Abstract
Surgical intervention for umbilical diseases in calves, when indicated, is a complementary and indispensable therapeutic resource for the treatment of umbilical conditions and is commonly performed using celiotomy. However, laparoscopy has demonstrated feasibility in many diagnostic and therapeutic procedures. The aim of this study was to assess the feasibility of the techniques and the surgical time of laparoscopy and celiotomy used in intra-abdominal resection of the umbilical vein and urachus of bovine fetuses (cadavers). Resection of the umbilical vein and urachus using laparoscopy and celiotomy was performed in 26 anatomical specimens (bovine fetuses obtained from an official slaughterhouse). Resection of umbilical structures was feasible with both techniques, but shorter surgical time and minimal tissue damage were achieved using laparoscopy. Laparoscopy requires specialized training and appropriate instruments and is an important tool for diagnostic and therapeutic exploration of the umbilical structures, liver, bladder, and associated/adjacent structures.
Similar content being viewed by others
Introduction
Umbilical disorders are often diagnosed in newborn bovine calves, and their etiologies may be associated with infections of the umbilical vessels and urachus, persistent urachus, and umbilical hernias1. In many cases, drug therapy alone is not sufficient to treat these conditions, and surgical intervention is a complementary and indispensable therapeutic resource for effective management of these disorders2,3,4.
For the satisfactory and effective treatment of umbilical infections, reduction of bacterial load and removal of infected structures likely to have low antimicrobial penetration are indispensable as they significantly improve the prognosis of these diseases5. Surgical resection of umbilical structures is indicated for the treatment of calves with infected umbilical components and patent urachus and is usually performed using celiotomy6,7.
Surgical resection of umbilical components using celiotomy has been shown to be effective for the treatment of omphalitis in calves, and it is easily performed by the surgeon using conventional surgical instruments, unlike laparoscopy, which requires special equipment and instruments that are usually more expensive than conventional ones, a fact that greatly influences their application in veterinary medicine8,9,10. In addition, performing laparoscopy requires the surgeon to have specific skills that can only be acquired with specialized training11,12,13. Therefore, the advantages of celiotomy make it the most used surgical technique in cases of umbilical conditions requiring surgical treatment3,7.
Laparoscopy is a minimally invasive technique and an important alternative to celiotomy that allows, in addition to the observation of abdominal organs and structures, surgical techniques and exploratory procedures to be performed with less pain and better recovery for the patient than conventional techniques13. The use of laparoscopy in cattle is promising; there are many potential applications, and, because it is a safe and effective technique, it is an important alternative to conventional methods11,14.
Surgical indication for the treatment of omphalitis should be preceded by a complete clinical examination, in particular an examination of the umbilical structures, with palpation of the umbilical region associated with ultrasound and/or laparoscopy, thereby allowing the surgeon to determine the severity of the abnormality and establish an appropriate surgical plan for the management of the specific case10,15,16,17.
Data on the feasibility of the techniques and surgical time of procedures performed for anatomical specimens provide important information for the execution of these procedures in live animals. Thus, the objective of the present study was to assess the feasibility and the surgical time of laparoscopy and celiotomy for intra-abdominal resection of the umbilical vein and urachus of bovine fetuses (cadavers).
Materials and methods
Study site and groups
This study was carried out in accordance with the recommendations of the National Council for Experimentation Control in Brazil (CONCEA). This research was approved by the Animal Ethics and Welfare Committee of the Federal University of Pará (protocol N ° 4848261017). As the study corresponds to a new experimental technique, all surgical procedures were performed on cadavers from a local slaughterhouse in accordance with inspection requirements. Thus, the procedures did not cause pain or suffering in animals, as they were performed on bovine fetuses from the slaughtered of pregnant cows.
The experiment was conducted at the Institute of Veterinary Medicine (IMV) in Campus II of the Federal University of Pará (UFPA), located in the municipality of Castanhal, Pará, Brazil, and involved the resection of the umbilical vein and urachus using laparoscopy and celiotomy in 26 anatomical specimens (weighing between 30 and 40 kg, bovine fetuses from cows slaughtered in the last third of gestation.
