Abstract
Study design:
A retrospective study.
Objective:
To elucidate the correlation between compound muscle action potentials (CMAPs) amplitudes and responsible level of compressive cervical myelopathy (CCM), and the accuracy of level diagnosis by using CMAPs.
Setting:
This study was conducted at the Department of Orthopedic surgery, Yamaguchi University Graduate School of Medicine, Japan.
Method:
A total of 28 patients with CCM were investigated in this study. Erb’s point-stimulated CMAPs were measured from deltoid, biceps, triceps in all patients as compared with 88 healthy subjects. We performed a level diagnosis on the basis of CMAPs amplitudes. We performed a level diagnosis on the basis of CMAPs amplitudes and using an index that measures the deviation of CMAPs amplitudes between triceps and deltoid or biceps.
Results:
Significant correlations between the mean CMAPs amplitudes and responsible level were showed for deltoid (6.82±2.33 mV) at C3/4 (P<0.01) and biceps (8.75±4.42 mV) at C4/5 (P=0.015). Despite considerable individual variability in CMAP amplitudes, there were correlations among CMAPs amplitudes for deltoid, biceps and triceps in the same individual. The sensitivity was 75.0%, specificity 75.0% in the index for diagnosis of C3/4. The sensitivity was 75.0%, specificity 66.7% in the index for diagnosis of C4/5.
Conclusion:
This study showed small CMAPs amplitudes in the deltoid indicated a C3/4 level of myelopathy and in biceps at the C4/5 level and could help exclude clinically silent cord compression and determine the surgical procedure to the suitable level of concern.
Similar content being viewed by others
Introduction
Magnetic resonance imaging (MRI) can be used to demonstrate compression of the spinal cord and has an important role for level diagnosis in cases with compressive myelopathy. However, MRI can show abnormal findings despite clinically asymptomatic presentation and therefore it is difficult to determine the responsible level in patients with multilevel spinal compression, as, for example, in elderly people. Ossification of the posterior longitudinal ligament may also occur at several vertebral levels during spinal cord compression, but not all levels compressed by the ossification of the posterior longitudinal ligament lead to symptomatic spinal cord compression. Spinal cord-evoked potentials (SCEPs) are useful for investigating the functional integrity of the spinal cord, in spite of MRI evidence of compression at several levels.1, 2
We also reported compound muscle action potential (CMAPs) amplitudes that were lower than normal values indicated the involvement of anterior horns.3 However, there have so far been no reports that correlated the responsible level of cervical myelopathy (CCM) with CMAPs amplitudes.
We hypothesized that preoperative measurement of CMAPs could be used for level diagnosis of CCM. In the present study, we correlated CMAPs amplitudes with the responsible level in an attempt to provide preoperative level diagnosis.
Materials and methods
Patients
A total of 28 patients with CCM (18 with cervical spondylotic myelopathy and 10 with ossification of the posterior longitudinal ligament) were determined by intraoperative SCEPs to have a single site of conduction abnormalities at the intervertebral level. Eighteen were men and 10 were women and their average age was 70.8 years (range; 48–86). All patients underwent cervical laminoplasty. Written informed consent with the approval of Yamaguchi University Graduate School of medicine was obtained for preoperative MRI investigation and electrophysiological studies in all patients. Those who fulfilled the following criteria were included in the study.
A diagnosis of myelopathy was established based on the presence of hyperreflexia, including a positive Hoffmann sign, upper extremity sensory disturbance and obvious MRI-documented cervical spinal cord compression. Sensory and motor nerve conduction velocities in the peripheral nerves were within normal limits.
Patients who had peripheral neuropathy and concomitant radiculopathy were excluded.
Normative data
Thirty-nine male and forty-nine female subjects (average age 54.3 years, age range 23–91 years) with no history of injury or pathology of the upper limb were studied. They were submitted to a medical examination consisting of a detailed history regarding motor and sensory upper limb symptoms, followed by thorough physical examination. Exclusion criteria were a history of upper limb symptoms, glove and stocking sensory symptoms, diabetes mellitus, any form of medication and abnormal tendon reflexes or sensory and motor examination.
