Abstract
High plasma matrix metalloproteases-9 (MMP-9) levels have been reported in Fragile X Syndrome in a limited number of animal and human studies. Since the results obtained are method-dependent and not directly comparable, the clinical utility of MMP-9 measurement in FXS remains unclear. This study aimed to compare quantitative gel zymography and ELISA and to determine which method better discriminates abnormal MMP-9 levels of individuals with FXS from healthy controls and correlates with the clinical profile. The active and total forms of MMP-9 were quantified respectively, by gel zymography and ELISA in a cohort of FXS (n = 23) and healthy controls (n = 20). The clinical profile was assessed for the FXS group using the Aberrant Behavior Checklist FXS adapted version (ABC-CFX), Adaptive Behavior Assessment System (ABAS), Social Communication Questionnaire (SCQ), and Anxiety Depression and Mood Scale questionnaires. Method comparison showed a disagreement between gel zymography and ELISA with a constant error of − 0.18 [95% CI: − 0.35 to − 0.02] and a proportional error of 2.31 [95% CI: 1.53 to 3.24]. Plasma level of MMP-9 active form was significantly higher in FXS (n = 12) as compared to their age-sex and BMI matched controls (n = 12) (p = 0.039) and correlated with ABC-CFX (rs = 0.60; p = 0.039) and ADAMS (rs = 0.57; p = 0.043) scores. As compared to the plasma total form, the plasma MMP-9 active form better enables the discrimination of individuals with FXS from controls and correlates with the clinical profile. Our results highlight the importance of choosing the appropriate method to quantify plasma MMP-9 in future FXS clinical studies.
Similar content being viewed by others
Introduction
Fragile X Syndrome (FXS) is the most common monogenic cause of autism spectrum disorder (ASD) and intellectual disability (ID)1,2. FXS is caused by mutations of the X-linked Fragile X messenger ribonucleoprotein 1 (FMR1)3,4. In the majority of cases, it results from an abnormal trinucleotide repeat (CGG) in the promotor region of FMR15 leading to a deficit of X messenger ribonucleoprotein, or FMRP. FMRP is a ubiquitous RNA-binding protein, highly expressed in the brain6,7, where it controls the translation of up to 4% of RNAs coding proteins8 essential for synaptic plasticity9. Hence, the absence of FMRP leads to a hyper-synthesis of dendritic proteins resulting in immature, thin, and long dendritic spines, which are in part responsible for the neurodevelopmental impairment of FXS10,11,12.
Matrix metalloproteinase 9 (MMP-9), a member of the MMPs family, is a dendritic protein whose expression is tightly regulated by FMRP in neurons13. Specifically, upon synaptic stimulation of the glutamate receptor (mGluR), FMRP dissociates from the MMP-9 mRNA complex allowing MMP-9 translation to occur14. In FXS, the absence of FMRP leads to excessive synthesis of MMP-9. Studies in Fmr1 knock‐out (KO) mice highlight the implication of MMP-9 in the FXS pathophysiology13,14,15. Indeed, high MMP-9 levels have been reported in brain tissue and plasma of FXS animal models and humans. Moreover, treatment with minocycline (a tetracycline derivative) an inhibitor of circulating metalloproteinases, reduced MMP-9 activity, restored the synaptic development in Fmr1 KO mice, and improved aberrant behavior of Fmr1 KO mice and FXS patients16,17,18.
MMP-9 is synthesized as an inactive proenzyme (pro-MMP-9, 92 kD) that requires removal of the pro-domain to achieve the active form (MMP-9, 87 kD). The latter is a Zn2+ dependent endopeptidase that degrades collagen type IV substrate19,20. Different methods have been applied to quantify MMP-9 total (pro and active form) and active forms in brain tissues or plasma. Specifically, gelatin-based zymography16,21 measures measure both, the pro-MMP-9 and the active forms. Whereas, Enzyme-Linked Immunosorbent Assays (ELISA)14 and Western Blot22 measure the total form.
