Abstract
China has the largest number of vaccinated population around the world. However, there has been few research on the prevalence and associated factors of vaccine hesitation among parents of preschool children. Therefore, we conducted this study to evaluate the status of vaccine hesitation and its associated factors among children’s parents. A cluster random sampling method was adopted to select six community health service centers in Shenzhen, and parents of preschool children who were immunized in the vaccination outpatient department of the selected community health centers were surveyed using a structured self-administered questionnaire. Vaccine hesitation was assessed by the Parent Attitudes about Childhood Vaccines (PACV) scale. A multiple linear regression analysis was used to assess the associated factors for vaccine hesitance among children's parents. A total of 1025 parents (response rate, 93.18%) filled out the questionnaires. The average score of vaccine hesitancy was 43.37 (SD = 10.34) points. 23.61% of parents wanted children to get all the recommended shots, 53.76% of them did not believe that many of the illnesses shots prevent were severe, and 75.41% of them could not guarantee the information they receive about shots. The results of multiple linear regression showed that the number of children in the family (β = −0.93, 95% CI: −1.31 to 0.54), health status of the child (β = 0.47, 95% CI: 0.07 to 0.87), education level of the parents (Father: β = −0.84, 95%CI: −1.37 to 0.31; Mother: = −1.59, 95%CI:−2.13 to −1.05), and annual family income (β = 1.64, 95%CI: 1.13–2.16) were significantly associated with vaccine hesitation. The average score of parents' vaccine hesitation in Shenzhen was 43.37. The results showed that the number of children in the family, health status of the children, education level of the parents and annual family income were important factors associated with the parents' vaccine hesitation.
Similar content being viewed by others
Introduction
Vaccine is one of the most effective measures to prevent infectious diseases, which saves more than three million deaths and prevents 750 thousand children from disability worldwide each year1. Since the invention of the first vaccine in the seventeenth century, more than twenty kinds of vaccines have been gradually applied to prevent diseases2.With the spread of COVID-19 around the world, great efforts were taken to develop vaccines against it, which also implied that vaccines play a pivotal role in the control of infectious diseases3.
In recent years, many researches have been carried out to improve vaccination rates worldwide. Vaccine hesitation, as an important aspect, received a lot of attention. Vaccine hesitancy is different from vaccination denial, which is somewhere in between total anti-vaccine and total pro-vaccine, and varies across time4. In 2012, vaccine hesitancy was defined by the World Health Organization (WHO) as a delay in acceptance or refusal of vaccination despite availability of vaccination services5,6.
According to the report of Centers for Disease Control of the United States, a quarter to a third of American children were affected by vaccine hesitancy7. A study conducted by Larson et al. reported that vaccine hesitation was particularly pronounced in Europe, where the rate of vaccine hesitation was 45.20% in France8. Jessica et al. 9 found that 43.00% of parents of children in Australia heavily concerned about vaccine efficacy, and approximately 25% of parents lacked confidence in vaccines. In addition, previous studies have shown that there were a few factors associated with vaccine hesitancy. A study by MacDonald et al.4 showed that age, sex, and place of residence were the influencing factors for vaccine hesitancy. Another study by Jacobson et al.10 showed that the number of children in one family and health status of children had a significant impact on parental vaccine hesitancy. This study by Xiao et al.11 showed that parents' education and income level were also potential influencing factors. Final, Williams12 found that the role of the primary caregiver of the children and time spent with children per day were possible associated with parents’ vaccine hesitancy.
China has the largest number of vaccination in the world each year13. According to the report by the Chinese Center for Disease Control, a total of 536 million vaccinations were administered in 201913,14. The Chinese government has attached great importance to vaccination. Since 1978, it has been implemented the National Program for Immunization of Children, and has established a complete vaccine chain and a strict vaccine management system15. However, there has been few research on the prevalence and associated factors of vaccine hesitation among Chinese parents of children. Rend et al.16 and Wagner et al.17 investigated the vaccine hesitancy among parents of infants and children (age < 18 years) in Shanghai, respectively. However, Wang et al.17 conducted a study to examine childhood vaccination delay, explore the association between vaccination delay and parental vaccine hesitancy, and assess childhood vaccination delays during the coronavirus disease 2019 (COVID-19) pandemic in Wuxi, China. However, our focused on the prevalence and associated factors of parental vaccine hesitancy in Songgang Street, Shenzhen. This study aimed to investigate the current situation of vaccine hesitation among Shenzhen parents of preschool children based on a cross-sectional survey, and to explore its influencing factors. This study will fill in the shortage of data on vaccine hesitancy, and provide an important basis for the progress of vaccination planning.
