Abstract
Pancreatic enzyme replacement therapy (PERT) has been recommended as the preferred method for pancreatic exocrine insufficiency caused by chronic pancreatitis (CP). However, at present, the patient-related factors for the poor PERT management are not clear, and there are no studies on the adherence to PERT in patients with CP in East China. This was a mixed-method study following the principle of sequential explanatory design and included two parts: a quantitative and qualitative study. A cross-sectional survey of medication adherence (MA) was first carried out, followed by a semi-structured interview to further explore and explain the influencing factors of adherence to PERT. Of the 148 patients included in this study, 48.0% had poor MA and only 12.8% had good MA. Multivariate logistic regression showed that lower levels of education and income were contributing factors for non-adherence to PERT. Semi-structured interviews with 24 patients revealed that the reasons for non-adherence also included lack of knowledge, self-adjustment of PERT, lifetime of medication, side effects of PERT, forgetfulness, financial burdens, and accessibility issues. The adherence to PERT was poor among patients with CP in East China. Healthcare providers should personalize medication strategies to improve patients’ MA.
Similar content being viewed by others
Introduction
Chronic pancreatitis (CP) is a rare progressive inflammatory disease of the pancreas characterized by irreversible pancreatic acinar atrophy and fibrosis1. The global incidence of CP is about 4.4–14.0 per 100,000 people, the prevalence is about 36.9–52.4 per 100,000 people, and there is a trend of increasing year by year2,3. The main symptoms of CP patients are chronic abdominal pain and pancreatic endocrine and exocrine loss symptoms such as elevated blood sugar, maldigestion, and weight loss. In addition, patients may also have complications such as pancreatic duct stones, pancreatic duct stenosis, and pancreatic cysts and have a higher risk of pancreatic cancer, which significantly affects their quality of life4,5.
Pancreatic exocrine insufficiency (PEI) is one of the common complications of CP, and its incidence increases progressively with the development of disease and prolongation of course6. Steatorrhea occurs when pancreatic enzyme production decreases by more than 90%7. PEI is associated with maldigestion and significantly affects the absorption of protein, fat, micronutrients, and fat-soluble vitamins, resulting in nutritional deficiencies8,9, complications such as osteoporosis10, adverse cardiovascular events11, infections12 and an increased risk of death13. Guidelines have recommended pancreatic enzyme replacement therapy (PERT) as the cornerstone and preferred treatment method for PEI to improve malabsorption and malnutrition and prevent their adverse outcomes in CP patients14,15. However, studies have shown that the current status of treatment for PEI in CP patients is not ideal: there are significant insufficiencies in the diagnosis and treatment for PEI and there is still much room for improvement in PERT management6,16,17,18.
Medication adherence (MA) refers to “the extent to which patients take medications as prescribed by their health care providers”19. Great MA plays an important role in disease control, symptom relief, and improving prognosis20. The status of patients’ MA has been extensively explored in a wide range of other chronic diseases. However, at present, research on patients’ adherence on PERT in pancreatic diseases is still quite limited. Of the available research evidence, Barkin et al. found that the adherence rate of PERT in pancreatic cancer patients was 50.1%21. A US study of patients undergoing total pancreatectomy with islet autotransplantation found a 79% adherence rate of PERT after surgery22. A retrospective study by Khandelwal et al. discovered that the PERT adherence rate in patients with PEI caused by CP, pancreatic cancer and pancreatectomy was 48%, 52% and 52%, respectively, and this figure declined rapidly to about 20% within a one-year follow-up period23. These data were all from Western countries, to date, there are no studies on adherence to PERT in Chinese CP patients. The influencing factors of adherence to PERT among patients with CP in China are still unclear.
It is of great significance to identify the status and factors of adherence disorder of PERT for the individualized formulation of medication strategies and to improve the level of patients’ MA. Therefore, the aims of this study were to (1) clarify the status of adherence to PERT among patients with CP in East China, and (2) explore the influencing factors of adherence to PERT to provide reference and inspiration for PERT management among CP patients.
Materials and methods
Study design
This was a cross-sectional study based on a mixed-method approach conducted at First Affiliated Hospital of Naval Medical University (Changhai Hospital) in Shanghai, China, including two parts: a quantitative and qualitative study. Following the principle of sequential explanatory design, quantitative analysis was conducted first, followed by in-depth interviews to explore and explain various subjective and objective influencing factors to adherence to PERT among Chinese CP patients from a more comprehensive perspective.
