Abstract
Study design:
Retrospective cohort analysis with prospective follow-up.
Objectives:
To evaluate neurological and functional recovery following central cord syndrome.
Setting:
Northern Ireland, population 1.8 million.
Methods:
Twenty-seven cords were identified in 1 year. Five managed conservatively and 22 with surgery. American Spinal Injury Association (ASIA) motor scores (AMS) were calculated to assess neurological recovery. Rotterdam scores assessed functional independence at 3 years.
Results:
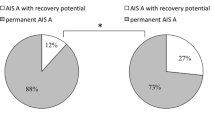
Average age was 62 years. Mechanism of injury was a fall with neck hyperextension in 81% patients. Average AMS in surgical patients improved from injury, preoperatively, postoperatively, 6 months and 3 years from 51, 81, 83, 90 to 96, respectively. Conservative patients improved from time of injury to day 10 from 57 to 86 and then fell to 84 at 6 months. By 3 years, this had recovered to 91. There was no statistical significant difference in AMS (P=0.15)/change in AMS (ΔAMS) (P=0.92) or percentage of motor deficit resolution (P=0.23) between groups at 3 years. Two patients underwent surgery within 48 h and achieved full motor recovery by 3 years, but this was not significant (P=0.2). ASIA score improvement had a positive correlation with age at injury. Patients treated with surgery had better Rotterdam scores at 3 years than those managed conservatively (P=0.05).
Conclusions:
This study confirms the natural history of central cord syndrome. Although it demonstrates equivocal neurological recovery for both groups, patients treated with surgery regained a greater degree of functional independence.
Similar content being viewed by others
Introduction
Central cord syndrome is the most common incomplete acute spinal cord injury (SCI) accounting for approximately 70% of incomplete injuries.1 Schneider et al.2 first described the condition in 1954 as ‘disproportionately more motor impairment of the upper than the lower extremities, bladder dysfunction, usually urinary retention and varying degrees of sensory loss below the level of the lesion’. The syndrome results from a hyperextension injury causing cord compression and injury to the central portion of the spinal cord, sparing the lateral tracts to the sacrum and lower limbs.3, 4, 5 It has been noted that this clinical picture occurs in a bimodal distribution with young and elderly patients. Injury in the younger patient occurs following high-energy trauma with or without congenital cervical stenosis; however, in the older patient, this syndrome develops as a result of a hyperextension injury in a preexisting stenotic canal. The pathophysiology is thought to result from pinching of the spinal cord between a buckled hypertrophied ligamentum flavum posteriorly and bulging disc osteophyte complex anteriorly.6
Schneider initially advocated surgery for the treatment of this condition but with limited success. One of the patients in his initial case series became quadriplegic from surgery. He subsequently managed the remaining patients conservatively and noted that the natural history of this condition was for spontaneous neurological improvement. That study concluded that surgical decompression was unnecessary and detrimental and shaped the management of this condition for many years to come.
Most patients do improve initially; however, recovery is often incomplete and not sustained. Bosch et al.7 and Bose et al.8 reported that many conservatively managed patients experience late-onset neurological deterioration and only 60% remained functional despite a period of initial improvement. This deterioration can have severe functional limitation on basic activities of daily living. It could mean the difference between assisted living and functional independence.
There have been many developments in the management of acute traumatic SCI in the past 50 years. The involvement of the multidisciplinary team improved surgical technique and early mobilization with focused rehabilitation has revolutionized patient care. A number of studies have been published reporting favorable results for surgical intervention and early decompression,9, 10, 11, 12 and more recently, in 2013, a systematic review of 22 trials examining the timing of surgery in SCI found a significant improvement in neurological outcomes and length of hospital stay with early decompression.13 Yet it can be difficult to predict the neurological recovery to be expected. Some patients experience a rapid improvement, whereas others have continued to have significant residual neurodisability. Central cord syndrome remains controversial with widespread variability between centers in both treatment and outcome.
The primary aim of this study was to evaluate whether surgical decompression improved neurological recovery compared with conservative management. The secondary aim was to evaluate whether surgery within 48 h led to better neurological outcome than late decompression. The third aim was to assess whether surgery improved functional independence at 3 years.
Methods
Design and setting
Between April 2011 and April 2012, 27 consecutive patients who presented to the Royal Victoria Hospital, Belfast, UK with traumatic central cord syndrome were included in this study. Patients were identified using the regional trauma database cross referenced with the spinal multi-disciplinary team register.
Participant selection criteria
Neurological exam and imaging confirmed the diagnosis. An inclusion criterion was a primary diagnosis of TCCS (defined as a cervical SCI producing disproportionately greater weakness in the upper limbs than the lower limbs with varying degrees of sensory loss and bladder dysfunction). Magnetic resonance imaging was the modality of choice, or computed tomography if magnetic resonance imaging was contra-indicated. Information gathered included demographics, mechanism of injury, length of hospital stay and functional status.