Results
Characteristics of participants
The average age of the mothers and fathers were 29.60 (SD = 4.70) and 31.70 (SD = 5.00) years, respectively. About 30% of children’s mothers and fathers had primary school or below. Less than half (44.10%) of respondents s annual family income ranged from 100 to 200 thousand RMB. Among them, the majority (80.00%) lived in rural areas and approximately 70% migrated from other provinces. More than 75% children were cared by their mothers (76.30%). The basic information of children and their parents is shown in Table 1.
Survey findings
The average score of vaccine hesitation was 43.37 (standard deviation, SD = 10.34). Responses to the individual items that make up the PACV scale are shown in Table 2.
With regard to vaccination behaviors, 71.22% of parents have delayed to have their child get a shot for reasons other than illness or allergy, and 74.73% of parents decided not to have their child get a shot for reasons other than illness or allergy.
In the aspect of general attitudes with vaccine, 25.56% of parents reported their concern that a shot might not prevent the disease. 23.61% of parents wanted children to get all the recommended shots, 53.76% of parents hesitated to believe that many of the illnesses shots prevent are severe, 75.41% of parents could not guarantee the information they receive about shots.
For vaccine safety and efficacy, 79.02% of parents concerned that their child might have a serious side effect from a shot in the item 14. 37.27% of parents worried that anyone of the childhood shots might not be safe. 85.17% of parents believed it is better for children to get fewer vaccines at the same time.
Influencing factors of parents' vaccine hesitation
Table 3 presents the results of the multiple linear regression model analysis. The fitted model was statistically significant (P < 0.001). The results showed that parents' vaccine hesitation was associated with five factors including the number of children in the family, the health status of the child, the education level of the parents (both father and mother), and the annual family income.
Vaccine hesitation among parents of child who was not the first child in the family was lower than that of those who had only one child (β = −0.93, 95%CI: −1.31 to −0.54). Parents of child who have poor health status had higher vaccine hesitation score than that of those whose child had good health status (β = 0.47, 95%CI: 0.07–0.87). The vaccine hesitation scores of parents with high financial status were higher compared with those with poor financial status (β = 1.64, 95%CI: 1.13–2.16). Compared with parents who had primary school of below, parents who had achieved a bachelor degree or above had lower vaccine hesitation scores (Father: β = −0.84, 95%CI: −1.37 to −0.31; Mother: β = −1.59, 95%CI: −2.13 to −1.05).
Discussion
As the decision makers of childhood immunization, parents' cognition and attitude about childhood vaccines have significant influence on their vaccine hesitation. Given the serious consequences of vaccine hesitation, it has attracted global concern in recent years. In order to solve the problem of vaccine hesitation, it is necessary to understand the current situation of vaccine hesitation among parents of child and clarify its influencing factors. This study showed that parents had a high level of vaccine hesitation in Shenzhen, China, and parents’ vaccine hesitation was significant associated with the number of children in the family, health status of children, education level of the parents, and annual family income.
The WHO Strategic Advisory Group of Experts (SAGE) Report from the Working Group on vaccine hesitancy showed that 93% of WHO member states reported vaccine hesitation, which indicated that vaccine hesitation was a globally social problem18. The results of this study showed that most Chinese parents had vaccine hesitation, although there was a difference in response. Vaccine hesitancy is different from vaccination denial, which is somewhere in between total anti-vaccine and total pro-vaccine, and varies across timeFor example, Qing He et al.19 found that 33.04% of parents were hesitant about vaccines one week after the vaccine safety accident occurred, but the percentage decreased six months later. In addition, vaccine hesitation was influenced by policy, culture, and religion, as well as measurement criteria of vaccine hesitant. It was certain that vaccine hesitant was common around the world18. For example, Alexander et al. examined global trendy of vaccine confidence using data from 290 surveys across 149 countries in 2015–201920 and found that confidence in the importance, safety, and effectiveness of vaccine decreased in Afghanistan, Indonesia, Pakistan, Philippines, and South Korean.