This study protocol was approved by the Changhai Hospital Ethics Committee (CHEC2020-026) and registered on ClinicalTrial.gov (NCT05489003). The study was conducted following the Declaration of Helsinki, and all patients signed informed consent.
Quantitative study
Data source, sampling method, and eligibility criteria
As part of an ongoing prospective study of symptoms and quality of life among patients with CP in China, this study included all CP patients admitted to the Department of Gastroenterology in our hospital from June to September 2022. The diagnosis of CP conformed to the Asia–Pacific consensus24. We excluded patients who (1) were under 18 or over 70 years old, (2) received PERT for less than 3 months, (3) were pregnant, (4) had a comorbid malignancy, (5) had communication disorders, (6) had a history of mental illness or were taking psychotropic drugs, and (7) refused to participate in this study or participated in other relevant studies at the same time.
Measurements and data collection
Patients’ MA was measured by the Chinese version of the Morisky Medication Adherence Scale (C-MMAS-8)25.
According to literature search and expert opinions, patients’ data were collected through self-designed sociodemographic and clinical characteristics questionnaire. The questionnaire included patient’s age, gender (male or female), education level (junior high school or below, senior high school, university or above), marital status (married, unmarried, divorced, widowed), employment status (employed, unemployed, retired, in study), monthly household income (CNY) (< 5000, 5000–10,000, ≥ 10,000)26, residence (urban or rural), type of medical insurance (rural cooperative medical insurance, urban residents’ medical insurance, employee medical insurance), course of disease, type of pain after taking medication (repeat attacks of acute pancreatitis, repeat pain, repeat acute attacks and pain, chronic pain), and history of diabetes, smoking, and drinking (yes or no)27.
The MMAS-8 was developed by Morisky et al. in 2008 to evaluate MA of outpatients28. The scale consists of 8 items, items 1–4 and 6–7 are scored 0 for “yes” and 1 for “no”, item 5 is reverse scored, and item 8 is scored on a 5-point Likert scale (1: “never”, 0.75: “occasionally”, 0.5: “sometimes”, 0.25: “usually”, 0: “always”). The total MMAS-8 score is the sum of the scores of each item. A score of less than 6 indicates poor MA, greater than 6 and less than 8 indicates moderate MA, and a score of 8 indicates good MA. There were no significant differences between MMAS-8 and C-MMAS-8 in terms of items, contents, and scoring. The validity and reliability of C-MMAS-8 has been validated in a Chinese population25.
Data analysis
According to the C-MMAS-8 scoring standard, patients were divided into two groups: medication adherence and medication nonadherence, with a cut-off score of 6. Statistical analysis was performed using SPSS 26.0 software. All data were analyzed descriptively. The Kolmogorov–Smirnov test was used to test the normality of data. Continuous variables with normal distribution and skewed distribution and categorical variables were described by mean and standard deviations, median with interquartile range, and frequencies and proportions, respectively. Pearson χ2 test was used for between-group comparisons of categorical variables. Based on the results of univariate analysis, variables with statistically significant differences were selected for multivariate logistic regression analysis to further explore the influencing factors of adherence to PERT. All statistics were two-sided, and P values less than 0.05 were considered statistically significant.
Qualitative study
The qualitative study was designed and conducted following the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist.
Sampling method
To further explore the factors of barriers to adherence to PERT, the interviewed patients were recruited by purposive sampling based on different C-MMAS-8 scores.
Data collection
Qualitative data were collected using a semi-structured interview, which was conducted after written consents (including permission to record) were obtained from the patients. The interviews were conducted by two experts with a doctor’s degree and a master’s degree in medicine and nursing, who were experienced in PERT management and qualitative research, respectively, in the form of face-to-face in the meeting room of the ward. Each interview lasted for 25 to 40 min and revolved around five open-ended questions that asked to the participants: “How do you feel about your current MA?”, “How do you take your pancreatic enzyme?”, “How do you feel after taking pancreatic enzyme?”, “Have you encountered any problems and difficulties in the process of taking pancreatic enzyme?”, “What do you think of the current prescription of pancreatic enzyme?”. Field notes were taken throughout the interviews. Data saturation was considered only after no new contents appeared in three consecutive interviews29. After 20 interviews, the authors found that no new contents appeared. To check the data saturation, four more interviews were conducted. Finally, the data collection stopped after 24 interviews due to there were no new information and themes obtained in the four additional interviews. To protect patient privacy, during the interviews, only the interviewee and participants were present. All participants were given numerical numbers. Individual information (name, occupation, etc.) that can identify the patient shall be kept by another author.
