Abstract
We aimed to investigate the association between pulse rate variability (PRV) and health-related quality of life (HRQOL) in the general population. A cross-sectional study was conducted with 5908 Japanese men and women aged 30–79 years. PRV was assessed at rest using 5-min recordings of pulse waves with a photoplethysmographic signal from a fingertip sensor, and the time and frequency domains of PRV were determined. HRQOL was assessed with the Short Form-8 (SF-8) Japanese version, and poor HRQOL was defined as an SF-8 sub-scale score < 50. A test for nonlinear trends was performed with the generalized additive model with a smoothing spline adjusted for confounders. The lowest multivariable-adjusted odds ratios for poor physical component score were found in those who had second or third quartile levels of standard deviation of normal-to-normal intervals (SDNN) and root mean square of successive difference (RMSSD), and high-frequency (HF) power and trended slightly upward in the higher levels. PRV-derived parameters were nonlinearly associated with poor physical component scores. In conclusion, reduced PRV-derived SDNN, RMSSD and HF power were associated with poor HRQOL in the domain of physical function. Higher levels of these parameters did not necessarily translate into better HRQOL.
Similar content being viewed by others
Introduction
Health-related quality of life (HRQOL) is measured as an outcome for chronic disease and medical evaluations in clinical settings and has been measured in the general population1,2. HRQOL scores consist of physical and mental components and are decreased in individuals with low physical activity3, insomnia4, diabetes5, and hypertension6. Furthermore, poor self-rated health, which is one of the domains of HRQOL7, strongly predicts mortality and major outcomes8,9,10.
Heart rate variability (HRV) parameters are indicators of autonomic nervous system function11. These indicators represent sympathetic and parasympathetic nervous system activity and balance, and cohort studies have reported that autonomic nervous system dysfunction increases the risk of mortality12 and is an independent risk factor for incident diabetes13,14 and cardiovascular disease15,16. Alternatively, a systematic review found that increases in levels of endocrine hormones, such as cortisol, and decreases in HRV were biomarkers of psychological stress, with various studies showing an association between workplace stressors and HRV17.
Pulse rate variability (PRV) has been used as a potential surrogate marker of HRV and is measured with photoplethysmography. A review of studies that compared photoplethysmography with electrocardiography found that PRV accurately reflects HRV conditions for healthy subjects when measured at rest18. However, some studies indicated that PRV did not agree with the results from HRV under certain conditions, such as body posture and exercise, suggesting that PRV may be a useful biomarker distinct from HRV19. In line with this, a recent review has suggested that it would be difficult to assume that PRV is a validated surrogate for HRV, rather that HRV may reflect another aspect of cardiovascular dynamics20.
Poor HRQOL is usually explained by mental and physical conditions in individuals suffering from chronic diseases or stressors as a whole2. Consequently, poor HRQOL is associated with an increased risk of mortality and other major outcomes10. However, the biological mechanisms by which poor HRQOL influences these outcomes have not been established21.
Some studies have demonstrated an association between HRV and HRQOL in patients with functional somatic syndrome22, intellectual disabilities23, and elderly individuals with cognitive impairment24. Another study reported an association between HRV and HRQOL in 329 healthy volunteers aged 20–54 years and found that poor HRQOL in the physical domain was associated with a reduction in HRV25. Nonetheless, evidence from the general population is limited.
Although there is some debate as to whether the PRV-derived parameters reflect autonomic function or another circulatory dynamics, previous studies that applied PRV in several settings suggested that PRV-derived parameters represent some aspects of health status20. Therefore, the purpose of this study was to examine the relationship between these indices and HRQOL in the general population.
Methods
Study subjects
We enrolled 6013 men and women, 30–79 years of age, who lived in Ozu and Toon Cities in Ehime prefecture, Japan, from 2009 to 2012 and 2014–2018 (Toon City only). Both cities are in rural areas of Shikoku Island Japan. We excluded subjects who did not have a PRV examination (n = 33) and who had atrial fibrillation on an electrocardiogram (ECG) (n = 37). After the exclusion of those who did not respond to the HRQOL questionnaire (n = 36), 5908 individuals remained and were included in the analysis.
This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants. The study protocol was approved by the Human Ethics Review Committee of the Faculty of Medicine, Oita University (approval number, 2114).
