Abstract
Bacterial contamination of blood products is a major problem in transfusion medicine, in terms of both morbidity and mortality. Platelets (PLTs) are stored at room temperature (under constant agitation) for more than 5 days, and bacteria can thus grow significantly from a low level to high titers. However, conventional methods like blood culture and lateral flow assay have disadvantages such as long detection time, low sensitivity, and the need for a large volume of blood components. We used real-time polymerase chain reaction (PCR) assays with antibiotic-conjugated magnetic nanobeads (MNBs) to detect enriched Gram-positive and -negative bacteria. The MNBs were coated with polyethylene glycol (PEG) to prevent aggregation by blood components. Over 80% of all bacteria were captured by the MNBs, and the levels of detection were 101 colony forming unit [CFU]/mL and 102 CFU/mL for Gram-positive and -negative bacteria, respectively. The detection time is < 3 h using only small volumes of blood components. Thus, compared to conventional methods, real-time PCR using MNBs allows for rapid detection with high sensitivity using only a small volume of blood components.
Similar content being viewed by others
Introduction
Bacterial contamination of blood products is a major problem in transfusion medicine1,2,3. Especially, transfusion of contaminated platelets (PLT) may cause serious infections and septic reactions1,4. PLTs are stored at room temperature (under constant agitation) for 5 days; bacteria can thus easily multiply from low levels (< 1 colony forming unit [CFU]/mL) to high titers (< 108 CFU/mL)5,6,7. The US Food and Drug Administration (FDA) reported that transfusion of contaminated PLTs caused 51 deaths from 2001 to 20168. The European Commission reported that 43 transfusions were contaminated in the European Union from 2010 to 2013; 36 involved contaminated PLTs9. Although there have been a few cases, the morbidity and mortality rates are very high10,11. To reduce mortality, accurate and rapid bacterial detection is required7. The gold standard for the detection is blood culture, which is one of the oldest clinical techniques12,13. However, bacterial growth to detectable levels usually requires from 24 h14 to several days15. Also, low bacterial titers and slow bacterial growth can cause false-negative results when automated blood culture systems are employed16,17. Much effort has thus been devoted to the rapid and sensitive detection of bacterial pathogens in blood18,19,20,21. The enhanced bacterial detection (eBDS) system (Haemonetics Corporation, Braintree, MA, USA) indirectly detects bacteria by measuring decreases in oxygen concentration over 24 h, but cannot detect anaerobic bacteria22. The Platelet Pan-Genera Detection (PGD) test (Verax Biomedical, Marlborough, MA, USA) is a lateral flow immunoassay detecting lipoteichoic acid (LTA) and lipopolysaccharide (LPS) in aerobic and anaerobic Gram-positive and -negative bacterial species, respectively, within 30 min23. However, the sensitivity is low (approximately 104 CFU/mL) and the false-positive rate is high24.
Nucleic acid (NA) amplification via polymerase chain reaction (PCR) sensitively and specifically detects bacterial pathogens25,26,27,28,29. However, on the day of PLT production, the PCR sensitivity was only 12.8% that of the BacT/ALERT system (Organon Teknika Corp., Durham, NC, USA) because the bacterial loads were very low30. There are commercially available molecular diagnostic systems such as T2Bacteria Panel (T2 Biosystems, Lexington, MA, US) and Micro-DxTM (Molzyme, Bremen, Germany) for the identification of patients with symptoms of sepsis. However, no molecular systems have been developed to validate the safety of blood components for transfusion services and conventional products such as PGD test and eBDS system are not related to molecular diagnosis. Also, PLTs contain many substances (such as immunoglobulin G) that interfere with NA amplification31. It is thus essential to enrich bacteria and prepare purified bacterial DNA for accurate and rapid detection. Many commercial kits are used to extract NA from blood products; most employ solid-phase extraction32. However, these cannot remove inhibitors or enrich pathogens and bacteria are not isolated. Immunomagnetic separation (IMS) using antibody-conjugated magnetic nanobeads (Ab-MNBs) is widely applied to isolate pathogens and thus eliminate inhibitory substances33,34,35,36. However, Ab-MNBs do not detect all bacteria that cause sepsis; the antibody is specific for 1 species but at least 10 species of bacteria cause sepsis. Thus, MNBs must be conjugated with materials that bind a broad spectrum of bacterial species. Although there have been previous studies using vancomycin conjugated nanobeads to capture several bacterial species, those nanobeads were used in urine and orange juice without molecular detection methods37,38,39,40,41.