Studies in Fmr1 KO mice had shown an increase of both, total and active MMP-9 forms in the brain15,22,23. To the best of our knowledge, only two studies focused on MMP-9 measurements in individuals with FXS. The first showed an increase of MMP-9 total form in post-mortem brains (measured by Western blotting) in eight individuals with FXS as compared to nine controls22. The second study revealed an increase of plasma MMP-9 active form (as measured by semiquantitative gel zymography) of ten individuals with FXS as compared to eight age and sex-matched controls16. Moreover, plasma MMP-9 has been suggested as a potential biomarker to monitor outcomes of clinical trial in FXS24,25. To the best of our knowledge, no study compared the clinical significance of plasma total versus active MMP-9 forms in FXS.
The present work focused on the quantification of plasma total and active MMP-9 forms using, respectively, ELISA and gel zymography in individuals with FXS and healthy controls. Our objectives were to compare the two methods in order to determine which MMP-9 plasma form (total vs. active form) enables the best discrimination of individuals with FXS from controls and correlates better to the clinical profile.
Materials and methods
Study population
The study population is a sub-cohort of the LipidX study comprising 23 individuals with FXS(diagnosis confirmed by southern blot and polymerase chain reaction) and 20 healthy controls26. FXS participants were recruited at the FXS clinic located at CIUSSS de l’Estrie-CHUS, while controls were recruited via local community. Admissibility criteria were previously reported26. All participants gave their written informed consent before participating in the study. The project was performed according to the protocol approved by the Ethics Board of the Research Center of the Centre Hospitalier Universitaire de Sherbrooke, Canada (Project number 2020–3552). The study was performed in accordance with the Declaration of Helsinki. Blood samples were collected in K2EDTA tubes (BD Vacutainer®). Plasma was recovered following successive centrifugations (300 X g for 10 min and 2400 × g for 15 min to remove all cellular components) and stored at − 20 °C. FMRP was performed on whole cell extracts from platelets (pg/106 platelets), by Western blot as previously prescribed27.
Gel zymography
The gel zymography protocol has been previously described21,28. Briefly, 1 µl of plasma was diluted in Laemmli buffer and loaded on an 8% polyacrylamide gel (SDS-PAGE) containing 2 mg/ml gelatin. Following electrophoretic separation, gels were washed twice for 30 min in 2.5% Triton X-100, 50 mM Tris-HCL-PH 7.5, 5 mM CaCl2 and 1 µM ZnCl2 and then incubated for 18 h at 37 °C in 50 mM Tris-HCl-pH 7.5, 5 mM CaCl2, 1 µM ZnCl2, 1% Triton X100 buffer, with gentle agitation. Proteins were stained with Coomassie Brilliant Blue in 40% methanol for 45 min and distained in 40% methanol and 10% acetic acid for 30 min. The gels were scanned on a BIORAD; ChemiDoc™ MP Imaging System. Areas of enzyme activity (clear bands over the blue dark background) were quantified in Image J software29. Only the active form of MMP-9 at 82 kD (identified with molecular weight standards) was quantified. The recombinant human MMP-9 standard (Abcam© Inc: Natural human MMP-9 protein: proenzyme monomer, N° 157,344) was first activated with 1 mM 4-aminophenylmercuric acetate (APMA) and then used for quantification as calibrator in a standard curve within the range of 100 pg/well to 600 pg/well. Samples were quantified in duplicates and a positive plasma control was carried on every gel to monitor the reproducibility of the assay.
Immunoassay ELISA
ELISA immunoassays were performed according to the manufacturer's instruction (R&D systems) (Catalog#DY911-05). Briefly, the standard curve was obtained using serial dilutions of recombinant human MMP-9 (quantification range: 31.3 to 2000 pg/ml). Plasma samples were diluted 1/1000 in phosphate buffered saline (PBS) containing 1% bovine serum albumin (BSA).
Clinical profile
The clinical profile was assessed using the following questionnaires: Aberrant Behavior Checklist-Community (ABC-C), Adaptive Behavior Assessment System (ABAS), Social Communication Questionnaire (SCQ), and Anxiety Depression and Mood Scale (ADAMS).
The ABC-C was developed to measure aberrant behavioral among individuals with ID30. This questionnaire has been validated in the FXS population as a six-factor structure known as the FXS version of ABC-C (ABC-CFX)31. It uses a 58-items rating scale evaluating six behavior domains: irritability, hyperactivity, social unresponsive, social avoidance, stereotypy, and inappropriate speech. Each item is rated from 0 to 3 as follow: 0 (not at all a problem); 1 (slight problem); 2 (moderately serious problem); 3 (severe problem).
