Abstract
Undesirable living environment may impose risk on myopia development. Furthermore, peripheral refractive error was suggested to contribute to juvenile eye growth modulation. This study aimed to investigate the interaction between peripheral refractive error and living environment in relation to central refractive status in Hong Kong schoolchildren. Central and peripheral refractive errors, axial length (AL), and corneal radius of curvature (CR) were measured in 573 schoolchildren (age 9.5 ± 0.9 years). The AL/CR ratio was used to represent the central refractive status, accounting for non-cycloplegic refraction. The relative peripheral refractive errors (RPRE) up to ± 20° eccentricities were converted into power vectors: spherical-equivalent error (SER) and J0 astigmatic components and fitted with quadratic equations. The second-order coefficients of SER (aSER) and J0 astigmatism (aJ0) and home size reported by parental questionnaires were analyzed to indicate their relationships with AL/CR. Our results showed that children with higher AL/CR lived in smaller homes (p = 0.01) and had a more hyperopic (p < 0.001) but less astigmatic RPRE (p = 0.01). We further analyzed the relationship between AL/CR with RPRE for children living in small (< 300 ft2), moderate (300–600 ft2), and large home sizes (> 600 ft2). Regardless of the home size, a higher AL/CR remained moderately correlated with a more hyperopic aSER (all p < 0.001). However, a higher AL/CR was associated with a more positive aJ0 only in children living in large homes, and the relationships were not significant for small and moderate home sizes. Linear regression models further indicated that home size was a significant moderator contributing to the relationship between AL/CR and aJ0. In conclusion, our results were consistent with previous studies, showing that children with axial myopia usually lived in smaller homes and had more hyperopic defocus and more positive J0 astigmatism. However, the relationship between peripheral astigmatism and axial refraction was modulated by the home size of Hong Kong schoolchildren. While peripheral astigmatism is hypothesized as a visual cue for axial refractive development in children, extrinsic environmental factors, such as home size, might interfere with the relationship and dominate refractive development.
Similar content being viewed by others
Introduction
Short-sightedness, or myopia, has been a global epidemic affecting billions1, and the prevalence is still rising2. Myopes, especially those with high myopia, are subject to irreversible vision loss3, leading to reduced productivity and quality of life4.
Environmental factors have consistently been addressed in the myopia literature, for instance the characteristics of the indoor and outdoor scenes5. In particular, the crowdedness and urbanicity of the living environment were associated with juvenile refractive error. The Sydney Myopia study reported that children living close to the city center, where the population density is higher, had a higher prevalence and degree of myopia6. Also, a flat-style type of housing in Sydney, as well as a taller residential building in China7, were associated with more myopia. A higher population density and smaller home size were also associated with a more myopic refractive error in Hong Kong8. Urbanization and limited living space are risk factors for myopia in the modern world.
The contribution of peripheral refractive errors to myopia development has attracted considerable attention over the past decades. Over the decades, studies reported an association between axial myopia and relative peripheral hyperopia9,10,11. These studies raised the question of whether visual inputs from the central, peripheral, or entire retina would be utilized and contribute to modulation of juvenile eye growth. Emerging evidence from animal studies indicates that the peripheral retina, rather than only the fovea centralis, plays a critical role. For examples, the peripheral retina was able to compensate for localized blurred signals by modulating regional eye growth12,13. In addition, even after eliminating the foveal input by laser-ablation, the eye was still able to detect the imposed optical defocus and modulate the growth towards the focal plane14. In clinical trials, several optical interventions showed promising myopia control effects by inducing peripheral myopic defocus to bring the focal plane in front of the retina15,16,17,18. Despite the convincing evidence from animal studies and clinical trials, the results from longitudinal observational studies failed to establish a solid causal relationship between the baseline peripheral refractive error and the subsequent myopia progression in children11,19,20. The current study addressed the gap in our understanding of the relationship between peripheral refractive error and myopia development. Specifically, we hypothesized that additional factors should be considered to elucidate the role of peripheral refractive error on myopia development.
