Abstract
Mismatch negativity (MMN) is an event-related potential (ERP) component generated when an unexpected deviant stimulus occurs in a pattern of standard stimuli. Several studies showed that the MMN response to both auditory and visual stimuli is attenuated in schizophrenia. While previous studies investigated auditory and visual MMN in different cohorts, here we examined the potential clinical utility of MMN responses to auditory and visual stimuli within the same group of patients. Altogether 39 patients with schizophrenia and 39 healthy controls matched in age, gender, and education were enrolled. We recorded EEG using 64 channels in eight experimental blocks where we presented auditory and visual stimulus sequences. Mismatch responses were obtained by subtracting responses to standard from the physically identical deviant stimuli. We found a significant MMN response to the acoustic stimuli in the control group, whereas no significant mismatch response was observed in the patient group. The group difference was significant for the acoustic stimuli. The 12 vane windmill pattern evoked a significant MMN response in the early time window in the control group but not in the patient group. The 6 vane windmill pattern evoked MMN only in the patient group. However, we found no significant difference between the groups. Furthermore, we found no correlation between the clinical variables and the MMN amplitudes. Our results suggest that predictive processes underlying mismatch generation in patients with schizophrenia may be more affected in the acoustic compared to the visual domain. Acoustic MMN tends to be a more promising biomarker in schizophrenia.
Similar content being viewed by others
Introduction
Schizophrenia is a severe mental disorder, with a lifetime prevalence of 1%1. The pathomechanism is still unclear, the diagnosis is based on a clinical interview. We are still lacking a biomarker, that may help with setting up the diagnosis, and with the follow-up of the pharmacological treatment or the prevention of relapses.
Mismatch negativity (MMN) is a widely investigated event-related potential (ERP) component, elicited in sequences of visual or acoustic stimuli (standards), interspersed by infrequent (deviant) stimuli (oddball paradigm)2,3. MMN is elicited automatically, i.e., by unattended4 and task-irrelevant stimuli5. The onset of auditory MMN (aMMN) is observed from 50 ms and with a peak between 100 and 250 ms post-stimulus. Latency of visual mismatch negativity (vMMN) is usually longer. However, in both modalities the latency and amplitude varies according to the stimulus characteristics6.
MMN is studied in several psychiatric disorders. Umbricht and colleagues described that patients with major depression or bipolar disorder did not show significantly decreased MMN signal compared to matched control subjects7. Auditory MMN is impaired in bipolar disorder with psychotic features, but in a lesser extent, compared to schizophrenia. Patients with ADHD do not show significant MMN impairment, compared to healthy control subjects8. These findings indicate that MMN impairment tends to be somewhat specific to schizophrenia. Because of the easy, inexpensive and quick measurement and the robust results in schizophrenia, mismatch negativity is considered as a potential biomarker of the disorder9. Compared to other biomarker candidates (P50, N100, P300), MMN showed the greatest effect size10. Patients with reduced mismatch negativity amplitude showed a significantly worse performance on the tests of working memory, emotion recognition11 and attention/information processing12, which indicates that MMN detection is closely related to cognitive impairments in schizophrenia13,14, or is even connected to cognitive dysfunction in general15. In the last years, MMN was intensely studied in different psychiatric disorders with cognitive decline. The result show different MMN latency or amplitude in patients with cognitive impairment, such as chronic alcoholism, multiple sclerosis or Alzheimer’s disease16, which indicates that MMN could be a useful tool to understand the pathophysiology of these psychiatric disorders6. MMN impairment worsens over the course of chronic schizophrenia. These findings suggest that MMN could be useful in monitoring the progression of schizophrenia17.Acoustic MMN can be examined with duration18, pitch19, frequency or complex deviants. Deficits in acoustic mismatch negativity (aMMN) generation in schizophrenia were first reported by Shelley and colleagues20 in 1991, who used duration-deviant stimuli. Duration-deviants are candidates to be a biomarker in schizophrenia, while pitch and frequency deviants showed a smaller effect size (see the meta-analysis21, or the review22). Bodatsch and colleagues23 found reduced MMN in at-risk subjects converting to first psychosis but not in nonconverters. Furthermore, Jessen and colleagues24 described reduced MMN in first-degree relatives of patients with schizophrenia compared to controls. These findings indicate that MMN examinations might help the prediction of conversion and prevention.
Visual mismatch negativity (vMMN) can be elicited by a high variability of different stimuli such as brightness changes25, facial gender difference26, facial emotions27,28 or even simple visual stimuli29. Compared to aMMN, there are relatively few clinical trials investigating vMMN in schizophrenia2,30. Farkas and colleagues found significantly decreased MMN in patients with schizophrenia, using simple visual stimuli29. Urban and colleagues used a motion-direction paradigm to compare the mismatch (MM) signal between schizophrenia patients and control subjects. Their results showed significantly decreased MMN in the patient group31.
Functional interpretation of auditory and visual MMN is connected to the predictive coding theory4,6,32. According to this theory, the brain creates a model to interpret the sensory input and this model serves to predict the following sensory input. Based on this model, the brain calculates the difference between the prediction and the real input, and updates the model based on the prediction error. It can be hypothesized that in pathological conditions alterations in this aspect generates a maladaptive model and it can lead to hallucinations and delusion. Patients with auditory hallucinations rely more on predictions than on sensory evidence, which leads to false assumptions and psychosis33. Patients with chronic schizophrenia have rigid response pattern. While patientsc with acute unmedicated psychosis show increased tendency to update their model according to the prediction error34.