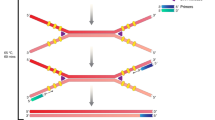
Thus, we developed a method that enriches both Gram-positive and -negative bacteria using MNBs coated with two different materials; we then extracted bacterial DNA. Figure 1 shows two methods used for sample preparation (with and without specimen incubation). Performance was tested by spiking 2.5-mL amounts of apheresis plasma with Escherichia coli O157:H7 (E. coli O157:H7) and Staphylococcus aureus (S. aureus). Extracted bacterial DNAs were amplified via real-time PCR.
Schematic illustration of pathogen enrichment by MNBs (magnetic nanobeads) and NA (nucleic acid) extraction from 1-mL samples of blood components spiked with bacteria (a) after 12 h of specimen incubation at RT (room temperature), and (b) without prior specimen incubation. The procedural steps were as follows: sampling, specimen preparation, pathogen enrichment by MNBs, and NA extraction.
Results
Characterization of antibiotics conjugated MNBs
The synthesis of antibiotic-conjugated MNBs with PEG coatings is shown in Fig. 2a and b. First, superparamagnetic Fe3O4 nanobeads with an average diameter of 150 nm were synthesized using a one-step hydrothermal method42, coated with PEG, and conjugated with vancomycin (Van) or allantoin (Al) to yield MNBs@PEG-Van and MNBs@PEG-Al. Transmission electron microscopy (TEM) (JSM-3010, JEOL Ltd. Tokyo, Japan) (Fig. 2c) showed that the MNBs had a typical core–shell structure, i.e., a 150-nm-diameter Fe3O4 core and 5.5-nm-thick PEG coating. The zeta potentials were derived using dynamic light scattering (DLS) (Nano ZS, Malvern Instruments, Malvern, UK). The zeta potential of unconjugated MNBs was −20.33 ± 0.67 mV, whereas those of MNBs@PEG, MNBs@PEG-Al, and MNBs@PEG-Van were −10.58 ± 0.86, −12.40 ± 0.42, and −6.93 ± 0.71, respectively (Supplementary Table S1).
Conjugation of materials to MNBs (magnetic nanobeads). (a) Schematic of the synthesis of MNBs@PEG-Van (polyethylene glycol-vancomycin). (b) Schematic of the synthesis of MNBs@PEG-Al (polyethylene glycol-allantoin). (c) TEM (Transmission electron microscopy) images of unconjugated MNBs, MNBs@PEG, MNBs@PEG-Van, and MNBs@PEG-Al.
Efficiencies of bacterial enrichment by MNBs
As shown in Fig. 3a, the MNBs@PEG-Al’s capture efficiencies of E. coli spiked in phosphate-buffered saline (PBS) and apheresis plasma were 90% and 80.1%, respectively. The MNBs@PEG-Van’s capture efficiencies of S. aureus spiked in PBS and apheresis plasma were 92.3% and 82.1%, respectively (Fig. 3b). Field-effect scanning electron microscopy (FE-SEM) (JSM7500F, JEOL Ltd. Tokyo, Japan) (Fig. 3c and d) showed E. coli and S. aureus bound specifically to MNBs@PEG-Al and MNBs@PEG-Van, respectively.
(a) Capture efficiencies of E. coli with MNBs@PEG-Al (polyethylene glycol-allantoin) and MNBs@PEG from PBS (phosphate-buffered saline) and apheresis plasma. (b) Capture efficiencies of S. aureus with MNBs@PEG-Van (magnetic nanobeads@polyethylene glycol-vancomycin) and MNBs@PEG from PBS and apheresis plasma. (c) FE-SEM (Field-effect scanning electron microscopy) images showing E. coli bound to MNBs@PEG-Al. (d) FE-SEM images showing S. aureus bound to MNBs@PEG-Van.