For influencing factors of vaccine hesitation, study of Metin et al.21 and Jessica et al.22 shown that parents' education level had an important impact on their vaccine hesitation. Previous studies conducted in Nigeria, India and Kyrgyzstan indicated that parents' lower education level was an obstacle to their children's vaccination23,24. Similarly, previous studies from the United States, Greece and the Netherlands had found that parents’ higher education was a promoter of vaccination15,21,25,26,27. This study also found the significant association between parents' educational background and their vaccine hesitation. To be specific, Chinese parents' vaccine hesitation decreased with the improvement of their educational background. A prior qualitative study showed that highly educated parents believed in their ability to make correct vaccination decisions based on their higher education level and self-sourced vaccination information28. Family income has also been identified in previous studies as an important factor affecting vaccine acceptance. Studies from the United States and Nigeria have shown that low family income is a barrier to vaccination services29,30. However, this study showed that parents with higher income levels scored higher on vaccine hesitation, which was inconsistent with the results from the United States and Nigeria. This could be due to that richer families are more likely to downplay the ill effects of illness.
In addition to parental factors, this study also found that factors such as the number of children and the health status of children were also significant associated with parental vaccine hesitation. To be specific, if the child was the first child in the family, parents’ hesitation degree would increase; by contrast, if the child was not the first child, parents has a stronger willingness to vaccinate their children, which may be associated with their vaccination experience.
Studies found that parents realized their responsibility in their children's health, but the responsibility was associated with anxiety and fear; thus, they were very cautious in vaccination for their children. One possible explanation was that parents worried that vaccination may hurt their children31,32. The results of this study confirmed this view, that is to say, the worse the health status of the vaccinated children, the higher the level of their parents' vaccine hesitation. Parental behaviors of vaccine rejection or vaccine hesitation was complex and multifaceted. It should be noted that concern about the efficacy and safety of vaccination among parents of preschool children should be considered in policy-making.
Strength and limitations
In 2020, more than 536 million vaccines were administered in China. As a country with a maximum of vaccination for children, China had few researches on preschool children parents' vaccine hesitation. This is the first study to be carried out in Shenzhen. Although this study was a cross-sectional study in cities, it recruited the largest number of participants and described parents’ vaccine hesitation comprehensively. This study can precisely reflect the current statuses of vaccine hesitant among parents of preschool children, which will be helpful to improve vaccination program, and provide valuable results regarding vaccine hesitant internationally.
The limitation of this study was that the potential influencing factors for vaccine hesitancy among parents could be more than those included in the questionnaire. The respondents we included in the study were all parents of preschool children, but may not be representative of all parents of preschool children, because some parents may choose hospitals or other medical institutions to vaccinate their children. Secondly, this was a cross-sectional study design, which precluded evaluation of temporality and causality of the observed relationships. Additional studies could consider conducting a community-based survey to evaluate the situation of parents' vaccine hesitation more comprehensively in China.
Conclusions
The average score of parents' vaccine hesitation in Shenzhen was 43.37. The number of children in the family, health status of the children, education level of the mother/father, and annual family income were significant associated with parents' vaccine hesitation. Appropriate interventions are recommended to alter parents' hesitation about vaccines and ultimately ensure the sustainable development of immunization programme.
Methods
Ethics statement
This study was approved by the Research Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China and performed in accordance with the principles of the Declaration of Helsinki. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire.
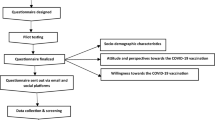
Survey instrument
In the present study, vaccine hesitation was measured using the Parent Attitudes about Childhood Vaccines (PACV) scale, which was developed by Opel et al. PACV was a 15-item scale that assessed the vaccine hesitation in three dimensions, including the vaccination behaviors, immunization safety and beliefs on vaccine safety and efficacy, and the attitudes on vaccine mandates. Each item has three answers including "agree", "uncertain" and "disagree", coded with value of "2", "1" and "0", respectively. The total score was computed as the sum of all items, ranging from 0 to 30, with higher scores indicating higher levels of vaccine hesitation. We converted this raw score to a 0–100 scale using simple linear transformation33. In previous studies, this scale has been applied to the Chinese population, and its reliability in the Chinese population has been verified34. The scale has shown good internal consistency (Cronbach’s α for the 3 sub-scale were 0.72, 0.83, and 0.77, respectively35.