The anatomical specimens were classified into two study groups: one group with 13 anatomical specimens that underwent resection of the umbilical vein and urachus using laparoscopy, i.e., laparoscopic surgery (LG, n = 13) and the other group with 13 anatomical specimens that underwent resection of the umbilical vein and urachus using celiotomy, i.e., open surgery (OG, n = 13).
All the steps of the procedures in both groups were performed by the same surgeon in a standardized and systematic manner throughout the study.
The feasibility of the techniques and the surgical time (both the total time and that of the steps of abdominal cavity entry, resection of the umbilical vein, resection of the urachus, and closure of the abdominal cavity) were analyzed in all the anatomical specimens in both groups. A descriptive comparison of both techniques was performed, in which the feasibility of performing the surgical procedures was assessed.
Instruments and equipment used in the study
The experimental simulation of the surgical procedures took into consideration all the surgical principles applicable to laparoscopy and conventional open surgery, and the necessary equipment and instruments were used to perform the techniques. We used a 10-mm laparoscope, 10-mm or 5-mm Babcock forceps, 5-mm laparoscopic scissors, a set of gas insufflator/light source/monitor, and basic surgical instruments for conventional surgery.
Access to the umbilical vein and urachus using laparoscopic surgery with three access ports
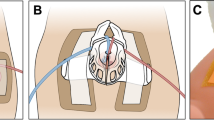
The anatomical specimens of the LG group were placed in the left lateral recumbency position and underwent laparoscopy using three laparoscopic access ports in the right flank, with two 10-mm cannulas in the first and second access ports and a 5-mm cannula in the third port for access to the umbilical vein and allantoic duct, or urachus. The access ports were established in the right flank near the paralumbar fossa, caudal to the ribs, using the modified hasson technique (Fig. 1A). Skin incisions of approximately 8 to 10 mm for 10-mm ports and 3 to 5 mm for 5-mm ports were made using a scalpel to insert the trocars transmurally into the abdominal cavity, maintaining the triangulation of the access doors (Fig. 1B).
The first 10-mm laparoscopic access port with an insufflation valve was inserted, through which a carbon dioxide (CO2)-induced pneumoperitoneum of 8 mmHg was established, and the abdominal cavity was inspected by viewing the image on the monitor. The inspected elements included the umbilical vein from the umbilical ring to its insertion in the liver, the umbilical arteries from the umbilical ring to the vicinity of the bladder, and the urachus from the umbilical ring to the bladder.
The second laparoscopic access port was established using a 10-mm trocar to insert the Babcock forceps, through which manipulation of the umbilical structures was performed, simulating the clipping of these components and maintaining an appropriate position to perform the resections in the insertion regions and vicinity of the umbilical ring.
The third 5-mm port was established to perform the umbilical vein and urachal resection, in the insertion regions and near the umbilical ring, through which the laparoscopic scissors were introduced and resection of these components was performed. Subsequently, the components were removed through the second access port using the Babcock forceps.
Resection of the umbilical vein using laparoscopic surgery with three access ports
For resection of the umbilical vein, the assistant operated the optics placed on the first port. The surgeon manipulated the umbilical vein, performed the clipping simulation, positioned the vein for resection, and resected it using laparoscopic scissors inserted in the third port. First, the surgeon placed the Babcock forceps in the second port and manipulated the umbilical vein for a better inspection of the regions to be resected, later removing the forceps. Subsequently, the Babcock forceps were reinserted to mimic a laparoscopic clipper used for hemostasis of large vessels, thereby simulating the application of four hemostatic clips in the umbilical vein: two in the vicinity of the umbilical ring and two in the vicinity of the liver, at the vein insertion site, and the Babcock forceps were again removed from the port. Finally, the Babcock forceps were reinserted to position and secure the umbilical vein. The surgeon placed the laparoscopic scissors through the third portal and resected the umbilical vein that was secured by the Babcock forceps at the “clipped” sites, and the vein was removed through the second access port using the Babcock forceps.