The ABAS-II questionnaire evaluates adaptive behavior and skills, categorised in three domains including conceptual, social, and practical. Each item is scored as follow: 0 (not able); 1 (never or rarely); 2 (sometimes) and 3 (always or almost always)32.
The SCQ is a screening questionnaire for ASD composed of 40 questions (yes/no) evaluating language, communication, reciprocal social interaction, stereotyped and repetitive patterns of behavior33.
The ADAMS questionnaire is used to assess behavior-based affective symptoms of individuals with ID older than 10 years old. It consists of 29 items clustered into five subscales: hyperactive behavior, depressed mood, social avoidance general anxiety, and obsessive/compulsive behavior.
Each item is scored from 0 (behavior has not occurred or is not a problem) to 3 (behavior occurs a lot or is a severe problem)34.
Statistical analysis
All statistics were performed in GraphPad Prism 8. For the ELISA assay, the concentration of MMP-9 was calculated using a four-parameter logistic function (4-PL). The distribution of each data was tested by D'Agostino & Pearson test and the Shapiro–Wilk test. Deming (Model II) linear regression was used to compare the two analysis methods and the Bland–Altman (BA) to compare the measurements of the same variable by both methods. Spearman’s rank correlation was performed to evaluate the association between MMP-9 activity and the clinical profile. A false discovery (FDR) adjusted p-value of 0.05 was used as a statistical significance threshold.
Ethics approval and consent to participate
The project was approved by the Ethics Board of the Research Center of the Centre Hospitalier Universitaire de Sherbrooke, Canada. All participants gave their written informed consent before participating in the study.
Results
Study population
Our study population included 23 individuals with FXS and 20 healthy controls. Males represented the majority of both groups with a higher representation in FXS than in controls (87% vs. 57%). 14 individuals with FXS were under medication, with 10 of them taking at least 2 medications. The latter included: antipsychotics, selective serotonin reuptake inhibitors and stimulants. None of the participants experienced or reported an acute illness. The FXS group had a higher body mass index (BMI) as compared to controls (26 vs. 21.9 kg/m2). In a subgroup of 12 FXS participants matched for age and sex with 12 healthy controls, the BMI was not significantly different between the groups. Characteristics of participants are shown in Table 1.
Method comparison
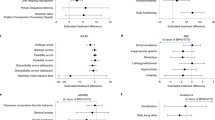
Based on the ability of MMP-9 and MMP-2 to degrade gelatin, gel zymography allowed the identification of their active forms (Fig. 1A). Only the active form of MMP-9 (87 KD) was quantified in the present study. The linearity of the standard curve for gel zymography obtained within a range of 100 to 600 pg of MMP-9 per well (corresponding to plasma concentration ranging from 0.1 to 0.6 mg/l) showed consistently a R2 > 0.99 (Fig. 1B). The linearity of the standard curve for ELISA obtained within a range of 31.3 to 2000 pg/ml (corresponding to plasma concentration starting from 0.03 to 2 mg/l) consistently show a R2 > 0.99. For both methods, the same plasma pool was run as a positive quality control (QC+). The intra-assay and inter-assay coefficient of variation (CV) were lower than 20%.
Gel Zymography quantification. (A) A representative separation of active MMP-9 and MMP-2 by gel zymography. St.1 to St.4 correspond to standard recombinant human MMP-9 used as calibrator; Ctrl and FXS are samples from controls and FXS participants, in duplicate; QC + represents the positive quality control. (B) A typical standard curve of active MMP-9 obtained by gel zymography.
To compare results obtained by gel zymography and ELISA, we first performed a Pearson correlation test. Since the Pearson’s coefficient r was lower than 0.97 (r = 0.81), the Deming’s (Model II) regression was applied to test the agreement between the two methods. Our results showed a statistically significant proportional and constant difference between the two methods, respectively, with a slope coefficient of 2.31 (confidential interval: 1.53 to 3.24; p < 0.001) and an intercept value of − 0.18 (Confidential interval: − 0.35 to − 0.02) (Fig. 2A).
