Abstract
Obesity is an independent risk factor for atherosclerotic cardiovascular disease (ASCVD). However, ‘obesity paradox’ is observed in patients with coronary artery disease while defining obesity by body mass index (BMI). The purpose of this study is to identify a better anthropometric parameter to predict cardiovascular events in patients with ASCVD. The study was conducted using the Taiwanese Secondary Prevention for patients with AtheRosCLErotic disease (T-SPARCLE) Registry. A total of 6,920 adult patients with stable ASCVD, enrolled from January 2010 to November 2014, were included, with a mean age of 65.9 years, 73.9% males, and a mean BMI of 26.3 kg/m2 at baseline. These patients were followed up for a median of 2.5 years. The study endpoint was the composite major adverse cardiovascular event (MACE), defined as cardiovascular death, nonfatal myocardial infarction or stroke, or cardiac arrest with resuscitation. Multivariable Cox proportional hazards regression showed a significant positive association between waist-to-BMI ratio and MACE (adjusted hazard ratio 1.69 per cm‧m2/kg increase in waist-to-BMI ratio, 95% CI 1.12–2.49, p = 0.01) after adjusting for potential risk factors and confounders. Traditional anthropometric parameters, such as BMI, weight, waist and waist-hip ratio, or newer waist-based indices, such as body roundness index and a body shape index, did not show any significant linear associations (p = 0.09, 0.30, 0.89, 0.54, 0.79 and 0.06, respectively). In the restricted cubic spline regression analysis, the positive dose–response association between waist-to-BMI ratio and MACE persisted across all the range of waist-to-BMI ratio. The positive dose–response association was non-linear with a much steeper increase in the risk of MACE for waist-to-BMI ratio > 3.6 cm‧m2/kg. In conclusion, waist-to-BMI ratio may function as a positive predictor for the risk of MACE in established ASCVD patients.
Similar content being viewed by others
Introduction
Obesity is an independent risk factor for cardiovascular diseases, such as hypertension, coronary artery disease (CAD), stroke and heart failure1,2. The clinical and epidemiological data indicate prevalence of modifiable risk factors for atherosclerotic cardiovascular disease (ASCVD), including hypertension, diabetes mellitus, and dyslipidemia, is higher in overweight and obese individuals3,4,5. While BMI is widely accepted and applied to evaluate obesity, a limitation of its use is that it cannot distinguish between fat mass, fat-free mass and lean mass1 and differentiate the distribution of subcutaneous or visceral fat. Emerging evidence has shown a phenomenon, called ‘obesity paradox’, in patients with established ASCVD6,7,8, in which the BMI-mortality curve is U-shaped. That is, overweight and mild to moderately obese patients have a better prognosis than patients with normal BMI and severe obesity.
It has been well known that increased visceral adipose tissue is associated with vascular inflammation, and subsequent atherosclerosis9,10. Visceral or central obesity plays an important role in ASCVD patients. Waist indices, such as waist circumference (WC) and waist-hip ratio (WHR), have been the two most common measures for central obesity. Both measures correlate with visceral adipose tissue and are associated with increased incident cardiovascular events11,12, and seem to be better anthropometric parameters for the prediction of cardiovascular outcome than BMI. However, WC alone is theoretically unable to allow comparison between individuals with different body size and mass. Hip circumference is technically more difficult to assess, and this made WHR a less reliable measure than WC12. Recently, two new WC-based anthropometric indices, body roundness index (BRI) and a body shape index (ABSI), have been proposed. BRI was developed by Thomas et al.13, and is calculated as 364.2–365.5x(1-((0.5xWC/π)2/(0.5xheight)2))1/2. One study has shown that BRI could identify cardiovascular disease and risk factors, but was not superior compared to traditional anthropometric indices like BMI and WC14. In 2012, Krakauer and Krakauer developed ABSI base on the allometric power law analysis to normalize WC for weight and height (and thus to BMI). It is defined as WC/(BMI2/3xheight1/2) and was designed to be independent from BMI15. ABSI has been demonstrated to predict premature mortality and cardiovascular risk in some studies15,16,17. However, both indices are too complicated to calculate and inconvenient for daily practice.