Myopia is a multifactorial condition influenced by intrinsic and extrinsic factors, including peripheral refractive error and living environment. However, the interplay between these factors remains unclear. Our previous study has shown that children living in small homes are at a higher risk of developing myopia8,21, possibly because the living environment can introduce a different dioptric profile to the eye that might interact with the intrinsic peripheral refractive errors22. Our previous longitudinal study demonstrated that peripheral refractive error alone was not sufficient to predict myopia progression. However, after considering the environmental dioptric profile, peripheral refractive error became a significant contributor to myopia development. Building on these findings, we hypothesized that the impact of intrinsic peripheral refractive error on myopia progression would be inhibited by extrinsic environmental factors. Specifically, weak extrinsic environmental stimulation would increase the importance of intrinsic peripheral refractive error, while dominant environmental influences would diminish its role. However, our previous study was limited by a small sample (n = 50). To test this hypothesis, the current study examined Chinese schoolchildren’s peripheral refractive error stratified by the size of living space. Our aim was to elucidate the interaction between these intrinsic and extrinsic factors in modulating myopia, with a particular focus on the differential effects of peripheral refractive error and home sizes. Our results would provide valuable insights into the mechanisms underlying myopia and contribute to the development of future interventions.
Materials and methods
Study design and population
This study was conducted in five Hong Kong local primary schools by random-cluster sampling stratified according to the population density due to its potential association with the myopia6,8: two schools from low (< 10 k persons/km2) and mid (10–30 k persons/km2), respectively, and one school from high (> 30 k persons/km2) population density regions. A total of 635 children participated, of whom 43 were excluded because of abnormal visual acuity (pinhole visual acuity worse than LogMAR 0.0 equivalent, n = 3), corneal opacity (n = 1), strabismus (n = 6), or receiving myopia control intervention, such as orthokeratology, progressive lenses, or dual-focus contact lenses (n = 33). An additional 19 children were excluded because their pupils were too small for peripheral refraction. Therefore, 573 of them had completed peripheral refraction up to 20° eccentricity and were included for analysis. Their age and refractive status were comparable with the excluded data (independent t-test, all p > 0.35). The experimental procedures followed the tenets of the Declaration of Helsinki and were approved by the Human Subjects Ethics Sub-committee of The Hong Kong Polytechnic University. Informed consent and written assent were obtained from the parents/legal guardians and subjects, respectively.
Data collection procedures
Central and peripheral refractive errors were measured using an open-field autorefractor (Shin-Nippon, NVision K5001, Japan) operated by a registered optometrist at the school campus during school teaching hours. No cycloplegic agent was instilled to avoid disturbing children’s classroom learning. Subjects were instructed to binocularly fixate at Maltese crosses (angular size: 2.4°) located at the central, ± 10°, and ± 20° eccentricities along the horizontal visual field at a viewing distance of 6 m. The selected central field size was based on the findings of previous studies indicating these retinal regions were the most responsive to optical defocus23,24,25, as well as avoiding the location of the optic nerve head (i.e., the blind spot) at approximately 15° eccentricity of the temporal visual field26. Subjects were asked to keep their head stationary on the headrest and turn their eyes to the distant fixation targets during central and peripheral objective refractions. Refraction was carried out only after the subject achieved steady fixation as monitored through the display of the autorefractor. For each subject, the whole measurement at all five eccentricities (i.e., nasal 20°, nasal 10°, central, temporal 10°, and temporal 20° fields) was completed within 2 min. Measurements were repeated until five repeatable readings (± 0.50 DS and ± 0.50 DC) for each field location were obtained. The on-axis axial length (AL) and corneal radius of curvature (CR) were measured using an optical biometer (IOLMaster, Carl Zeiss Meditec, Germany) operated by a trained ophthalmic assistant. Five measurements with a signal-to-noise ratio > 2 were taken. The averaged refraction and ocular biometry data were used for analyses.
Data processing and statistical analysis
Refractive errors obtained from autorefraction were decomposed into vector components, i.e., the spherical-equivalent refraction (SER), J0, and J45 astigmatic components27:
where S is the spherical power, C is the cylindrical power, and α is the axis of the negative sphero-cylindrical form (\(S+C\times \alpha\)). SER indicates the dioptric position of the circle of least confusion. Positive J0 indicates the tendency of with-the-rule astigmatism while negative J0 indicates the tendency of against-the-rule astigmatism. J45 indicates the tendency of oblique astigmatism, by which a positive value indicates tendency towards 45° meridian while negative value indicates tendency towards 135° meridian. Relative peripheral refractive error (RPRE) was calculated by subtracting the vector components of the central field from the peripheral fields. Although the accommodation was not pharmacologically controlled, it was reported to have minimal effect on the RPRE profile.