Real-time PCR for the detection of enriched bacteria
DNA was extracted from the enriched Gram-negative and -positive bacteria and subjected to real-time PCR. As shown in Fig. 4a, E. coli at 102 CFU/mL was detected after 12 h of specimen incubation, and Fig. 4b shows that E. coli not captured by MNBs were detected at only 104 CFU/mL. As shown in Fig. 4c, 103 CFU/mL of E. coli was detected without prior specimen incubation, but DNA extracted from 101 to 102 CFU/mL could not be amplified. Figure 4d shows that the difference in cycle threshold (Ct) value was approximately 1.4 when apheresis plasma containing E. coli captured (Ct; 30.54 ± 0.48) and not captured (Ct; 31.95 ± 0.95) by MNBs at a level of 104 CFU/mL were compared, while MNBs@PEG-Al captured the bacteria effectively at a level of 103 CFU/mL (Table 1). As shown in Fig. 5a, S. aureus at 101 CFU/mL was detected after 12 h of specimen incubation. Figure 5b shows that S. aureus not captured by MNBs was detected at only 104 CFU/mL. 102 CFU/mL of S. aureus was detected without prior specimen incubation, but DNA extracted from 101 CFU/mL could not be detected (Fig. 5c). Figure 5d shows that MNBs@PEG-Van captured the bacteria effectively at a level of 104 CFU/mL.
Results of real-time PCR for the detection of E. coli. Each figure shows amplification and melting curves. The CFU (colony forming unit) values in each figure are the concentrations at the time of spiking and are independent of specimen incubation. The quantified actual numbers of E. coli in plasma with different concentration (101–104 CFU/mL) after 12 h specimen incubation at RT are 98.3 ± 22.4, 741 ± 98, 6,210 ± 1540, and 53,300 ± 12,700, respectively (Supplementary Table S3). Nucleic acid amplification and melting curves in each figure are dependent on specimen incubation. (a) Real-time PCR results after 12 h incubation and with E. coli captured by MNBs, (b) after 12 h incubation and with E. coli uncaptured by MNBs, (c) without prior specimen incubation and with E. coli captured by MNBs, (d) without prior specimen incubation and with E. coli uncaptured by MNBs.
Results of real-time PCR for the detection of S. aureus. Each figure shows amplification and melting curves. The CFU (colony forming unit) values in each figure are the concentrations at the time of spiking and are independent of specimen incubation. The quantified actual numbers of S. aureus in plasma with different concentration (101–104 CFU/mL) after 12 h specimen incubation at RT are 88.6 ± 14.7, 606 ± 144, 7,210 ± 1070, and 54,000 ± 10,600, respectively (Supplementary Table S3). Nucleic acid amplification and melting curves in each figure are dependent on specimen incubation. (a) Real-time PCR results after 12 h incubation and with S. aureus captured by MNBs, (b) after 12 h incubation and with S. aureus uncaptured by MNBs, (c) without prior specimen incubation and with S. aureus captured by MNBs, (d) without prior specimen incubation and with S. aureus uncaptured by MNBs.