Comparison of two MMP-9 quantification methods (gel Zymography and ELISA) in 43 individuals. (A) Deming regression (blue line) with confidence interval (gray lines); black dashed line represents ideal correlation (Y = X). (B) Associated Bland Altman plots. The limits of agreement are defined as the mean differences ± 1.96 SD of differences and is shown in red dashed lines. Samples were run in duplicate.
In addition, the Bland–Altman difference plot confirmed the presence of a positive bias of 0.11 mg/l between zymography and ELISA results, with a disagreement between the two methods at concentrations higher than 0.5 mg/l (Fig. 2B).
Active and total MMP-9 plasma levels in FXS and healthy controls
Active and total MMP-9 plasma levels were first compared for all study participants and no significant difference was obtained between FXS and controls (Supplemental Table 1). Since MMP-9 plasma levels are influenced by age35, sex36 and BMI37, the comparison was then performed in a subgroup of 12 FXS and 12 controls matched for all these variables. The concentration of plasma MMP-9 active form as measured by gel zymography was higher in the FXS group as compared to controls (0.48 mg/l ± 0.28 vs. 0.27 mg/l ± 0.14; p < 0.05) (Fig. 3), while plasma total MMP-9 level assessed by ELISA showed no statically significant difference (Supplemental Table 1).
MMP-9 and clinical profile of individuals with FXS
The plasma MMP-9 active form showed a positive association with the aberrant behavior of FXS participants as evaluated by the ABC-CFX 's total score (rs = 0.60, p = 0.039).
Specifically, a significant correlation was obtained for four over six ABC-CFX sub-domains including hyperactivity (rs = 0.55, p = 0.033), social unresponsive (rs = 0.73, p = 0.003), stereotypy (rs = 0.51, p = 0.019) and inappropriate speech (rs = 0.55, p = 0.040). Moreover, the level of plasma MMP-9 active form significantly correlated with the ADAMS score (rs = 0.57, p = 0.043) (Table 2). On the other hand, plasma MMP-9 total form measured by ELISA showed a significant association only with the social unresponsive ABC-CFX subdomain (Table 2). No significant association was observed with ABAS or SCQ scores for neither the active nor the total MMP-9 forms (Supplemental Table 2).
Discussion
Here we report the first study comparing two quantification methods of plasma MMP-9 in FXS. From the clinical endpoint, the MMP-9 active form better discriminates individuals with FXS from healthy controls and better correlates with the clinical profile as compared to the MMP-9 total form.
As in previous reports, we found a strong correlation (r = 0.81) between MMP-9 active and total form measured, respectively, by gel zymography and ELISA38,39. However, the Pearson’s correlation coefficient (r) does not assess agreement between the two methods but rather measures the association between them. Therefore, it is not adequate to use the correlation as a single metric for method comparison studies40. According to CLSI guidelines41 when the correlation coefficient is greater than 0.975, simple linear regressions could be used to further explore constant and proportional errors; otherwise, more rigorous analyses such as Deming or Passing-Bablok regressions are needed42. Numerous studies quantified plasma MMP-9 in different pathologies, by gel zymography along with ELISA43,44,45,46. Heo et al. focused on method comparison of gel zymography and ELISA to ensure the reliability of the measurements and their results were based only on the coefficient of correlation39. To our knowledge, only one study performed additional statistical analyses. Specifically, Prescimone et al., compared both methods in 25 volunteers using correlation coefficient and Bland–Altman difference analysis. Based on the correlation coefficient and regardless of the absolute systematic error (0.006 mg/l) revealed by Bland–Altman analysis, they concluded that both methods offer similar reliability for quantifying MMP-938. In accordance with their results, we obtained a positive bias between gel zymography and ELISA, but on a significant larger scale (0.11 mg/l). The discrepancy between the bias results might be explained by distinct MMP-9 standards used as calibrators for gel zymography and/or ELISA kits; the variation of ranges of measure (0.00025–0.001 mg/l vs. 0.1–0.6 mg/l of our cohort) and the difference in samples size (25 vs. 43 participants of our cohort).
We should note that Bland–Altman analysis is used to evaluate the acceptability based on the analytical imprecision of both methods, yet, to test whether a proportional error exists, a regression analysis must be applied. Considering a Pearson’s correlation coefficient of 0.81, we also performed Deming regression analysis. Our results revealed the presence of statistically significant systematic and proportional errors between the two methods. Indeed, circulating MMP-9 has different forms: the active and total MMP-9. Although their concentrations measured respectively by gel zymography and ELISA correlate between them, they do not represent the same biomarker. As such, finding that they differentially associate with clinical outcomes is unsurprising. Moreover, the present study includes the minimum number of samples (> 40 samples) required for a proper comparison of two biochemical methods40.
