Abstract
The optimal time when surgery can be safely performed after stroke is unknown. The purpose of this study was to investigate how cardiac surgery timing after stroke impacts postoperative outcomes between 2011–2017 were reviewed. Variables were extracted from the institutional Society of Thoracic Surgeons database, statewide patient registry, and medical records. Subjects were classified based upon presence of endocarditis and further grouped by timing of preoperative stroke relative to cardiac surgery: Recent (stroke within two weeks before surgery), Intermediate (between two and six weeks before), and Remote (greater than six weeks before). Postoperative outcomes were compared amongst groups. 157 patients were included: 54 in endocarditis and 103 in non-endocarditis, with 47 in Recent, 26 in Intermediate, and 84 in Remote. 30-day mortality and postoperative stroke rate were similar across the three subgroups for both endocarditis and non-endocarditis. Of patients with postoperative stroke, mortality was 30% (95% CI 4.6–66). Timing of cardiac surgery after stroke occurrence does not seem to affect postoperative stroke or mortality. If postoperative stroke does occur, subsequent stroke-related mortality is high.
Similar content being viewed by others
Introduction
Stroke in the perioperative period represents a major source of the stroke burden in the United States, with up to $4 billion in additional healthcare costs annually being attributed to cardiac surgery patients alone1,2. Compared to general surgical operations, cardiac surgery carries a much greater risk of stroke especially with valvular procedures1,2,3. Stroke following cardiac surgery has been shown to result in worse short- and long-term mortality as well as increased lengths of stay3,4.
Risk factors for postoperative stroke after cardiac surgery are numerous1,3,4,5. In fact, one such risk factor is previous stroke3,4,5,6. Timing of non-cardiac surgery has been well studied, and some have demonstrated elevated risk of postoperative stroke for up to nine months following neurological insult7,8. However, there is scant data regarding stroke and cardiac surgery, and the optimal timing when cardiac surgery can be safely performed after stroke is largely unknown. Guidelines from major cardiothoracic surgical professional societies generally indicate that surgery within 48 h of stroke is reasonable in the presence of strong surgical indications for surgery, but, if possible, to delay surgery for up to 4 weeks in cases of large territorial stroke or intracranial hemorrhage9,10,11,12. Some have shown acceptable outcomes for surgery within 2 weeks even in cases of intracranial hemorrhage13,14. There remains a paucity of data on whether the etiology of stroke plays a role; for example, stroke in patients with infective endocarditis (IE) is likely due to septic embolization, which may inherently be different than stroke in patients with atherosclerotic vascular and coronary artery disease.
We reviewed our experience with preoperative stroke in both IE and non-IE patient populations. We not only sought to define optimal timing from stroke to intervention but also to characterize how preoperative stroke impacts postoperative outcomes including stroke. We hypothesized that the shorter the duration between preoperative stroke and cardiac surgery, the greater the risk of postoperative stroke and mortality.
Materials and methods
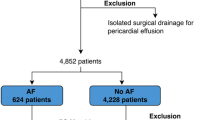
This single-center retrospective study was approved by the Institutional Review Board of Indiana University and conducted in accordance with all University guidelines and regulations. Informed consent by individual study patients was waived by the Institutional Review Board of Indiana University. We queried the prospective institutional Society of Thoracic Surgeons (STS) data registry to identify all patients with preoperative stroke who underwent cardiac surgery at our institution between 2011 and 2017 and also confirmed by ICD-9 codes. Cases where the index operation was ventricular assist device implantation, heart transplantation, or transcatheter valve replacement were excluded. Preoperative, intraoperative, and postoperative variables were extracted from this STS data registry, individual medical records, and a state-wide patient data registry (Regenstrief Institute, Indianapolis, IN). The latter allowed capture of patient data even if medical attention were received at an institution other than ours as long as it was within the state.
Patients were divided into two groups based on the presence of IE (IE vs. non-IE), and then further classified by timing of the preoperative stroke relative to the cardiac surgical procedure date (Fig. 1): Recent (stroke within 2 weeks before surgery), Intermediate (greater than 2 weeks but less than 6 weeks before), and Remote (greater than 6 weeks before). Patients with unknown preoperative stroke date were excluded from analysis. All preoperative stroke imaging, either magnetic resonance imaging (MRI) or computed tomography (CT), was reviewed to ascertain anatomic location and territory. Postoperative outcomes were reviewed and compared amongst the three subgroups for both the IE and non-IE populations. Primary outcomes studied were 30-day mortality and incidence of postoperative stroke. Secondary outcomes included postoperative length of stay (LOS) and complications.
