employing a 25 mm needle (Fig. 1).
Ethics committee approval had been obtained for the documentation and anonymous data evaluation of the venous puncture training the students performed on each other. All students were informed about the intention of the study and gave written informed consent to participate. A general ethical approval for the cadaver experiments issued by the local ethics committee had been obtained, and included the body donors' consent to the scientific and educational use of their bodies after death when they had enrolled into the willed body donor programme of the university.
Statistical analysis
The time intervals between palpation of the puncture site and the possible start of intravascular infusion were recorded. In the venous puncture group time measurement was started after tourniquet application as well as disinfection of the puncture site. Data were entered into a Microsoft Excel spreadsheet and later analysed with the Excel add-in Analyse-it (version 2.30). The exact Fisher test was used to compare the success rates of both procedures. The Mann-Whitney test was employed to compare the distribution of time intervals to perform a successful puncture. Data distribution was considered as statistically different at p values lower than 0.05.
Results
In the venous puncture group of students with the same level of experience 21 individuals could be recruited. The test group using the cadaver model for tibial intraosseous access puncture contained 24 individuals.
A successful intraosseous puncture after dissection of the tibia is demonstrated in Figure 2. Six of 21 venous punctures (28.5%) were successful. In these six cases the vascular catheters would have been usable for the infusion of fluid or medication. In 20 out of 24 intraosseous punctures (83.3%) India ink was detected in the bone marrow and partly in adjacent vessels, indicating a successful intraosseous application of the needle. The groups statistically differ at p = 0.0005, indicating a relative risk of a failed puncture of 3.4 (95% CI 1.6–7.2) using the venous catheter (Table 1).
The students in the venous puncture group needed 163.3 ± 23.2 (mean ± SD) seconds to perform a successful procedure, whereas intraosseous tibial punctures took 30.2 ± 27.8 seconds. The difference was significant at p = 0.0003 (Fig. 3).
No immediate complications occurred. In reality the venous puncture failures would have resulted at least in extravasation of the administered fluid. Soft tissue ink staining observed after intraosseous punctures indicated a failure of intravascular medication.
Discussion
The tibial intraosseous route has the highest success rate of all intraosseous puncture techniques ranging between 67–100%.11
This study evaluated two dental student study populations, who had never performed intravenous or intraosseous puncture procedures. It can be demonstrated that the participants performed intraosseous access punctures at a higher success rate compared to intravenous accesses. The puncture times12 and success rates11 using the intraosseous devices were within the ranges of other publications. However, faster access rates, ranging from 3–25 seconds have also been reported.13 Venous puncture times markedly exceeded the intraosseous ones, but were in the range of published data about emergency venous cannulations.14
Published venous puncture success rates were also lower than the ones found using intraosseous technique.14 Medical students achieved a 50% success rate in this evaluation, but nothing is reported about their experience.
The longer times needed for the intravenous procedures in the present study may be explained by the fact that these had been performed on living subjects.
Limitations
There was no emergency simulation setting around the students. Measures such as tourniquet application, disinfection of the skin as well as preparation of the emergency infusion kit were not examined. However, it is assumed that time intervals needed for additional preparation would not have been different in both procedures.
The non-experience regarding the tested procedures was assumed to reflect residual knowledge of a practicing dentist who had undergone a training session a certain time before the actual emergency procedure is needed. However, the situation may still be different compared to reality as practicing dentists usually acquire manual skills during their career, which may also influence performance characteristics of vascular access procedures. The students of the present study were inexperienced in any puncture procedure. It may be speculated that some groups of dentists may gain experience in vascular access procedures during daily work, for example, for intravenous sedation treatment. The venous puncture success rates may be higher in these groups; however, these dentists using venous cannulation during daily work with a high success rate may, at best, perform comparable to experienced emergency physicians. Even for this specialised population it is recommended to use an intraosseous route when intravenous cannulation is impossible. Therefore, it may be concluded that dentists will have a higher success rate using the tibial intraosseous puncture technique, even if they are experienced in intravenous techniques.
The study populations, though assumed to be equally inexperienced, were not identical. This study configuration was chosen to avoid participants' preparedness for the respective procedures and to exclude carry-over effects; however, matched pairs testing might have revealed different results.
The power calculation had been made to estimate a number needed to achieve a level of significance to reject the null hypothesis at least at the 5% α-level.
The actual number of participants in the study differs from the sample size in the power calculation. The study required a number of individuals at the same level of experience. There were more than 18 but less than 28 available in each group. The decision to reject the null hypothesis (both groups have similar success rates) has been made at p = 0.0005. The post-hoc calculation revealed that the recommended corresponding power level was not reached. This means that the probability of rejecting the null hypothesis tested, when the alternative hypothesis (different puncture results using both devices) is in fact true, was lower than necessary. The α-level of 0.0005 achieved in this first evaluation means a likelihood of 0.05% (in five of 10,000 tests) that the results obtained in this study occurred by chance, and the true result would be that all other groups of dentists at the same level of experience would perform equally successful using intravenous and intraosseous puncture devices.
The venous punctures in the remaining individuals not available for testing the venous access with a more conservative approach at high test power would all have been successful. That means seven (28 minus 21) more successful venipunctures and, at worst, four (28 minus 24) more failed intraosseous punctures. Using these counts, the exact Fisher test would result in acceptance of the null hypothesis: both puncture techniques have the same proportions of success. This would mean that the intraosseous puncture technique would be at least an alternative procedure to consider in special situations.