In addition, information about participants' sociodemographic characteristics including age, sex, education, monthly family income, number of children, and age, sex, and health status of the youngest children were also collected. These factors mainly come from the previous literature4,9,10,11 and consultation with experts in related fields.
Study population
This was a cross-sectional study and data were collected from October to December 2019 in the city of Shenzhen, Guangdong Province (Southern China). A cluster random sampling method was adopted in the present study. First, six community health service centers were randomly selected from the twelve community health service centers affiliated to the Song-gang People's Hospital in Shenzhen, which covered more than 600 thousand population in Song-gang Street. In our study, a 95% confidence level and ± 5% precision are assumed for the Equation.
where n is the sample size, N is the population size, and e was the level of precision. Thus, the conservative total sample size for this questionnaire was 400.
Second, all parents of preschool children who were immunized in the vaccination outpatient department at the study sites during the study period were recruited. A total of 1100 parents of children were enrolled and filled out a structured self-administered questionnaire, and 1025 valid questionnaires were collected with effective response rate of 93.18%. We noted in the questionnaire: Good health status meant that children adopt to various changes in the environment, had no general diseases, and had sufficient energy. Moderate health status meant that children were in an intermediate state between health and disease, and they experienced fatigue, weight loss, weakness and indigestion. Poor health was when a child was in a serious health-threatening condition such as infection, illness or malnutrition.
Statistical analysis
SPSS 25.0 was applied to analyze the data. Descriptive analyses included means for continuous variables and percentages for categorical data. A multiple linear regression model was used to examine the associations of independent variables with parents’ vaccine hesitation scores. All comparisons were two-tailed and a P value of < 0.05 was defined as statistically significant.
Ethics approval and consent to participate
This study protocol was approved by the institutional review board of Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China. Respondents were informed that their participation was voluntary, and informed consent was implied on the completion of the questionnaire.
Data availability
Data may be made available by contacting the corresponding author.
References
Gualano, M. R. et al. Knowledge, attitudes and beliefs towards compulsory vaccination: A systematic review. Hum. Vaccin. Immunother. 15(4), 918–931 (2019).
Costa-Pinto, J. C. et al. Parental immunisation needs and attitudes survey in paediatric hospital clinics and community maternal and child health centres in Melbourne, Australia. J. Paediatr. Child Health. 54(5), 522–529 (2018).
Callaway, E. The race for coronavirus vaccines: A graphical guide. Nature 580(7805), 576–577 (2020).
MacDonald, N. E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 33(34), 4161–4164 (2015).
Peng, Z. B. et al. Current situation and related policies on the implementation and promotion of influenza vaccination, in China. Zhonghua Liu Xing Bing Xue Za Zhi 39(8), 1045–1050 (2018).
Dubé, E., Gagnon, D., Nickels, E., Jeram, S. & Schuster, M. Mapping vaccine hesitancy–country-specific characteristics of a global phenomenon. Vaccine 32(49), 6649–6654 (2014).
Prevention CFDC. Frequently asked questions about measles in the U.S.; 2019.
Larson, H. J. et al. The state of vaccine confidence 2016: Global insights through a 67-Country survey. EBioMedicine 12, 295–301 (2016).
Kaufman, J., Tuckerman, J. & Danchin, M. Overcoming COVID-19 vaccine hesitancy: Can Australia reach the last 20 percent?. Exp. Rev. Vacc. 21, 1–3 (2021).
Jacobson, R. M., St, S. J. & Finney, R. L. Vaccine hesitancy. Mayo. Clin. Proc. 90(11), 1562–1568 (2015).
Xiao, X. & Wong, R. M. Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 38(33), 5131–5138 (2020).
Williams, S. E. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it?. Hum. Vaccin. Immunother. 10(9), 2584–2596 (2014).
WHO. Vaccines and immunization, 2021.
Yang, R., Penders, B., Horstman, K. Addressing vaccine hesitancy in China: A scoping review of Chinese scholarship. Vaccines (Basel). 8(1), 2019.
Akmatov, M. K., Mikolajczyk, R. T., Kretzschmar, M. & Krämer, A. Attitudes and beliefs of parents about childhood vaccinations in post-soviet countries: The example of Kyrgyzstan. Pediatr. Infect. Dis. J. 28(7), 637–640 (2009).