The refractive profiles of SER and J0 along the horizontal visual field were modeled using a quadratic equation, \({a(Eccentricity-b)}^{2}+c\), with the built-in “LINEST” function in Microsoft Excel (Microsoft 365, Redmond, WA, USA). The resulting second-order coefficients were obtained (i.e., aSER and aJ0) and were used to quantify the change of refractive errors across the visual field10,28. A negative second-order coefficient indicates a more myopic blur for aSER and more against-the-rule astigmatism for aJ0, while positive second-order coefficients reveal more hyperopic defocus and with-the-rule astigmatism. Due to the low magnitude, J45 was omitted in the analysis. For the present analysis, the first- (b) and zero-order (c) coefficients, which indicated the symmetry and y-intercept of the refractive profile, were excluded, as our focus was to characterize the variation of refractive profile across eccentricities.
In this study, non-cycloplegic refraction was used to assess children’s central spherical refractive status, but uncontrolled accommodation might over-estimate the magnitude of myopia. Therefore, axial length to corneal radius of curvature (AL/CR) ratio was chosen as the primary outcome instead of non-cycloplegic SER. This decision was made because AL/CR ratio was strongly associated with cycloplegic SER29 and independent to ocular accommodation30. In addition to AL, which is correlated with myopia resulting from excessive elongation of the eyeball, AL/CR ratio also accounts for the variations in corneal power among emmetropic and ametropic eyes29,30. Consequently, AL/CR ratio provides a more comprehensive measure of central spherical refractive status. Non-cycloplegic SER and AL were used as secondary outcomes to supplement the refractive and ocular biometrical findings.
All statistical procedures were performed using SPSS (IBM, ver. 22, United States). As data from right and left eyes were strongly correlated, only the data from the right eye were presented in this study. The AL/CR, AL, and SER were compared across three home size groups: < 300 ft2, 300–600 ft2, and > 600 ft2, obtained from a parental questionnaire, using one-way analysis of co-variance (ANCOVA) controlled for age. The age-controlled relationship between central refractive and biometric status (i.e., AL/CR, AL, and SER) and the second-order coefficients of peripheral refractive errors (i.e., aSER and aJ0) was analyzed in regression analyses (Variance inflation factors < 2.0) stratified by home size. A moderator term was created to investigate the interaction effect between home size and the second-order coefficients as the primary analysis. In addition, a Fisher’s R-to-Z transformation, followed by a χ2-test for heterogeneity, was applied to compare the age-controlled partial correlation coefficients for central and peripheral refractive errors in each home size group as a secondary analysis.
Results
Demographics, refraction, and relationship with home size
The demographic information, refractive status, and ocular biometry of the subjects are shown in Table 1. Subjects were stratified into three home size groups. While no significant differences in age (F2,570 = 0.80, p = 0.45) and the proportion of gender (χ22,570 = 1.48, p = 0.48) were found among the three groups, home size had a significant aged-adjusted effect on AL/CR (F2,570 = 4.46, p = 0.01) and SER (F2,570 = 7.77, p < 0.001) as previously reported, except AL (F2,570 = 2.60, p = 0.08) which could be due to a reduced statistical power owing to a smaller sample size than the previous study. For astigmatism at the central field, home size was neither associated with J0 (One-way ANCOVA, p = 0.06) or J45 (One-way ANCOVA, p = 0.39) after controlled for age.
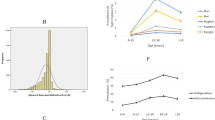
Peripheral refractive profiles in myopes and non-myopes
Regardless of the home size, peripheral refractive profile alone was different in children with and without myopia. Figure 1 shows the respective peripheral refractive profile for children with AL/CR < 3.00 versus those with AL/CR ≥ 3.00, corresponding to approximately − 0.38 D of SER (Supplementary Fig. S3) stratified by home sizes. Consistent with previous reports, a more hyperopic peripheral refractive error was observed in children with a more myopic axial refractive error in all home sizes. Particularly, peripheral SER was significantly more myopic in children with AL/CR < 3.00 (aSER − 0.51 ± 1.29) than those with AL/CR ≥ 3.00 (aSER 0.71 ± 1.57, t = − 10.12, p < 0.001). On the other hand, differences for peripheral J0 was less prominent in children with AL/CR < 3.00 (aJ0 − 1.29 ± 0.89) compared with those with AL/CR ≥ 3.00 (aJ0 − 1.11 ± 0.80, t = − 2.52, p = 0.01).
