Abstract
Large language models (LLMs) have shown potential in various applications, including clinical practice. However, their accuracy and utility in providing treatment recommendations for orthopedic conditions remain to be investigated. Thus, this pilot study aims to evaluate the validity of treatment recommendations generated by GPT-4 for common knee and shoulder orthopedic conditions using anonymized clinical MRI reports. A retrospective analysis was conducted using 20 anonymized clinical MRI reports, with varying severity and complexity. Treatment recommendations were elicited from GPT-4 and evaluated by two board-certified specialty-trained senior orthopedic surgeons. Their evaluation focused on semiquantitative gradings of accuracy and clinical utility and potential limitations of the LLM-generated recommendations. GPT-4 provided treatment recommendations for 20 patients (mean age, 50 years ± 19 [standard deviation]; 12 men) with acute and chronic knee and shoulder conditions. The LLM produced largely accurate and clinically useful recommendations. However, limited awareness of a patient’s overall situation, a tendency to incorrectly appreciate treatment urgency, and largely schematic and unspecific treatment recommendations were observed and may reduce its clinical usefulness. In conclusion, LLM-based treatment recommendations are largely adequate and not prone to ‘hallucinations’, yet inadequate in particular situations. Critical guidance by healthcare professionals is obligatory, and independent use by patients is discouraged, given the dependency on precise data input.
Similar content being viewed by others
Introduction
Large language models (LLMs) have recently spread into virtually all aspects of life, including medicine. Within the first two months of its launch, chatGPT, the most popular LLM and the archetype of dialogue-based artificial intelligence, attracted more than 100 million users and, in 2023, averaged more than 13 million daily visitors1,2.
While chatGPT (based on the GPT-3.5-model) performed at or near the passing threshold of 60% accuracy when undergoing the three standardized examinations of the United States Medical Licensing Exam (USMLE)3, its successor GPT-4 as the latest state-of-the-art LLM performed considerably better4. In addition to exceeding the USMLE passing threshold by over 20 percentage points, GPT-4 performs medical reasoning similarly to well-studied experts5. Beyond taking tests, chatGPT has diagnostic and triage abilities close to practicing physicians when dealing with case vignettes of conditions with variable severity6,7. GPT-4 has a clinical value in diagnosing challenging geriatric patients8. It also generates broadly appropriate recommendations for common questions about cardiovascular disease prevention9, breast cancer prevention, and screening10. It can also generate structured radiologic reports from written (prosaic) text11, and draft Impressions sections of radiologic reports, even though the GPT-4-generated Impressions are not (yet) as good as the radiologist-generated ones regarding coherence, comprehensiveness, and factual consistency12. For a comprehensive overview of LLMs and their utilization in radiology, the reader is referred to recent review articles13,14,15.
Despite the growing popularity of LLMs, concerns have arisen regarding the validity and reliability of their recommendations, particularly in medicine. LLMs tend to produce convincing but factual incorrect text (commonly referred to as “hallucinations”), which raises the question if LLMs are sufficiently sophisticated to be used as resources for health advice or may pose a potential danger16. In particular, patients may rely on information provided by artificial intelligence without consulting healthcare professionals17,18.
Likely, LLMs will also be extensively used by radiologists in the future. In this era of complex interdisciplinary patient management, a radiologist’s work often does not end with submitting a report of an imaging study. Addressing patients’ concerns and questions and communicating appropriately with non-radiologist colleagues requires solid knowledge of treatment options, prioritization, and limitations.
Consequently, the present study aims to investigate the validity of treatment recommendations provided by GPT-4, explicitly focusing on common orthopedic conditions, where accurate diagnosis and appropriate treatment are crucial for patients' recovery and long-term well-being19,20,21. By analyzing the treatment recommendations derived from clinical MRI reports, we evaluate whether the advice given by GPT-4 is scientifically sound and clinically safe. We hypothesize that GPT-4 produces largely accurate treatment recommendations yet is at substantial risk of hallucinations and may thus pose a potential risk for patients seeking health advice.