Here, we explored the clinical implication of different circulating forms of MMP-9 by questioning: first, the difference in total and active forms between FXS and controls; second, the association of specific MMP-9 forms with the clinical profile. No significant difference was observed between FXS and control individuals for neither active nor total form in the whole study population. However, considering changes in MMP-9 plasma level as a function of age35,47, sex36,48, and BMI37,49, we measured MMP-9 in a subgroup of 12 FXS and 12 controls matched for all these variables. Plasma levels of active MMP-9 obtained by gel zymography were significantly higher in FXS as compared to matched controls. These results are in agreement with a previous study16 showing an increase in plasma MMP-9 active form (semi-quantitatively determined by gel zymography) in ten individuals with FXS as compared to eight age-sex matched controls. In this study, we observed no significant difference in MMP-9 total form in FXS suggesting a better sensibility of gel zymography to distinguish FXS from control, based on MMP-9 active form.
Associations were observed between MMP-9 active form and several clinical features related to aberrant behavior, such as hyperactivity, social unresponsive, stereotypy, and inappropriate speech. Indeed, interventional trials in mice and humans with minocycline, a tetracycline derivative and an inhibitor of MMP-9 activity support these observations. Specifically, the minocycline treatment lowered MMP-9 active form, restored dendritic spine morphology15, and improved behavior performance of Fmr1 KO mice50. Moreover, minocycline treatment was associated with a decrease of plasma MMP-9 active form16 and behavior improvement of FXS in humans including hyperactivity, stereotypy, inappropriate speech18.
Moreover, a direct association was also observed between the MMP-9 active form and the ADAMS score. Interestingly, anxiety is among neuropsychiatric FXS associated symptoms34,51,52,53 and inhibition of MMP-9 activity by minocycline showed an improvement of anxiety in individuals with FXS18,54. No significant association was obtained between MMP-9 plasma active or total forms and ABAS and SCQ scores suggesting that upregulation of MMP-9 active form might rather contribute to FXS-associated aberrant behavior and mood profile than to the cognitive dysfunction.
MMP-9 mRNA translation into MMP-9 is controlled by FMRP23. The proteolytic activation of MMP-9 which is required for synaptic activity is tightly regulated14,50. The up or down regulation of MMP-9 activity has detrimental effects on brain function13 and underlies deficits associated with many neurodevelopmental disorders such as autism spectrum disorder55. Indeed increased levels of MMP-9 have been reported in the amniotic fluid55 and in the serum of the patients with ASD56. The experimental data in ASD without FXS remains very limited as compared to ASD with FXS. Specifically, genetic removal of MMP-9 rescued the ASD-like symptoms of Fragile X in Fmr1 KO mice14. In FXS, the deficit of FMRP leads to an uncontrolled upregulation of MMP-9 synthesis and consecutive increase of MMP-9 active form23. However, the underlining mechanism remains unknown and requires further investigation.
The results of current study should be considered in the light of some limitations. The sample size of matched groups was limited, therefore a larger number of FXS and matched controls are warranted to confirm the superiority of gel zymography utility over ELISA in FXS. In addition, both methods do not provide an accurate determination of plasma MMP-9 levels, but rather an estimation of MMP-9 activity (zymography) and total MMP-9 (ELISA). The MMP-9 regulating factors such as Tissue Inhibitor of Metalloproteinases (TIMPs) dissociate from MMP-9 during electrophoresis, therefore gel zymography might not give a precise measure of in vivo activity. Moreover, ELISA antibodies might cross react with TIMP-1 and thus preclude an accurate determination of the total form.The determination of the abundance of individual inhibitors would have provided an estimation of the degree of occupancy of MMP-9 by those inhibitors and thus a better measure of total MMP-9. However, the correction of the MMP-9 total form as measured by ELISA is theoretically needed but technically very challenging to obtain with today's methods. Furthermore, we used a manual technique to quantify the active form. Indeed, gel zymography is a time-consuming method that can be challenging to be performed properly and needs a well-trained technician. Although we considered the analytical variation of the methods and all experiments were performed by the same well-trained master student, other techniques providing optimal sensitivities and specificities, such as mass spectrometry could also be considered for the quantification of MMP-9 forms in a clinical context.