Resection of the urachus using laparoscopic surgery with three access ports
The procedures for urachal resection followed the same sequence as those performed for umbilical vein resection described in the previous paragraph; however, separation of the tissues surrounding the urachus and bladder was performed using laparoscopic scissors introduced in the third port, for better identification of the “clipping” sites and resection. Simulation of clipping and urachal resection were performed near the umbilical ring and anterior to the bladder, following the same procedure used for simulation of clipping and resection of the umbilical vein.
Closure of the abdominal cavity in laparoscopic surgery with three access ports
After resection of the urachus, the pneumoperitoneum was undone, the trocar cannulas and laparoscopic ports were removed, and the skin incisions were sutured with one stitch (U suture) using 0.6-mm polyamide thread.
Access to the umbilical vein and urachus using celiotomy (open surgery grup—OG).
OG procedures were performed according to Marchionatti et al.7 adapted, working with the anatomical examples in the dolsal recumbency position, making elliptical access at the umbilical base, accessing as structures that make up the umbilical cord. After access was established, an umbilical vein was inspected, connected with a Miller knot in the region adjacent to the liver, without marsupialization maneuver. The tissues between the urachus and the artery were separated for better bladder identification inspection. Two block ligatures were made in the region close to the bladder using the Miller knots. Subsequently, the entire region of the umbilical ring was removed and the access reversed. Myorrhaphy was performed with superimposed suture, reduction of the subcutaneous space in a continuous suture and demorraphy using U suture.
Statistical analyses
The Shapiro–Wilk test was used to confirm that surgical time data were distributed normally. Data on total surgical time and duration of each surgical step were grouped for the GV and GA groups. Student's t-test was used to compare normally distributed data on surgical time, and the Mann–Whitney test (Wilcoxon) was used for non-normally distributed data.
Descriptive statistics were processed using the R statistical program, version 3.0.2. The confidence interval was 0.95, and when p ≤ 0.05, the difference was considered significant and the null hypothesis was rejected.
Results
All fetuses of bovine calves in the final third of gestation had well defined umbilical structures, including the components of interest, i.e., the umbilical vein and the allantoic duct, or urachus. These components had a cylindrical shape, defined walls, and flaccid texture, and it was possible to distinguish the umbilical veins and arteries as separate units. The liver and bladder were also well formed and defined. The bladder was empty, and the allantoic duct was cranially inserted in the anterior apex.
In the LG, with the fetuses positioned in left lateral recumbency, it was possible to perform resection of the umbilical vein and urachus using laparoscopy with three access ports established in the right flank, in the paralumbar fossa region (Fig. 1A,B). In the OG group, the most appropriate position for performing the proposed procedures was dorsal recumbency with abducted legs (Fig. 1C).
The pneumoperitoneum established using an intra-abdominal pressure of 8 mmHg allowed satisfactory separation of the abdominal wall from the visceral structures, as well as excellent intra-abdominal visualization of the umbilical structures and associated/adjacent organs such as the liver and bladder.
Access to the abdominal cavity and target structures to perform the procedures was achieved through three laparoscopic ports in laparoscopy and through a paramedian and circumscribed incision in the abdominal wall (subcutaneous tissue, muscle, and peritoneum) in celiotomy (Figs. 1B and 2). In laparoscopy, the surgical wounds consisted of three openings of approximately 3 to 5 mm in length, and in celiotomy the openings in the abdominal cavity ranged from 5.5 to 18.5 cm, with an average of 9.7 cm (Fig. 2). Access to the abdominal cavity, down to the target structures, was secured in 5.52 (± 1.82) and 4.78 (± 0.74) min in the LG and OG groups, respectively (Table 1).
During access to the abdominal cavity using laparoscopy with three ports, the umbilical vein was the first component inspected because the laparoscope focused directly on the structure, thereby enabling its complete inspection (Fig. 3A). It was possible to simulate the clipping of the umbilical vein with Babcock forceps in the resection sites and extract it through the second access port using 10-mm Babcock forceps (Fig. 3A–C). Resection of the umbilical vein using celiotomy was achieved, and Miller’s knot was made to contain bleeding (Fig. 4B). The duration of umbilical vein resection was 2.27 (± 1.33) and 2.89 (± 0.87) min in the LG and OG groups, respectively (Table 1).