Measurements
Blood pressure was measured twice with an automatic sphygmomanometer (BP-103iII; OMRON Colin Co., Tokyo, Japan) with the subject in the sitting position after a rest of at least 5 min. We used the mean of the two measurements for the analysis. The use of antihypertensive drugs was ascertained by questionnaire. Diabetes was defined as hemoglobin A1c (HbA1c) ≥ 6.5% or current use of anti-diabetes agents. HbA1c was measured with high-performance liquid chromatography (Ozu City) and the immunoagglutination inhibition method (Toon City). Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared.
HRQOL was assessed with the Short Form-8 (SF-8) Japanese version questionnaire1, which consists of eight subscales—general health (GH), physical functioning (PF), role physical (RP), bodily pain (BP), vitality (VT), social functioning (SF), mental health (MH), and role emotional (RE)—and two summary scores—the physical component score (PCS), which consists of GH, PF, RP, and BP and the mental component score (MCS), which consists of VT, SF, MH, and RE. All subscales and summary scores were standardized in the general Japanese population (mean = 50 and standard deviation = 10). In the present study, poor HRQOL was defined as a score of less than 50 for each subscale and summary score.
A self-administered questionnaire was used to assess medical history (heart disease, stroke, and kidney disease), smoking habits (≥ 20 cigarettes/day, 1–19 cigarettes/day, past smoker, and never smoker), regular alcohol drinking, exercise habits, and sleep duration. Current smokers were defined as individuals who had smoked 100 cigarettes in their lifetime and who currently smoked cigarettes. Exercise was defined as doing continuous sports or physical exercise ≥ 2 times/week during the year. Unhealthy sleep duration was defined as < 6-h or ≥ 9-h of sleep per day26.
Assessment of autonomic function
Analysis of PRV was performed with the TAS9 device (YKC Co. Ltd, Japan) and its software to assess cardiac autonomic control. The pulse rate was recorded for 5 min with a fingertip pulse wave sensor using a photoplethysmographic signal. The sensor was attached to the index finger, with the subject in the sitting position after a rest of at least 5 min, with the software filtering out arrhythmias and artifacts. Filtering was based on the Butterworth bandpass filter method to detect the normal-to-normal intervals accurately27. The five-minute PRV measurement procedure, including PRV indices and standardization, was based on the recommendation of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology28. The Task Force recommends appropriate HRV parameters in the time and frequency domains and states that five-minute recordings with a stationary system are preferable. The sampling frequency for all recordings was 1000 Hz. PRV obtained from the fingertip pulse wave sensor is comparable with that of an ECG signal29.
All PRV assessments were done between 10:00 am and 12:00 pm to control for daily variation. We maintained a comfortable room temperature with air conditioners. Participants were required to have at least a five-minute rest before the measurement. The TAS9 software-provided resting heart rate (RHR) was expressed as beats per minute (bpm), and the following time-domain measures of PRV were then determined: standard deviation of normal-to-normal intervals (SDNN), root mean square of successive difference (RMSSD), and percentage differences between normal NN intervals > 50 ms (pNN50). PRV in the frequency domain was calculated using the fast Fourier Transform with a sample rate of 3 Hz. The area under the curve fitted by the power spectral density was measured for the frequency bands of low-frequency (LF) power (0.04–0.15 Hz) and high-frequency (HF) power (0.15–0.40 Hz).
In general, SDNN reflects the total modulation of autonomic function, while RMSSD and pNN50 reflect vagal control of the heart. LF power reflects both sympathetic and parasympathetic stimulation of the heart, and HF power reflects vagal activity28.
Although PRV-derived parameters were determined based on five-minute recordings, we confirmed that they were significantly correlated with those provided by 24-h Holter ECG assessment30.