Therefore, we proposed a new and simplified waist-based index, waist-to-BMI ratio. In this new index, WC represents the visceral adiposity, and BMI is used for normalization of body size and mass. This study hypothesized the waist-to-BMI ratio as a good positive measure for central obesity, and a good anthropometric tool in patients with ASCVD. To test this hypothesis, the waist-to-BMI ratio was evaluated and compared with traditional anthropometric measures and newer waist-based indices in predicting the cardiovascular outcome in patients with established ASCVD from the Taiwanese Secondary Prevention for patients with AtheRosCLErotic disease (T-SPARCLE) Registry.
Methods
Study population
The study was conducted using the T-SPARCLE Registry, a multi-center prospective observational registry which involves 14 medical centers in Taiwan18. Briefly, the registry recruits and follows up a large population of patients with established ASCVD receiving secondary prevention therapy. Adult patients aged > 18 years with stable ASCVD, including CAD, cerebrovascular disease and peripheral artery disease, were enrolled. CAD was defined as the presence of coronary stenosis > 50% by coronary angiography, having a history of myocardial infarction, or angina with a positive stress test. Cerebrovascular disease was defined as cerebral infarction, or transient ischemic attack with carotid artery stenosis > 70% by ultrasound. Peripheral artery disease was defined as peripheral atherosclerosis with ischemic symptoms and confirmed by ankle-brachial index, Doppler ultrasound, or angiography. Patients were excluded if having a severe heart failure (New York Heart Association functional class III-IV), hemodynamically significant valvular or congenital heart disease, life expectancy of less than 6 months, neurocognitive or psychiatric condition, or being treated with immunosuppressive agents. Patients with acute stroke, acute myocardial infarction, or coronary revascularization within the last 3 months or being scheduled to receive coronary bypass graft surgery were also excluded. The study was approved by the Joint Institutional Review Board, Taiwan, R.O.C. for each participating hospital, and informed consent were obtained from all patients. All methods were performed in accordance with the relevant guidelines and regulations.
Clinical and demographic data
After the enrollment, patients’ baseline characteristics, including anthropometric measures, vital signs, medical history and current medications, were recorded, and the lipid profiles, liver enzymes and creatine phosphokinase levels were evaluated. Patients were followed up at the 6th, and 12th month, and every year thereafter. At each follow-up, anthropometric measures, vital signs, medications, laboratory data, and major adverse cardiovascular event (MACE) were obtained. The baseline lipid profile, including total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and triglyceride (TG), were checked. The subjects’ fasting sugar, liver function and renal function were also measured at the same time.
Study outcomes
The end point of this study was the composite MACE, defined as cardiovascular death, nonfatal myocardial infarction or stroke, or cardiac arrest with resuscitation.
Statistical analysis
All continuous variables were expressed as mean ± standard deviation (SD) and dichotomous variables as percentage. Association between various anthropometric indices were examined using the Pearson correlation coefficients. Multivariable Cox proportional hazards regression models were used to estimate the hazard ratio (HR) and 95% confidence interval of categorical BMI for MACE with the normal weight group as the reference, adjusting for potential risk factors, such as age, sex, history of cigarette smoking, medical history of hypertension, diabetes mellitus, heart failure, CAD and stroke or transient ischemic attack, previous coronary intervention, statin use and its intensity, other medication (such as antiplatelet agent, angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, beta-blocker), level of non-HDL-C and estimated glomerular filtration rate . BMI was divided into categories according to the definition of WHO for Asian populations19: underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 23 kg/m2), overweight (23 kg/m2 ≤ BMI < 27.5 kg/m2), and obese (27.5 kg/m2 ≤ BMI). Dose–response association between risk of MACE and each continuous anthropometric measure, including weight, BMI, WC, WHR, BRI, ABSI and the waist-to-BMI ratio, was examined using the Cox proportional hazards regression model. We used restricted cubic spline regression to investigate the potential nonlinear relationship between each anthropometric measure and risk of MACE, and the likelihood ratio test was used to test for nonlinearity20. All statistical analyses were performed with the Statistical Analysis System (SAS) version 9.4 (SAS Institute, Cary, NC) and R version 3.5.2 (The R Foundation for Statistical Computing, 2018). A p value < 0.05 was considered significant.
Missing data imputation
Approximately 5% of the enrolled patients had missing data on weight, BMI, and TG, and 8–12% in LDL-C, HDL-C, non-HDL-C, or estimated glomerular filtration rate. The missing rate of WC, and therefore WHR and waist-to-BMI ratio, was around 20%. Multiple imputation (by PROC MI procedure in SAS) was used to handle all the missing data. Under the assumption of missing at random, multiple imputation was considered as the most effective way of treating missing data that may provide unbiased results21. In this study, 20 plausible values were generated and imputed for each unobserved data point, resulting in 20 complete data sets for pooled analysis. Cox proportional hazards model was then estimated for each complete data set, and then used PROC MIANALYZE procedure in SAS to combine results from the twenty Cox models.