Discussion
When PLTs are stored for 5 days at RT with agitation, even if the initial suspension contains < 1 CFU/mL, the bacteria can proliferate1,4. Current culture methods do not yield contamination data during PLT storage. Culture requires 1–5 days and data are available only after the PLTs have been released. Second, a large amount of blood (> 20 mL) is required for culture of both aerobic and anaerobic bacteria23. Molecular diagnostics requires small sample volumes (< 1 mL) and detects pathogens within 3 h. It is essential to reduce culture time by improving bacterial enrichment. Such enrichment by MNBs requires that they be dispersible in blood components, and that receptors such as vancomycin and allantoin bind to the bacterial pathogens. Plasma contains many proteins, clotting factors, and IgG43; these readily adsorb to non-PEG-coated MNBs. After a 20-min incubation, MNBs aggregated in plasma, but MNBs@PEG did not (Supplementary Fig. S1). PEG prevented non-specific binding to the surfaces of MNBs. The MNBs (4 × 109 to 4 × 1012 beads/mL) were added to 1 mL amounts of apheresis plasma containing bacterial pathogens. Over 80% of all E. coli and S. aureus were captured at MNB levels of 4 × 1011 to 4 × 1012/mL (Supplementary Table S2). Many bacterial species contaminate PLTs. IMS is not diagnostically useful; the species of bacteria present remain unknown until the results are confirmed. MNBs must be conjugated with receptors that bind to a broad spectrum of bacterial species. Vancomycin binds to the peptidoglycan layer of Gram-positive bacteria that terminate in -Lys-D-Ala-D-Ala44,45,46, and it is known to bind to vancomycin-resistant bacteria47. The LPS structure of the outer membrane of Gram-negative bacteria varies depending on the bacterial strain48, but it is known that allantoin can bind to most LPS structures regardless of the strain49. The capture efficiencies and SEM images showed that these compounds were immobilized on MNBs@PEGs that bound E. coli and S. aureus, respectively.
According to the current FDA guidance50, standard protocol for bacterial contamination of PLT essentially includes incubation for 12 h. Even if there are low cases of bacterial contamination of PLT, but it is essential for safety validation of blood components for public health. Pathogen enrichment by MNBs prior to NA extraction reduced the levels of possible inhibitors and yielded more NA than commercial kits. The detection time was thus dramatically reduced (< 15 h). Both the E. coli and S. aureus enrichment rates were > 80% and levels of 101 and 102 CFU/mL, respectively, were detected after 12 h of specimen incubation. The levels of detection without incubation were 102 and 103 CFU/mL, respectively. Thus, our method is at least 100-fold more sensitive than lateral flow assay kits such as the Platelet PGD test (limit of detection = 104–5 CFU/mL) after 12 h of specimen incubation24. In addition, our method requires only small sample volumes (< 1 mL) for monitoring bacterial contamination. This also means that there is no need to consider the adverse effects of MNBs on PLT as the remaining PLT which is not used for testing will be transfused. However, we aim to further improve the sensitivity and devise a fully automated high-throughput system. Our current focus is on optimization of sample preparation methods for various bacterial strains and their application to other blood components as well.
Methods
Bacterial strains
Escherichia coli (ATCC 25,922; American Type Culture Collection, Bethesda, MD, USA) and S. aureus (ATCC 25,923) were used. A single colony of either strain was transferred to 5 mL of Luria–Bertani (LB) broth (BD, Franklin Lakes, NJ, USA) and cultured for 18 h at 200 rpm and 37 °C. The cultures were then diluted 100-fold with fresh LB broth and incubated at 200 rpm and 37 °C until the optical density at 600 nm (OD600) reached 1. Bacterial viability was measured using the standard colony counting method51 and suspensions of 108 CFU/mL in PBS (pH 7.4) were prepared.
Preparation of antibiotics conjugated MNBs
Figure 2a and b show the synthesis of antibiotic conjugated MNBs. Vancomycin and allantoin were obtained from Sigma-Aldrich (St. Louis, MO, USA). The MNBs (100 nm in diameter) were sonicated for about 40 s to prevent aggregation. MNBs (200 mg) were dispersed in 40 mL of 1 M HCl and stirred at room temperature (RT) for 1 h. The MNBs were separated over 2 min using a magnetic rack (Bioneer Co., Ltd, Daejeon, Korea), and residual HCl was removed by washing in 40 mL of PBS three times followed by dispersal in 10 mL PBS. PEG (25 mg) (Sigma-Aldrich) dissolved in 25 mL of Tris buffer (pH 8.5) was mixed with 50 mg MNBs overnight at RT. To conjugate Van to MNBs@PEG-COOH, 5 mg MNBs@PEG-COOH was added to 500 µL of 2-(N-morpholino) ethane sulfonic acid (MES) buffer (0.1 M, pH 6.0) (Sigma-Aldrich); 4 mg ethyl carbodiimide hydrochloride (EDC) (Sigma-Aldrich), 7 mg N-hydroxy succinimide (NHS) (Sigma-Aldrich), and 10 mg vancomycin dissolved in 1 mL of MES buffer were added and the mixture was stirred at RT for 15 min. Then, the MNBs@PEG-COOH suspension was dispersed in the vancomycin-EDC-NHS suspension via continuous stirring at RT for 2 h. MNBs@PEG-Van were separated using the magnetic rack and washed with 500 µL of PBS. Finally, MNBs@PEG-Van were resuspended in 1 mL of PBS and stored at 4 °C. MNBs@PEG-Al were similarly prepared.