Statistical analysis
Because of their skewed distribution, SDNN, RMSSD, LF power, and HF power were log-transformed before analysis. An analysis was also carried out to measure differences in the means of age, BMI, RHR, systolic blood pressure (SBP), and the proportions of men and women, subjects with hypertension, diabetes, smoking, regular alcohol drinking, regular exercise, unhealthy sleep duration, and medical history, grouped by PCS and MCS (poor versus good conditions). The differences between groups were tested with a t-test or chi-square test. While stratified by community, we created a sex and age-adjusted model, and a multivariable model including covariates, i.e., BMI (continuous), hypertension (Yes or No), diabetes (Yes or No), smoking (≥ 20 cigarettes, 1–19 cigarettes, past smoker, and never smoker), regular alcohol drinking (Yes or No), regular exercise (Yes or No), unhealthy sleep duration (Yes or No), and medical history (Yes or No) and to estimate odds ratios (ORs) and 95% confidence intervals (Cis) for poor HRQOL. Trend tests were performed in the two models with linear or quadratic equations for a linear or nonlinear trend test, respectively. To illustrate the nonlinear trends of lnSDNN, lnRMSSD, lnLF power, and lnHF power for poor HRQOL, the generalized additive model (GAM) with a smoothing spline [degree of freedom = 3] was adopted in the logistic regression model31, adjusting for covariates in the multivariable-adjusted model. Statistical significance was assumed at P < 0.05. All statistical analyses were performed with SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
Table 1 shows the comparison of variables for cardiovascular risk factors and lifestyle between groups with poor and good PCS and MCS. The mean age was higher in the poor PCS group and lower in the poor MCS group. Individuals in the poor PCS group had higher means or percentages of BMI, SBP, diabetes, anti-hypertensive drug use, and medical history. PRV-derived parameters were significantly lower in the poor PCS group except for RMSSD. On the other hand, the poor MCS group had lower levels of BMI and SBP, and a significant difference in PRV-derived parameters between groups was not seen. The percentage of subjects with regular exercise habits was significantly lower in both the poor PCS and MCS groups compared with the good PCS and MCS groups, and that of subjects with unhealthy sleep duration was significantly higher in both the poor PCS and MCS groups compared with the good PCS and MCS groups.
Sex- and age-adjusted ORs and 95% CIs for poor HRQOL subscales according to quartile of PRV parameter (as referenced to the lowest quartile) and results of linear and nonlinear tests are presented (S1 and S2 Tables). ORs of RHR for subjects with the poor GH, PF, RP, and VT increased linearly, and the OR of RHR for 80 + bpm versus < 60 bpm in individuals with poor VT increased to 1.56 (95% CI 1.29–1.89). The association between SDNN and poor GH, PF, RP, VT, SF, and RE showed a significant nonlinear trend rather than a linear trend. Similarly, for RMSSD, LF power, and HF power, there were significant nonlinear trends toward the poor SF-8 subscale groups.
Tables 2 and 3 show multivariable-adjusted ORs and 95% CIs and results of linear and nonlinear trend tests after multivariable adjustment. The linear association between RHR; and poor GH, PF, RP, and VT remained significant after adjustment for covariates. Nonlinear trends in SDNN, RMSSD, and HF power were found for poor GH, PF, and RP. The nonlinear trends in SDNN, RMSSD, LF power, and HF power for poor VT weakened consistently; however, the ORs of RMSSD and HF power and the nonlinear trends remained significant.
Regarding the summary component of PCS and MCS, SDNN, RMSSD, and HF parameters were associated with poor PCS in nonlinear manners (Table 4). On the other hand, the associations were not clear for poor MCS.
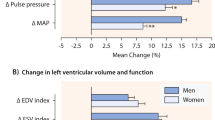
The associations between SDNN, RMSSD, and HF power; and the summary components of SF-8 were illustrated using GAM for nonlinear trends (Fig. 1). The spline lines for poor PCS increased in those who had lower SDNN, RMSSD, and HF power conditions and trended slightly upward in the higher levels. The nonlinear trends were all significant (P for nonlinear trend: 0.040 for SDNN, 0.036 for RMSSD, and 0.019 for HF power). On the contrary, the effect on poor MCS was almost even across the levels of PRV-derived parameters.
Associations between SDNN, RMSSD, and HF power; and the summary components of SF-8 using the generalized additive model with a smoothing spline [degree of freedom = 3]. Covariates included variables of sex, age, community, BMI, hypertension, diabetes, smoking, regular alcohol drinking, regular exercise, unhealthy sleep duration, and medical history. PCS physical component score, MCS mental component score, SDNN standard deviation of the normal-to-normal intervals, RMSSD root mean square of the successive differences of NN intervals, and HF high-frequency.
Discussion
We found that PRV-derived parameters, such as SDNN, RMSSD, and HF power were associated with poor HRQOL on the GH, PF, RP, VT, and SF subscales of the SF-8. Factors related to the PCS were more strongly associated compared with those related to the MCS. The association was robust after adjustment for several confounders. RHR was positively correlated with a decrease in HRQOL, mainly represented by GH, PF, and VT. GAM suggested that the relationship between PRV-derived parameters and poor PCS was nonlinear.