Materials and methods
Study design and dataset characteristics
The local ethical committee (Medical Faculty, RWTH Aachen University, Aachen, Germany, reference number 23/111) approved this retrospective study on anonymized data and waived the requirement to obtain individual informed consent. All methods were carried out in accordance with relevant guidelines and regulations. Following local data protection regulations, the board-certified senior musculoskeletal radiologist with ten years of experience (SN) screened all knee and shoulder MRI studies and associated clinical reports produced during the clinical routine at our tertiary academic medical center (University Hospital Aachen, Aachen, Germany) during February and March of 2023. Ninety-four knee MRI studies and 38 shoulder MRI studies were available for selection. We selected ten studies per joint, ensuring various conditions with variable severity and complexity. Table 1 provides a synopsis of the selected imaging studies with patient demographics, referring disciplines, reasons for the exam, principal diagnoses and treatment recommendations, and a statement on whether the treatment recommendations were considered problematic. Supplementary Table 1 provides more details on the reported diagnoses. Intentionally, we included MRI reports from patients with different demographic characteristics (i.e., age and sex) and referrals from various clinical disciplines. The diagnosis was checked for coherence and consistency using the associated clinical documentation (e.g., history and physical findings) and other non-imaging findings (e.g., laboratory values, intra-operative findings, functional tests, and others). Consequently, MRI studies were disregarded if additional findings were incoherent, inconsistent, or contradictory with the reference diagnosis.
The selected MRI reports were extracted from the local Picture Archiving and Communication System (iSite, Philips Healthcare, Best, Netherlands) as intended for clinical communication, i.e., in German. The MRI reports were anonymized by removing the patient's name, age, sex, and reference to earlier imaging studies. In the history and reason-for-exam section, any reference that may influence treatment recommendations, e.g., “preoperative evaluation [requested]”, was removed, too.
GPT-4 Encoding and Prompting
GPT-4 was accessed online (https://chat.openai.com/) on April 11th and 12th, 2023, and operated as the chatGPT March 23 version. Prompts were provided in a standardized format and the following sequence:
-
Prompt #1: Please translate the following MRI report into English.
-
Prompt #2: This is the MRI report of a [numerical age]-year-old [sex, woman/man]. Do the conditions need to be treated? And if so, how? Please be as specific as possible.
-
Prompt #3: This is too unspecific. Please advise the patient on what to do. Imagine you are the treating physician. Prioritize your treatment recommendations—begin with what is most sensible and relevant.
Consequently, GPT-4 was provided with the patient’s age and sex only. The translated (English) version of the clinical MRI report was checked for overall quality and in terms of accuracy, consistency, fluency, and context by the senior musculoskeletal radiologist (SN), who holds the certificate of the Educational Commission for Foreign Medical Graduates (ECFMG). A new chat session was started for each patient to avoid memory retention bias.
Alongside the MRI reports, the treatment recommendations made by GPT-4 following the initial (prompt #2) and the follow-up request (prompt #3) were saved.
Figure 1 provides an overview of the workflow.
Workflow of the Artificial Intelligence-powered MRI-to-treatment recommendation pipeline. GPT-4, denoted as the AI icon, was prompted three times to translate the MRI report, provide general treatment recommendations, and prioritize its recommendations. Two experienced orthopedic surgeons rated the patient-specific treatment recommendations.
Evaluation of treatment recommendations
Two board-certified and specialty-trained senior orthopedic surgeons with ten (BB) and 12 (CW) years of clinical experience in orthopedic and trauma surgery, evaluated the treatment recommendations made by GPT-4.
Both raters evaluated the treatment recommendations separately by answering the itemized questions in Table 2. Treatment recommendations were rated on Likert scales extending from 1 (poor or strongly disagree) to 5 (excellent or strongly agree) regarding overall quality, scientific and clinical basis, and clinical usefulness and relevance. Whether the treatment recommendations are up-to-date and consistent was rated on a binary basis, i.e., yes or no.