Previous pharmaceutical studies found that NMDA-receptor antagonists, such as ketamine can trigger positive, negative and cognitive symptoms of schizophrenia35. These agents also caused the decrease of the auditory MMN signal in healthy volunteers, proving the link to NMDA-receptor function36,37,38. These findings led to the glutamate hypothesis of schizophrenia, which is supported by indirect and direct evidence. Postmortem studies found decreased NMDA-receptor density in the brains of patients with schizophrenia39. According to a previous meta-analysis NMDA-modulatory drugs caused significant improvement of positive and negative symptoms in the patients when added to their treatment40. The connection between vMMN and the glutamatergic system is not as well studied as the molecular background of aMMN, however Heekeren and colleagues observed vMMN reduction after the admission of ketamine, implying the involvement of the glutamatergic system in vMMN generation38.
The α7 nicotinic cholinoceptor function and nicotine intake also influence the MMN in schizophrenia. Nicotine increases the patients’ duration MMN amplitude to a level comparable with that seen in control subjects41. Furthermore, nicotine improves sensory gating, which has positive effect on negative symptoms. The smoking rate among schizophrenia patients is higher (90%) compared to the healthy population (20–30%). This behavior can be considered as “self-medication”, because nicotine improves sensory gating, thus has a positive effect on working memory and attention deficit41. Alpha 7 nicotinic receptor agonists found to have beneficial effect in animal studies and are promising drugs to treat the cognitive and negative symptoms in schizophrenia42. The connection to the MMN can help to monitor the effect of these drugs and to find new pharmaceutical agents to treat negative symptoms of schizophrenia.
The first EEG and MEG studies located the source of auditory MMN as single dipole generators within the region of bilateral superior temporal gyri (STG) in the vicinity of the transverse (Heschl's) gyrus43,44. Shinn and colleagues described increased functional connectivity in this region in schizophrenia patients45. Salisbury and colleagues46 described that mismatch negativity is reduced in chronic but not in first-episode schizophrenia, which is correlated with the Heschl-gyrus gray matter volume. These results could be explained by the findings of Kasai and colleagues, who recorded progressive Heschl-gyrus volume reduction in schizophrenia patients47,48. Later, surface and intracranial EEG, PET and fMRI research helped us to understand MMN generators in detail. The results of these studies also suggest the involvement of the inferior frontal gyrus, medial frontal gyrus and anterior cingulate cortex49. Li and colleagues described two pathways of MMN generation: first from the auditory cortex the signal propagates to the motor areas and then from the auditory cortex to the inferior frontal gyrus50. MEG studies located visual MMN in the occipital lobe51. Previous studies recorded structural, functional and metabolic changes in the occipital lobe of patients with schizophrenia52. Previous fMRI results described the involvement of the left inferior and middle frontal gyri in vMMN generation53. Most recent theories describe, that the visual mismatch response is modulated by a fronto-occipital network54.
In summary, the generation of aMMN and vMMN is strongly connected to the primary sensory cortices,and they share a partially overlapping network in the frontal cortex , which leads us to the assumption that there might be a correlation between the two modalities, however no previous study examined MMN generation in schizophrenia in both modalities.
Based on the above results, we hypothesize that patients with schizophrenia would show decreased auditory MMN over the central and frontal and decreased visual MMN at the occipital and frontal regions compared to neurotypicals. In addition, we expect a negative effect of symptom severity and antipsychotic dose and a positive effect of nicotine intake on MMN amplitudes. An exploratory part of the study was to investigate if auditory or visual MMN is more sensitive to diagnosis.
Methods and materials
Ethical statement
The study was approved by the Scientific and Research Ethics Committee of the Medical Research Council, Budapest, Hungary, and participants gave their written informed consent before the procedures. The experiments were carried out in full compliance with the Helsinki Declaration.
Subjects
Altogether 39 patients with schizophrenia and 39 healthy control subjects matched in age, gender and education were enrolled to the study. Their demographic data is provided in Table 1. Selection criteria were the absence in their history of any central nervous system disorder, mental retardation, epileptic seizure and no history of head injury with loss of consciousness more than 10 min, and in addition at healthy participants, no history of psychiatric disease. All patients met the criteria for schizophrenia based on the Structural Clinical Interview for DSM IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition)55. Positive and Negative Syndrome Scale (PANSS) was evaluated by a trained psychiatrist56.
Stimuli and procedures
Both visual and acoustic stimuli were used during the experiment. The visual stimuli consisted of 6 and 12 vane windmill patterns, the same as File and colleagues used in their previous study57. The stimuli were presented with Matlab2014a and it was in the middle of the monitor. The diameter of the windmill patterns was 32.28 angular degree, their contrast was high, 37.21 cd/m2 for bright and 0.14 cd/m2 for the dark segments. The colors were defined with RGB codes, as the following: the background was [0.3 0.3 0.3], the lighter parts of the windmill patterns were described as [0.6 0.6 0.6] and the darker parts were defined with the code [0 0 0 ]. The visual stimuli were visible for 200 ms and they were followed by a 600 ms long interstimulus interval. The presented acoustic stimuli were 100 ms and 200 ms duration binaural tones with 1000 Hz frequency. The volume of the tones was set according the hearing threshold of the subjests, which was measured before the examination.