Treatment selection criteria
Five patients were managed conservatively and 22 with surgical intervention. There were six Consultant Spinal surgeons working in this unit and treatment was decided on an individual case basis, as there is no consensus in the literature or national guideline to dictate management. Absolute indication for surgery included deteriorating neurology with evidence of radiological compression and spinal instability. The timing of surgical intervention was based on evolving neurology, theater availability, suitability for general anesthesia and anticipation of recovery based on radiological diagnosis.
The choice of surgical approach was dependent on the number of levels involved and whether the compression was anterior or posterior. Single-level disease from anterior disc osteophyte complex at C5/6 would be treated with anterior cervical discectomy and fusion at C5/6, whereas multi-level stenosis would be treated with posterior instrumentation and decompression. Other patient factors were also taken into consideration such as patient positioning, that is, the ability to prone under general anesthesia.
Zero patients received steroids in keeping with hospital protocol. One of the surgical patients passed away prior to follow-up at 6months owing to gastric lymphoma and was therefore excluded from analysis. A second surgical patient passed away prior to final follow-up and was excluded from the 3-year analysis.
Assessment tools
The American Spinal Injury Association (ASIA) motor scores (AMS)14 were obtained in the operative group from the time of injury, preoperatively, postoperatively and at follow-up. The ASIA scores were collected at time of injury, day 10 and at follow-up in the conservative group. Follow-up for both groups was at 6 months and 3 years. AMS were further subclassified according to age for analysis: group 1 (<50 years), group 2 (50–70 years), and group 3 (70+ years).
Change in motor score (ΔAMS) and the motor percentage deficit resolution (motor %DR), were calculated for each time interval.
Deficit resolution was calculated using the formula described by Ishida and Tominaga15: (Review AMS−initial AMS)/(100−initial AMS) × 100%.
Mobility aid requirements at follow-up were compared with premorbid mobility. The Rotterdam nine-item handicap scale16 was used at 3 years to assess nine parameters: mobility indoors, mobility outdoors, kitchen tasks, domestic tasks indoors, domestic tasks outdoors, leisure activities indoors, leisure activities outdoors, ability to drive, and finally return to occupation. Bladder and bowel control was also assessed at 3-year review.
Statistical analysis
Continuous variables were described as mean±s.d. Mann–Whitney U and Kruskal–Wallis tests were used to compare non-parametric data sets. Data analysis and visualization was aided by the QIMacros for excel (KnowWare International Inc., Denver, CO, USA), Daniel’s XL Toolbox add in for Excel, version 6.60 (Daniel Kraus, Würzburg, Germany) and Microsoft Excel (2010), (Microsoft corporation, Redmond, WA, USA) software packages. Statistical significance was set at P<0.05.
Results
Demographics
Twenty-seven patients with central cord syndrome were identified in 1 year. Five were managed conservatively and 22 with surgery. Average age of patient was 62 years (range 33–85). Twenty-two (81%) were male. In 22 patients (81%), the mechanism of injury was a simple fall with neck hyperextension. Two surgical patients had passed away before completion of follow-up at 3 years. Twenty of the surviving 25 patients (80%) completed follow-up at 3 years. This comprises 16 of the 20 (76%) managed operatively and 4 of the 5 (80%) non-operatively. A further patient from the surgical cohort was excluded from the 3-year analysis as he had suffered a cerebral vascular event that left him with a hemiplegia and would therefore confound results.
Imaging and surgical approach
Twenty-one (78%) had preexisting cervical stenosis on imaging. The most common level of injury was C5/6, occurring in 11 (41%) patients. Thirteen patients underwent a posterior approach, of which 11 had multi-level decompression and stabilization. Eight patients had a single-level anterior cervical discectomy and fusion. One patient had an anterior cervical discectomy and fusion followed by multi-level posterior decompression and stabilization at a later date. Average time to surgery was 24 days (1–120).
Neurological assessment
The average ASM in the surgical cohort improved from injury, preoperatively, postoperatively, 6 months and at 3 years follow-up from 51, 81, 83, 90 to 96, respectively (Figure 1). The average ASM in the conservative group improved from time of injury to day 10 from 57 to 86 but then fell to 84 at 6 months. Interestingly at 3-year follow-up this had improved to 91 (Figure 2).
Despite the average AMS at 3 years in the surgical group being higher than that of the non-operative group, 96 vs 90, this did not reach statistical significance (P=0.15). Neither did ΔAMS (P=0.92) or motor %DR (P=0.23).