Afterward, both raters held a consensus meeting where discrepant ratings were discussed until a consensus was reached. Only the consented scores were registered and subsequently analyzed.
Results
In all responses, GPT-4 consistently disclaimed it was not a doctor. GPT-4 offered some general information on the conditions and potential treatment options, yet would not be willing to provide specific medical advice. It repetitiously stressed the importance of consulting with healthcare professionals for personalized treatment recommendations.
GPT-4 explained the MRI findings separately using layman’s language. It continuously worked down the list of findings when formulating its treatment recommendations, following the radiologist’s prioritization.
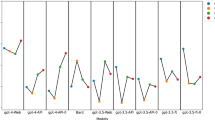
The overall quality of the treatment recommendations was rated as good or better for the knee and shoulder. Similarly, the recommendations were mainly up-to-date and consistent, adhering to clinical and scientific evidence and clinically useful/relevant (Fig. 2). Notably, the treatment recommendations provided for the shoulder were rated more favorably. We did not find signs of hallucinations, i.e., seemingly correct responses that (i) were non-sensical when considered against common knowledge in radiology or orthopedic surgery/traumatology or (ii) inconsistent with framework information or conditions stated in the radiologist’s request. Moreover, we did not find signs of speculations or oversimplifications.
Multidimensional ratings of the treatment recommendations provided by GPT-4. In a consensus meeting, two experienced orthopedic surgeons evaluated the treatment recommendations for various knee and shoulder conditions derived from clinical MRI reports. Ratings were based on five-item Likert scales, and counts were provided only for selected answers.
GPT-4's treatment recommendations generally followed a schematic approach. In most cases, conservative treatment was recommended initially, regularly accompanied by physical therapy. Surgical treatment was considered a potential option for those patients where conservative treatment, including physical therapy, would not yield satisfactory results. Representative MR images, MRI report findings, and GPT-4-based treatment recommendations are provided for the knee (Fig. 3) and shoulder (Fig. 4).
Representative knee joint MR images of a patient with a joint infection, key MRI report findings, and specific treatment recommendations by GPT-4. Axial proton density-weighted fat-saturated image above the patella (upper image) and sagittal post-contrast T1-weighted fat-saturated image through the central femur diaphysis (lower image). Of all 20 MRI studies/reports and associated treatment recommendations, these treatment recommendations were rated lowest.
The two orthopedic surgeons agreed that some recommendations could have been more specific. In numerous patients, GPT-4 provided general advice instead of tailoring the treatment recommendations to the particular condition or patient, thereby limiting their clinical usefulness. Furthermore, GPT-4 tended to err on the side of caution, recommending more conservative treatment options and leaving the decision for surgery to the specialists to be consulted. Supplementary Table 2 provides further details on the treatment recommendations for each patient/MRI report and associated comments by the two orthopedic surgeons.
Discussion
Our study suggests that GPT-4 can produce valuable treatment recommendations for common knee and shoulder conditions. The recommendations were largely up-to-date, consistent, clinically useful/relevant, and aligned with the most recent clinical and scientific evidence.
We observed signs of reasoning and inference across multiple key findings. For example, GPT-4 correctly deduced that meniscus tears may be associated with bone marrow edema (as a sign of excessive load transmission). Hence, its recommendation to “address focal bone marrow edema: As this issue could be related to the medial meniscus tear […]" was entirely plausible.
Similarly, GPT-4 demonstrated considerable foresight as it recommended organizing post-surgical care and rehabilitation for the patient with multi-ligament knee injuries and imminent surgery. Whether this recommendation can be regarded as "planning" is questionable, though, as true planning abilities in the non-medical domain are still limited4,16. Instead, these recommendations are likely based on the schematic treatment regime that GPT-4 encountered in its training data.