Magnetic resonance imaging
All patients underwent MRI with a 1.5-tesla imaging system. Sections were 5-mm thick, with a 2-mm gap between intersections. T1-weighted and T2-weighted sagittal and axial imaging were obtained.
Electrophysiological investigation
Erb’s point-stimulated CMAPs
All electrophysiological examinations were performed using a Nicolet Viking 4 instrument. Erb’s point-stimulated CMAPs were recorded in the deltoid, biceps brachii (biceps), and triceps brachii (triceps) muscles in all subjects. An 11 mm diameter disc (Dantec 13L 29, Dantec Medical, Skovlunde, Denmark) was placed over the middle of the deltoid as an active electrode, on the acromion as a reference electrode in the deltoid, over the middle of the biceps muscle as an active electrode and on the lateral epicondyle of humerus as a reference electrode in the biceps muscle, and over the middle of the triceps muscle as an active electrode and on the olecranon as a reference electrode in the triceps muscle. The skin was prepared with an abrasive solution to reduce impedance and a ground strap was wrapped around the elbow. The bipolar stimulator probe (Nicolet S403, Natus Medical, San Carlos, CA, USA) provides a pair of bare metal contacts, 3 mm in diameter and with an adjustable inter-electrode distance which was set to 25 mm in our study. The stimulus intensity was gradually increased until it no longer altered the size of the recorded response. Measurement of CMAPs included the negative-peak amplitude from baseline to peak. Average amplitudes for CMAPs were calculated for both sides. The amplitude ratio was calculated by dividing the response from one side by the other and multiplying by 100.
Recording of SCEPs for diagnosis of symptomatic lesion
SCEPs after median nerve stimulation (MN-SCEPs), transcranical electric stimulation (TES-SCEPs), and spinal cord stimulation (Spinal-SCEPs) were recorded intraoperatively. The median nerves were stimulated (square wave pulse, 0.2-ms duration, 3-Hz rate) at the wrist with the cathode placed proximally. The stimulus intensity was set at 1.5 times for producing the thumb twitch in an awakened condition. TES was delivered as square pulses of 0.2 ms duration and at an intensity of 100 mA through needle electrodes (13R25, length 8 mm, diameter 0.8 mm; Dantec, Skovlunde, Denmark) placed on the skull. The anode was placed 7 cm laterally to the right of the vertex on line joining the external auditory meatus. The cathode was placed on the opposite side. Spinal-SCEPs were delivered by an epidural catheter electrode (UKG-100-2PM, diameter 0.8 mm, length 900 mm, Unique Medical Corporation, Kobe, Japan) inserted into the dorsal epidural space from the C7-T1 and T11-T12 interlaminar space. Square wave pulse (0.2 ms duration, 3-Hz rate) was delivered at an intensity of 15–20 mA. Before laminoplasty, all SCEPs were recorded intraoperatively with recording electrodes (13R25) inserted in the ligamentum flavum at each interlaminar space. A reference electrode was inserted into the subcutaneous tissue in the posterior aspect of the neck for the recording of MN-SCEPs and Spinal-SCEPs. A bipolar recording method was used (active proximal and reference distal) for the recording of TES-SCEPs. All SCEPs signals were amplified and filtered with a bandpass of 20 to 3000 Hz using a standard evoked potential/electromyography machine (Nicolet Viking, Natus Medical). Average of 100 to 200 MN-SCEPs, 40–60 TES-SCEPs and 20–30 spinal-SCEPs responses were obtained. Two different averaged responses were superimposed and displayed. In MN-SCEPs, abnormality was determined from the amplitude ratio of spinal responses at each intervertebral level to that recorded at the C6/7 intervertebral level as reported earlier.4 In TES-SCEPs and Spinal-SCEPs, intervertebral levels with a marked reduction in size of the negative peak (reduction of >50%) were considered as significant (Figure 1).5
SCEPs obtained from patients with compressive cervical myelopathy. MN-SCEPs demonstrate marked attenuation of amplitude at the C3/4 intervertebral level. TCE-SCEPs also show marked attenuation of amplitude at the C3/4 level. Spinal-SCEPs also show marked attenuation of amplitude at the C3/4 level. The marked attenuation of amplitudes at C3/4 in all SCEPs indicates a conduction block at C3/4. MN-SCEPs, spinal cord-evoked potentials following median nerve stimulation; TCE-SCEPs, spinal cord-evoked potentials following TES; Spinal-SCEPs, spinal cord-evoked potentials following spinal cord stimulation.