Statistical analysis
Bivariate analysis was used to compare baseline characteristics between IE and non-IE groups. Kruskal–Wallis and Chi-Square tests were utilized for continuous and categorical variables, respectively. Using a backwards-stepwise logistic regression model, age, preoperative length LOS, and cross clamp time were selected as significant contributing variables for multivariable analysis against postoperative stroke rates. Boosted tree and random forest models also demonstrated these variables to be the top three important predictors of postoperative stroke. Statistical analysis was performed using RStudio (RStudio, Boston, MA) software.
Results
210 patients were identified as having preoperative stroke prior to cardiac surgery. Of these, 50 were excluded from the study due to unknown timing of the preoperative stroke, leaving 157 subjects in the study: 54 in IE and 103 in non-IE. Within the IE group, 27 (50.0%) were in Recent, 15 (27.8%) in Intermediate, and 12 (22.2%) in Remote. In the non-IE group, 20 (19.4%) were in Recent, 11 (10.7%) in Intermediate, and 72 (69.9%) in Remote. Median follow-up in those who did and did not experience postoperative stroke are 1938 and 1070 days, respectively. Overall mortality was 6/157, or 3.8% (95% CI 1–7).
Infective endocarditis
The mean age was 48 years, with 70% male and 69% Caucasian. Baseline characteristics were mostly similar across the three subgroups, with the exception of dyslipidemia and hypertension both being more common in the Remote group (Table 1). 37% had a history of illicit drug use. The majority of strokes were ischemic variant with either multi-territory or internal carotid artery anatomic distribution. The most common symptoms of the stroke were motor nerve defects and impaired consciousness. The proportion of cases classified as elective was different across the subgroups, comprising 41.7% of Remote cases and only 3.7% and 6.7% of Recent and Intermediate cases, respectively (Table 2). The majority of operations were isolated valve surgery with no significant differences in cardiopulmonary or crossclamp times across groups.
Postoperative stroke rates and 30-day mortality were 3.7% (95% CI 2–9) (n = 2) and 9.3% (95% CI 1.3–17) (n = 5), respectively, and were not different across the three subgroups (Table 3). Postoperative LOS was different across subgroups, with Remote having the shortest LOS (6.5 days) and Recent having the longest (13 days). Table 4 lists details of the postoperative strokes: patient 1 was in the Recent group with an ischemic stroke 7 days prior to undergoing mitral valve replacement with postoperative ECMO support. Postoperatively, stroke occurred on postoperative day 1 as an ischemic variant with multi-territory involvement and the patient died two days later due to multisystem organ failure. Patient 2 was in the Remote group with ischemic stroke 208 days prior to mitral valve replacement and suffered postoperative stroke on postoperative day 56 as a complex variant with left middle cerebral artery (MCA) territory involvement. There was hemorrhagic conversion of this stroke and the patient died 3 days later. There was no correlation between preoperative stroke variables, including variant, anatomic/territory involvement, and presenting symptom, and postoperative outcomes.
Non-endocarditis
Baseline demographics were similar across the three subgroups with respect to age and BMI. Prior MI, dyslipidemia, and hypertension were more common in the Remote group (Table 1). The majority of pre-operative strokes were ischemic and symptomatic with motor nerve involvement, but there was no difference amongst the three subgroups. There were significantly more elective cases in the Remote group than others and the types of cases across groups were similar. Intraoperative variables were similar, including the duration of cardiopulmonary bypass and crossclamp period (Table 2).
Postoperative stroke rate and 30-day mortality were 7.7% (n = 8) (95% CI 2.5–13) and 4.9% (n = 5) (95% CI 7–9.4), respectively, and were not different across subgroups (Table 3). Remote had the lowest postoperative stroke rate followed by Intermediate and then Recent, although this was not statistically significant. Postoperative atrial fibrillation (AF) was most common in Recent, followed by Intermediate and then Remote. Postoperative LOS was shortest in the Remote group (7.0 days) and longest in Recent (11.5 days), with Remote having the greatest proportion that discharged to home (vs. an institutional facility).
All postoperative strokes were ischemic in nature and the occurrence of stroke ranged from day of surgery to postoperative day 1908 (Table 4), with most occurring within the first 10 days after surgery. Of the patients who suffered postoperative stroke, three died due to stroke related complications, including hemorrhagic conversion, tonsillar herniation, and absence of neurologic recovery/brain death. These stroke deaths occurred relatively quickly after stroke, ranging from day of stroke to 5 days after stroke. Multivariate logistic analysis did not identify any particular variables that predicted postoperative stroke in any of the subgroups (Table 5).