Interestingly, GPT-4 recommended lifestyle modifications, i.e., weight loss and low-impact exercise, and assistive devices (such as braces, canes, or walkers) for shoulder degeneration. While these are sensible and appropriate recommendations for knee osteoarthritis, such recommendations are of doubtful value in shoulder osteoarthritis. In patients with shoulder osteoarthritis or degeneration, exercises to improve the range of motion were not recommended, even though they are indicated22. Again, this observation is likely attributable to the statistical modeling behavior of GPT-4, given the epidemiologic dominance of knee OA over shoulder OA.
Additional limitations of GPT-4 became apparent when the model was tasked to make treatment recommendations for patients with complex conditions or multiple relevant findings.
Critically, the patient with septic arthritis of the knee was not recommended to seek immediate treatment. This particular treatment recommendation, or rather the failure to stress its urgency, is negligent and dangerous. Septic arthritis constitutes a medical emergency, which may lead to irreversible joint destruction, morbidity, and mortality. Literature studies report mortality rates of 4% to 42%23,24,25. Furthermore, because of the stated cartilage damage in this patient, GPT-4 also recommended cartilage resurfacing treatment. However, doing so in a septic joint is contraindicated and medical malpractice26.
GPT-4 was similarly unaware of the patient’s overall situation after knee dislocation. Even though the surgical treatment recommendations for multi-ligament knee injuries were plausible, a potential concomitant popliteal artery injury was not mentioned. It occurs in around 10% of knee dislocations and may dramatically alter treatment2.
Remarkably, we did not find signs of so-called "hallucinations", i.e., GPT-4 "inventing" facts and confidently stating them. Even though speculative at this stage, the absence of such hallucinations may be due to the substantial and highly specific information provided in the prompt (i.e., the entire MRI report per patient) and our straightforward prompting strategy compared to more suggestive promptings of other studies16.
No patient is treated on the basis of the MR images or the MRI report. Nonetheless, using real-patient (anonymized) MRI reports rather than artificial data, increases our study’s applicability and impact.
However, while GPT-4 offered treatment recommendations, it is crucial to understand that it is not a replacement for professional medical evaluation and management. The accuracy of its recommendations is largely contingent upon the input's specificity, correctness, and reasoning, which is typically not how a patient would phrase the input and prompt the tool. Therefore, LLMs, including GPT-4, should be used as supplementary resources by healthcare professionals only, as they provide critical oversight and contextual judgment. Optimally, healthcare professionals know a patient's constitution and circumstances to provide effective, safe, and nuanced diagnostic and treatment decisions. Consequently, we caution against the use of GPT-4 by laypersons for specific treatment suggestions.
Along similar lines, integrating LLMs into clinical practice warrants ethical considerations, particularly regarding medical errors. First and foremost, their use does not obviate the need for professional judgment from healthcare professionals who are ultimately responsible for interpreting the LLM's output. As with any tool applied in the clinic, LLMs should only assist (rather than replace) healthcare professionals. However, the safe and efficient application of LLMs requires a thorough understanding of their capabilities and limitations. Second, developers must ensure that their LLMs are rigorously tested and validated for clinical use and that potential limitations and errors are communicated, necessitating ongoing performance monitoring. Third, healthcare institutions integrating LLMs into their clinical workflows should establish governance structures and procedures to monitor performance and manage errors. Fourth, the patient (as a potential end-user) must be made aware of the potential for hallucinations and erroneous and potentially harmful advice. Our study highlights the not-so-theoretical occurrence of harmful advice—in that case, we advocate a framework of shared responsibility. The healthcare professional is immediately responsible for patient care if involved in alleged malpractice. Simultaneously, LLM developers and healthcare institutions share an ethical obligation to maximize the benefits of LLMs in medicine while minimizing the potential for harm. While there is no absolute safeguard against medical errors, informed patients make informed decisions—this applies to LLMs as to any other health resource utilized by patients seeking medical advice.