Following the interpretation of HRV parameters, SDNN represents overall autonomic function, and RMSSD and HF power reflect parasympathetic regulation, but caution should be used in the interpretation of PRV-derived parameters. We measured resting PRV in participants from the general population. The accuracy of PRV measurements has been reviewed18, and PRV was found to be sufficiently accurate as a measure of HRV when measured at rest in healthy subjects. A five-minute measurement of PRV (LF power, HF power, LF/HF ratio) in the present study was moderately correlated with the measurement given from 24-h recordings of HRV30. Nevertheless, it is possible that PRV represents the different cardiovascular dynamics than HRV, and further research is needed, including research in relation to autonomic function20. Whereas the SF-8 could evaluate HRQOL related to both physical and mental health. HRQOL often decreases due to physical or mental stresses5,32 and socioeconomic status33.
Although we analyzed our data with a multivariable-adjusted model, including BMI, hypertension, diabetes, smoking, regular alcohol drinking, regular exercise, unhealthy sleep duration, and medical history, these factors did not attenuate the association. This implied that the association was not explained only by the confounders which strongly affect both PRV-derived parameters and HRQOL.
The SF-8 Japanese version was developed as a short version of the SF-362 and the two versions are comparable34. Although the two summary scores are classified into the physical and mental aspects, GH and VT were interpreted to be involved with both physical and mental conditions2. SF, MH, and RE, which mainly comprise the MCS, also showed a trend toward lower ORs with some higher PRV-derived parameters. Thus, we could not deny the association of poor HRQOL with psychological causes. Vital exhaustion, a psychological stressor, has been associated with decreased SDNN and LF power35. PRV-derived parameters might be influenced by psychological factors, probably leading to a decline in self-rated health as represented in the GH or VT subscales.
Of note, for some PRV-derived parameters, higher values were not preferable for HRQOL for reasons that are not well understood. Higher HRV was associated with abnormal heart rate patterns in the elderly which increased the mortality risk36. In the present study, individuals with atrial fibrillation on ECG were excluded; thus, this effect was not considered. When values of PRV-derived parameters are very high, physicians should detect some of the causes for lower self-rated health.
Given the well-established link between socioeconomic inequalities and health, the association between PRV and HRQOL may be confounded or mediated by the socioeconomic status or underlying chronic diseases, which we could not access. Socioeconomic status affected psychological stress assessed by depressed HRV conditions37, though it will also be required to examine the association using PRV-derived parameters.
Although we analyzed a large population to determine an association between PRV and HRQOL in Japan, several limitations should be mentioned. First, we did not have information on socioeconomic status, such as work, income, and education. Indeed, socioeconomic status affects HRV parameters as a stressor and affects HRQOL33. Second, we could not identify the various kinds of illnesses the participants may have had or the medications they were taking, and that possibly influenced PRV. Third, a causal relationship between PRV-derived parameters and HRQOL scores could not be determined, because a possible bi-directional impact was considered in this cross-sectional study. A longitudinal study is needed to investigate this relationship. Finally, a variety of reasons may explain the difference from HRV, including the effect of pulse wave noise, the measurement position, and the location of the measurement sensor20. In particular, the pre-processing techniques, including the method of removing noise in the pulse wave signal, are dependent on the measurement device, and the lack of standardization is a major issue.
In conclusion, reduced PRV-derived SDNN, RMSSD and HF power were associated with poor HRQOL in the domain of physical function. Higher levels of these parameters did not necessarily translate into better HRQOL. Data suggest that maintaining PRV-derived parameters in the range indicated as the second or third quartile of PRV-derived parameters is important for good HRQOL. PRV measurement is a useful and non-invasive tool to assess an individual’s perceived health.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Tokuda, Y. et al. Assessing items on the SF-8 Japanese version for health-related quality of life: A psychometric analysis based on the nominal categories model of item response theory. Value Health 12, 568–573. https://doi.org/10.1111/j.1524-4733.2008.00449.x (2009).
Fukuhara, S., Ware, J. E. Jr., Kosinski, M., Wada, S. & Gandek, B. Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J. Clin. Epidemiol. 51, 1045–1053. https://doi.org/10.1016/s0895-4356(98)00096-1 (1998).
Dugan, S. A. et al. The impact of physical activity level on SF-36 role-physical and bodily pain indices in midlife women. J. Phys. Act. Health 6, 33–42. https://doi.org/10.1123/jpah.6.1.33 (2009).
Sasai, T. et al. Effects of insomnia and sleep medication on health-related quality of life. Sleep Med. 11, 452–457. https://doi.org/10.1016/j.sleep.2009.09.011 (2010).
Saito, I. et al. Impact of diabetes on health-related quality of life in a population study in Japan. Diabet. Res. Clin. Pract. 73, 51–57. https://doi.org/10.1016/j.diabres.2005.11.015 (2006).