Ren, J. et al. The demographics of vaccine hesitancy in Shanghai, China. PLoS ONE 13(12), e209117 (2018).
Wang, Q. et al. Delays in routine childhood vaccinations and their relationship with parental vaccine hesitancy: A cross-sectional study in Wuxi, China. Exp. Rev. Vacc. 26, 1–9 (2021).
Lane, S., MacDonald, N. E., Marti, M. & Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF joint reporting form data-2015–2017. Vaccine 36(26), 3861–3867 (2018).
He, Q. et al. Changes in parents’ decisions pertaining to vaccination of their children after the Changchun Changsheng vaccine scandal in Guangzhou, China. Vaccine 38(43), 6751–6756 (2020).
de Figueiredo, A., Simas, C., Karafillakis, E., Paterson, P. & Larson, H. J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 396(10255), 898–908 (2020).
Yigit, M., Ozkaya-Parlakay, A. & Senel, E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr. Infect. Dis. J. 40(4), e134–e136 (2021).
Kaufman, J. et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst. Rev. 5(5), D10038 (2018).
Antai, D. Gender inequities, relationship power, and childhood immunization uptake in Nigeria: A population-based cross-sectional study. Int. J. Infect. Dis. 16(2), e136–e145 (2012).
Patel, T. A. & Pandit, N. B. Why infants miss vaccination during routine immunization sessions? Study in a rural area of Anand District, Gujarat. Indian J. Publ. Health. 55(4), 321–323 (2011).
Rammohan, A., Awofeso, N. & Fernandez, R. C. Paternal education status significantly influences infants’ measles vaccination uptake, independent of maternal education status. BMC Publ. Health. 12, 336 (2012).
Danis, K., Georgakopoulou, T., Stavrou, T., Laggas, D. & Panagiotopoulos, T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: A cross-sectional study in Greece. Vaccine 28(7), 1861–1869 (2010).
Uwemedimo, O. T., Findley, S. E., Andres, R., Irigoyen, M. & Stockwell, M. S. Determinants of influenza vaccination among young children in an inner-city community. J. Comm. Health. 37(3), 663–672 (2012).
Swaney, S. E. & Burns, S. Exploring reasons for vaccine-hesitancy among higher-SES parents in Perth, Western Australia. Health Promot. J. Austr. 30(2), 143–152 (2019).
Wu, A. C. et al. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern. Child Health J. 12(6), 766–773 (2008).
Antai, D. Faith and child survival: The role of religion in childhood immunization in Nigeria. J. Biosoc. Sci. 41(1), 57–76 (2009).
Glanz, J. M. et al. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad. Pediatr. 13(5), 481–488 (2013).
Harmsen, I. A. et al. Factors that influence vaccination decision-making by parents who visit an anthroposophical child welfare center: A focus group study. Adv. Prev. Med. 2012, 175694 (2012).
Wolfensberger, W. & Tullman, S. A brief outline of the principle of normalization. Rehabil. Psychol. 27(3), 131–145 (1982).
Kong, G., Morean, M. E., Cavallo, D. A., Camenga, D. R. & Krishnan-Sarin, S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob. Res. 17(7), 847–854 (2015).
Opel, D. J. et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 29(38), 6598–6605 (2011).
Acknowledgements
We thank all the participants in this study.
Funding
This study was supported by the National Social Science Foundation of China (18ZDA085) and Science and Technology Innovation Commission of Shenzhen.
Author information
Authors and Affiliations
Contributions
X.S. and X.W. conceived and designed the study. Z.D. and X.L. participated in the acquisition of data. Y.Z. and Y.H. analyzed the data. Y.D. and Q.T. gave advice on methodology. X.S. drafted the manuscript. Z.L., Y.G. and Y.H.G. revised the manuscript. All authors read and approved the final manuscript. Z.L. is the guarantor of this work and had full access to all the data in the study and takes responsibility for its integrity and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, X., Wu, X., Deng, Z. et al. Analysis on vaccine hesitation and its associated factors among parents of preschool children in Songgang Street, Shenzhen. Sci Rep 12, 9467 (2022). https://doi.org/10.1038/s41598-022-12530-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12530-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.