Characterization of antibiotics conjugated to MNBs
MNBs were dispersed in 99.5% (v/v) ethanol at 20 μg/mL. Copper grids bearing carbon films (Electron Microscopy Sciences, Hatfield, PA, USA) were immersed in 1-mL MNB dispersions for 10 min, removed using tweezers, dried at 70 °C, and examined by TEM (JEOL Ltd.) operating at 200 kV.
Bacterial enrichment by MNBs
Apheresis plasma containing bacteria (E. coli O157:H7 and S. aureus) at 101–104 CFU/mL were incubated at RT for 12 h. One milliliter of plasma was mixed with 200 μL of either MNBs@PEG-Al or MNBs@PEG-Van (4 × 1011 particles/mL, final concentration) and the mixtures were incubated at RT for 20 min. Bacteria-MNB clusters were separated using a magnetic rack. The residues, which contained uncaptured bacteria, were transferred to 1.5-mL tubes. The MNBs were washed with 1 mL PBS twice and dispersed in 200 µL PBS.
FE-SEM of bacteria binding to antibiotics conjugated MNBs
Bacteria-enriched MNBs were washed twice with PBS and MNBs separated on a magnetic rack. Fixation [in 2% (w/v) glutaraldehyde] proceeded at RT for 1 h. MNB-bacteria complexes were washed three times with 1 mL PBS, incubated with 1% (w/v) osmium tetroxide for 1 h at 4 °C in the dark, and washed three times with PBS followed by gradual dehydration in ethanol (30, 50, 70, 80, 90, and 99.5% [v/v]) for 10 min each time. Ten microliters of MNB-bacteria complexes were dropped onto copper grids covered with amorphous carbon and dried at RT for 2 h. FE-SEM (JEOL Ltd.) was used to image the complexes.
NA extraction
MagListo 5 M Genomic NA extraction kits (Bioneer) were used to extract bacterial DNA as suggested by the manufacturer. Two hundred microliters of lysis buffer were added to a suspension of BE-MNBs followed by incubation for 10 min at RT. The elution volume was 100 µL; the extracted DNA was stored at −80 °C. DNA purity and yield were assessed by quantifying absorbance at 230, 260, and 280 nm using a Nano-200 spectrophotometer (Allsheng, Hangzhou, China). To detect Gram-positive bacteria, 10 µg lysostaphin (Sigma-Aldrich) was added to the BE-MNBs followed by incubation for 10 min at 37 °C prior to the addition of lysis buffer.
Real-time PCR assay
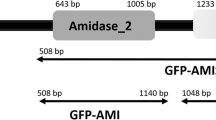
Real-time PCR was used to confirm the identities of the captured bacteria. The primers were designed using PrimerQuest (Integrated DNA Technologies Inc., Coralville, IA, USA): SA nuc_F (5′-TATGGACGTGGCTTAGCGTAT-3′) and SA nuc_R (5′-GACCTGAATCAGCGTTGTCTT-3′) for S. aureus; and EB tyrB_F (5′-AAGAGGATGCCTACGCCATT-3′) and EB tyrB_R (5′-CTTGGCGGGCTGGAGTAGTT-3′) for E. coli. Power SYBR Green PCR Master Mix (Applied Biosystems, Waltham, MA, USA) served as the PCR master mix; all primers were added to 0.2 µM. QuantStudio 3 (Applied Biosystems) was used to perform PCR. Positive and negative amplification controls were included in every run. The positive controls contained DNA directly extracted from S. aureus and E. coli, and the negative control was RNase- and DNase-free water. A result was considered positive when the threshold cycle (Ct) was > 37.0 and the melting temperature (Tm) was appropriate (76.0 ± 0.5 °C).