Kitaoka, M. et al. The relationship between hypertension and health-related quality of life: Adjusted by chronic pain, chronic diseases, and life habits in the general middle-aged population in Japan. Environ. Health Prev. Med. 21, 193–214. https://doi.org/10.1007/s12199-016-0514-6 (2016).
Parra, D. C. et al. Perceived and objective neighborhood environment attributes and health related quality of life among the elderly in Bogota, Colombia. Soc. Sci. Med. 70, 1070–1076. https://doi.org/10.1016/j.socscimed.2009.12.024 (2010).
Tsai, S. Y., Chi, L. Y., Lee, C. H. & Chou, P. Health-related quality of life as a predictor of mortality among community-dwelling older persons. Eur. J. Epidemiol. 22, 19–26. https://doi.org/10.1007/s10654-006-9092-z (2007).
Nilsson, E., Festin, K., Lowen, M. & Kristenson, M. SF-36 predicts 13-year CHD incidence in a middle-aged Swedish general population. Qual. Life Res. 29, 971–975. https://doi.org/10.1007/s11136-019-02362-y (2020).
Friedman, E. M. & Teas, E. Self-rated health and mortality: Moderation by purpose in life. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph20126171 (2023).
Goldberger, J. J., Arora, R., Buckley, U. & Shivkumar, K. Autonomic nervous system dysfunction: JACC focus seminar. J. Am. Coll. Cardiol. 73, 1189–1206. https://doi.org/10.1016/j.jacc.2018.12.064 (2019).
Jarczok, M. N. et al. Heart rate variability in the prediction of mortality: A systematic review and meta-analysis of healthy and patient populations. Neurosci. Biobehav. Rev. 143, 104907. https://doi.org/10.1016/j.neubiorev.2022.104907 (2022).
Carnethon, M. R., Golden, S. H., Folsom, A. R., Haskell, W. & Liao, D. Prospective investigation of autonomic nervous system function and the development of type 2 diabetes: The atherosclerosis risk in communities study, 1987–1998. Circulation 107, 2190–2195. https://doi.org/10.1161/01.CIR.0000066324.74807.95 (2003).
Saito, I. et al. Role of insulin resistance in the association between resting heart rate and type 2 diabetes: A prospective study. J. Diabet. Compl. 36, 108319. https://doi.org/10.1016/j.jdiacomp.2022.108319 (2022).
Wulsin, L. R., Horn, P. S., Perry, J. L., Massaro, J. M. & D’Agostino, R. B. Autonomic imbalance as a predictor of metabolic risks, cardiovascular disease, diabetes, and mortality. J. Clin. Endocrinol. Metab. 100, 2443–2448. https://doi.org/10.1210/jc.2015-1748 (2015).
Weinstein, G., Davis-Plourde, K., Beiser, A. S. & Seshadri, S. Autonomic imbalance and risk of dementia and stroke: The framingham study. Stroke 52, 2068–2076. https://doi.org/10.1161/STROKEAHA.120.030601 (2021).
Chandola, T., Heraclides, A. & Kumari, M. Psychophysiological biomarkers of workplace stressors. Neurosci. Biobehav. Rev. 35, 51–57. https://doi.org/10.1016/j.neubiorev.2009.11.005 (2010).
Schafer, A. & Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 166, 15–29. https://doi.org/10.1016/j.ijcard.2012.03.119 (2013).
Yuda, E. et al. Pulse rate variability: A new biomarker, not a surrogate for heart rate variability. J. Physiol. Anthropol. 39, 21. https://doi.org/10.1186/s40101-020-00233-x (2020).
Mejia-Mejia, E., May, J. M., Torres, R. & Kyriacou, P. A. Pulse rate variability in cardiovascular health: A review on its applications and relationship with heart rate variability. Physiol. Meas. 41, 07TR01. https://doi.org/10.1088/1361-6579/ab998c (2020).
Jylha, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 69, 307–316. https://doi.org/10.1016/j.socscimed.2009.05.013 (2009).
Kanbara, K., Morita, Y., Hasuo, H. & Abe, T. The association between heart rate variability and quality of life in patients with functional somatic syndrome and healthy controls. Appl. Psychophysiol. Biofeedback 46, 279–285. https://doi.org/10.1007/s10484-021-09515-1 (2021).