Importantly, LLMs, including GPT-4, are currently not approved as medical devices by regulatory bodies. Therefore, LLMs cannot and should not be used in the clinical routine. However, our study indicates that the capability of LLMs to make complex treatment recommendations should be considered in their regulation.
Moreover, the recent advent of multimodal LLMs such as GPT-4Vision (GPT-4V) has highlighted the (potentially) vast capacities of multimodal LLMs in medicine. In practice, the text prompt (e.g., original MRI report) could be supplemented by select MR images or additional clinical parameters such as laboratory values. Recent literature evidence studying patients in intensive care confirmed that models trained on imaging and non-imaging data outperformed their counterparts trained on only one data type.27 Consequently, future studies are needed to elucidate the potentially enhanced diagnostic performance as well as the concomitant therapeutic implications.
When evaluating the original MRI report (in German) and its translated version (in English), we observed them to be excellently aligned regarding accuracy, consistency, fluency, and context. This finding is confirmed by earlier literature, indicating an excellent quality of GPT-4-based translations, at least for high-resource European languages such as English and German28. Inconsistent taxonomies in MRI reports may be problematic for various natural language processing tasks but did not affect the quality of report translations in this study.
Our study has limitations. First, we studied only a few patients, i.e., ten patients each for the shoulder and knee. Consequently, our investigation is a pilot study with preliminary results and lacks a solid quantitative basis for statistical analyses. Consequently, no statistical analysis was attempted based on our dataset. Second, to enhance its depth and relevance to clinical scenarios, GPT-4’s predictions need to be more specific. Additional ‘fine-tuning’ and domain-specific training using medical datasets, clinical examples, and multimodal data may enhance its robustness and specificity as well as its overall value as a supplementary resource in healthcare. Third, the patient spectrum was broad. A more thorough performance assessment would require substantially more patients with rare conditions and subtle findings to be included. Fourth, treatment recommendations were qualitatively judged by two experienced orthopedic surgeons. Given the excellent level of inter-surgeon agreement, we consider the involvement of two surgeons sufficient, yet involving three or more surgeons could have strengthened the outcome basis even further. Fifth, the tendency of GPT-4 to give generic and unspecific answers and to err on the side of caution rendered it challenging to assess its adherence to guidelines or best practices exactly. Sixth, we used a standardized and straightforward way of prompting GPT-4. After more extensive modifications of these prompts, outcomes may be different.
In summary, common conditions and associated treatment recommendations were well handled by GPT-4, whereas the quality of the treatment recommendations for rare and more complex conditions remains to be studied. Most treatment recommendations provided by GPT-4 were largely consistent with the expectations of the evaluating orthopedic surgeons. The schematic approach used by GPT-4 often aligns well with the typical treatment progression in orthopedic surgery and sports medicine, where conservative treatments are usually attempted first, and surgical intervention is considered only after the failure of conservative treatments.
Conclusion
In conclusion, GPT-4 demonstrates the potential to provide largely accurate and clinically useful treatment recommendations for common orthopedic knee and shoulder conditions. Expert surgeons rated the recommendations at least as "good", but the patient's situation and treatment urgency were not fully considered. Therefore, patients need to consult healthcare professionals for personalized treatment recommendations, while GPT -4 may be a supplementary resource rather than a replacement for professional medical advice after regulatory approval.
Data availability
Data generated or analyzed during the study (i.e., the original MRI reports) are available from the corresponding author upon reasonable request.
Change history
05 March 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-56029-x
Abbreviations
- AI:
-
Artificial intelligence
- LLM:
-
Large language model
- MRI:
-
Magnetic resonance imaging
References
Ruby, D. ChatGPT Statistics for 2023 (New Data + GPT-4 Facts), <https://www.demandsage.com/chatgpt-statistics/> (2023).
Naziri, Q. et al. Knee dislocation with popliteal artery disruption: A nationwide analysis from 2005 to 2013. J. Orthop. 15, 837–841 (2018).
Kung, T. H. et al. Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLoS Digit. Health 2, e0000198 (2023).