Neurological assessment subclassified for age
Patients were subclassified according to age for a more detailed analysis. Group 1 (<50 years) consisted of 7 patients with a mean age of 42.8 years (33–50). Group 2 (50–70 years) consisted of 6 patients with a mean age of 57 years (51–63) and group 3 had 8 patients with a mean age of 77 years (71–85). All patients demonstrate a rapid initial improvement in AMS (Table 1), but younger patients at the time of injury did better overall (Table 2). Not only did they have ultimately better AMS at follow-up, they had greater change in AMS and better %DR when compared with patients in groups 2 and 3. This supports Penrod’s finding that patients aged <50 years have ultimately better ASIA motor scores and therefore better potential to regain functional independence.17
Of the eight surgical patients in group 3, two were deceased, one had a cerebrovascular event, one had advanced dementia and one had terminal lung cancer by 3-year review. This highlights the frailty of the population intended to treat and the need for appropriate management to ensure maximum quality of remaining life.
Functional assessment
Mean Rotterdam scores at 3 years were 83% s.d.±23 in the surgical group (n=15) vs 70% s.d.±21 in the conservative group (n=4). This difference was found to be statistically significant (P=0.05).
Complications
No intra-operative complications were observed. One superficial wound infection occurred. In all, 14% of the surgical cohort developed chest sepsis in comparison with 40% in the conservatively managed group.
Bladder/bowel
At 3 years, only 2 patients from each group reported bladder/bowel dysfunction. The 4 patients with deficits were numbers 8, 12, 24 and 26 (Table 3).
Mobility
At 6 months, 67% of surgical patients reached their premorbid mobility status, compared with 60% of patients managed conservatively. However, when subclassified for age, 86% of surgical patients in group 1 (<50yrs) were mobile unaided compared with 67% in group 2 and 38% in group 3. At 3 years, 100% of the surgical cohort had reached baseline mobility (Table 3) as compared with 50% of the conservative cohort.
Crossover
One patient (patient number 23) was initially managed conservatively owing to intra-abdominal sepsis at the time of injury. He transferred to the spinal rehabilitation unit and his motor score improved from injury, day 10 to 6 months from 74, 86 to 88. However, he plateaued and further imaging confirmed persistent compression. He underwent decompression on day 485, and at 3-year review, his motor score had improved to 92.
Discussion
The classic paper on central cord syndrome by Schneider et al.2 in 1954 described the spontaneous neurological recovery experienced by these patients. The paper set a trend in the subsequent literature for these patients to be managed conservatively, and it was only when Bosch et al.7 and Bose et al.8 evaluated the long-term neurological status of these patients was it suggested that their management could be improved. Newey et al.1 in 2000 studied 32 patients with central cord syndrome managed conservatively and found that, after a mean of 8.6 years of follow-up, ASIA score was usually maintained but patients who were >70 years of age did poorly. Brodkey et al.18 in 1980 further supported this finding and demonstrated a decline in function in their conservative cohort. Cervical myelography was performed in these patients that showed persistent cord compression. These patients proceeded to have surgery and improve. This was similar to the result of patient number 23 in our study who was initially managed conservatively but, when his neurological recovery plateaued, further imaging revealed persistent compression. He went on to have surgery and his motor function continued to improve.
The initial study by Schneider was a single-surgeon case series of 8 patients that influenced the management of central cord for a further 30 years. Since then, dramatic improvements have been made in the management of acute SCI but a lack of robust peer-reviewed data leads to the controversy surrounding its management. This study highlights that, even within a tertiary referral center for 1.8 million patients, no consensus exists among surgeons regarding the timing of surgical decompression. Although the average time taken to theater was 24 days, this ranged from anywhere between 24 h and 120 days.
Lenehan et al.19 and Guest et al.20 have reported that early surgery (<24 h) is safe and cost-effective compared with late surgery.
In our study, only two patients were operated on within 48 h but they went on to achieve a full motor and functional recovery.
Chen et al.21 in 2009 claimed that surgical intervention can be safely undertaken in patients with traumatic central cord syndrome. The Surgical Timing in Acute Spinal Cord Injury Study9 demonstrated recovery by ⩾2 ASIA grades in an additional 10% of cervical spinal cord injuries with surgery <24 h from injury. However, motor incomplete grade ‘D’ can only improve by one category.
There is convincing evidence in the literature to suggest that surgery provides two potential advantages over conservative treatment. First, improved neurological recovery achieved after early decompression of the cord and nerve roots may permit earlier rehabilitation; second, stable spinal fixation may prevent further SCI and subsequent neurological deterioration. Although we failed to demonstrate a statistical difference in neurological recovery between groups, patients treated with surgery did have significantly improved mobility and functional independence at 3 years.