Meule, A. et al. Quality of life, emotion regulation, and heart rate variability in individuals with intellectual disabilities and concomitant impaired vision. Psychol. Well-Being: Theory Res. Pract. 3, 1. https://doi.org/10.1186/2211-1522-3-1 (2013).
Kim, D. et al. Association between health-related quality of life and heart rate variability in elderly individuals with cognitive impairment in Korea: Cross-sectional study. BMC Geriatr. 23, 847. https://doi.org/10.1186/s12877-023-04529-2 (2023).
Lu, W. C. et al. Correlation between health-related quality of life in the physical domain and heart rate variability in asymptomatic adults. Health Qual Life Outcomes 14, 149. https://doi.org/10.1186/s12955-016-0555-y (2016).
Andreasson, A., Axelsson, J., Bosch, J. A. & Balter, L. J. Poor sleep quality is associated with worse self-rated health in long sleep duration but not short sleep duration. Sleep Med. 88, 262–266. https://doi.org/10.1016/j.sleep.2021.10.028 (2021).
Kim, J. K. & Ahn, J. M. Digital IIR filters for heart rate variability: A comparison between butterworth and elliptic filters. Eng. Med. Comput. Sci. 8, 3509–3513 (2019).
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 17, 354–381 (1996).
Ahn, J. M. Heart rate variability (HRV) analysis using simultaneous handgrip electrocardiogram and fingertip photoplethysmogram. Adv. Inf. Sci. Serv. Sci. (AISS) 5, 164–170 (2013).
Saito, I. et al. Association Between heart rate variability and home blood pressure: The toon health study. Am. J. Hypertens. 31, 1120–1126. https://doi.org/10.1093/ajh/hpy100 (2018).
Benedetti, A. & Abrahamowicz, M. Using generalized additive models to reduce residual confounding. Stat. Med. 23, 3781–3801. https://doi.org/10.1002/sim.2073 (2004).
Du, R. et al. Health-related quality of life and associated factors in patients with myocardial infarction after returning to work: A cross-sectional study. Health Qual Life Outcomes 18, 190. https://doi.org/10.1186/s12955-020-01447-4 (2020).
Hemingway, H. et al. Does autonomic function link social position to coronary risk? The Whitehall II study. Circulation 111, 3071–3077. https://doi.org/10.1161/circulationaha.104.497347 (2005).
Fukuhara, S. & Suzukamo, Y. Instruments for measuring health-related quality of life: SF-8 and SF-36. Igakuno ayumi 213, 133–136 (2005).
Shah, A. S. et al. Association of psychosocial factors with short-term resting heart rate variability: The atherosclerosis risk in communities study. J. Am. Heart Assoc. 10, e017172. https://doi.org/10.1161/JAHA.120.017172 (2021).
Stein, P. K., Domitrovich, P. P., Hui, N., Rautaharju, P. & Gottdiener, J. Sometimes higher heart rate variability is not better heart rate variability: Results of graphical and nonlinear analyses. J. Cardiovasc Electrophysiol. 16, 954–959. https://doi.org/10.1111/j.1540-8167.2005.40788.x (2005).
Lampert, R., Ickovics, J., Horwitz, R. & Lee, F. Depressed autonomic nervous system function in African Americans and individuals of lower social class: A potential mechanism of race- and class-related disparities in health outcomes. Am. Heart J. 150, 153–160. https://doi.org/10.1016/j.ahj.2004.08.008 (2005).
Acknowledgements
We wish to thank the staff and participants of the Toon Health Study and Ozu Cohort II, and the municipal authorities, officers, and health professionals of both cities for their valuable contributions.
Funding
This study was supported, in part, by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (Grants-in-Aid for Research B: no. 21H03202 in 2021–2024) and AMED under Grant Number JP23rea522104.
Author information
Authors and Affiliations
Contributions
I.S.: Conceptualization, Formal Analysis, Funding Acquisition (equal), Investigation (equal), Methodology, Resources (equal), Validation, and Writing—Original Draft Preparation; K.M.: Data Curation, Investigation (equal), Funding Acquisition (equal), and Writing—Review and Editing (equal); K.Y., Y.F., Y.T. and R.K.: Investigation (equal) and Writing—Review and Editing (equal); T.K. (Ozu Cohort II) and H.O. (Toon Health Study): Project Administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saito, I., Maruyama, K., Yamauchi, K. et al. Pulse rate variability and health-related quality of life assessment with the Short Form-8 Japanese version in the general Japanese population. Sci Rep 14, 4157 (2024). https://doi.org/10.1038/s41598-024-54748-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54748-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.