Peripheral refractive profile and home size
In multiple regression analyses controlled with age, all the second-order coefficients were significantly correlated with AL/CR (Table 2), in which a higher AL/CR was moderately associated with a more hyperopic and weakly associated with a less astigmatic blur. A similar trend was also observed in AL and SER (Supplementary Tables S1 and S2).
Figures 1 and 2 show the relationship between AL/CR and the second-order coefficients of relative peripheral refractive errors, stratified by home sizes. Across all home size groups, children with higher AL/CR exhibited more positive aSER, indicating a greater hyperopic shift in the peripheral visual field than those with lower AL/CR (all p < 0.001). Notably, the slopes of linear regression lines between AL/CR ratio and aSER were similar across all three home size groups (Fig. 2A). On the other hand, for children living in large homes (> 600 ft2), those with lower AL/CR exhibited a more negative aJ0, indicating a greater against-the-rule astigmatic shift towards the peripheral fields than those with higher AL/CR (Fig. 1B and 2B). The relationship remained significant even after controlling for multiple comparison via Bonferroni adjustment (Table 2). However, for children living in small (< 300 ft2) and medium (300–600 ft2) homes, the relationships between AL/CR and aJ0 were insignificant (p = 0.40). Our linear regression models confirmed these observations and revealed that home size significantly moderated the relationship between AL/CR and aJ0, with a significant interaction effect (p = 0.02). However, no such interaction effect was found for aSER (p = 0.69). A similar trend was also observed in SER (Supplementary Fig. S1), although the results did not reach statistical significance for AL (Supplementary Fig. S2).
Relationships between AL/CR ratio against the second-order coefficients of relative peripheral refractive errors. (A) Spherical equivalent refraction—aSER; (B) J0 astigmatic component—aJ0. Home sizes are represented by red triangles and solid lines: < 300 ft2; green squares and dotted lines: 300–600 ft2; and blue circles and dashed lines: > 600 ft2.
Discussion
The current study investigated the effect of living space and peripheral refractive error on central refractive status (i.e., AL/CR) in a schoolchildren population. Our results found that the relationships between AL/CR and peripheral SER remained relatively consistent across children living in different home sizes. On the other hand, the correlation between AL/CR and peripheral J0 was significant only in children residing in large homes. This relationship was abolished in children living in small and medium homes. Our results highlighted a significant interaction between the home size and the relative peripheral astigmatic profile, characterized by the second-order coefficient obtained from quadratically regressing peripheral J0.
It has been proposed that the two perpendicular focal planes created by peripheral astigmatism could provide the retina with a cue to differentiate the sign of optical defocus. By comparing the output signal strength of the orientation-tuned neurons, the retina may be able to utilize this signal to direct the eye growth towards the focal plane. Astigmatism is a major component of peripheral refractive error, for which the magnitude could be greater than 10 D at 60° eccentric visual field31,32,33. While most recent studies focused on peripheral SER, few have investigated the relationship between peripheral astigmatism and axial refraction, even rarer in children who are prone to myopia progression. Existing clinical data and animal experiments have demonstrated supportive evidence that uncorrected or lens-induced astigmatism could disrupt the retinal image quality and natural eye-growth process34,35,36. In addition, the peripheral astigmatism was found to be negatively, but weakly, correlated with axial myopia10. In a longitudinal study, children who were myopic, as well as those who turned myopic, had less peripheral astigmatism at baseline37, suggesting a role of adequate peripheral astigmatism in halting juvenile eye growth. However, the results could not be repeated in a later study20. The current study may provide further evidence on the peripheral astigmatic error being a contributing factor to the development of axial myopia38,39 in children by revealing a significant relationship between peripheral astigmatism and central refractive error.
As shown in Fig. 1, the refractive profiles shared similar characteristics, with greater AL/CR group differences observed in peripheral SER than in J0. As for the relationship with AL/CR, aSER showed a moderate correlation (Table 2), indicating that a more hyperopic peripheral SER may be attributed to posterior stretching during the myopization, as well as the relatively prolate eye shape in myopes40. Owing to the independence between AL/CR and aJ0 in the overall sample, the hypothesis may not be held true that peripheral astigmatism, only when analyzed alone, would provide optical cues to guide the vision-dominated eye growth. Our findings provided insight from the environmental perspective and are discussed in the followings.