The experiment consisted of eight blocks. Each block contained a visual and an acoustic sequence, separated with a 15 s break. In each sequence 24 deviant and 125 standard, altogether 149 stimuli were presented. Altogether, during the EEG registration, 1000 visual standard and 192 visual deviant (sum of the 6 and 12 vane windmill patterns), 1000 acoustic standard and 192 acoustic deviant stimuli (sum of long and short acoustic stimuli) were presented. Deviant stimuli were distributed such that between each deviant stimuli we placed multiple standard stimuli. The number of standard stimuli between each deviant was randomly selected from the set {3,4,5,6,7}. We changed the deviant and standard stimulus in every session, so every visual and acoustic stimulus appeared four times as a deviant and four times as a standard durind the examination. This way we could remove adaptional bias. The schematic illustration of the paradigm is presented in Fig. 1. To maintain the subjects’ attention, a simple visual task was used. The subjects had to navigate a blue spaceship with the keyboard. They had to avoid the appearing red spaceships and catch the green spaceships. For more details, we refer to the article of Sulykos and colleagues58.
(a) Schematic illustration of the experimental paradigm. In the visual session, an oddball sequence of windmill patterns was presented for 200 ms followed by an inter-stimulus interval (ISI) of 600 ms. In the acoustic session, 100 and 200 ms long beeping sounds were presented, the stimuli were followed by an ISI of 600 ms. (b) The left scalp figure presents the acoustic regions of interest (green: left frontal (AF3, F5, FC5, FC3), red: frontocentral (F3, FZ, F4), blue: right frontal (AF4, F6, FC4, FC6)) the visual regions are shown in the right scalp figure (yellow:frontal(FP1, FPZ, FP2), red:left occipital (PO7, PO5, PO3), blue: midline occipital (PZ, POZ, OZ), green: right occipital (PO4, PO6, PO8)).
EEG recording and processing
EEG was recorded with a 64 channel quikcap and a Curry7XS EEG recording system. The sampling rate was 1000 Hz. For data processing, the EEGLAB toolbox of Matlab59 was used. During the preprocessing, electrodes with many artifacts caused by movement were collected and interpolated with the mean of the surrounding electrodes. A 0.3 Hz highpass and a 40 Hz lowpass filter were applied on the data. Artifacts caused by movement or speech were eliminated by the ADJUST plugin, based on Independent Component Analysis (ICA). The final data was baseline corrected and rereferred to the average potential. EEG segments under − 80 µV and above 80 µV were rejected. EEG epochs of 600 ms with 100 ms prestimulus interval were selected for further analysis. At the end of the data processing, in average 169 visual deviant (SD = 26), 877 visual standard (SD = 133), 167 acoustic deviant (SD = 26), 866 acoustic standard (SD = 142) stimuli per subject were used for further analysis in the patient group. In the control group, in average 179 visual deviant (SD = 18), 929 visual standard (SD = 97), 198 acoustic deviant (SD = 19) and 928 acoustic standard (SD = 96) stimuli remained after the data processing.
Data analysis
Mismatch negativity was calculated by subtracting the response to the standard from the physically identical deviant. We defined seven regions of interest (ROI) and the MMN amplitude was calculated as the mean amplitude inside these ROIs in the selected time window. The regions were selected according to previous studies29,60,61,62, the channels of the regions are presented on Fig. 1b. VMMN was examined in an early (160–200 ms) and a late (260–300 ms) time window, while we applied a single time window (120–200 ms) on the acoustic MMN epochs. The time windows were defined on previous study results60,61,63.
The effect of study group, ROI and their interaction on MMN amplitude was analyzed by a repeated measures mixed linear model (PROC MIXED in SAS 9.4) separately for acoustic and visual stimuli in the different time windows resulting in six different analyses altogether. Age and gender were included as covariates in all MIXED model analyses. Where the interaction of study group and ROI was significant post-hoc t comparisons were applied. Furthermore, we tested by post hoc t-tests in the mixed model if the MMN amplitude was different from zero in both study groups for all stimuli in all ROIs separately in order to detect if a mismatch signal was produced in the given group and ROI for a given stimulus. In case of post-hoc tests a Bonferroni correction for multiple comparisons were applied (level of significant p = 0.05/number of ROIs in the analysis).
Correlations between the clinical, demographical and the EEG data were analyzed by Pearson and Spearman correlations using R Studio and its packages. In the correlational analyses, also the Bonferroni correction for multiple comparisons was applied.
Results
Behavioral results
The control group was in average 77.89% successful in catching or avoiding spaceships (SD = 16.98). The patient group completed in average 69.91% of the task successfully (SD = 20.29).
Acoustic MMN
Long acoustic
The results were analyzed in the 120–200 ms time window. In the control group, a significant MMN sign was detected in all three regions (left and right frontal and frontocentral), while no mismatch sign was detected in the patient group. Accordingly, the between group difference was significant (F(1;73) = 7.5, p = 0.008) indicating a decreased MMM in patients, while region (F(2;150) = 0.7, p = 0.51) and group * region (F(2;150) = 0.1, p = 0.86) effects were non-significant. The largest effect size was found in the right frontal region (Cohen’s d = 0.54).