In conclusion, our results highlight the importance of choosing the appropriate method to quantify plasma MMP-9 in FXS studies, specifically in future clinical trials where MMP-9 might be used as a measure of outcomes57. Technically, ELISA is generally easier to perform than gel zymography and is more adaptable to upscale. However, gel zymography seems to be a more sensitive method to detect differences in MMP-9 active form between FXS and healthy controls as well as the association with aberrant behavior, and anxiety related symptoms.
Data availability
All data generated and analysed are included in this article.
References
Auerbach, B. D., Osterweil, E. K. & Bear, M. F. Mutations causing syndromic autism define an axis of synaptic pathophysiology. Nature 480, 63–68 (2011).
Martin, J. P. & Bell, J. A pedigree of mental defect showing sex-linkage. J. Neurol. Neurosurg. Psychiatry 6, 154–157 (1943).
Mulligan, L. M. et al. Genetic mapping of DNA segments relative to the locus for the fragile-X Syndrome at Xq27.3. Am. J. Hum. Genet. 37, 463–472 (1985).
Quartier, A. et al. Intragenic FMR1 disease-causing variants: A significant mutational mechanism leading to Fragile-X Syndrome. Eur. J. Hum. Genet. 25, 423–431 (2017).
Verkerk, A. J. et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in Fragile X Syndrome. Cell 65, 905–914 (1991).
Bassell, G. J. & Warren, S. T. Fragile X Syndrome: Loss of local mRNA regulation alters synaptic development and function. Neuron 60, 201–214 (2008).
Khandjian, E. W. et al. Biochemical evidence for the association of Fragile X mental retardation protein with brain polyribosomal ribonucleoparticles. PNAS 101, 13357–13362 (2004).
Brown, V. et al. Microarray identification of FMRP-associated brain mRNAs and altered mRNA translational profiles in Fragile X Syndrome. Cell 107, 477–487 (2001).
Darnell, J. C. & Klann, E. The translation of translational control by FMRP: Therapeutic targets for Fragile X Syndrome. Nat. Neurosci. 16, 1530–1536 (2013).
Booker, S. A. et al. Altered dendritic spine function and integration in a mouse model of Fragile X Syndrome. Nat. Commun. 10, 4813 (2019).
Irwin, S. A. et al. Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with Fragile-X Syndrome: A quantitative examination. Am. J. Med. Genet. 98, 161–167 (2001).
Irwin, S. A., Galvez, R. & Greenough, W. T. Dendritic spine structural anomalies in Fragile-X mental retardation Syndrome. Cereb. Cortex 10, 1038–1044 (2000).
Reinhard, S. M., Razak, K. & Ethell, I. M. A delicate balance: Role of MMP-9 in brain development and pathophysiology of neurodevelopmental disorders. Front. Cell. Neurosci. 9, 280 (2015).
Sidhu, H., Dansie, L. E., Hickmott, P. W., Ethell, D. W. & Ethell, I. M. Genetic removal of matrix metalloproteinase 9 rescues the symptoms of Fragile X Syndrome in a mouse model. J. Neurosci. 34, 9867–9879 (2014).
Bilousova, T. V. et al. Minocycline promotes dendritic spine maturation and improves behavioural performance in the Fragile X mouse model. J. Med. Genet. 46, 94–102 (2009).
Dziembowska, M. et al. High MMP-9 activity levels in Fragile X Syndrome are lowered by minocycline. Am. J. Med. Genet. A 161, 1897–1903 (2013).
Siller, S. S. & Broadie, K. Matrix metalloproteinases and minocycline: Therapeutic avenues for Fragile X Syndrome. Neural Plast. 2012, e124548 (2012).
Paribello, C. et al. Open-label add-on treatment trial of minocycline in Fragile X Syndrome. BMC Neurol 10, 91 (2010).
Bar-Or, A. et al. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain 126, 2738–2749 (2003).