The first null hypothesis to be tested here was that there would be no differences in success rates comparing both procedures. The testing environment was rated as close to reality as achievable. It included venipunctures only in healthy individuals, that all had visible filled forearm veins. Furthermore, as a standard in this type of education, the instructor is always close to the student performing the venipuncture and - in contrast to the cadaver part of the study, where no comments were made throughout the whole procedure – a student not being stopped or guided by the instructor may gain confidence in proceeding with the puncture. The results may have been biased as all students were aware of the safety referee, who was able to interfere and prevent severe damage. The cadaver model for intraosseous puncture however, can easily serve to simulate a shock situation. It may be assumed that all successful venipunctures in the present evaluation would have been unsuccessful in case of shock, and the unsuccessful venipunctures in the experiment would also have been unsuccessful in a shock situation. The results in the intraosseous group, however, would remain unchanged. The exact Fisher test result would then indicate a p <0.0001 at a power of 0.98. For ethical reasons, such an experiment would not be performed, however. The main finding of the present study is that the students had a failure rate of only 16.7% using the intraosseous tibial access, which is within the range of observations in the pertinent literature investigating other healthcare providers.
A rapid fluid challenge using either of both techniques, venous and intraosseous access, would be a second line intervention when first line measures such as intramuscular adrenaline application in case of anaphylaxis would not deliver the desired result – a stabilisation of circulation. Although the intraosseous access is not recognised for use in dental practice, the UK Resuscitation Council recommends the intraosseous route for trained individuals, if the intravenous access is delayed or impossible.15 As dentists have also been trained to perform intravenous sedation, it may be even easier for this population of healthcare providers, as well as those not trained in intravenous access procedures, to learn intraosseous puncture techniques for the emergency treatment of anaphylactic shock.
An exact definition of 'rapid' has not been made. However, in the present evaluation the successful venous puncture procedures needed longer than two minutes, whereas three out of four successful intraosseous punctures were performed in less than 30 seconds and all but one were ready for infusion in less than 50 seconds.
Dental societies should discuss the recommendation for dental communities to administer medication via the tibial intraosseous route in desperate situations such as severe anaphylaxis for example, when adrenaline given intramuscularly has not resulted in circulatory stabilisation and measures such as fluid replacement cannot be achieved by intravenous application.
Conclusions
In this study, two intravascular access techniques were employed by two equally inexperienced groups of dental students. Intravenous puncture procedures in healthy volunteers were compared to anterior tibial intraosseous drilling punctures aided by a battery powered motor driven device in body donors. The success rates and times to perform a successful procedure were recorded. Within the limitation of the present study, it can be demonstrated that the chances to perform a successful vascular access for dentists inexperienced in venous puncture techniques may be higher when using the tibial intraosseous route in case of a medical emergency requiring intravascular medication. The relatively high success rate and the possibility to achieve a vascular access within a short time interval advocates the tibial intraosseous access as a valuable alternative emergency procedure for the dental office.
References
Atherton G J, McCaul J A, Williams S A . Medical emergencies in general dental practice in Great Britain. Part 1: their prevalence over a 10-year period. Br Dent J 1999; 186: 72–79.
Greenwood M, Meechan J G . General medicine and surgery for dental practitioners: part 3. Management of specific medical emergencies in dental practice. Br Dent J 2014; 217: 21–26.
Simons F E R, Ardusso L R, Bilò M B et al. International consensus on (ICON) anaphylaxis. World Allergy Organ J 2014; 7: 9.
Murgatroyd H, Jones J, Kola S, George D . Cumulative sum scoring for medical students. Clin Teach 2012; 9: 233–237.
Nolan J P, Soar J, Zideman D A et al. European resuscitation council guidelines for resuscitation 2010, section 1. Executive summary. Resuscitation 2010; 81: 1219–1276.
Tocantins L M, O'Neill J F . Complications of intra-osseous therapy. Ann Surg 1945; 122: 266–277.
Kovar J, Gillum L . Alternate route: the humerus bone a viable option for IO access. JEMS 2010; 35: 52–59.
Waisman M, Waisman D . Bone marrow infusion in adults. J Trauma 1997; 42: 288–293.
Tocantins LM, O'Neill J F, Price A H . Infusions of blood and other fluids via the bone marrow in traumatic shock and other forms of peripheral circulatory failure. Ann Surg 1941; 114: 1085–1092.
Erdmann L, Doll S, Ihle B, Kirsch J, Mutzbauer T S . Evaluation of the sternal intraosseous route as alternative emergency vascular access for the dental office: a manikin and cadaver model pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 686–691.
Santos D, Carron P-N, Yersin B, Pasquier M . EZ-IO(®) intraosseous device implementation in a pre-hospital emergency service: a prospective study and review of the literature. Resuscitation 2013; 84: 440–445.
Torres F, Galán M D, Alonso M del M, Suárez R, Camacho C, Almagro V . Intraosseous access EZ-IO in a prehospital emergency service. J Emerg Nurs 2013; 39: 511–514.
Levitan R M, Bortle C D, Snyder T A, Nitsch D A, Pisaturo J T, Butler K H . Use of a battery-operated needle driver for intraosseous access by novice users: skill acquisition with cadavers. Ann Emerg Med 2009; 54: 692–694.
Lapostolle F, Catineau J, Garrigue B et al. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med 2007; 33: 1452–1457.
Soar J, Pumphrey R, Cant A et al. Emergency treatment of anaphylactic reactionsguidelines for healthcare providers. Resuscitation 2008; 77: 157–169.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Goldschalt, C., Doll, S., Ihle, B. et al. Peripheral venous or tibial intraosseous access for medical emergency treatment in the dental office?. Br Dent J 218, E16 (2015). https://doi.org/10.1038/sj.bdj.2015.384
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.384