Data analysis
The thematic analysis by Braun and Clarke was used for qualitative data analysis30. All records were transcribed and validated by two researchers within 24 h after each interview. Two researchers independently coded the first four transcripts by reading and comparing the notes. After another four coding of transcripts, the initial codebook agreed by the researchers was established. Subsequently, the first researcher continued to code the remaining transcripts and discussed with the second researcher to reach a consensus when new codes appeared. After the coding was completed, the research team organized the coded data into themes. All research results were based on discussions and consensus reached by the entire research team.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Changhai Hospital Ethics Committee (CHEC2020-026). All the participants have signed an informed consent.
Results
Quantitative analysis
Characteristics of participants
A total of 148 patients were recruited for this study, 11 were directly considered to have poor MA because they proactively reported had not continued their medication after their last PERT medication had been exhausted several months earlier, and 137 completed the C-MMAS-8. Table 1 showed the characteristics of the participants. The mean age of the patients was 40.18 ± 13.44 years, and 67.6% (100/148) were male. The mean C-MMAS-8 score was 5.92 ± 1.65 points, 48.0% (71/148) of patients had poor MA, 39.2% (58/148) had moderate MA, and 12.8% (19/148) had good MA.
Factors associated with medication adherence.
Table 2 showed the results of the univariate analysis. There were significant differences between the two groups in terms of gender (P = 0.036), age (P = 0.043), education level (P = 0.005), employment status (P = 0.016), monthly household income (P = 0.003), type of health insurance (P = 0.014), and history of smoking (P = 0.021) and drinking (P = 0.033). There was no statistically significant difference in MA between patients with different marital status, residence, course of disease, type of pain after taking medication, diabetes, and steatorrhea.
Table 3 presented the results of the multivariable logistic regression analysis based on the eight variables that were statistically significant in univariate analysis. Patients with senior high school (adj.OR = 0.18, 95% CI 0.06–0.56, P = 0.003) and university and higher (adj.OR = 0.32, 95% CI 0.11–0.94, P = 0.039) education had lower odds of poor MA to PERT compared to those with junior high school or lower education. Patients with monthly household income less than 5,000 (adj.OR = 4.16, 95% CI 1.36–12.75, P = 0.013) and 5000–10,000 (adj.OR = 2.94, 95% CI 1.01–8.58, P = 0.049) had higher odds of poor MA compared to those with monthly household income over 10,000.
Qualitative analysis
Characteristics of participants
27 of the 148 patients were invited to participate in the interview, and three of them declined. Table 4 showed the characteristics of the 24 interviewed participants. Supplement Table 1 showed the detailed information of each interviewed participate. Among them, 14 (58.33%) were male, age ranged 25–59 years, the mean score of C-MMAS-8 was 5.25 ± 1.99, and 16 (66.67%) had poor adherence to PERT.
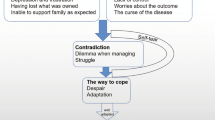
Key themes
Seven themes regarding barriers to MA emerged from interviews: (1) Lack of knowledge, (2) Self-adjustment of PERT, (3) Lifetime of medication, (4) Side effects of PERT, (5) Forgetfulness, (6) Financial burdens, and (7) Accessibility issues (Table 5).
Theme 1: Lack of knowledge
Some patients reported that they were unaware of their disease condition, treatment options, and the nature of drugs they are taking. They believed they did not need to take medication or need to adhere to it for a long period of time.
“I didn't know that I had to take this medicine all the time, and the doctor there didn't tell me. I stopped taking it, after eating up the medicine prescribed by the doctor every time.” (N15)
“I have taken the medicine before, and the doctor said that the medicine needed to be taken for the rest of my life. I was worried that the long-term use of it would cause damage to my liver and kidneys, and then I stopped taking it later.” (N24)
Theme 2: Self-adjustment of PERT
Some patients will exert their subjective initiative in taking the medication and changed the dosage according to the severity of their symptoms and type of diet.“Usually, I did not take medicine if I felt fine, and if I felt my stomach rising or a little uncomfortable, I would take more pills on my own.” (N7)
“If I ate porridge in the morning, I would not take the medicine, and if I went to a restaurant or ate greasy, or went out to socialize and drank, I would add a few pills myself.” (N22)
Theme 3: Lifetime of medication
Since CP patients will not show obvious symptoms during the stable phase, the benefits of taking the medication cannot be clearly perceived in a short term and coupled with the fact that pancreatic enzyme need to be taken by patients for a long period of time, a long-term use of the medication may reduce patients’ MA.