With regard to the urachus, it was possible to simulate clipping with the Babcock forceps and perform its resection using laparoscopy (Fig. 3E). Resection of the urachus using celiotomy was also achieved, and Miller’s knot in the duct was made in this case (Fig. 4C). The duration of urachal resection was 7.09 (± 1.27) and 3.13 (± 0.91) min in the LG and OG groups, respectively (Table 1).
In the LG group, closure of the abdominal cavity was performed by placing a stitch on the skin (U suture) that created a post-surgical wound of approximately 5 mm in length. In the OG group, peritoneum/muscle dieresis was performed with overlapping suture, subcutaneous tissue dieresis was performed with simple continuous suture, and dead space was reduced by anchoring the subcutaneous tissue to the musculature. Skin closure was performed with a U suture that created a post-surgical wound ranging from 10 to 20 cm, with an average of 13.6 cm (Fig. 5). The surgical time for abdominal cavity closure was 0.92 (± 0.09) min in the GV group and 28.64 (± 7.32) min in the OG group (Table 1).
The total surgical time in the LG and OG groups was 15.81 (± 3.26) and 39.44 (± 8.46) min, respectively (Table 1).
Discussion
The treatments indicated for umbilical vein and urachal diseases in newborn calves are based on clinical and/or surgical therapy, with conventional open surgery commonly performed in cases requiring surgical treatment. The aim of the present study was to assess the use of laparoscopy in umbilical vein and urachal interventions when surgical treatment is indicated. The surgical management of umbilical conditions usually has a good prognosis. The use of laparoscopy improves prognosis, with better postoperative results including less pain and better recovery for patients3,18.
In OG, a satisfactory procedure involving the umbilical structures was possible, with adequate inspection and palpation of the umbilical structures, which allowed the surgeon to examine and resect each component. However, a more comprehensive exploration of the abdominal cavity was achieved using laparoscopy, with good intervention in the umbilical structures and adjacent tissues/organs because the visual field projected on the monitor enlarged the structures and improved the visualization of smaller areas. Using laparoscopy, intervention in tissues present in small areas and that are difficult to access is possible. This is a minimally invasive procedure that, when associated with advanced multimedia resources, enables new approaches and procedures that are more precise and objective, thereby improving the outcomes and reducing complications11,14.
In the first step, there was no statistically significant difference in the time required to access the umbilical vein and urachus between the two groups. The duration of access in the LG was longer because the time to insufflate the abdominal cavity was included in this step. In both groups, caution as well as the establishment of standardized access ports allowed the procedures to be completed without complications, both morphological complications and macroscopic lesions of abdominal structures. In laparoscopy, a skin incision smaller than the diameter of the trocar allowed the latter to be introduced slowly and carefully, thereby preventing potential injuries to the abdominal organs and CO2 losses from the cannulas of the laparoscopic ports during pneumoperitoneum. The trocars were inserted directly without injuring the abdominal organs and structures adjacent to the umbilical components and allowed working with instruments sufficiently far from the umbilical structures. Standardizing abdominal access techniques with safer and reliable methods reduces the likelihood of perioperative complications14,19,20.
Although preventive measures were not adopted during CO2 insufflation in laparoscopy, it may be important to adopt them in live patients, especially in those with infected umbilical structures and with metabolic impairment, because pneumoperitoneum can induce hypothermia and respiratory and cardiovascular changes2,21,22.
The difference in the surgical times of umbilical vein resection (second step) between the LG and OG groups was not statistically significant. In laparoscopy, the time required for simulation of the clipping and umbilical vein resection was shorter than that for the execution of Miller’s knot followed by vein resection in conventional open surgery; however, the surgeon's skill may have been a factor that influenced the surgical time of this step. A surgeon's skill is directly related to specialized training that ensures the ability to perform procedures quickly and efficiently11,13. In laparoscopy, umbilical vein resection was performed with ease, and the positioning of laparoscopic ports, in particular, was very important to guarantee direct access to the structure, avoiding organs or tissues that could prevent or hinder the procedures and allowing resection to be performed safely and without complications2,15. Animals with omphalophlebitis would have swollen structures due to the condition; however, there are different sizes of clips as well as other options for electrosurgical vessel sealing23,24,25. Thus, there are several possibilities for in vivo procedures, requiring few adaptations of the model described. Another question to investigate is the exteriorization of the sectioned structure (segment of umbilical vein and portion of the urachus). The removal of intra-abdominal structures is common in laparoscopic procedures, requiring small extensions in the portal access or the use of laparoscopic specimen retrieval bags26,27.