Preoperative level diagnosis using CMAPs
Studies on the level diagnosis for CCM have shown the C5 motor segment in the spinal cord to be at the level of the C3/4 disc and the C6 motor segment at the level of the C4/5 disc. We have previously reported that C5 and C6 nerve roots are distributed to the deltoid and biceps muscle, with the deltoid predominantly innervated by the C5 nerve root and the biceps by the C6 nerve root.6, 7 We hypothesized the main myotomal distribution was as follows: deltoid in C5 cord segment, biceps in C6 and triceps in C7. If the preoperative CMAPs amplitudes in deltoid were smaller than the normal limits, the responsible level was estimated to be C3/4. This meant that the C5 cord segment was involved. In the same way, if the CMAPs in biceps were smaller, we estimated the responsible level to be C4/5 and this meant the C6 cord segment was involved. We used CMAPs in deltoid and biceps on the affected side and in triceps on the normal side. As described further below, CMAPs amplitudes in triceps correlated with CMAPs amplitudes in the deltoid and biceps. On the basis of this correlation, we designed an index for level diagnosis. When the observed CMAPs amplitudes in the deltoid or biceps were lower than those extrapolated from the CMAPs amplitudes in triceps, this was an indication of C3/4 or C4/5 myelopathy (Table 1).
Statistical analysis
Descriptive statistics, including the mean and standard deviation (s.d.), were applied to each CMAPs value. Related on sex and age factors in CMAPs amplitudes were analyzed. Regression analysis was used to evaluate the correlation among CMAPs amplitudes for the different muscles. (Dependent variables: CMAPs amplitudes in the deltoid- or biceps-independent variable: CMAPs amplitudes in triceps) The Mann–Whitney U test was used for unpaired data. The cutoff points for CMAPs amplitudes or for the index were selected by receiver-operating characteristic curve analysis. Receiver-operating characteristic curves were also used to calculate the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the preoperative diagnosis corresponding to each intervertebral level. All P-values <0.05 were regarded as statistically significant. The free software program R version 2.14 (http://www.r-project.org/) was used for statistical analysis.
Results
Normative data
The normal value (mean±s.d.) for CMAPs in the deltoid muscle was 10.44±2.18 mV amplitude (range 6.17–16.7), in biceps it was 10.83±2.65 mV (4.79–17.18) and in triceps it was 12.59±3.25 mV (4–21.3). Each amplitude showed large variation. Amplitudes in all muscles decreased with advancing age, but these correlations were weak (deltoid: R*2=0.13; biceps: R*2=0.05; triceps; R*2=0.01; where R*2 is the coefficient of determination adjusted for degree of freedom). Compared with women (mean age 53 years, n=49), men (mean age 55 years, n=39) showed significantly higher amplitude in all three muscles (deltoid: 11.5±2.15 mV vs 9.6±1.81 mV, P<0.01; biceps: 12.21±2.65 mV vs 9.73±2.09 mV, P<0.01; triceps: 14.15±3.45 mV vs 11.36±2.49 mV, P<0.01).
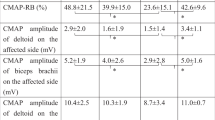
The ratio between deltoid and biceps (D/B) amplitude was 99±18%, between biceps and triceps (B/T) 88±18% and between deltoid and triceps (D/T) 86±20%. These ratios did not show age-related differences (D/B: R*2=−0.008; B/T: R*2=0.01; D/T: R*2=0.04) or gender differences (D/B: P=0.26; B/T: P=0.78; D/T: P=0.50). For each muscle, regression analysis was used to express the amplitudes as a correlation coefficient (Figures 2a and b). CMAPs amplitudes in deltoid or biceps could therefore be estimated from CMAPs amplitudes in triceps, regardless of age or gender. Normative data for CMAPs values are summarized in Table 2.