“The doctor told me to take the drug for life, and the dosage could be a little less when I was young and increased when I was older. I took it for a while, but it didn't seem to have much effect, so I stopped taking it. I wanted to wait until I get older.” (N5)
Theme 4: Side effects of PERT
A few patients reported some side effects after taking the medication, which in severe cases affected their daily life, so they chose not to take the medication.
“Originally, I had symptoms of diarrhea and had to have bowel movements 3–4 times a day. However, once I took this medicine, I would become constipated, I may not have a bowel movement for several days, and my stomach felt bloated, so I just stopped taking it.” (N10)
Theme 5: Forgetfulness
Some patients said that they would forget to bring their medicines or forget to take drugs because they were busy at work or needed to go out. In addition, a small number of patients said that they relied on reminders from others to improve MA.
“I am working as a salesman, and the nature of my work is different from that of others sitting in the office, with medicine on their desk. Sometimes I forgot to take my medicine when I go out. Sometimes I would forget to take medicine when I was busy or had irregular meals.” (N14)
“This medicine should be taken at mealtime, and I easily forget to take it without being reminded. Sometimes I remembered it after meal.” (N8, N23)
Theme 6: Financial burdens
Some patients reported that taking medicine would cause a certain financial burden, so they chose not to take medicine or switch to other drugs.
“I had to take four pills at a time, three times a day is 12 pills, and a bottle of medicine was finished within a few days. My wife and I were both part-time workers. We can't afford to eat so much, so we switched to domestic pancreatic enzyme tablets later.” (N6)
Theme 7: Accessibility issues
Considering that CP is a rare disease, not all hospitals can provide the medications patients need. Some patients reported that they lacked access to medication.
“This drug cannot be bought in our county at all, only the two hospitals in the provincial capital had the sale. Also, I cannot buy a lot at once. I can only buy 2 weeks of drugs at a time with my medical insurance reimbursement. In addition, it was inconvenient to travel due to the COVID-19 epidemic. It was too troublesome to buy medicine.” (N20)
Discussion
Although PERT has been recommended as the first choice for the treatment of PEI caused by CP, there are significant center related variances in the management of PERT in clinical practice, and many patients have not been treated in a standardized way18. In available studies, data on adherence to PERT among CP patients is limited. This may be very important as identifying the levels of and factors influencing MA may help to better implement PERT management and improve the prognosis of PEI. To our knowledge, this study was the first to explore the adherence to PERT among patients with CP in China. The mixed study design was also a strength of this paper, allowing for a more comprehensive perspective on the factors influencing MA. Overall, MA to PERT was currently poor in Chinese CP patients. During the qualitative interviews, we found that factors affecting MA included lack of knowledge, self-adjustment of PERT, lifetime of medication, side effects of PERT, forgetfulness, financial burdens, and accessibility issues.
In this study, the rate of non-adherence to PERT reached 48.0% and only 12.8% had good MA. This result was close to the adherence to PERT after 1 year follow-up in the study by Khandelwal et al.23. We believed that this result was true and consistent with the current status of long-term adherence to PERT in patients with CP. However, this figure was significantly lower than that in the studies by Barkin et al. and Crosby et al.21,22. In their studies, the rate of adherence to PERT respectively reached 50% and 79% in patients with pancreatic cancer and those undergoing total pancreatectomy with islet autotransplantation. One possible explanation for such high MA in their studies was that patients included in our study all chose to receive interventional treatment for pancreatic duct stones, and the serious condition of pancreatic cancer and painful and traumatic surgical treatment experiences of the patients in their studies may contribute to their higher medication consciousness and adherence to PERT.
Adherence to PERT in patients with CP in our study was also lower than in some common chronic diseases. In a meta-analysis by Khunti et al. involving over 300,000 patients with type 2 diabetes, the mean rate of poor MA was 37.8%31. Another meta-analysis by Durand et al. on MA in patients with refractory hypertension reported that the pooled rates of non-adherence was 31.2%32. Cancer, cardiovascular diseases, diabetes and chronic respiratory diseases have been listed by the World Health Organization (WHO) as the top four non-infectious diseases worldwide33. Compared with these common chronic diseases widely publicized and well-known by the individuals, given the rarity of CP, there is a clear lack of knowledge of CP among patients, as evidenced by the interviews in this study, where patients reported that they were not well informed about their conditions and the medication they were taking (N15, N24). Therefore, we believed that a lack of disease knowledge may be one of the potential reasons for the poor adherence to PERT among CP patients. In addition, inadequate and inconsistent medication guidance from health care providers may be another reason for poor MA. Existing studies have concluded that there is a lack of uniform consensus among gastroenterologists on the diagnosis and treatment of PEI and that only a small number of pancreatic specialists can surveil and treat PEI adequately compared to primary care providers17,34.