Short acoustic
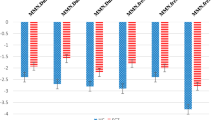
The results were analyzed in the 120–200 ms time window and the results showed a similar pattern to the short stimulus type. In the control group a significant MMN was detected in all three regions (left and right frontal and frontocentral). The MMN signal in the patient group was not significantly different from zero, analysed by a post-hoc t-test. The between group difference was significant (F(1;73) = 13.5, p = 0.0005) indicating a decreased MMN in patients, while region (F(2;150) = 1.3, p = 0.27) and group * region (F(2;150) = 0.5, p = 0.58) did not have a significant effect. This stimulus had the largest effect size among all stimuli, in the left frontal region (Cohen’s d = 0.69). The topoplots and the line plots of auditory MMN are presented in Fig. 2.
(a) Grand average ERPs and topoplots of the mismatch signal for long acoustic stimulus. The standard (red line) and the deviant stimuli (blue line), and the mismatch response (yellow line) from the three ROIs in the two study groups. The gray area shows the 120–200 ms time window. In the time windows marked with black * a significant mismatch signal was found. The blue star markes the significant different in the mismatch signal amplitude between the study groups. The topoplots show the mismatch responses in the 120–200 ms interval. (b) Grand average ERPs and topoplots of the mismatch signal for short acoustic stimulus.
Visual MMN
V6 windmill stimulus
No mismatch negativity was found (corrected p > 0.05) in the early time window (160–200 ms) in any of the study groups. In the late time window (260–300 ms) a significant vMMN was detected in the frontal and right occipital regions in patients, while no vMMN was detected in the control group. However, neither between group difference was detected, nor the region * group interaction had a significant effect on the MMN amplitude. The effect of region was significant (F(3;228) = 4.6; p = 0.004). The effect sizes were in a wide range, the smallest was calculated in the midline occipital region in the early time window (Cohen’s d = 0.04), the largest was found in the frontal region in the same time window (Cohen’s d = 0.44).
V12 windmill
VMMN was detected in the control group in all four regions (frontal, right occipital, left occipital and midline occipital) in the early time window (160–200 ms), while in the patient group a mismatch signal was only detected in the frontal region. No between group difference (F(1;73) = 2.3; p = 0.13) or group*ROI interaction (F(3;225) = 0.5, p = 0.69) was detected. The effect of region was significant (F(3;228) = 25.8; p < 0.0001). In the late time window (260–300 ms) significant MMN was detected in patients only in the frontal region, while no vMMN was detected in controls in any regions. There was no between group or inter-region difference or interaction effect. The right occipital region in the early time window showed the largest effect size (Cohen’s d = 0.26). The topoplots and the line plots of visual MMN are shown in Fig. 3.
Correlation
No significant correlation (p ≤ 0.005) was found between the demographic variables and MMN amplitude. There was no significant correlation of MMN amplitudes with chlorpromazine equivalent antipsychotic dose (p = 0.038–0.904), illness duration (p = 0.101–0.746) or PANSS scores (PANSS total score: p = 0.04–0.728, PANSS positive subscale: p = 0.047–0991, PANSS general subscale p = 0.038–0.961, PANSS negative items p = 0.13–0.602). Furthermore, no significant correlation was found between the visual and acoustic MMN amplitude in any region (p = 0.085–0.928), analyzed by Pearson correlation. The patients’ nicotine intake (cigarettes/day) shows significant correlation with the amplitude of the auditory MM signal in the frontocentral region (p = 0.004, r = − 0.46) and in the right frontal region (p = 0.005, r = − 0.45), analyzed by Spearman correlation. The results describe no significant correlation with patients’ nicotine intake and vMMN in any region (p = 0.23–0.99, r = − 0.05 to 0.2).
Discussion
This was the first investigation studying both acoustic and visual MMN on the same population of patients with schizophrenia and neurotypical control subjects.
Decreased auditory mismatch negativity was found in the patient group relative to controls independent of referencing (average or mastoid). This robust difference is consistent with previous findings64,65. While using the average reference no auditory mismach reponse was detected in the patient group, they showed a significant mismatch response after rereferencing to the average of mastoid electrodes, which produced a better signal-to-noise ratio (supplementary material). Auditory mismatch negativity (aMMN) is thought to reflect low level auditory processing. According to the predictive coding theory, the human brain tries to predict the subsequent stimulus based on the model representing previous regularity of information. An unexpected stimulus creates a prediction error, which modifies the model. In this theoretical framework, our finding, i.e., decreased auditory MMN can be interpreted as a signature of impaired predictive coding in schizophrenia. The reason of such impairment can be considered as the increased role of prediction, in comparison to the actual sensory input34.