The surgical time for urachal resection in laparoscopy was longer than that in conventional open surgery because access to the urachus in laparoscopy was not direct, similar to the access to the umbilical vein. The urachus lies in the ventral region of the abdomen, between the umbilical arteries, and is enveloped by tissues that make its identification and manipulation difficult (not detected during laparoscopic visualization). For satisfactory intervention in the urachus, it is important to perform tissue divulsion around the duct, a procedure that requires a skilled laparoscopist and may have influenced the surgical time of this stage, although not greatly and not affecting the final surgical time. In general, urachal resection was achieved in all the animals in laparoscopy, which was shown to be an efficient technique for urachal interventions, both from a therapeutic and a diagnostic perspective. Considerable advances have already been achieved in the use of laparoscopy in urachal conditions15,28.
In convencional open surgery, the umbilical artery is seccioned and disconected from the abdominal wall. The same procedure could be performed in the laparoscopy. However, the authors believe that the techinique connecting the urachus to the bladder could be the best option. This procedure avoids potential trauma to adjacent structures, minimizing the formation of intra-abdominal adhesions, besides considering that the umbilical artery atrophy with the development of the calf29,30.
In the final step, i.e., closure of the abdominal cavity, the surgical time in the GA group was longer than that in the GV group. This was expected because the opening of the abdominal wall in conventional open surgery was multiple times larger than that in laparoscopy, and additional time was required to perform abdominal tissue closure. In laparoscopy, a simple stitch ensured closure of the cavity, whereas in conventional open surgery, several stitches were required to perform peritoneum/muscle and subcutaneous dieresis and skin closure. Abdominal tissue closure in laparoscopy is satisfactorily performed with one or two simple stitches in each created wound and has lower rates of complications compared with abdominal tissue closure performed in conventional open surgeries15,19.
The total surgical time of laparoscopy was significantly shorter than that of conventional open surgery (exactly 15.81 ± 3.26 min), which shows that resection using endosurgery of the umbilical vein and urachus is faster than resection using conventional open surgery. The step of abdominal cavity closure in conventional open surgery significantly affected the total surgical time in the GA group because access wounds in the abdominal wall were significantly larger than those caused by laparoscopy. This increased the time of abdominal cavity closure and, consequently, the total surgical time of conventional open surgery. The total surgical time of laparoscopy in the present study was significantly shorter than that in other similar studies in which the laparoscopy technique was used in diagnostic and surgical interventions of umbilical structures with times ranging from 36 to 160 min2,15,31.
Abdominal wall injuries were less common in laparoscopy than in conventional open surgery; laparoscopy caused only three lesions of approximately 10 mm, as well as less tissue damage. This allows us to infer that laparoscopy causes less surgical trauma in living patients and provides better postoperative recovery of newborn calves. Because it is a minimally invasive technique, it is important to determine whether it is possible to perform it under regional anesthesia and sedation, a suitable alternative for treating calves with umbilical disorders associated with concomitant diseases and with reduced ability to adapt to general anesthesia15. Other studies have shown that laparoscopic techniques are less traumatic than conventional open techniques32,33,34,35.
The results of laparoscopy allowed the identification of additional benefits of its use in production animals because the technique enabled a large visual field for the diagnostic exploration of the abdominal cavity, thereby providing diagnostic advantages from a macroscopic and morphological perspective, including the accurate detection of macroscopic disorders in the umbilical structures, liver, bladder, and other adjacent structures, with results that can be correlated with ultrasound and laparatomy. Laparoscopy is a potentially viable diagnostic alternative that allows diagnosing multifocal abscesses in the liver, changes in umbilical arteries near their branching from the internal iliac artery, and focal thickenings and adhesions15,20,36. The use of laparoscopy in production animals is still incipient, but its use provides better results in semiological and clinical/surgical procedures in bovine veterinary medicine, with advances in sanitary/production methods and animal welfare18,37,38,39.