Therefore, we recommend, first, standardized guidelines and additional education are necessary for healthcare providers. National advanced pancreatic disease institutions should develop and promote PEI treatment guidelines applicable to CP patients in their country and conduct educational courses and guideline interpretations for non-pancreatologist on PEI and PERT to help them prescribe uniform and standardized plan of PERT. Second, it is positive for patients to be informed about the disease and the medication they are taking. For example, providing patients with information about prescribed medications has been shown to improve patients’ MA35,36. In addition, given that MA usually decreases over time, and given the long-term nature of PERT and the lack of short-term effects (N5), the follow-up monitoring and management of medication behavior is also integral to improving MA37. For example, electronic pill boxes38, electronic reminders39,40, smartphone applications41,42 and closer communication between doctors and patients43 are thought to help improve patients’ MA.
In this study, the results of multivariate analysis showed that lower levels of education and income were contributing factors for non-adherence to PERT. In addition, forgetfulness, side effects and the cost of medication were potential factors affecting patients’ MA. These findings fall within the WHO framework for MA and were consistent with previous research findings44,45,46.
Economic factors are considered one of the most important influences on patients’ MA. In the quantitative analysis, patients with poor MA were more likely to have lower monthly household income (< 5000 CNY). Excessive medical costs and financial burden may be the cause of poor MA. Therefore, for patients who may have financial difficulties, health care providers should offer them an alternative cheaper drug choice at the time of prescribing. In terms of medication guidance, doctors and nurses should personalize the medication strategy according to patients’ lifestyle and guide them to adjust the dosage reasonably according to their diet to reduce medication expenditure. For medical administrations and medical institutions, improving non-local medical insurance settlement services and reducing patients’ own expenses are effective means to improve patients’ MA. In addition, during the interviews we also found that even patients with stable jobs similarly reported difficulties with MA (N14). The type of work, work environment and working hours of patients may influence their willingness and behavior of taking medication, however, these factors have not been explored in depth in previous articles.
The level of education was another important factor influencing patients’ adherence to PERT. This is easy to understand, as patients who have received better education usually have better comprehension and acceptance of knowledge related to diseases and medications and have a richer knowledge reserve, resulting in their better MA. Meanwhile, existing views suggested that patients’ cognition of diseases (such as etiology, disease harms, outcome, and controllability) will directly influence their MA47. However, we also found an interesting phenomenon. Generally, younger patients usually have a higher level of education compared to older patients, so their adherence to PERT should have been better. However, in fact, we found that MA appeared to be worse in younger patients. The possible explanations were, first, younger patients had a relatively new diagnosis and a shorter course of disease, and that their relapses and disease experiences were less frequent. Second, young patients tended to have a better level of education. On the one hand, good education made it easier for them to understand and accept disease knowledge, but on the other hand, these patients were also relatively more rebellious, more likely to exert their subjective initiative in the process of taking drugs, and did not comply with drug prescriptions48,49. Considering the youthfulness and good acceptance of medication non-adherent patients, with the rapid development of new media technology and instant music video platforms, based on the existing e-reminders, smartphone applications and social platforms, video pushing of medication instructions on instant music video platforms such as TikTok and bilibili may be a new way to improve the MA of patients.
This study also had some limitations. First, this was a small sample study based on a single center. Although Changhai Hospital is the largest CP diagnosis and treatment center in China and even Asia, patients at our center are more representative only for East China. Small sample may also lead to some bias in the results of this study. In addition, patients who visited our center tended to be more severely ill and had better adherence than those in primary medical institutions. Therefore, the findings of our study may not be fully representative of the MA to PERT of other CP patients in other institutions. Second, we only used the C-MMAS-8 to measure patients’ MA and did not use other scales and data such as medication possession ratio and proportion of days covered for validation, which may lead to some bias of the MA results from the real situation. Third, although this study provided first-hand information on the adherence to PERT in Chinese CP patients, the limited number of factors influencing patients’ MA included in the analysis may have led to the results of this study was not novel. It is expected that the future studies can, based on our research, cooperate with more centers of different scales in China to carry out extensive and large-sample research, adopt multiple MA measurement methods, and incorporate more indicators such as patients’ disease knowledge, health literacy, self-efficacy, and indicators of patients’ exocrine pancreatic function et al. to further explore various subjective, objective, and disease-related factors of adherence to PERT in Chinese CP patients and validate the results of our study, providing a reference for the management of PERT.