Our results showed no significant correlation between aMMN and vMMN in any ROI, indicating that partially different brain networks are responsible for decreased acoustic and visual mismatch generation in schizophrenia. This lack of correlation could be explained by the pattern of different impairments for each person in the primary cortices responsible for acoustic and visual mismatch generations. The generators of aMMN are located in the primary acoustic sensory cortex. Previous fMRI studies described a difference in the Heschl gyrus volume and connectivity in schizophrenia, which can be the cause of the impaired acoustic stimulus processing and acoustic MMN45,47 in patients with schizophrenia. The vMMN is connected to the primary visual cortex in the occipital lobe, which also shows structural and functional impairments in schizophrenia52. Several previous studies shows the involvement of the frontal cortex in mismatch generation in both modalities50,53,54. The aMMN is found to be connected to the right prefrontal, inferior and middle frontal gyrus66,67, while the left inferior and middle frontal cortices take part in the generation of the vMMN53. A recent fMRI study by Grundei described an overlapping network , involving the inferior frontal cortex, the temporo-parietal areas and sensory cortices68. Future fMRI studies applying both vMMN and aMMN paradigms are needed to identify the common pathways of visual and acoustic mismatch generation and their impairment in schizophrenia and other neuropsychiatric disorders16. While there is strong evidence that NMDA function plays a crucial role in acoustic mismatch generation36, this link to visual mismatch generation is still unclear. Investigations administarating NMDA antagonist such as ketamine and applying vMMN paradimgs need to reveal this connection.
Though the results are controversial, glutamatergic transmission still remains a promising drug targets in schizophrenia, especially in terms of negative symptoms and cognitive deficit69,70. NMDA-receptor modulation can also be part of treatment of mood disorders or Alzheimer’s disease71,72. Our results show significant correlation between the acoustic MMN amplitude and the patients’ nicotine intake, indicating that nicotine is associated with the generation of MMN. This finding is in line with previous EEG studies showing that nicotine admission altered visual and acoustic mismatch generation compared to placebo73,74. Interestingly, these findings could not be reproduced by de la Salle et al.75, who did not find significant difference between the two study groups in the same setting. Therefore, it is still need to be clarified if the connection between the nicotinerg system and MMN generation is direct or is influenced by other social, enviromental or medical factors. Preclinical studies described that nicotine had beneficial effect on cognitive performance in schizophrenia patients76. This conclusion led to the intensive study of alpha 7 nicotinic receptor agonists as candidates for treatment of cognitive impairment42. AMMN could be helpful in monitoring the effect of these drugs.
Fisher et al.77 described a correlation between MMN amplitude and hallucinatory traits. In the present study we did not find correlation between the symptom severity and the MMN amplitude in the patient group. However, our results can be biased by the fact that we only examined patients with lower symptom severity and PANSS scores due to the need for compliance in a high density EEG experiment. We have to note here, that in our previous study29, we did not find correlations between MMN and symptom severity.
This is also the first experiment with schizophrenia patients using the windmill patterns in a vMMN paradigm. In control subjects, vMMN for the V12 windmill pattern was detected both in the frontal and occipital regions, while in patients vMMN appeared only over the frontal region, but between-group difference was not detected in visual stimuli in any regions. This pattern of result is consistent with previous studies using the same paradigm with healthy controls78. We detected vMMN in the patient group only in the late time window at the frontal region. This finding, taken together with the results of several previous studies (for a review see2) indicate that MM generation to visual stimuli also might be impaired in schizophrenia. Interestingly, the V6 windmill pattern produced a vMMN only in patients. A possible solution is suggested by File and colleagues, who obtained that V6 did not elicit vMMN in healthy participants, because this stimulus does not carry new information compared to the V12 pattern as the V12 stimulus contains the V6 pattern implicitly but not vice versa (V12 and V6 patterns were used as standard/deviant counterparts during the experiment). In other words, representation of the more complex stimulus included the representation of the less complex stimulus57. The frontal localization of the V6 mismatch negativity in patients suggest the involvement of a higher level processing mechanism, such as attention orientation and triggering53. Since we detect vMMN in both groups, it is unlikely that the lack of group difference is a result of a methodological issue in the design of our visual experiment. This view is also supported by the fact the same visual MMN paradigm was successfully applied in previous studies with similar negative results at V6 (but not V12) patterns in healthy participants.
Our results showed medium effect sizes (Cohens d = 0.46–0.69) to duration deviant auditory stimuli and small (non-significant) effect sizes to visual stimuli (Cohen’s d = 0.003–0.44). Our results are in line with previous meta-analyses describing the largest effect size (Cohen’s d = 0.79–0.88 (95% confidence interval)) for duration deviants compared to other acoustic deviant types21. The robust difference between the study groups suggests, that aMMN can be a more reliable biomarker for monitoring drug effects and drug development, than vMMN. Mismatch negativity is still a promising candidate, since MMN impairment thought to be selective to schizophrenia8,79. Previous studies found reduced MMN in at-risk subjects converting to first psychosis but not in nonconverters and even in first degree relatives of schizophrenia patients23,24. The impairment persists long term and tends to be correlated with disease progression. However, as Erickson and colleagues suggest this relationship with disease progression is not linear. The MMN impairment worsens within the first years after the diagnosis and stabilizes after the critical period has passed79.
Limitations
Because of the long EEG experiment and the need for compliance, only patients with good functioning and compliance were enrolled. Therefore, patients with high symptom severity were excluded from the research. We only examined medicated patients, however no significant correlation was found between antipsychotic medication dose (in terms of CPZ equivalent) and the amplitudes of the MMN mismatch. The demanding visual task can be a limitation of the observation of the MMN.