Data availability
The data supporting this study are included in this published article and its Supplementary Information.
References
Brecher, M. E. & Hay, S. N. Bacterial contamination of blood components. Clin. Microbiol. Rev. 18, 195–204 (2005).
Brecher, M. E., Blajchman, M. A., Yomtovian, R., Ness, P. & AuBuchon, J. P. Addressing the risk of bacterial contamination of platelets within the United States: A history to help illuminate the future. Transfusion 53, 221–231 (2013).
Blajchman, M. A. et al. Bacterial detection of platelets: Current problems and possible resolutions. Transfusion Med. Rev. 19, 259–272 (2005).
U. FDA, Draft guidance for industry, Food and Drug Administration staff, and clinical laboratories: Framework for regulatory oversight of laboratory developed tests (LDTs) US Food and Drug Administration, Silver Spring, MD. http://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm416685.pdf (2016).
Müller, T. H., Mohr, H. & Montag, T. Methods for the detection of bacterial contamination in blood products. Clin. Chem. Lab. Med. 46, 933–946 (2008).
Vossier, L. et al. Combining culture and microbead-based immunoassay for the early and generic detection of bacteria in platelet concentrates. Transfusion 59, 277–286 (2019).
Trampuz, A., Salzmann, S., Antheaume, J. & Daniels, A. U. Microcalorimetry: A novel method for detection of microbial contamination in platelet products. Transfusion 47, 1643–1650 (2007).
U. Food, D. Administration, Fatalities reported to FDA following blood collection and transfusion: Annual summary for fiscal year 2010, http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ReportaProblem/TransfusionDonationFatalities/ucm254802.htm (2011).
Domanović, D. et al. Prioritizing of bacterial infections transmitted through substances of human origin in Europe. Transfusion 57, 1311–1317 (2017).
D. Védy, D. Robert, D. Gasparini, G. Canellini, S. Waldvogel, J.-D. Tissot, Bacterial contamination of platelet concentrates: Pathogen detection and inactivation methods. Hematol. Rev. 1 (2009).
McDonald, C. et al. Bacterial screening of platelet components by National Health Service Blood and Transplant, an effective risk reduction measure. Transfusion 57, 1122–1131 (2017).
Yamane, N. Blood culture: Gold standard for definitive diagnosis of bacterial and fungal infections–from the laboratory aspect, Rinsho byori. Jpn. J. Clin. Pathol. 46, 887–892 (1998).
Hall, K. K. & Lyman, J. A. Updated review of blood culture contamination. Clin. Microbiol. Rev. 19, 788–802 (2006).
Ray, S. T., Drew, R. J., Hardiman, F., Pizer, B. & Riordan, A. Rapid identification of microorganisms by FilmArray blood culture identification panel improves clinical management in children. Pediatr. Infect. Dis. J. 35, e134–e138 (2016).
Gal, D., Mayo, M., Spencer, E., Cheng, A. C. & Currie, B. J. Application of a polymerase chain reaction to detect Burkholderia pseudomallei in clinical specimens from patients with suspected melioidosis. Am. J. Trop. Med. Hyg. 73, 1162–1164 (2005).
Dumont, L. J. et al. BLOOD COMPONENTS: Screening of single-donor apheresis platelets for bacterial contamination: The PASSPORT study results. Transfusion 50, 589–599 (2010).
Lessa, F. et al. Fatal group C streptococcal infection due to transfusion of a bacterially contaminated pooled platelet unit despite routine bacterial culture screening. Transfusion 48, 2177–2183 (2008).
Driskell, J. D. et al. Rapid and sensitive detection of rotavirus molecular signatures using surface enhanced Raman spectroscopy. PLoS ONE 5, e10222 (2010).