Conclusions
This study revealed the status of adherence to PERT among patients with CP in East China through a mixed study design. Overall, the MA of East Chinese CP patients was poor, and the low education and income level were the contributing factors of poor MA. The qualitative analysis results showed that, seven themes associated with non-adherence included lack of knowledge, self-adjustment of PERT, lifetime of medication, side effects of PERT, forgetfulness, financial burdens, and accessibility issues. Healthcare providers should personalize medication strategies to improve the MA of patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNY:
-
Chinese Yuan
- CP:
-
Chronic pancreatitis
- MA:
-
Medication adherence
- MMAS-8:
-
Morisky Medication Adherence Scale
- PEI:
-
Pancreatic exocrine insufficiency
- PERT:
-
Pancreatic enzyme replacement therapy
References
Zhang, G. et al. Flavonoids prevent NLRP3 inflammasome activation and alleviate the pancreatic fibrosis in a chronic pancreatitis mouse model. Am. J. Chin. Med. 49, 2001–2015. https://doi.org/10.1142/S0192415X21500944 (2021).
Kichler, A. & Jang, S. Chronic pancreatitis: Epidemiology, diagnosis, and management updates. Drugs 80, 1155–1168. https://doi.org/10.1007/s40265-020-01360-6 (2020).
Kleeff, J. et al. Chronic pancreatitis. Nat. Rev. Dis. Primers 3, 17060. https://doi.org/10.1038/nrdp.2017.60 (2017).
Vege, S. S. & Chari, S. T. Chronic pancreatitis. N. Engl. J. Med. 386, 869–878. https://doi.org/10.1056/NEJMcp1809396 (2022).
Bang, U. C., Benfield, T., Hyldstrup, L., Bendtsen, F. & Beck Jensen, J.-E. Mortality, cancer, and comorbidities associated with chronic pancreatitis: A Danish nationwide matched-cohort study. Gastroenterology 146, 989–994. https://doi.org/10.1053/j.gastro.2013.12.033 (2014).
Kempeneers, M. A. et al. Natural course and treatment of pancreatic exocrine insufficiency in a nationwide cohort of chronic pancreatitis. Pancreas 49, 242–248. https://doi.org/10.1097/MPA.0000000000001473 (2020).
D’Haese, J. G. et al. Pancreatic enzyme replacement therapy in patients with exocrine pancreatic insufficiency due to chronic pancreatitis: A 1-year disease management study on symptom control and quality of life. Pancreas 43, 834–841. https://doi.org/10.1097/MPA.0000000000000131 (2014).
Lindkvist, B. et al. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology 12, 305–310. https://doi.org/10.1016/j.pan.2012.04.006 (2012).
Liu, Y. et al. Risk factor analysis and nomogram development for steatorrhea in idiopathic chronic pancreatitis. J. Dig. Dis. 23, 331–340. https://doi.org/10.1111/1751-2980.13102 (2022).
Duggan, S. N. et al. High prevalence of osteoporosis in patients with chronic pancreatitis: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 12, 219–228. https://doi.org/10.1016/j.cgh.2013.06.016 (2014).
de la Iglesia, D. et al. Pancreatic exocrine insufficiency and cardiovascular risk in patients with chronic pancreatitis: A prospective, longitudinal cohort study. J. Gastroenterol. Hepatol. 34, 277–283. https://doi.org/10.1111/jgh.14460 (2019).
Bresnahan, K. A. & Tanumihardjo, S. A. Undernutrition, the acute phase response to infection, and its effects on micronutrient status indicators. Adv. Nutr. 5, 702–711. https://doi.org/10.3945/an.114.006361 (2014).
de la Iglesia-Garcia, D. et al. Increased risk of mortality associated with pancreatic exocrine insufficiency in patients with chronic pancreatitis. J. Clin. Gastroenterol. 52, e63–e72. https://doi.org/10.1097/MCG.0000000000000917 (2018).
Löhr, J. M. et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United Eur. Gastroenterol. J. 5, 153–199. https://doi.org/10.1177/2050640616684695 (2017).