Conclusions
The laparoscopic technique proposed in our study allowed to perform the ressection of the umbilical vein and urachus. The effectiveness in the evaluation of the structures is highlighted, allowing an excellent diagnosis.
Even though this research was performed in an experimental model, the study supports the attempt to perform the technique in patients in vivo, based on its minimally invasive quality and the short surgical time in the proposed assessment.
More studies in the clinical routine are required to verify each operative step in the face of altered structures, however, the team allows few adaptations in live animals.
References
Hopker, A. Umbilical swellings in calves: A continuing challenge. Vet. Rec. 174, 219–220. https://doi.org/10.1136/vr.g1790 (2014).
Bouré, L., Foster, R. A., Palmer, M. & Hathway, A. Use of an endoscopic suturing device for laparoscopic resection of the apex of the bladder and umbilical structures in normal neonatal calves. Vet. Surg. 30, 319–326 (2001).
Williams, H. J., Gillespie, A. V., Oultram, J. W., Cripps, P. J. & Holman, A. N. Outcome of surgical treatment for umbilical swellings in bovine youngstock. Vet. Rec. 174(9), 221–221. https://doi.org/10.1136/vr.101736 (2014).
Rodrigues, C. A. et al. Correlação entre os métodos de concepção, ocorrência e formas de tratamento das onfalopatias em bovinos: Estudo retrospectivo. Pesqui Vet. Bras. 30(8), 618–622. https://doi.org/10.1590/S0100-736X2010000800002 (2010).
Reig Cordina, L., Were, S. R. & Brown, J. A. Short-term outcome and risk factors for post-operative complications following umbilical resection in 82 Foals (2004–2016). Equine Vet. J. Suppl. https://doi.org/10.1111/evj.13021 (2018).
Baird, A. N. Umbilical surgery in calves. Vet. Clin. N. Am. Food Anim. Pract. 24(3), 467–477. https://doi.org/10.1016/j.cvfa.2008.06.005 (2008).
Marchionatti, E. et al. Surgical management of omphalophlebitis and long term outcome in calves: 39 cases (2008–2013). Vet. Surg. 45, 194. https://doi.org/10.1111/vsu.12433 (2016).
Mulon, P. Y. & Desrochers, A. Surgical abdomen on the calf. Vet. Clin. N. Am. Food Anim. Pract. 21(1), 101–132. https://doi.org/10.1016/j.cvfa.2004.12.004 (2005).
Yanmaz, L. E., Okumus, Z. & Dogan, E. Laparoscopic surgery in veterinary medicine. Medwell J. Vet. Res. 1(1), 23–39 (2007).
Nichols, S. Umbilical surgery in calves. in: ProcMich Vet Conf. https://pdfs.semanticscholar.org/7a17/77e92de2ec1d10f423f0f080949d9a6948f5.pdf. (2014).
Buia, A., Stockhausen, F. & Hanisch, E. Laparoscopic surgery: A qualified systematic review. World J. Methodol. 5(4), 238–254. https://doi.org/10.5662/wjm.v5.i4.238 (2015).
Ferrufino, F. L. et al. Simulation in laparoscopic surgery. Circ. Esp. 93(1), 4–11. https://doi.org/10.1016/j.cireng.2014.02.022 (2015).
Saber, A., Bayumi, E. K., Sophia, L. & Hoek, L. S. V. D. Minimal access and minimally invasive surgery in veterinary practice. J. Surg. 5(3–1), 39–42. https://doi.org/10.11648/j.js.s.2017050301.18 (2017).
Babkine, M. & Desrochers, A. Laparoscopic surgery in adult cattle. Vet. Clin. N. Am. Food Anim. Pract. 21(1), 251–279. https://doi.org/10.1016/j.cvfa.2004.12.003 (2005).