Consistent with our previous report on AL and non-cycloplegic SER8, a lower AL/CR was also associated with a less constricted living space. Owing to the interrelationship, the peripheral refractive profiles were expected to be more hyperopic in children living in a more constricted space due to a more myopic central refractive error, which was true for peripheral SER (p = 0.01, statistics shown in Supplementary Table S3). However, peripheral aJ0 was independent of home size, as well as having weak correlations with AL/CR regardless of home sizes. As there was a significant interaction effect between peripheral J0 profile and home size on AL/CR, it is speculated that the living environment interacted with the peripheral astigmatism and contributed to the central refractive error, of which the effect was also demonstrated in a previous longitudinal study investigating the near work environment at home. This interaction did not appear to come from the direct impact of home size on peripheral astigmatism itself, as both axial and peripheral astigmatisms were similar among all home size groups (Supplementary Table S3). It is deduced that the peripheral astigmatism may be an optical cue for children under a spacious environment with less extrinsic dioptric stimuli. On the other hand, the intrinsic peripheral refractive error, particularly the peripheral astigmatism, had subtle effect for children living in a constricted space, which exerts a greater extrinsic stimulation.
Although accommodation was not pharmacologically controlled by the cycloplegic agent, it is shown to have limited effect on the measurement of the RPRE, which is one of the primary outcomes of this study. Both the central and peripheral fixation targets were positioned equidistant at 6 m away from the eye, only creating a 0.17 D accommodative stimulus at each eccentricity, which was negligible in clinical condition. Assuming that the level of accommodation remained constant during refractive measurement at each eccentricity, it is unlikely to have a significant impact on the RPRE, which is determined by the difference between central and peripheral refractive errors. The refractive status was presented based on the AL/CR ratio, a biometric parameter that is suggested to be independent of the accommodative status29,30. The strong correlation between the AL/CR ratio and central M (Supplementary Fig. S3), as consistent with previous epidemiological studies performed under cycloplegic condition29,41, also suggested an adequate control of accommodation when performing peripheral refraction. However, the relationship between AL/CR and central SER is non-linear, especially in extreme cases, that careful interpretation of the results is warranted. The primary analysis was based on the quadratic coefficients of peripheral refractive profile obtained by quadratic regressions. Generally, all the fitted curves achieved high R-squares (close to or above 0.90). However, to enhance the representativeness of the fitted curves, it may be needed to increase the number of coordinates (i.e., the number of eccentricities measured across the visual field). Lastly, while home size was the variable of interest in the current study, it may not fully capture the various visual scenes that can impose myopiagenic stimulation on the eye throughout the day42. Further studies incorporating personalized sensors may be warranted to observe myopiagenic factors in daily life.
Conclusions
To conclude, this study provided representative data of the peripheral refractive profile of Hong Kong schoolchildren by adopting a random-cluster sampling, where myopia has reached an epidemic proportion43,44, and also revealed a significant interaction between living environment and peripheral astigmatism in relation to axial refractive error in Hong Kong Chinese schoolchildren. Our findings has inputted an environmental factor to evaluate the contribution of peripheral refractive error to the ocular development, as previous researchers have proposed that the retina might distinguish the sign of defocus by comparing orientational input in the periphery38,39,45. For instance, a positive defocus, which brings the peripheral astigmatic foci forward, would emphasize the radial component of the retinal image, and increase the retinal signal output as demonstrated in electroretinography studies25,46. Further study is needed to understand whether and how other environmental factors, for instance spatial frequency and chromaticity, would contribute to the development and progression of myopia.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Morgan, I. G., Ohno-Matsui, K. & Saw, S. M. Myopia. Lancet 379, 1739–1748 (2012).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016).
Verkicharla, P. K., Ohno-Matsui, K. & Saw, S. M. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol. Opt. 35, 465–475 (2015).
Naidoo, K. S. et al. Potential lost productivity resulting from the global burden of myopia: Systematic review, meta-analysis, and modeling. Ophthalmology 126, 338–346 (2019).
Choi, K. Y., Chan, S. S.-H. & Chan, H. H.-L. The effect of spatially-related environmental risk factors in visual scenes on myopia. Clin. Exp. Optom. 105, 353–361 (2022).