Our study has a few limitations. First, the cohort had few patients treated conservatively. This was a result of the study design in that it was retrospective and not randomized. However, this study is a snapshot and is therefore reflective of the practice in Northern Ireland. Second, owing to small numbers, the groups were not matched to eliminate selection bias.
In conclusion, this study confirms the natural history of central cord syndrome by showing that the majority of patients are males, aged >75 years presenting following a simple fall with neck hyperextension with preexisting stenosis. It has demonstrated that the majority of recovery does happen spontaneously in the first few weeks after injury and that the younger patient does better. This study also suggests that early surgical intervention (<48 h) will produce ultimately better motor ASIA scores at follow-up as compared with conservatively managed patients. Patients treated with surgery regained a greater level of functional independence. Controversy persists in the literature and no clear consensus can be proposed because of the lack of prospective controlled studies. Further research in this area is required.
Data archiving
There were no data to deposit.
References
Newey ML, Sen PK, Fraser RD . The long-term outcome after central cord syndrome: a study of the natural history. J Bone Joint Surg Br 2000; 82: 851–855.
Schneider RC, Cherry G, Pantek H . The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg 1954; 11: 546–577.
Shrosbree RD . Acute central cervical spinal cord syndrome—aetiology, age incidence and relationship to the orthopaedic injury. Paraplegia 1977; 14: 251–258.
Merriam WF, Taylor TK, Ruff SJ, McPhail MJ . A reappraisal of acute traumatic central cord syndrome. J. Bone Joint Surg Br 1986; 68: 708–713.
Roth EJ, Lawler MH, Yarkony GM . Traumatic central cord syndrome: clinical features and functional outcomes. Arch Phys Med Rehabil 1990; 71: 18–23.
Aito S, Andrea M, Werhagen L, Farsetti L, Capelli S, Bandini B et al. Neurological and functional outcome in traumatic central cord syndrome. Spinal Cord 2007; 45: 292–297.
Bosch A, Stauffer ES, Nickel VL . Incomplete traumatic quadriplegia. A ten-year review. JAMA 1971; 216: 473–478.
Bose B, Northrup BE, Osterholm JL, Cotler JM, DiTunno JF . Reanalysis of central cervical cord injury management. Neurosurgery 1984; 15: 367–372.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE 2012; 7: e32037.
Anderson DG, Sayadipour A, Limthongkul W, Martin ND, Vaccaro A, Harrop JS . Traumatic central cord syndrome: neurologic recovery after surgical management. Am J Orthop 2012; 41: 104–108.
Harrop JS, Sharan A, Ratliff J . Central cord injury: pathophysiology, management and outcomes. Spine J 2006; 6: S198–S206.
Quencer RM, Bunge RP, Egnor M, Green BA, Puckett W, Naidich TP et al. Acute traumatic central cord syndrome: MRI-pathological correlations. Neuroradiology 1992; 34: 85–94.
van Middendorp JJ, Hosman AJ, Doi SA . The effects of the timing of spinal surgery after traumatic spinal cord injury: a systematic review and meta-analysis. J Neurotrauma 2013; 30: 1781–1794.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Ishida Y, Tominaga T . Predictors of neurologic recovery in acute central cervical cord injury with only upper extremity impairment. Spine 2002; 27: 1652–1658.
Merkies IS, Schmitz PI, Van Der Meché FG, Samijn J, Van Doorn PA . Psychometric evaluation of a new handicap scale in immuneuneatic review and metaies. Muscle Nerve 2002; 25: 370–377.
Penrod LE, Hegde SK, Ditunno JF . Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehabil 1990; 71: 963–968.
Brodkey JS, Miller CF, Harmody RM . The syndrome of acute central cervical spinal cord injury revisited. Surg Neurol 1980; 14: 251–257.
Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF . The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine 2010; 35: 180–186.
Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VKH . Traumatic central cord syndrome: results of surgical management. J Neurosurg 2002; 97: 25–32.
Chen L, Yang H, Yang T, Xu Y, Bao Z, Tang T . Effectiveness of surgical treatment for traumatic central cord syndrome: clinical article. J Neurosurg Spine 2009; 10: 3–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Stevenson, C., Dargan, D., Warnock, J. et al. Traumatic central cord syndrome: neurological and functional outcome at 3 years. Spinal Cord 54, 1010–1015 (2016). https://doi.org/10.1038/sc.2016.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.34
This article is cited by
-
Timing of decompression in central cord syndrome: a systematic review and meta-analysis
European Spine Journal (2024)
-
Treatment of acute traumatic central cord syndrome: a score-based approach based on the literature
European Spine Journal (2023)
-
Is it time to redefine or rename the term “Central Cord Syndrome”?
Spinal Cord (2021)
-
Early durotomy with duroplasty for severe adult spinal cord injury without radiographic abnormality: a novel concept and method of surgical decompression
European Spine Journal (2019)