Bubeck, S. et al. Sparks of artificial general intelligence: Early experiments with gpt-4. http://arxiv.org/abs/2303.12712 (2023).
Nori, H., King, N., McKinney, S. M., Carignan, D. & Horvitz, E. Capabilities of gpt-4 on medical challenge problems. http://arxiv.org/abs/2303.13375 (2023).
Rao, A. S. et al. Assessing the utility of ChatGPT throughout the entire clinical workflow. medRxiv https://doi.org/10.1101/2023.02.21.23285886 (2023).
Levine, D. M. et al. The diagnostic and triage accuracy of the GPT-3 artificial intelligence model. medRxiv https://doi.org/10.1101/2023.01.30.23285067 (2023).
Shea, Y.-F., Lee, C. M. Y., Ip, W. C. T., Luk, D. W. A. & Wong, S. S. W. Use of GPT-4 to analyze medical records of patients with extensive investigations and delayed diagnosis. JAMA Netw. Open 6, e2325000–e2325000 (2023).
Sarraju, A. et al. Appropriateness of cardiovascular disease prevention recommendations obtained from a popular online chat-based artificial intelligence model. JAMA 329, 842–844 (2023).
Haver, H. L. et al. Appropriateness of breast cancer prevention and screening recommendations provided by ChatGPT. Radiology 307(4), e230424 (2023).
Adams, L. C. et al. Leveraging GPT-4 for post hoc transformation of free-text radiology reports into structured reporting: A multilingual feasibility study. Radiology 307, e230725. https://doi.org/10.1148/radiol.230725 (2023).
Sun, Z. et al. Evaluating GPT-4 on impressions generation in radiology reports. Radiology 307, e231259 (2023).
Stanzione, A. et al. Large language models in radiology: fundamentals, applications, ethical considerations, risks, and future directions. In Diagnostic and Interventional Radiology (Ankara, Turkey) (2023).
Tippareddy, C., Jiang, S., Bera, K. & Ramaiya, N. Radiology reading room for the future: Harnessing the power of large language models like ChatGPT. Current Probl. Diagn. Radiol. https://doi.org/10.1067/j.cpradiol.2023.08.018 (2023).
Bera, K., O’Connor, G., Jiang, S., Tirumani, S. H. & Ramaiya, N. Analysis of ChatGPT publications in radiology: Literature so far. Current Probl. Diagn. Radiol. https://doi.org/10.1067/j.cpradiol.2023.10.013 (2023).
Lee, P., Bubeck, S. & Petro, J. Benefits, limits, and risks of GPT-4 as an AI Chatbot for medicine. N. Engl. J. Med. 388, 1233–1239 (2023).
Richardson, J. P. et al. Patient apprehensions about the use of artificial intelligence in healthcare. NPJ. Digit. Med. 4, 140 (2021).
Ayers, J. W. et al. Comparing physician and artificial intelligence chatbot responses to patient questions posted to a public social media forum. JAMA Int. Med. https://doi.org/10.1001/jamainternmed.2023.1838 (2023).
Vallier, H. A., Wang, X., Moore, T. A., Wilber, J. H. & Como, J. J. Timing of orthopaedic surgery in multiple trauma patients: Development of a protocol for early appropriate care. J. Orthop. Trauma 27, 543–551 (2013).
Shan, L., Shan, B., Suzuki, A., Nouh, F. & Saxena, A. Intermediate and long-term quality of life after total knee replacement: A systematic review and meta-analysis. JBJS 97, 156–168 (2015).
Vuurberg, G. et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 52, 956–956 (2018).
Chillemi, C. & Franceschini, V. Shoulder osteoarthritis. Arthritis 2013 (2013).
Coakley, G. et al. BSR & BHPR, BOA, RCGP and BSAC guidelines for management of the hot swollen joint in adults. Rheumatology 45, 1039–1041 (2006).