Discussion
There remains little published data regarding the effect of preoperative stroke and outcomes following cardiac surgery. Most recommendations are based on either the experience of non-cardiac surgery or observational studies focusing on the IE population in cardiac surgery8,13,14,15,16,17,18. The decision and timing of cardiac surgery following stroke remains debated. Our results suggest that there is no direct relationship between timing of cardiac surgery after a stroke and postoperative outcomes of stroke and mortality—our data do not reveal a protective effect of time between stroke and cardiac surgery. Time to intervention from preoperative stroke did not influence frequency of mortality or postoperative stroke in either IE or non-IE populations. This contradicts some published data that suggest there is an increased risk of postoperative stroke particularly in IE, and that waiting 2–4 weeks following stroke might reduce the risk of postoperative stroke8,9,10,11,12,19. However, other investigators have reported results similar to ours, whereby preoperative stroke in IE is not associated with significant increase in postoperative stroke after valve surgery14,20,21. We surmise that preoperative stroke in IE is primarily related to septic emboli, and it is likely that induction of antimicrobial therapy prior to cardiac surgery reduces subsequent stroke risk22. Unlike the non-IE groups, there is likely no underlying atherosclerotic disease in patients with IE that would predispose to stroke occurrence. Based on our data, in patients with IE it appears that the presence of stroke should not necessarily affect timing of surgery, as there is no significant increase in postoperative mortality or stroke.
In the non-IE population, our data show a greater rate of postoperative stroke (7.7%) than in IE, but again there does not seem to be a correlation with the time interval between preoperative stroke and surgery. The Recent group had a greater absolute percentage of postoperative stroke than the Remote group, but this difference was not statistically significant. Interestingly, the rates of postoperative AF were greatest in Recent and lowest in Remote, which initially led us to believe that postoperative AF and postoperative stroke were related. However, we could not find a meaningful association between the two. Among the cases with postoperative stroke, there were equal numbers of isolated coronary bypass and isolated valve surgery. The strokes following isolated coronary surgery seemed to occur later, but again this was not statistically significant. The territory and symptoms of postoperative stroke were not affected by details of the preoperative stroke; in other words, a patient with hemiparesis due to left middle cerebral artery involvement in preoperative stroke did not place the patient at higher risk for a similarly located postoperative stroke. Furthermore, six of the ten postoperative occurred within the first ten postoperative days; the other four occurred at postoperative day 56, 99, 108, and 1908. We surmise that the six strokes occurring in the early postoperative period are likely related to the surgery itself (as a postoperative complication), while the four that occurred more than one month after surgery are likely unrelated to surgery. Even taking into account these late strokes, our data suggest that the presence of pre-operative stroke does not definitively increase risk of postoperative stroke. As with IE, in non-IE patients with a history of stroke, our data suggest that cardiac surgery can be performed without affecting postoperative mortality or stroke, regardless of interval between stroke and surgery.
Across all patients who have postoperative stroke, the stroke-related mortality was 30%. This is consistent with a recent review by Sultan et al. of 10,250 patients which revealed a mortality of 14.9% in patients who suffered a symptomatic postoperative stroke after cardiac surgery23. This underscores the importance of preventing postoperative stroke, as it seems the presence of postoperative stroke correlates with increased mortality. Before discharge all patients are administered medical therapy for cardiovascular optimization (blood pressure control, antiplatelets/anticoagulation, hyperlipidemia control, etc.) as long as there are no contraindications. The specific agents were determined often by preoperative baseline medications (if a patient was on amlodipine preoperatively, for example, that agent was resumed) and contemporary cardiac surgery/cardiology guidelines (for instance, antiplatelets with either aspirin or clopidogrel as well as a statin for patients undergoing coronary bypass surgery). It is possible that the variability in postoperative medical regimen could have affected risk of postoperative stroke, but the present study was not designed to distinguish this effect. Nonetheless, the timing of surgery following preoperative stroke does not appear to affect postoperative stroke rate and our data would not support delaying cardiac surgical intervention merely due to the presence of stroke alone.
There are limitations to this single center retrospective study. First, the relatively low sample size combined with the low incidence of postoperative stroke and mortality may contribute to difficulty in identifying significant relationships. We had initially sought to utilize a larger multi-institutional data registry, yet there was no such registry that contained the granular level of information (e.g., stroke variant, territory involvement, symptoms, intraoperative details, postoperative stroke and death details, etc.) necessary to test our hypothesis. Analyzing individual patient level data allowed us to investigate more detailed variables than would have been possible with larger registries. Second, this study selected for patients who ultimately underwent cardiac surgery. Excluded were patients who were too ill from the preoperative stroke to tolerate cardiac surgery, which may have affected outcomes. Our institutional database does not allow for identification of patients who were deemed not surgical candidates and were treated with non-surgical modalities for their cardiac disease.
Conclusions
Our study suggests that the presence of preoperative stroke may not affect postoperative mortality and stroke, and that cardiac surgery can be safely performed regardless of the time interval between stroke and surgery. Preoperative variables including details of preoperative stroke do not correlate with risk of postoperative stroke. Multiple factors are considered in the decision and timing of cardiac surgery, but the presence and type of preoperative stroke may not need to play a major role.
References
Selim, M. Perioperative stroke. N. Engl. J. Med. 356(7), 706–713 (2007).