Regression analysis was used to express the amplitudes as a correlation coefficient for deltoid, biceps barchii and triceps brachii. The formulae used for this were: (a) biceps brachii amplitude B=triceps brachii amplitude (T) × 0.62+3.02 mV (R*2=0.57), (b) deltoid amplitude D=T × 0.46+4.68 mV (R*2=0.46) (R*2, the coefficient of determination adjusted for degree of freedom).
Magnetic resonance imaging
MRI showed multiple compressions in 26 patients (92.8%). Details were shown in Table 4.
CMAPs of patients with CCM
The level of conduction abnormalities was C3/4 in 16 cases and C4/5 in 12 cases by monitoring SCEPs intraoperatively. Table 3 shows the responsible level estimated from SCEPs and CMAPs amplitudes of deltoid, biceps and triceps, whereas Table 4 shows the mean CMAPs amplitude at each responsible level.
In patients with C3/4 myelopathy, the CMAPs amplitudes of deltoid were 6.82±2.33 mV (mean±s.d.) (P<0.0001) and those of biceps were 9.43±2.85 mV (P=0.10). In patients with C4/5 myelopathy, the CMAPs amplitudes of deltoid were 8.52±3.34 mV (P=0.11) and those of biceps were 8.75±4.42 mV (P=0.015). There were no statistically significant differences between the mean CMAPs amplitudes in triceps of C3/4 (P=0.89) or C4/5 (P=0.97) myelopathy patients and the normal values.
The most discriminative cutoff value for CMAPs amplitudes in the deltoid for the diagnosis of C3/4 myelopathy was 8.73 mV, giving an area under the curve value of 0.671 (95% confidence interval, 0.44–0.90). This resulted in a sensitivity of 87.5%, specificity of 57.3%, PPV of 73.2% and NPV of 77.5%. The most discriminative cutoff value using the index for diagnosis of C3/4 myelopathy was 0.52, with an area under the curve value of 0.750 (95% confidence interval, 0.55–0.95) and a sensitivity of 75.0%, specificity of 75.0%, PPV of 80.0% and NPV of 69.2% (Figure 3).
The receiver-operating characteristic (ROC) analysis was performed on the patients with C3/4 myelopathy yielded 0.75 (95% confidence interval (CI), 0.55–0.95) for an area under the curve (AUC) value for the index. (The sensitivity is 75.0% and specificity is 75.0%). CMAPs amplitude in the deltoid had 0.67 (95% CI, 0.44–0.90) for an AUC. (The sensitivity is 87.5% and specificity is 57.3%).
The most discriminative cutoff value for CMAPs amplitudes in biceps for the diagnosis of C4/5 myelopathy was 8.62 mV, giving an area under the curve value of 0.594 (95% confidence interval, 0.35–0.83) and a sensitivity of 62.5%, specificity of 75%, PPV of 73.2% and NPV of 77.5%. The most discriminative cutoff value using the index for diagnosis of C4/5 myelopathy was 0.325, with an area under the curve value of 0.646 (95% confidence interval,0.41–0.88) and a sensitivity of 75.0%, specificity of 66.7%, PPV of 62.8% and NPV of 78.1% (Figure 4).
Discussion
CMAPs amplitudes obtained by stimulating below the lesion after injury determine the degree of axonal loss and thus allow for an accurate assessment of prognosis.8 However, we reported that small CMAP amplitudes indicated not only the involvement of ventral nerve roots but also that of anterior horns with proximal-type cervical spondylotic amyotrophy.3 Ito et al.9 reported a common pattern for lesion progression in cervical spondylotic myelopathy that involved initial atrophy and neuronal loss in the anterior horn and intermediate zone, followed by degeneration of the lateral and posterior funiculus. MN-SCEPs are mediated by the lateral part of posterior columns, TES-SCEPs by the lateral corticospinal tract and spinal-SCEPs by medial parts of the posterior columns.10 In the current patient series all SCEPs showed abnormalities, thus indicating the involvement of anterior horns. Small CMAPs amplitudes corresponding to compressed cord segments (deltoid, C3/4 and biceps, C4/5) also showed involvement of the anterior horns, but could not detect the involvement of the long tract. We confirmed that CMAPs amplitudes were better suited for assessing involvement of the anterior horns.