Robert, M. et al. Laparoscopic evaluation of umbilical disorders in calves. Vet. Surg. 45(8), 1041–1048. https://doi.org/10.1111/vsu.12559 (2016).
Seino, C. H. et al. Avaliação ultrassonográfica de componentes umbilicais inflamados em bezerros da raça Holandesa com até 30 dias de vida. Pesqui Vet. Bras. 36(6), 492–502. https://doi.org/10.1590/S0100-736X2016000600006 (2016).
Sato, R., Yamada, K., Shinozuka, Y., Ochiai, H. & Onda, K. Gas-filled urachal abcess with a pinging sound in a heifer calf. Vet. Med. 64(8), 362–366. https://doi.org/10.17221/61/2019-VETMED (2019).
Patel, A. M., Parikh, P. V. & Patil, D. B. Laparoscopy in veterinary practice. Vet. Res. Int. 2(1), 01–07 (2014).
Bianchi, G. et al. Laparoscopic access overview: Is there a safest entry method?. Actas Urol. Esp. 40(6), 386–392 (2016).
Oztoprak, M. Y. & Karaca, I. Abdominal access techniques used in laparoscopic surgery. Int. J. Exp. Clin. Anat. 13(2), 129 (2019).
Rezende, M., Prado, O., Bandeira, C., Petri, A. & Montero, E. Body temperature evaluation during induced pneumoperitoneum with CO2: An experimental study in pigs. Surg. Endosc. 26(6), 1724–1729. https://doi.org/10.1007/s00464-011-2099-x (2012).
Radlinsky, M. G. Complications and conversion from endoscopic to open surgery veterinary. Vet. Clin. N. Am. Food Anim. Pract. 46(1), 137–145. https://doi.org/10.1016/j.cvsm.2015.07.004 (2016).
Nuss, K. Erkrankungen der inneren Nabelstrukturen beim Rind. Tierarzti Prax. 35(G), 149–156. https://doi.org/10.1055/s-0038-1624018 (2007).
Yip, S. K. et al. Routine vascular control using the Hem-o-lok clip in laparoscopic nephrectomy: Animal study and clinical application. J. Endourol. 18(1), 77–81. https://doi.org/10.1089/089277904322836730 (2004).
Barnes, R. F., Greenfield, C. L., Schaeffer, D. J., Landolfi, J. & Andrews, J. Comparison of biopsy samples obtained using standard endoscopic instruments and the harmonic scalpel during laparoscopic and laparoscopic assisted surgery in normal dogs. Vet. Surg. 35, 243–251. https://doi.org/10.1111/j.1532-950X.2006.00134.x (2006).
Stavroulis, A., Memtsa, M. & Yoong, W. Methods for specimen removal from the peritoneal cavity after laparoscopic excision. Obstet. Gynaecol. 15(1), 26–30. https://doi.org/10.1111/j.1744-4667.2012.00148.x (2013).
Baird, A. N. Surgery of the umbilicus and related structures. Vet. Clin. Food. Anim. 32, 673–685. https://doi.org/10.1016/j.cvfa.2016.05.008 (2016).
Marques, L. C., Marques, J. A., Marques, I. C. S. & Teixeira, M. C. A. Dilatação cística do úraco e uroperitônio em touros: Relato de cinco casos. Arq. Bras. Med. Vet. Zootec. 62(6), 1320–1324. https://doi.org/10.1590/S0102-09352010000600004 (2010).
Araújo, S. E. A., Caravatto, P. P. P., Chang, A. J. B. A., Campos, F. G. C. M. & Sousa, M. Impacto da vídeocirurgia na prevenção de aderências. Rev. Bras. Colo-proctol. https://doi.org/10.1590/S0101-98802006000200014 (2006).
Guerri, G., Vignoli, M., Palombi, C., Monaci, M. & Petrizzi, L. Ultrasonographic evaluation of umbilical structures in Holstein calves: A comparison between healthy calves and calves affected by umbilical disorders. J. Dairy Sci. 103(3), 2578–2590. https://doi.org/10.3168/jds.2019-16737 (2019).