Kaandorp, C. J., Krijnen, P., Moens, H. J., Habbema, J. D. & van Schaardenburg, D. The outcome of bacterial arthritis: A prospective community-based study. Arthritis Rheum 40, 884–892. https://doi.org/10.1002/art.1780400516 (1997).
Fangtham, M. & Baer, A. N. Methicillin-resistant Staphylococcus aureus arthritis in adults: Case report and review of the literature. Semin Arthritis Rheum 41, 604–610. https://doi.org/10.1016/j.semarthrit.2011.06.018 (2012).
Olsen, A. S. & Shah, V. M. Surgical Approaches to Advanced Knee OA (TKA, UKA, Osteotomy). In Principles of Orthopedic Practice for Primary Care Providers, 425–435 (2021).
Khader, F. et al. Multimodal deep learning for integrating chest radiographs and clinical parameters: A case for transformers. Radiology 309, e230806 (2023).
Jiao, W., Wang, W., Huang, J., Wang, X. & Tu, Z. Is ChatGPT a good translator? Yes with GPT-4 as the engine. http://arxiv.org/abs/2301.08745 (2023)
Acknowledgements
In accordance with the COPE (Committee on Publication Ethics) position statement of 13 February 2023 (https://publicationethics.org/cope-position-statements/ai-author), the authors hereby disclose the use of the following artificial intelligence models during the writing of this article. GPT-4 (OpenAI) for checking spelling and grammar.
Funding
Open Access funding enabled and organized by Projekt DEAL. JNK is supported by the German Federal Ministry of Health (DEEP LIVER, ZMVI1-2520DAT111) and the Max-Eder-Programme of the German Cancer Aid (grant #70113864), the German Federal Ministry of Education and Research (PEARL, 01KD2104C; CAMINO, 01EO2101; SWAG, 01KD2215A; TRANSFORM LIVER, 031L0312A; TANGERINE, 01KT2302 through ERA-NET Transcan), the German Academic Exchange Service (SECAI, 57616814), the German Federal Joint Committee (Transplant.KI, 01VSF21048) the European Union’s Horizon Europe and innovation programme (ODELIA, 101057091; GENIAL, 101096312) and the National Institute for Health and Care Research (NIHR, NIHR213331) Leeds Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. DT is supported by the European Union’s Horizon Europe programme (ODELIA, 101057091), by grants from the Deutsche Forschungsgemeinschaft (DFG) (TR 1700/7-1), and the German Federal Ministry of Education and Research (SWAG, 01KD2215A; TRANSFORM LIVER, 031L0312A). SN is funded by grants from the Deutsche Forschungsgemeinschaft (DFG) (NE 2136/3-1). KB is supported by the European Union’s Horizon Europe programme (COMFORT, 101079894).
Author information
Authors and Affiliations
Contributions
Guarantors of integrity of entire study, all authors; study concepts/study design or data acquisition or data analysis/interpretation, all authors; manuscript drafting, D.T.; manuscript revision for important intellectual content, all authors; approval of final version of submitted manuscript, all authors; literature research, D.T., S.N.; experimental studies, D.T., C.K., C.D.W., B.J.B., S.N., D.T.; data analysis, D.T., S.N.; manuscript editing: all authors.
Corresponding author
Ethics declarations
Competing interests
JNK declares consulting services for Owkin, France; DoMore Diagnostics, Norway and Panakeia, UK and has received honoraria for lectures by Eisai, Roche, MSD and Fresenius. The other authors report no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Author Contributions section in the original version of this Article was incomplete. Full information regarding the corrections made can be found in the correction notice for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Truhn, D., Weber, C.D., Braun, B.J. et al. A pilot study on the efficacy of GPT-4 in providing orthopedic treatment recommendations from MRI reports. Sci Rep 13, 20159 (2023). https://doi.org/10.1038/s41598-023-47500-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47500-2
This article is cited by
-
Augmented non-hallucinating large language models as medical information curators
npj Digital Medicine (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.