Conclusion
According to our results, acoustic mismatch generation tends to be impaired more in schizophrenia compared to visual mismatch generation. Therefore, aMMN is a more adequate candidate for biomarker in schizophrenia. Glutamatergic and nicotinic transmissions are still promising drug targets in schizophrenia, while MMN is connected to both NMDA and nicotinic function, which connection makes it a potential biomarker for monitoring the effect of drugs affecting these neurotransmitter systems.
Data availability
The datasets that are used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
McCutcheon, R. A., Reis-Marques, T. & Howes, O. D. Schizophrenia—an overview. JAMA Psychiat. 77(2), 201–210 (2020).
Kremláček, J. et al. Visual mismatch negativity (vMMN): A review and meta-analysis of studies in psychiatric and neurological disorders. Cortex 80, 76–112 (2016).
Näätänen, R. Mismatch negativity (MMN) as an index of central auditory system plasticity. Int. J. Audiol. 47(Suppl 2), S16-20 (2008).
Stefanics, G., Kremláček, J. & Czigler, I. Visual mismatch negativity: A predictive coding view. Front. Hum. Neurosci. 8, 666–666 (2014).
Garrido, M. I. et al. The mismatch negativity: A review of underlying mechanisms. Clin. Neurophysiol. 120(3), 453–463 (2009).
Fitzgerald, K. & Todd, J. Making Sense of Mismatch Negativity. Front. Psychiatry 11, 468–468 (2020).
Umbricht, D. et al. How specific are deficits in mismatch negativity generation to schizophrenia?. Biol. Psychiatry 53(12), 1120–1131 (2003).
Le-Sommer, J. et al. Effects of methylphenidate on mismatch negativity and P3a amplitude of initially psychostimulant-naïve, adult ADHD patients. Psychol. Med. 2021, 1–9 (2021).
Haigh, S. M., Coffman, B. A. & Salisbury, D. F. Mismatch negativity in first-episode schizophrenia: A meta-analysis. Clin. EEG Neurosci. 48(1), 3–10 (2017).
Fong, C. Y. et al. Auditory mismatch negativity under predictive coding framework and its role in psychotic disorders. Front. Psychiatry 11, 557932 (2020).
Csukly, G. et al. Emotion-related visual mismatch responses in schizophrenia: Impairments and correlations with emotion recognition. PLoS One 8(10), e75444 (2013).
Higuchi, Y. et al. Mismatch negativity and cognitive performance for the prediction of psychosis in subjects with at-risk mental state. PLoS One 8(1), e54080 (2013).
Javitt, D. C. Cognitive impairment associated with schizophrenia: From pathophysiology to treatment. Annu. Rev. Pharmacol. Toxicol. 63(1), 119–141 (2023).
Javitt, D. C. Cognitive impairment associated with schizophrenia: From pathophysiology to treatment. Annu. Rev. Pharmacol. Toxicol. 63, 119–141 (2023).
Harms, L. et al. The Role of glutamate neurotransmission in mismatch negativity (MMN), a measure of auditory synaptic plasticity and change-detection. Neuroscience 456, 106–113 (2021).
Näätänen, R. et al. The mismatch negativity: An index of cognitive decline in neuropsychiatric and neurological diseases and in ageing. Brain 134(12), 3435–3453 (2011).
Lho, S. K. et al. Progressive impairment of mismatch negativity is reflective of underlying pathophysiological changes in patients with first-episode psychosis. Front. Psychiatry 11, 587 (2020).
Jacobsen, T. & Schröger, E. Measuring duration mismatch negativity. Clin. Neurophysiol. 114(6), 1133–1143 (2003).
Haigh, S. M. et al. Mismatch negativity to pitch pattern deviants in schizophrenia. Eur. J. Neurosci. 46(6), 2229–2239 (2017).
Shelley, A. M. et al. Mismatch negativity: An index of a preattentive processing deficit in schizophrenia. Biol. Psychiatry 30(10), 1059–1062 (1991).
Avissar, M. et al. Meta-analysis of mismatch negativity to simple versus complex deviants in schizophrenia. Schizophr. Res. 191, 25–34 (2018).
Onitsuka, T. et al. Review of neurophysiological findings in patients with schizophrenia. Psychiatry Clin. Neurosci. 67(7), 461–470 (2013).
Bodatsch, M. et al. Prediction of psychosis by mismatch negativity. Biol. Psychiatry 69(10), 959–966 (2011).
Jessen, F. et al. Amplitude reduction of the mismatch negativity in first-degree relatives of patients with schizophrenia. Neurosci. Lett. 309(3), 185–188 (2001).
Sulykos, I. & Czigler, I. Visual mismatch negativity is sensitive to illusory brightness changes. Brain Res. 1561, 48–59 (2014).
Kecskés-Kovács, K., Sulykos, I. & Czigler, I. Is it a face of a woman or a man? Visual mismatch negativity is sensitive to gender category. Front. Hum. Neurosci. 7, 532 (2013).
Zhao, L. & Li, J. Visual mismatch negativity elicited by facial expressions under non-attentional condition. Neurosci. Lett. 410(2), 126–131 (2006).