Sternlicht, M. D. & Werb, Z. How matrix metalloproteinases regulate cell behavior. Annu. Rev. Cell Dev. Biol. 17, 463–516 (2001).
Frankowski, H., Gu, Y.-H., Heo, J. H., Milner, R. & del Zoppo, G. J. Use of gel zymography to examine matrix metalloproteinase (Gelatinase) expression in brain tissue or in primary glial cultures. Methods Mol. Biol. 814, 221–233 (2012).
Gkogkas, C. G. et al. Pharmacogenetic inhibition of eIF4E-dependent Mmp9 mRNA translation reverses Fragile X Syndrome-like phenotypes. Cell Rep. 9, 1742–1755 (2014).
Janusz, A. et al. The Fragile X mental retardation protein regulates matrix metalloproteinase 9 mRNA at synapses. J. Neurosci. 33, 18234–18241 (2013).
Leigh, M. J. S. et al. A randomized double-blind, placebo-controlled trial of minocycline in children and adolescents with Fragile X Syndrome. J. Dev. Behav. Pediatr. 34, 147–155 (2013).
Andrea, S. et al. Electrocortical changes associated with minocycline treatment in Fragile X Syndrome. J. Psychopharmacol. 27, 956–963 (2013).
Çaku, A. et al. New insights of altered lipid profile in Fragile X Syndrome. PLoS ONE 12, e0174301 (2017).
Lessard, M., Chouiali, A., Drouin, R., Sébire, G. & Corbin, F. Quantitative measurement of FMRP in blood platelets as a new screening test for Fragile X Syndrome. Clin. Genet. 82, 472–477 (2012).
Snoek-van Beurden, P. A. M. & Von den Hoff, J. W. Zymographic techniques for the analysis of matrix metalloproteinases and their inhibitors. Biotechniques 38, 73–83 (2005).
Rueden, C. T. et al. Image J2: ImageJ for the next generation of scientific image data. BMC Bioinf. 18, 529 (2017).
Aman, M. G., Singh, N. N., Stewart, A. W. & Field, C. J. The aberrant behavior checklist: A behavior rating scale for the assessment of treatment effects. Am. J. Ment. Defic. 89, 485–491 (1985).
Sansone, S. M. et al. Psychometric study of the aberrant behavior checklist in Fragile X Syndrome and implications for targeted treatment. J. Autism. Dev. Disord. 42, 1377–1392 (2012).
Oakland, T. & Harrison, P. L. Adaptive Behavior Assessment System-II: Clinical Use and Interpretation (Academic Press, Cambridge, 2011).
Kidd, S. A. et al. Improving the diagnosis of autism spectrum disorder in Fragile X Syndrome by adapting the social communication questionnaire and the social responsiveness scale-2. J. Autism. Dev. Disord. 50, 3276–3295 (2020).
Cordeiro, L., Ballinger, E., Hagerman, R. & Hessl, D. Clinical assessment of DSM-IV anxiety disorders in Fragile X Syndrome: Prevalence and characterization. J. Neurodevelop. Disord. 3, 57–67 (2011).
Bonnema, D. et al. Effects of age on plasma matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases (TIMPs). J. Cardiac. Fail. 13, 530–540 (2007).
Samnegård, A. et al. Gender specific associations between matrix metalloproteinases and inflammatory markers in post myocardial infarction patients. Atherosclerosis 202, 550–556 (2009).
Boumiza, S. et al. MMPs and TIMPs levels are correlated with anthropometric parameters, blood pressure, and endothelial function in obesity. Sci. Rep. 11, 20052 (2021).
Prescimone, T. et al. Reappraisal of quantitative gel zymography for matrix metalloproteinases. J. Clin. Lab. Anal. 28, 374–380 (2014).
Heo, D. S., Choi, H., Yeom, M. Y., Song, B. J. & Oh, S. J. Serum levels of matrix metalloproteinase-9 predict lymph node metastasis in breast cancer patients. Oncol. Rep. 31, 1567–1572 (2014).
Westgard, J. O. & Hunt, M. R. Use and interpretation of common statistical tests in method-comparison studies. Clin. Chem. 19, 49–57 (1973).
EP09-A2 Method Comparison and Bias Estimation Using Patient Samples; Approved Guideline—Second Edition. 22, 75 (2002).