Zou, W.-B. et al. Guidelines for the diagnosis and treatment of chronic pancreatitis in China (2018 edition). Hepatobiliary Pancreat. Dis. Int. 18, 103–109. https://doi.org/10.1016/j.hbpd.2019.02.004 (2019).
Sikkens, E. C. M., Cahen, D. L., van Eijck, C., Kuipers, E. J. & Bruno, M. J. Patients with exocrine insufficiency due to chronic pancreatitis are undertreated: A Dutch national survey. Pancreatology 12, 71–73. https://doi.org/10.1016/j.pan.2011.12.010 (2012).
Srivoleti, P. et al. Provider differences in monitoring and management of exocrine pancreatic insufficiency in chronic pancreatitis. Pancreas 51, 25–27. https://doi.org/10.1097/MPA.0000000000001967 (2022).
Erchinger, F. et al. Pancreatic enzyme treatment in chronic pancreatitis: Quality of management and adherence to guidelines-A cross-sectional observational study. United Eur. Gastroenterol. J. https://doi.org/10.1002/ueg2.12276 (2022).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005).
Ruppar, T. M., Cooper, P. S., Mehr, D. R., Delgado, J. M. & Dunbar-Jacob, J. M. Medication adherence interventions improve heart failure mortality and readmission rates: Systematic review and meta-analysis of controlled trials. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.115.002606 (2016).
Barkin, J. A. et al. Frequency of appropriate use of pancreatic enzyme replacement therapy and symptomatic response in pancreatic cancer patients. Pancreas 48, 780–786. https://doi.org/10.1097/MPA.0000000000001330 (2019).
Crosby, J. et al. Gastrointestinal symptoms before and after total pancreatectomy with islet autotransplantation: The role of pancreatic enzyme dosing and adherence. Pancreas 44, 453–458. https://doi.org/10.1097/MPA.0000000000000266 (2015).
Khandelwal, N. et al. Economic impact of treatment adherence in exocrine pancreatic insufficiency (EPI) patients treated with pancreatic enzyme replacement therapy (PERT). Value Health 21, S85–S86 (2018).
Tandon, R. K., Sato, N. & Garg, P. K. Chronic pancreatitis: Asia-Pacific consensus report. J. Gastroenterol. Hepatol. 17, 508–518 (2002).
Yan, J. et al. Translation and validation of a Chinese version of the 8-item Morisky medication adherence scale in myocardial infarction patients. J. Eval. Clin. Pract. 20, 311–317. https://doi.org/10.1111/jep.12125 (2014).
Liu, Z. et al. Development of a nomogram to predict medication nonadherence risk in patients with rheumatoid arthritis. Am. J. Transl. Res. 14, 9057–9065 (2022).
Li, B.-R. et al. Risk factors for complications of pancreatic extracorporeal shock wave lithotripsy. Endoscopy 46, 1092–1100. https://doi.org/10.1055/s-0034-1377753 (2014).
Morisky, D. E., Ang, A., Krousel-Wood, M. & Ward, H. J. Predictive validity of a medication adherence measure in an outpatient setting. J. Clin. Hypertens. 10, 348–354 (2008).
Francis, J. J. et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol. Health 25, 1229–1245. https://doi.org/10.1080/08870440903194015 (2010).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. https://doi.org/10.1191/1478088706qp063oa (2006).
Khunti, K., Seidu, S., Kunutsor, S. & Davies, M. Association between adherence to pharmacotherapy and outcomes in type 2 diabetes: A meta-analysis. Diabetes Care 40, 1588–1596. https://doi.org/10.2337/dc16-1925 (2017).
Durand, H. et al. Medication adherence among patients with apparent treatment-resistant hypertension: Systematic review and meta-analysis. J. Hypertens. 35, 2346–2357. https://doi.org/10.1097/HJH.0000000000001502 (2017).
World health statistics 2021: monitoring health for the SDGs, sustainable development goals (World Health Organization, 2021) Licence: CC BY-NC-SA 3.0 IGO.
de Rijk, F. E. M. et al. Diagnosis and treatment of exocrine pancreatic insufficiency in chronic pancreatitis: An international expert survey and case vignette study. Pancreatology 22, 457–465. https://doi.org/10.1016/j.pan.2022.03.013 (2022).
Jalal, Z. et al. South Asians living in the UK and adherence to coronary heart disease medication: A mixed-method study. Int. J. Clin. Pharm. 41, 122–130. https://doi.org/10.1007/s11096-018-0760-3 (2019).