Level diagnosis for CCM is performed by investigating the muscle weakness, deep tendon reflex and sensory disturbance. The sensitivity of muscle weakness tends to be low, but its specificity is high,11 such that muscle weakness is not detected in mild cases. Cadaver dissection has revealed a close correlation between anterior horns and vertebral bodies;12 however, the anatomical features make it difficult to give a level diagnosis for CCM. In this respect, muscle weakness resulting from involvement of the anterior horn would be more accurate than sensory disturbance from the posterior horn. The accuracy of level diagnosis using CMAPs was about 70% and it is equivalent to the result of previous reports.11 However, we confirm that deltoid and biceps are innervated by both C5 and C6 motor segments and these have dominance to innervate muscles, it is difficult to clearly discriminate the nerve domination of C5 and C6. Therefore, it would also be difficult to clearly discriminate between C3/4 myelopathy and C4/5 myelopathy through the monitoring of CMAPs amplitudes. This point is included as the limitations of our study.
Sharrard13 reported from a study of cadavers with poliomyelitis that more than 40% of anterior horn cells maintained normal muscle strength. If more than 60% of the anterior horn cells were involved this lead to muscle weakness. Patients with a single responsible level of myelopathy do not show clinical muscle weakness because multiple anterior horns innervate the muscle. Small CMAPs amplitudes could indicate subclinical muscle weakness and implicate the involvement of anterior horns in a quantitative manner.
Wee14 reported that there are good correlation between the CMAPs amplitudes and the muscle bulk in biceps. Therefore, CMAPs amplitudes show considerable individual variation as well as gender and age differences. However, side to side differences in the same individual are much smaller.15 The distribution of muscle volume in the upper limb was highly conserved across normal subjects, as assessed by MRI.16 The conserved distribution of muscle volume probably accounts for the correlation of CMAPs amplitudes among the muscles of the upper extremity. The correlations among CMAPs amplitudes for deltoid, biceps and triceps in the same individual may be explained as follows. When CMAPs amplitudes are higher or lower than normal values in patients with large or small muscle volumes, they would be determined as false negative or false positive. The index we designed was therefore more accurate than CMAPs amplitudes, regardless of patient age or gender.
With advancing age, MRI tends to show multiple compression but the responsible level shifts from C5/6 to C3/4 or C4/5.17 Elderly patients with cervical spondylotic myelopathy show multiple cord compression on MRI, but SCEPs usually showed a single level of conduction block and 95% of focal conduction block at the C3/4 or C4/5 level.18 Azuma et al.19 reported that 78% of patients with cervical ossification of the posterior longitudinal ligament were determined by SCEPs to have a single site of conduction abnormalities and in about 70% the level was C3/4 or C4/5; however, they found multiple cord compression. These reports indicate multiple compression of the spinal cord on radiographic findings can include clinically silent compression. In our series, however, we evaluated only those patients with a single site of conduction abnormalities in the C3/4 and C4/5, as this has the most clinical relevance.
Conclusion
We have investigated 28 patients with CCM at the C3/4 and C4/5 intervertebral levels as determined by SCEPs. We suggest that small CMAPs amplitudes in the deltoid indicate a C3/4 level of myelopathy and in biceps at the C4/5 level. This study could help exclude clinically silent cord compression and determine the surgical procedure to the suitable level of concern.
Data Archiving
There were no data to deposit.
References
Satomi K, Okuma T, Kenmotsu K, Nakamura Y, Hirabayashi K . Level diagnosis of cervical myelopathy using evoked spinal cord potentials. Spine 1988; 13: 1217–1224.
Shinomiya K, Furuya K, Sato R, Okamoto A, Kurosa Y, Fuchioka M . Electrophysiologic diagnosis of cervical OPLL myelopathy using evoked spinal cord potentials. Spine 1988; 13: 1225–1233.
Imajo Y, Kato Y, Kanchiku T, Suzuki H, Taguchi T . Pathology and prognosis of proximal-type cervical spondylotic amyotrophy: New assessment using compound muscle action potentials of deltoid and biceps brachii muscles. Spine 2011; 36: E476–E481.
Kaneko K, Kawai S, Taguchi T . Correlation between spinal cord compression and abnormal pattern of median nerve somatosensory evoked potentials on compressive cervical myelopathy: common of surface and epidurally recorded response. J Neurol Sci 1998; 158: 193–202.