Astikainen, P. & Hietanen, J. K. Event-related potentials to task-irrelevant changes in facial expressions. Behav Brain Funct. 5, 30 (2009).
Farkas, K. et al. Elementary sensory deficits in schizophrenia indexed by impaired visual mismatch negativity. Schizophr. Res. 166(1–3), 164–170 (2015).
Umbricht, D. & Krljes, S. Mismatch negativity in schizophrenia: A meta-analysis. Schizophr. Res. 76(1), 1–23 (2005).
Urban, A. et al. Visual mismatch negativity among patients with schizophrenia. Schizophr. Res. 102(1–3), 320–328 (2008).
Ruiz-Martínez, F. J., Arjona, A. & Gómez, C. M. Mismatch negativity and stimulus-preceding negativity in paradigms of increasing auditory complexity: A possible role in predictive coding. Entropy Basel 23, 3 (2021).
Kirihara, K. et al. A predictive coding perspective on mismatch negativity impairment in schizophrenia. Front. Psychiatry 11, 660–660 (2020).
Griffin, J. D. & Fletcher, P. C. Predictive processing, source monitoring, and psychosis. Annu. Rev. Clin. Psychol. 13, 265–289 (2017).
Haaf, M. et al. Glutamatergic deficits in schizophrenia—biomarkers and pharmacological interventions within the ketamine model. Curr. Pharm. Biotechnol. 19(4), 293–307 (2018).
Javitt, D. C. et al. Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: Implications for schizophrenia. Proc. Natl. Acad. Sci. U. S. A. 93(21), 11962–11967 (1996).
Umbricht, D. et al. Mismatch negativity predicts psychotic experiences induced by nmda receptor antagonist in healthy volunteers. Biol. Psychiatry 51(5), 400–406 (2002).
Heekeren, K. et al. Mismatch negativity generation in the human 5HT2A agonist and NMDA antagonist model of psychosis. Psychopharmacol. (Berl) 199(1), 77–88 (2008).
Balu, D. T. The NMDA receptor and schizophrenia: From pathophysiology to treatment. Adv. Pharmacol. 76, 351–382 (2016).
Tsai, G. E. & Lin, P. Y. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr. Pharm. Des. 16(5), 522–537 (2010).
Olincy, A. & Freedman, R. Nicotinic mechanisms in the treatment of psychotic disorders: A focus on the α7 nicotinic receptor. Handb. Exp. Pharmacol. 213, 211–232 (2012).
Martin, L. F., Kem, W. R. & Freedman, R. Alpha-7 nicotinic receptor agonists: Potential new candidates for the treatment of schizophrenia. Psychopharmacology 174(1), 54–64 (2004).
Alho, K. et al. Processing of novel sounds and frequency changes in the human auditory cortex: Magnetoencephalographic recordings. Psychophysiology 35(2), 211–224 (1998).
Scherg, M., Vajsar, J. & Picton, T. W. A source analysis of the late human auditory evoked potentials. J. Cogn. Neurosci. 1(4), 336–355 (1989).
Shinn, A. K. et al. Functional connectivity of left Heschl’s gyrus in vulnerability to auditory hallucinations in schizophrenia. Schizophr. Res. 143(2–3), 260–268 (2013).
Salisbury, D. F. et al. Progressive and interrelated functional and structural evidence of post-onset brain reduction in schizophrenia. Arch. Gener. Psychiatry 64(5), 521–529 (2007).
Kasai, K. et al. Progressive decrease of left Heschl gyrus and planum temporale gray matter volume in first-episode schizophrenia: A longitudinal magnetic resonance imaging study. Arch. Gen. Psychiatry 60(8), 766–775 (2003).
Mubarik, A. & Tohid, H. Frontal lobe alterations in schizophrenia: A review. Trends Psychiatry Psychother. 38(4), 198–206 (2016).
Takahashi, H. et al. Neural substrates of normal and impaired preattentive sensory discrimination in large cohorts of nonpsychiatric subjects and schizophrenia patients as indexed by MMN and P3a change detection responses. NeuroImage 66, 594–603 (2013).
Li, Q. et al. Single-trial EEG-fMRI reveals the generation process of the mismatch negativity. Front. Hum. Neurosci. 13, 168 (2019).
Susac, A. et al. Magnetic source localization of early visual mismatch response. Brain Topogr. 27(5), 648–651 (2014).
Tohid, H., Faizan, M. & Faizan, U. Alterations of the occipital lobe in schizophrenia. Neurosci. (Riyadh) 20(3), 213–224 (2015).
Hedge, C. et al. A frontal attention mechanism in the visual mismatch negativity. Behav. Brain Res. 293, 173–181 (2015).
Tse, C. Y. et al. Fronto-occipital mismatch responses in pre-attentive detection of visual changes: Implication on a generic brain network underlying Mismatch Negativity (MMN). Neuroimage 244, 118633 (2021).
American Psychiatry Association. DSM IV: Diagnostic and Statistical Manual of Mental Disorders Schizophrenia and Other Psychotic Disorders. In DSM 4 (pp. 297–303) (1995).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13(2), 261–276 (1987).