Ip, J. M., Rose, K. A., Morgan, I. G., Burlutsky, G. & Mitchell, P. Myopia and the urban environment: Findings in a sample of 12-year-old Australian school children. Invest. Ophthalmol. Vis. Sci. 49, 3858–3863 (2008).
Wu, X. et al. Housing type and myopia: The mediating role of parental myopia. BMC Ophthalmol. 16, 151 (2016).
Choi, K. Y. et al. Childhood exposure to constricted living space: A possible environmental threat for myopia development. Ophthalmic Physiol. Opt. 37, 568–575 (2017).
Hoogerheide, J., Rempt, F. & Hoogenboom, W. P. Acquired myopia in young pilots. Ophthalmologica 163, 209–215 (1971).
Atchison, D. A., Pritchard, N. & Schmid, K. L. Peripheral refraction along the horizontal and vertical visual fields in myopia. Vis. Res. 46, 1450–1458 (2006).
Mutti, D. O. et al. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Investig. Ophthalmol. Vis. Sci. 52, 199–205 (2011).
Wallman, J., Gottlieb, M. D., Rajaram, V. & Fugate-Wentzek, L. A. Local retinal regions control local eye growth and myopia. Science 237, 73–77 (1987).
Smith, E. L., Hung, L. F., Huang, J. & Arumugam, B. Effects of local myopic defocus on refractive development in monkeys. Optom. Vis. Sci. 90, 1176–1186 (2013).
Smith, E. L., Hung, L. F. & Huang, J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vis. Res. 49, 2386–2392 (2009).
Cho, P. & Cheung, S. W. Retardation of myopia in orthokeratology (ROMIO) study: A 2-year randomized clinical trial. Investig. Ophthalmol. Vis. Sci. 53, 7077–7085 (2012).
Lam, C. S. Y., Tang, W. C., Tse, D. Y., Tang, Y. Y. & To, C. H. Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: A 2-year randomised clinical trial. Br. J. Ophthalmol. 98, 40–45 (2014).
Choi, K. Y. et al. Evaluation of an optical defocus treatment for myopia progression among schoolchildren during the COVID-19 pandemic. JAMA Netw. Open 5, e2143781–e2143781 (2022).
Lam, C. S. et al. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: Results of a 3-year follow-up study. Br. J. Ophthalmol. 106, 1110–1114 (2021).
Atchison, D. A. et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Investig. Ophthalmol. Vis. Sci. 56, 6162–6170 (2015).
Lee, T. T. & Cho, P. Relative peripheral refraction in children: Twelve-month changes in eyes with different ametropias. Ophthalmic Physiol. Opt. 33, 283–293 (2013).
Choi, K. Y., Mok, A. Y. T., Do, C. W., Lee, P. H. & Chan, H. H. I. The diversified defocus profile of the near-work environment and myopia development. Ophthalmic Physiol. Opt. 40, 463–471 (2020).
Choi, K. Y. & Chan, H.H.-L. Extrinsic and intrinsic factors regulating juvenile refractive development and eye growth. Investig. Ophthalmol. Vis. Sci. 62, 21–21 (2021).
Ho, W. C. et al. Sign-dependent changes in retinal electrical activity with positive and negative defocus in the human eye. Vis. Res. 52, 47–53 (2012).
Chin, M. P., Chu, P. H. W., Cheong, A. M. Y. & Chan, H. H. L. Human electroretinal responses to grating patterns and defocus changes by global flash multifocal electroretinogram. PLoS ONE 10, e0123480 (2015).
Fung, M. M., Choi, K. Y. & Chan, H. H. The effect of simultaneous dual-focus integration on the global flash multifocal electroretinogram in the human eye. Ophthalmic Physiol. Opt. 41, 171–178 (2021).
Wang, M. et al. Impact of natural blind spot location on perimetry. Sci. Rep. 7, 1–9 (2017).
Thibos, L. N., Wheeler, W. & Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 74, 367–375 (1997).
Verkicharla, P. K., Suheimat, M., Schmid, K. L. & Atchison, D. A. Peripheral refraction, peripheral eye length, and retinal shape in myopia. Optom. Vis. Sci. 93, 1072–1078 (2016).
He, X. et al. Axial length/corneal radius ratio: Association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE 10, e0111766 (2015).