D’Agostino, R. S. et al. The society of thoracic surgeons adult cardiac surgery database: 2019 update on outcomes and quality. Ann. Thorac. Surg. 107(1), 24–32 (2019).
John, R. et al. Multicenter review of preoperative risk factors for stroke after coronary artery bypass grafting. Ann. Thorac. Surg. 69(1), 30–35 (2000).
Filsoufi, F., Rahmanian, P. B., Castillo, J. G., Bronster, D. & Adams, D. H. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann. Thorac. Surg. 85(3), 862–870 (2008).
Ricotta, J. J., Faggioli, G. L., Castilone, A. & Hassett, J. M. Risk factors for stroke after cardiac surgery: Buffalo cardiac-cerebral study group. J. Vasc. Surg. 21(2), 359–363 (1995).
Merie, C. et al. Risk of stroke after coronary artery bypass grafting: Effect of age and comorbidities. Stroke 43(1), 38–43 (2012).
Jorgensen, M. E. et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA 312(3), 269–277 (2014).
Sanders, R. D., Jorgensen, M. E. & Mashour, G. A. Perioperative stroke: A question of timing?. Br. J. Anaesth. 115(1), 11–13 (2015).
Pettersson, G. B. et al. 2016 the american association for thoracic surgery (aats) consensus guidelines: Surgical treatment of infective endocarditis: Executive summary. J. Thorac. Cardiovasc. Surg. 153(6), 1241-1258.e1229 (2017).
Baddour, L. M. et al. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the american heart association. Circulation 132(15), 1435–1486 (2015).
Habib, G. et al. 2015 esc guidelines for the management of infective endocarditis The task force for the management of infective endocarditis of the European society of cardiology (esc). G. Ital. Cardiol. (Rome) 17(4), 277–319 (2016).
Byrne, J. G. et al. Surgical management of endocarditis: The society of thoracic surgeons clinical practice guideline. Ann. Thorac. Surg. 91(6), 2012–2019 (2011).
Angstwurm, K. et al. Timing the valve replacement in infective endocarditis involving the brain. J. Neurol. 251(10), 1220–1226 (2004).
Yoshioka, D. et al. Valve surgery in active endocarditis patients complicated by intracranial haemorrhage: The influence of the timing of surgery on neurological outcomes. Eur. J. Cardiothorac. Surg. 45(6), 1082–1088 (2014).
Tam, D. Y. et al. Early vs late surgery for patients with endocarditis and neurological injury: A systematic review and meta-analysis. Can. J. Cardiol. 34(9), 1185–1199 (2018).
Kang, D. H. et al. Early surgery versus conventional treatment for infective endocarditis. N. Engl. J. Med. 366(26), 2466–2473 (2012).
Eishi, K. et al. Surgical management of infective endocarditis associated with cerebral complications. Multi-center retrospective study in Japan. J. Thorac. Cardiovasc. Surg. 110(6), 1745–1755 (1995).
Okita, Y. et al. Optimal timing of surgery for active infective endocarditis with cerebral complications: A japanese multicentre study. Eur. J. Cardiothorac. Surg. 50(2), 374–382 (2016).
Rossi, M., Gallo, A., De Silva, R. J. & Sayeed, R. What is the optimal timing for surgery in infective endocarditis with cerebrovascular complications?. Interact. Cardiovasc. Thorac. Surg. 14(1), 72–80 (2012).
Piper, C., Wiemer, M., Schulte, H. D. & Horstkotte, D. Stroke is not a contraindication for urgent valve replacement in acute infective endocarditis. J. Heart Valve Dis. 10(6), 703–711 (2001).
Morita, K., Sasabuchi, Y., Matsui, H., Fushimi, K. & Yasunaga, H. Outcomes after early or late timing of surgery for infective endocarditis with ischaemic stroke: A retrospective cohort study. Interact. Cardiovasc. Thorac. Surg. 21(5), 604–609 (2015).
Dickerman, S. A. et al. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: An analysis from the ice prospective cohort study (ice-pcs). Am. Heart. J. 154(6), 1086–1094 (2007).
Sultan, I. et al. Predictors and outcomes of ischemic stroke after cardiac surgery. Ann. Thorac. Surg. 110(2), 448–456 (2020).
Author information
Authors and Affiliations
Contributions
Study conception and design: T.H., L.S.L. Data collection and analysis: T.H., C.R.M., M.M., N.W.V., Z.F., L.S.L. Statistical analysis: C.R.M., C.L.C., N.N. Manuscript writing: C.R.M., T.H., L.S.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matthews, C.R., Hartman, T., Madison, M. et al. Preoperative stroke before cardiac surgery does not increase risk of postoperative stroke. Sci Rep 11, 9025 (2021). https://doi.org/10.1038/s41598-021-88441-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88441-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.