File, D. et al. Visual mismatch negativity (vMMN) for low- and high-level deviances: A control study. Attention Percept. Psychophys. 79(7), 2153–2170 (2017).
Sulykos, I., Kecskés-Kovács, K. & Czigler, I. Asymmetric effect of automatic deviant detection: The effect of familiarity in visual mismatch negativity. Brain Res. 1626, 108–117 (2015).
Delorme, A. & Makeig, S. EEGLAB: An open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 134(1), 9–21 (2004).
Jahshan, C. et al. Cross-diagnostic comparison of duration mismatch negativity and P3a in bipolar disorder and schizophrenia. Bipolar Disord. 14(3), 239–248 (2012).
Lazarev, I. E. et al. Feature binding in auditory modality requires attention as indexed by mismatch negativity and N2b in an active discrimination task. Neuroreport 29(4), 308–313 (2018).
Michie, P. T. What has MMN revealed about the auditory system in schizophrenia?. Int. J. Psychophysiol. 42(2), 177–194 (2001).
Kimura, M. Visual mismatch negativity and representational momentum: Their possible involvement in the same automatic prediction. Biol. Psychol. 139, 178–185 (2018).
Michie, P. T. et al. Duration and frequency mismatch negativity in schizophrenia. Clin. Neurophysiol. 111(6), 1054–1065 (2000).
Todd, J. et al. Deviant matters: Duration, frequency, and intensity deviants reveal different patterns of mismatch negativity reduction in early and late schizophrenia. Biol. Psychiatry 63(1), 58–64 (2008).
Lappe, C., Steinsträter, O. & Pantev, C. A beamformer analysis of MEG data reveals frontal generators of the musically elicited mismatch negativity. PLoS One 8(4), e61296 (2013).
Oknina, L. B. et al. Frontal and temporal sources of mismatch negativity in healthy controls, patients at onset of schizophrenia in adolescence and others at 15 years after onset. Schizophr. Res. 76(1), 25–41 (2005).
Grundei, M., Schmidt, T. T. & Blankenburg, F. A multimodal cortical network of sensory expectation violation revealed by fMRI. Hum. Brain Mapp. 44(17), 5871–5891 (2023).
Goff, D. C. Drug development in schizophrenia: Are glutamatergic targets still worth aiming at?. Curr. Opin. Psychiatry 28(3), 207–215 (2015).
Yang, A. C. & Tsai, S.-J. New targets for schizophrenia treatment beyond the dopamine hypothesis. Int. J. Mol. Sci. 18(8), 1689 (2017).
Henter, I. D., Park, L. T. & Zarate, C. A. Jr. Novel glutamatergic modulators for the treatment of mood disorders: Current status. CNS Drugs 35(5), 527–543 (2021).
Breijyeh, Z. & Karaman, R. Comprehensive review on alzheimer’s disease: Causes and treatment. Molecules 25, 24 (2020).
Baldeweg, T., Wong, D. & Stephan, K. E. Nicotinic modulation of human auditory sensory memory: Evidence from mismatch negativity potentials. Int. J. Psychophysiol. 59(1), 49–58 (2006).
Fisher, D. J. et al. Light up and see: Enhancement of the visual mismatch negativity (vMMN) by nicotine. Brain Res. 1313, 162–171 (2010).
de la Salle, S. et al. Acute separate and combined effects of cannabinoid and nicotinic receptor agonists on MMN-indexed auditory deviance detection in healthy humans. Pharmacol. Biochem. Behav. 184, 172739 (2019).
Spasova, V. et al. Impact of nicotine on cognition in patients with schizophrenia: A narrative review. Cureus 14(4), e24306 (2022).
Fisher, D. J. et al. Attenuation of mismatch negativity (MMN) and novelty P300 in schizophrenia patients with auditory hallucinations experiencing acute exacerbation of illness. Biol. Psychol. 100, 43–49 (2014).
Bodnar, F. et al. Automatic change detection in vision: Adaptation, memory mismatch, or both? II: Oddball and adaptation effects on event-related potentials. Attention Percept. Psychophys. 79(8), 2396–2411 (2017).
Erickson, M. A., Ruffle, A. & Gold, J. M. A meta-analysis of mismatch negativity in schizophrenia: From clinical risk to disease specificity and progression. Biol. Psychiatry 79(12), 980–987 (2016).
Funding
This work was supported by the following grants: Hungarian Research Fund—OTKA PD 115837; Hungarian Research Fund—OTKA FK 138385; Higher Education Institutional Excellence Programme of the Ministry of Human Capacities in Hungary, within the framework of the Neurology thematic programme of Semmelweis University.
Author information
Authors and Affiliations
Contributions
M.H. and M.C.s performed the EEG recording. M.H. and C.s.G. performed the data analysis and manuscript preparation. M.C.s and C.s.G. were responsible for the study design. C.z.I contributed to the study design and reviewed the manuscript critically. B.E., F.K. and B.M. made substantial contributions to the analyses and interpretation of the data and revised the manuscript critically. All authors contributed to and accepted the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Molnár, H., Marosi, C., Becske, M. et al. A comparison of visual and acoustic mismatch negativity as potential biomarkers in schizophrenia. Sci Rep 14, 992 (2024). https://doi.org/10.1038/s41598-023-49983-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49983-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.