Kanchiku T, Taguchi T, Kaneko K, Fuchigami Y, Yonemura H, Kawai S . A correlation between magnetic resonance imaging and electrophysiological findings in cervical spondylotic myelopathy. Spine 2001; 26: 269–274.
Kaneko K, Taguchi T, Kawai S . Mechanism of postoperative C5 paralysis in cervical myelopathy: An investigation based on nerve root distribution to the deltoid and biceps brachii muscles. Rinsyo Seikei Geka 2003, 383–387.
Yonemura H, Kaneko K, Taguchi T, Fujimoto H, Toyoda K, Kawai S . Nerve root distribution of deltoid and biceps brachii muscle in cervical spondylotic myelopathy: A potential risk factor for postoperative shoulder muscle weakness after posterior decompression. J Orthop Sci 2004; 9: 540–544.
Kuntzer T, Melle G, Regli F . Clinical and prognostic feature in unilateral femoral neuropathies. Muscle Nerve 1997; 20: 205–211.
Ito T, Oyanagi K, Takahashi H, Takahashi HE, Ikuta F . Cervical sponsylotic myelopathy, clinicophathologic study on the progression pattern and thin myelinated fibers on the lesion of seven patients examined during complete autopsy. Spine 1996; 21: 827–833.
Imajo Y, Kato Y, Yonemura H, Kanchiku T, Suzuki H, Taguchi T . Relative vulnerability of various spinal tracts in C3-4 cervical spomdylotic myelopathy: multi-modal spinal cord evoked potentials. Spinal cord 2011; 49: 1128–1133.
Seichi A, Takeshita K, Kawaguchi H, Matsudaira K, Higashikawa A, Ogata N et al. Neurologic level diagbosis of cervical stenotic myelopathy. Spine 2006; 31: 1338–1343.
Tsuzuki N, Honda H, Tanaka Y . Morphological variation of human cervical spine cord segments and roots and their clinical significance. Orthop Surg 1983; 34: 329–335.
Sharrard WJW . The distribution of the permanent paralysis in the lower limb in poliomyelitis. A clinical and pathological study. J Bone Joint Surg(Br) 1955; 37: 540–558.
Wee AS . Correlation between the biceps brachii muscle bulk and the size of its evoked compound muscle action potentials. Electromyogr Clin Neurophysiol 2006; 46: 79–82.
Tani T, Kishimoto H, Tsuboya H, kimura J . Electrophysiologic assessment of shoulder girdle weakness in patients with cervical spondylosis: prognostic value of supraclavicular stimulation. J Clin Neuromusc Dis 2002; 4: 11–18.
Holzbaur KR, Murray WM, Gold GE, Delp SL . Upper limb muscle volumes in adult subjects. J Biomech 2007; 40: 742–749.
Tani T, Ushida T, Taniguchi S, Kimura J . Age related shift in the primary sites of involvement in cervical spondylotic myelopathy from lower to upper levels. J Neurol Neurosurg Psychiatry 2002; 73: 316–318.
Tani T, Yamamoto H, Kimura J . Cervical spondylotic myelopathy in elderly people: a high incidence of conduction block at C3-4 or C4-5. J Neurol Neurosurg Psychiatry 1999; 66: 456–464.
Azuma Y, Kato Y, Taguchi T . Etiology of cervical myelopathy induced by ossification of the posterior longitudinal ligament. Determining the responsible level of OPLL myelopathy by correlating static compression and dynamic factor. J Spinal Disord Tech 2010; 23: 166–169.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Funaba, M., Kanchiku, T., Imajo, Y. et al. Preoperative diagnosis of the responsible level in CCM using CMAPs: comparison with SCEPs. Spinal Cord 52, 191–196 (2014). https://doi.org/10.1038/sc.2013.149
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.149
Keywords
This article is cited by
-
Resting-state functional magnetic resonance imaging indices are related to electrophysiological dysfunction in degenerative cervical myelopathy
Scientific Reports (2024)
-
Preoperative factors that predict fair outcomes following surgery in patients with proximal cervical spondylotic amyotrophy. A retrospective study
Spinal Cord (2020)