Luk, J. M. & Lindberg, A. A. Rapid and sensitive detection of Salmonella (0: 6, 7) by immunomagnetic monoclonal antibody-based assays. J. Immunol. Methods 137, 1–8 (1991).
Vutukuru, M. R. et al. A rapid, highly sensitive and culture-free detection of pathogens from blood by positive enrichment. J. Microbiol. Methods 131, 105–109 (2016).
Tang, M.-J. et al. Rapid and sensitive detection of Listeria monocytogenes by loop-mediated isothermal amplification. Curr. Microbiol. 63, 511–516 (2011).
Chavan, P. et al. Detection of bacterial growth in blood components using oxygen consumption as a surrogate marker in a tertiary oncology setup. Indian J. Med. Microbiol. 30, 212–214 (2012).
Vollmer, T., Hinse, D., Kleesiek, K. & Dreier, J. The Pan Genera Detection immunoassay: A novel point-of-issue method for detection of bacterial contamination in platelet concentrates. J. Clin. Microbiol. 48, 3475–3481 (2010).
Harm, S. K. et al. Routine use of a rapid test to detect bacteria at the time of issue for nonleukoreduced, whole blood–derived platelets. Transfusion 53, 843–850 (2013).
Mothershed, E. A. & Whitney, A. M. Nucleic acid-based methods for the detection of bacterial pathogens: Present and future considerations for the clinical laboratory. Clin. Chim. Acta 363, 206–220 (2006).
Boutaga, K., Van Winkelhoff, A. J., Vandenbroucke-Grauls, C. M. & Savelkoul, P. H. The additional value of real-time PCR in the quantitative detection of periodontal pathogens. J. Clin. Periodontol. 33, 427–433 (2006).
Abafogi, A. T. et al. 3D-printed modular microfluidic device enabling preconcentrating bacteria and purifying bacterial DNA in blood for improving the sensitivity of molecular diagnostics. Sensors 20, 1202 (2020).
Ganesh, I. et al. An integrated microfluidic PCR system with immunomagnetic nanoparticles for the detection of bacterial pathogens. Biomed. Microdevice 18, 1–7 (2016).
Kim, Y. et al. Integrated microfluidic preconcentration and nucleic amplification system for detection of influenza A virus H1N1 in saliva. Micromachines 11, 203 (2020).
Rood, I. G., Pettersson, A., Savelkoul, P. H. & de Korte, D. Performance and suitability of polymerase chain reaction for early detection of bacteria in platelet concentrates. Transfusion 51, 2006–2011 (2011).
Al-Soud, W. A. & Rådström, P. Purification and characterization of PCR-inhibitory components in blood cells. J. Clin. Microbiol. 39, 485–493 (2001).
Wolfe, K. A. et al. Toward a microchip-based solid-phase extraction method for isolation of nucleic acids. Electrophoresis 23, 727–733 (2002).
Weagant, S. D. & Bound, A. J. Evaluation of techniques for enrichment and isolation of Escherichia coli O157: H7 from artificially contaminated sprouts. Int. J. Food Microbiol. 71, 87–92 (2001).
Chung, Y.-C. et al. Microfluidic chip for high efficiency DNA extraction. Lab Chip 4, 141–147 (2004).
Park, C. et al. 3D-printed microfluidic magnetic preconcentrator for the detection of bacterial pathogen using an ATP luminometer and antibody-conjugated magnetic nanoparticles. J. Microbiol. Methods 132, 128–133 (2017).
Kim, Y., Lee, J. & Park, S. A 3D-printed millifluidic platform enabling bacterial preconcentration and DNA purification for molecular detection of pathogens in blood. Micromachines 9, 472 (2018).
Lin, Y.-S., Tsai, P.-J., Weng, M.-F. & Chen, Y.-C.J.A. Affinity capture using vancomycin-bound magnetic nanoparticles for the MALDI-MS analysis of bacteria. Anal. Chemi. 77(6), 1753–1760 (2005).
You, Q., Zhang, X., Wu, F.-G., Chen, Y. J. S. & Chemical, A. B. Colorimetric and test stripe-based assay of bacteria by using vancomycin-modified gold nanoparticles. Sens. Actuators B Chem. 281, 408–414 (2019).