Rashid, M. A., Edwards, D., Walter, F. M. & Mant, J. Medication taking in coronary artery disease: A systematic review and qualitative synthesis. Ann. Fam. Med. 12, 224–232. https://doi.org/10.1370/afm.1620 (2014).
Al-Ganmi, A. H. A., Alotaibi, A., Gholizadeh, L. & Perry, L. Medication adherence and predictive factors in patients with cardiovascular disease: A cross-sectional study. Nurs. Health Sci. 22, 454–463. https://doi.org/10.1111/nhs.12681 (2020).
Rice, D. R. et al. Electronic pill bottles to monitor and promote medication adherence for people with multiple sclerosis: A randomized, virtual clinical trial. J. Neurol. Sci. 428, 117612. https://doi.org/10.1016/j.jns.2021.117612 (2021).
Pernell, B. M. et al. Improving medication adherence with two-way short message service reminders in sickle cell disease and asthma. A feasibility randomized controlled trial. Appl. Clin. Inform. 8, 541–559. https://doi.org/10.4338/ACI-2016-12-RA-0203 (2017).
Johnson, K. B. et al. The feasibility of text reminders to improve medication adherence in adolescents with asthma. J. Am. Med. Inform. Assoc. 23, 449–455. https://doi.org/10.1093/jamia/ocv158 (2016).
Morawski, K. et al. Association of a smartphone application with medication adherence and blood pressure control: The MedISAFE-BP randomized clinical trial. JAMA Intern. Med. 178, 802–809. https://doi.org/10.1001/jamainternmed.2018.0447 (2018).
Huang, Z. et al. A Smartphone app to improve medication adherence in patients with type 2 diabetes in Asia: Feasibility randomized controlled trial. JMIR Mhealth Uhealth 7, e14914. https://doi.org/10.2196/14914 (2019).
Cheiloudaki, E. & Alexopoulos, E. C. Adherence to treatment in stroke patients. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph16020196 (2019).
World Health Organization. Adherence to Long-Term Therapies: Evidence for Action (WHO, 2003).
Gutierrez, M. M. & Sakulbumrungsil, R. Factors associated with medication adherence of hypertensive patients in the Philippines: A systematic review. Clin. Hypertens. 27, 19. https://doi.org/10.1186/s40885-021-00176-0 (2021).
Ni, Z., Dardas, L., Wu, B. & Shaw, R. Cardioprotective medication adherence among patients with coronary heart disease in China: A systematic review. Heart Asia 11, e011173. https://doi.org/10.1136/heartasia-2018-011173 (2019).
Kucukarslan, S. N. et al. Exploring patient experiences with prescription medicines to identify unmet patient needs: Implications for research and practice. Res. Soc. Adm. Pharm. 8, 321–332. https://doi.org/10.1016/j.sapharm.2011.08.003 (2012).
Xu, F. et al. Medication adherence and its influencing factors among inflammatory bowel disease patients in China. Int. J. Gen. Med. 15, 4141–4149. https://doi.org/10.2147/IJGM.S359082 (2022).
Hu, W., Hu, S., Zhu, Y., Chen, H. & Chen, Y. Assessing oral medication adherence and identifying predictors of low adherence in Chinese inflammatory bowel disease patients. Patient Prefer. Adherence 14, 1083–1092. https://doi.org/10.2147/PPA.S250935 (2020).
Acknowledgements
The author thanked the First Affiliated Hospital of Naval Medical University and all the authors of the original studies.
Funding
This study was supported by the National Natural Science Foundation of China [No. 82070664 (LHH), No. 81801970 (GTL), and No. 82070668 (GTL)], and Programs of Shanghai Municipal Government [SHDC12021107 (ZSL)].
Author information
Authors and Affiliations
Contributions
Conceptualization, L.H., Y.Z. and D.W.; methodology, R.H., Y.Z. and C.C.; software, Y.Z., J.X. and D.W.; validation, L.H. and R.H.; formal analysis, Q.W., J.Y. and D.W.; investigation, Y.Z., R.H., Q.W., D.W. and C.C.; writing—original draft preparation, Y.Z. and R.H.; writing—review and editing, Z.L., G.L. and L.H.; supervision, Z.L. and L.H. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Y., Huang, RQ., Wu, QW. et al. Adherence to pancreatic enzyme replacement therapy among patients with chronic pancreatitis in East China: a mixed methods study. Sci Rep 13, 17147 (2023). https://doi.org/10.1038/s41598-023-44519-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-44519-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.