Westgard, J. O. Use and Interpretation of common statistical tests in method comparison studies. Clin. Chem. 54, 612 (2008).
Elahirad, S. et al. Association of matrix metalloproteinase-2 (MMP-2) and MMP-9 promoter polymorphisms, their serum levels, and activities with coronary artery calcification (CAC) in an Iranian population. Cardiovasc. Toxicol. 22, 118–129 (2022).
Verma, A. et al. Association of MMP-2 and MMP-9 with clinical outcome of neurocysticercosis. Parasitology 138, 1423–1428 (2011).
Chang, Y.-H. et al. Elevated circulatory MMP-2 and MMP-9 levels and activities in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin. Biochem. 41, 955–959 (2008).
Shiau, M.-Y. et al. Increased circulatory MMP-2 and MMP-9 levels and activities in patients with type 1 diabetes mellitus. Mt. Sinai J. Med. 73, 1024–1028 (2006).
Cancemi, P. et al. The role of matrix metalloproteinases (MMP-2 and MMP-9) in ageing and longevity: Focus on sicilian long-living individuals (LLIs). Mediat. Inflamm. 2020, e8635158 (2020).
Gu, C. et al. Sex-related differences in serum matrix metalloproteinase-9 screening non-calcified and mixed coronary atherosclerotic plaques in outpatients with chest pain. Heart Vessels 32, 1424–1431 (2017).
Derosa, G. et al. Matrix metalloproteinase-2 and -9 levels in obese patients. Endothelium 15, 219–224 (2008).
Dansie, L. E. et al. Long-lasting effects of minocycline on behavior in young but not adult Fragile X mice. Neuroscience https://doi.org/10.1016/j.neuroscience.2013.04.058 (2013).
DaWalt, L. S., Fielding-Gebhardt, H., Fleming, K. K., Warren, S. F. & Brady, N. Change in behavior problems from childhood through adolescence for children with Fragile X Syndrome. J. Autism. Dev. Disord. 52, 4056–4066 (2022).
Cregenzán-Royo, O., Brun-Gasca, C. & Fornieles-Deu, A. Behavior problems and social competence in Fragile X Syndrome: A systematic review. Genes (Basel) 13, 280 (2022).
Crawford, H., Moss, J., Oliver, C. & Riby, D. Differential effects of anxiety and autism on social scene scanning in males with Fragile X Syndrome. J. Neurodev. Disord. 9, 9 (2017).
Utari, A. et al. Side effects of minocycline treatment in patients with Fragile X Syndrome and exploration of outcome measures. Am. J. Intellect. Dev. Disabil. 115, 433–443 (2010).
Abdallah, M. W. et al. Amniotic fluid MMP-9 and neurotrophins in autism spectrum disorders: an exploratory study. Autism. Res. 5, 428–433 (2012).
Lord, J. R., Mashayekhi, F. & Salehi, Z. How matrix metalloproteinase (MMP)-9 (rs3918242) polymorphism affects MMP-9 serum concentration and associates with autism spectrum disorders: A case-control study in Iranian population. Dev. Psychopathol. 34, 882–888 (2022).
Budimirovic, D. B. et al. Updated report on tools to measure outcomes of clinical trials in Fragile X Syndrome. J. Neurodev. Disord. 9, 14 (2017).
Acknowledgements
We would like to show our gratitude to all the participants of this project including individuals with FXS and their families, and to the healthy controls for giving us the opportunity of doing this research. Furthermore, we thank the administrative personnel at the CRC-CHUS for their help with the recruitment.
Funding
This research was supported by Clinical Research Scholars Junior 1, a Grant provided by Fond de recherche du Québec en Santé (FRQS).
Author information
Authors and Affiliations
Contributions
Conceptualization, L.G., A.Ç.; investigation, A.L., A.Ç.; writing A.L.; review and editing, A.Ç., L.G., A.A., R.L. F.Z.B., J.F.L., and F.C.; visualization, A.L, A.Ç.; L.G.; A.A; R.L.; and S.B.; supervision, A.Ç.; project administration, A.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laroui, A., Galarneau, L., Abolghasemi, A. et al. Clinical significance of matrix metalloproteinase-9 in Fragile X Syndrome. Sci Rep 12, 15386 (2022). https://doi.org/10.1038/s41598-022-19476-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19476-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.