Grosvenor, T. & Scott, R. Role of the axial length/corneal radius ratio in determining the refractive state of the eye. Optom. Vis. Sci. 71, 573–579 (1994).
Gustafsson, J., Terenius, E., Buchheister, J. & Unsbo, P. Peripheral astigmatism in emmetropic eyes. Ophthalmic Physiol. Opt. 21, 393–400 (2001).
Millodot, M. Effect of ametropia on peripheral refraction. Am. J. Optom. Physiol. Opt. 58, 691–695 (1981).
Mathur, A. & Atchison, D. A. Peripheral refraction patterns out to large field angles. Optom. Vis. Sci. 90, 140–147 (2013).
Gwiazda, J., Grice, K., Held, R., McLellan, J. & Thorn, F. Astigmatism and the development of myopia in children. Vis. Res. 40, 1019–1026 (2000).
Kee, C. S., Hung, L. F., Qiao-Grider, Y., Roorda, A. & Smith, E. L. Effects of optically imposed astigmatism on emmetropization in infant monkeys. Investig. Ophthalmol. Vis. Sci. 45, 1647–1659 (2004).
Leung, T. W., Lam, A. K. C. & Kee, C. S. Ocular aberrations and corneal shape in adults with and without astigmatism. Optom. Vis. Sci. 92, 604–614 (2015).
Sng, C. C. A. et al. Change in peripheral refraction over time in Singapore Chinese children. Investig. Ophthalmol. Vis. Sci. 52, 7880–7887 (2011).
Charman, W. N. Keeping the world in focus: How might this be achieved?. Optom. Vis. Sci. 88, 373–376 (2011).
Atchison, D. A. & Rosén, R. The possible role of peripheral refraction in development of myopia. Optom. Vis. Sci. 93, 1042–1044 (2016).
Verkicharla, P. K., Mathur, A., Mallen, E. A. H., Pope, J. M. & Atchison, D. A. Eye shape and retinal shape, and their relation to peripheral refraction. Ophthalmic Physiol. Opt. 32, 184–199 (2012).
Calver, R., Radhakrishnan, H., Osuobeni, E. & O’Leary, D. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol. Opt. 27, 584–593 (2007).
Choi, K. Y., Chan, S. S. H. & Chan, H. H. L. The effect of spatially-related environmental risk factors in visual scenes on myopia. Clin. Exp. Optom. https://doi.org/10.1080/08164622.08162021.01983400 (2021).
Lam, C. S. Y., Lam, C. H., Cheng, S. C. & Chan, L. Y. Prevalence of myopia among Hong Kong Chinese schoolchildren: Changes over two decades. Ophthalmic Physiol. Opt. 32, 17–24 (2012).
Yam, J. C. et al. High prevalence of myopia in children and their parents in Hong Kong Chinese population: The Hong Kong children eye study. Acta Ophthalmol. (Copenh.) 98, e639–e648 (2020).
Flitcroft, D. I. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 31, 622–660 (2012).
Backhouse, S., Fox, S., Ibrahim, B. & Phillips, J. R. Peripheral refraction in myopia corrected with spectacles versus contact lenses. Ophthalmic Physiol. Opt. 32, 294–303 (2012).
Funding
This study was supported by the Research Centre for SHARP Vision (RCSV) of The Hong Kong Polytechnic University (1-BBC1), the Internal Funds of The Hong Kong Polytechnic University (BD5F, 1-ZVS4), the External Fund of The University of Hong Kong (H-ZL21), Lee Hysan Foundation and Sau Ching Charity Foundation (R-ZH5T), and the InnoHK initiative by the Hong Kong Special Administrative Region Goverment. The funding organizations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Conceptualization, K.Y.C., T.W.L., and H.H.C.; methodology; software; validation; formal analysis; data curation, K.Y.C. and T.W.L.; investigation, K.Y.C.; resources, H.H.C.; writing—original draft preparation, K.Y.C.; writing—review and editing, K.Y.C., T.W.L., and H.H.C.; visualization, K.Y.C.; supervision; project administration; funding acquisition, H.H.C. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, K.Y., Leung, T.W. & Chan, H.HL. Size of living space as a moderator for central and peripheral refractions in children. Sci Rep 13, 10797 (2023). https://doi.org/10.1038/s41598-023-37454-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37454-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.