Fisher, A. T. Jr. Laparoscopically assisted resection of umbilical structures in foals. J. Am. Vet. Med. Assoc. 214(12), 1813–1816 (1999).
Easley, J. T., Garofolo, S. Q., Ruehlman, D. & Hackett, E. S. A 3-portal laparoscopic ovariectomy technique in ewes. Small Ruminant. Res. 121(2–3), 336–339. https://doi.org/10.1016/j.smallrumres.2014.08.001 (2014).
Zhang, S., Hao, M. & Ma, Y. Comparasion of laparoscopic and traditional abomasal cannulation in sheep. J. Vet. 60, 113–117. https://doi.org/10.1515/jvetres-2016-0016 (2016).
Tripathi, S. D., Khandekar, G. S., Datir, A. A., Ambore, G. S. & Pawar, A. Comparative evaluation of laparoscopic and open vasectomy techniques in teaser bulls. Intas. Polivet. 18(2), 415 (2017).
Santos, G. M. A. et al. Minimally invasive video-assisted ruminostomy in sheep. Small Ruminant. Res. 167, 78–81. https://doi.org/10.1016/j.smallrumres.2018.07.023 (2018).
Milovancev, M. & Townsend, K. L. Current concepts in minimally invasive surgery of the abdomen. Vet. Clin. N. Am. Small Anim. Pract. 45(3), 507–522. https://doi.org/10.1016/j.cvsm.2015.01.00.4 (2015).
Corrêa, R. R. et al. Evaluation of ventral laparoscopic abomasopexy using surgical staples associated with suture material in dairy cattle. Acta Sci. Vet. 46, 1545. https://doi.org/10.22456/1679-9216.81834 (2018).
Gnus, M., Ratajczak, K. & Antosik, P. Application of a laparoscopic spieker of own design in reposition and fixation of the left displacement of the abomasum (LDA) in cattle. Med. Water. 74(2), 99–103. https://doi.org/10.21521/mw.6059 (2018).
Sofi, K. A., Singh, M., Kumar, P. & Sharma, A. Laparoscopic chromopertubation for the evaluation of tubal patency in dairy cattle. Indian J. Anim. Reprod. 39(1), 1 (2018).
Acknowledgements
We would like to thank the members of the VOR research team (UFPA) for their collaboration and contribution to this research work.
Author information
Authors and Affiliations
Contributions
F.D.O.M (Conceptualization, Investigation, Formal Analysis, Project administration, Validation, Writing—Review & Editing), H.J.G. (Investigation, Data Curation), S.S.S (Investigation, Data Curation), J.P.M.B. (Investigation, Data Curation), G.P.B.V. (Investigation, Data Curation), D.L.S. (Investigation, Data Curation), L.H.V.A. (Investigation, Data Curation), L.A.S. (Investigation, Data Curation), G.M.A.S. (Investigation, Data Curation), K.C.R. (Investigation, Writing—Original Draft Preparation), V.S.S. (Investigation, Data Curation), C.E.S.F. (Investigation, Data Curation), B.C.G. (Investigation, Data Curation), H.F.M. (Investigation, Data Curation), C.R.G.S. (Investigation, Data Curation), R.S.A. (Investigation, Data Curation), L.P.B.B. (Investigation, Writing—Original Draft Preparation), G.F.A. (Resources), R.S.M.L. (Investigation, Writing—Original Draft Preparation) and P.P.M.T. (Conceptualization, Writing—Review & Editing, Supervision, Project administration, Funding acquisition, Validation, Methodology). All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Oliveira Monteiro, F.D., Gurgel, H.J., de Sousa, S.S. et al. Intra-abdominal resection of the umbilical vein and urachus of bovine fetuses using laparoscopy and celiotomy: surgical time and feasibility (cadaveric study). Sci Rep 11, 5328 (2021). https://doi.org/10.1038/s41598-021-84621-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84621-y
This article is cited by
-
Laparoscopy assisted abomasal cannulation in cadavers of bovine fetuses
BMC Veterinary Research (2022)
-
Percutaneous ruminostomy guided by rumenoscopy: study in an experimental model in bovine fetus
BMC Veterinary Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.