Zhong, D., Zhuo, Y., Feng, Y. & Yang, X. J. B. Bioelectronics, Employing carbon dots modified with vancomycin for assaying Gram-positive bacteria like Staphylococcus aureus. Biosens. Bioelectron. 74, 546–553 (2015).
Domingues, M. M. et al. Biophysical characterization of polymyxin B interaction with LPS aggregates and membrane model systems. Pept. Sci. 98, 338–344 (2012).
WilmsSchröer, D. F., Paul, T. J. & Schmidt, S. Switchable adhesion of E. coli to thermosensitive carbohydrate-presenting microgel layers: A single-cell force spectroscopy study. Langmuir 36, 1255–1256 (2020).
Xuan, S., Wang, Y.-X.J., Yu, J. C. & Leung, K.C.-F. Tuning the grain size and particle size of superparamagnetic Fe3O4 microparticles. Chem. Mater. 21, 5079–5087 (2009).
Mathew, J., Sankar, P. & Varacallo, M. Physiology, blood plasma, StatPearls [Internet], DOI (2021)
Cristofaro, M. F., Beauregard, D. A., Yan, H., Osborn, N. J. & Williams, D. H. Cooperativity between non-polar and ionic forces in the binding of bacterial cell wall analogues by vancomycin in aqueous solution. J. Antibiot. 48, 805–810 (1995).
Cunha, B. A., Mickail, N. & Eisenstein, L. E. faecalis vancomycin-sensitive enterococcal bacteremia unresponsive to a vancomycin tolerant strain successfully treated with high-dose daptomycin. Heart Lung 36, 456–461 (2007).
Ataee, R. A. et al. Determination of vancomycin minimum inhibitory concentration for ceftazidime resistant Streptococcus pneumoniaein Iran. Ann. Clin. Microbiol. Antimicrob. 13, 1–8 (2014).
Gu, H., Ho, P.-L., Tsang, K. W., Wang, L. & Xu, B. Using biofunctional magnetic nanoparticles to capture vancomycin-resistant enterococci and other gram-positive bacteria at ultralow concentration. J. Am. Chem. Soc. 125, 15702–15703 (2003).
Raetz, C. R. Biochemistry of endotoxins. Annu. Rev. Biochem. 59, 129–170 (1990).
Vagenende, V., Ching, T.-J., Chua, R.-J., Jiang, Q. Z. & Gagnon, P. Self-assembly of lipopolysaccharide layers on allantoin crystals. Colloids Surf B: Biointerfaces 120, 8–14 (2014).
Jacobs, M. R. FDA guidance on bacterial contamination risk control strategies to enhance the safety and availability of platelets: Advantages and limitations. Ann Blood 6, 18 (2021).
Herigstad, B., Hamilton, M. & Heersink, J. How to optimize the drop plate method for enumerating bacteria. J. Microbiol. Methods 44, 121–129 (2001).
Acknowledgements
This work was supported by the “Collabo R&D between Industry, Academy, and Research Institute” program funded by the Korean Ministry of SMEs and Startups in 2021 (Project No. S3104763), and by research Grant No. 2019-ER5402-01 from the Korean Disease Control and Prevention Agency.
Author information
Authors and Affiliations
Contributions
J.L., K.U.P., and Y.J.H. conceived and planned the experiments. J.L., A.T.A., S.O., H.E.C., W.T., and D.L. performed the experiments. W.T. synthesized the nanobeads. H.E.C. performed real-time PCR. J.L., A.T.A., S.P., and K.U.P. analyzed the data and wrote the manuscript. J.L., A.T.A., K.U.P., and Y.J.H. interpreted the results, reviewed the data, and contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J., Abafogi, A.T., Oh, S. et al. Molecular detection of bacterial contamination in plasma using magnetic-based enrichment. Sci Rep 12, 9151 (2022). https://doi.org/10.1038/s41598-022-12960-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12960-5
This article is cited by
-
Automated sepsis detection with vancomycin- and allantoin-polydopamine magnetic nanoparticles
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.