Results
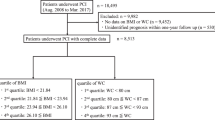
A total of 6,920 patients with ASCVD, enrolled from January 2010 to November 2014, were included in this analysis, with a mean age of 65.9 (SD 11.7) years, 73.9% males, and a mean BMI of 26.3 (SD 3.8) kg/m2 at baseline. Among them, 1.1% were underweight, 16.7% were normal weight, 48.5% were overweight, and 33.7% were obese. The mean weight, WC and WHR were 69.8 (SD 12.4) kg, 92.6 (10.1) cm and 0.93 (0.07) respectively. Of the 6,920 patients, 6,235 (90.1%) had CAD, most were acute coronary syndrome (77.2%), and 4862 (70.3%) received lipid-lowering therapy. Other baseline clinical and demographic characteristics were listed in Table 1. At follow-up, 58.2%, 60.6%, and 67.5% of the ASCVD patients achieved the optimal serum level of LDL-C < 100 mg/dL, non-HDL-C < 130 mg/dL, and TG < 150 mg/dL (the target of the guideline of national health insurance of Taiwan, during the study period), respectively. Correlation coefficients of each anthropometric index with BMI in this study cohort are shown in Table 2.
The 6,920 ASCVD patients were followed up for a median of 2.5 years, and 227 patients experienced MACE. The incident rate of MACE in our ASCVD patients was 1.25 (95% CI, 1.10–1.42) per 100 person-years. In the multivariable Cox regression analysis for categorical BMI, overweight ASCVD patients had the lowest hazard of MACE (adjusted HR 0.61, 95% CI 0.43–0.85, p = 0.004) (Table 3).
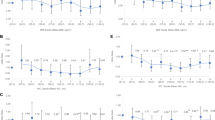
When analyzing continuous anthropometric parameters, multivariable Cox proportional hazards regression showed a significant positive association between waist-to-BMI ratio and the risk of MACE after adjusting for the covariates (adjusted HR 1.69 per cm·m2/kg increase in waist-to-BMI ratio, 95% CI 1.12–2.49, p = 0.01). Although non-significant, the hazard of MACE increased positively with ABSI with a trend (p = 0.06). Traditional anthropometric parameters, such as BMI, weight, WC and WHR, or the newer waist-based index, BRI, however, did not show significant associations with the risk of MACE (p = 0.09, 0.30, 0.89, 0.54, and 0.79, respectively) (Table 4). In the restricted cubic spline regression analysis, U-shaped associations were observed between traditional anthropometric parameters or BRI and the risk of MACE (Fig. 1). While dose–response association was also nonlinear between ABSI or waist-to-BMI ratio and the risk of MACE (the test for nonlinearity was statistically significant, p = 0.049 and < 0.001, respectively), positive associations persisted across all range of ABSI and waist-to-BMI ratio. By estimating the point of inflection from the figure of the restricted cubic spline regression analysis, a much steeper increase in the risk of MACE was found for waist-to-BMI ratio > 3.6 cm·m2/kg (Fig. 1).
Dose–response curves for various anthropometric parameters and risk of MACE. The red line and orange dashed line represent the point estimates and 95% confidence intervals from the non-linear analysis using the cubic spline regression. The blue line represents the point estimates from the linear analysis using the Cox proportional hazards regression.
Discussion
Obesity paradox was observed again in this study, and the results were consistent with previous studies when analyzing categorical BMI. Overweight ASCVD patients had the lowest risk of MACE during the follow-up period. Both the Cox proportional hazards model and cubic spline regression analysis showed a positive dose–response association between waist-to-BMI ratio and the risk of MACE, although the association was nonlinear. The shape of positive association between ABSI and the risk of MACE was similar with waist-to-BMI ratio by the cubic spline regression analysis although the positive association was non-significant by the Cox proportional hazards model. BMI and other traditional anthropometric measures, such as weight, WC and WHR, or the newer waist-based index, BRI, showed U-shaped associations with the cardiovascular outcome. We found that waist-to-BMI ratio is a good positive anthropometric measure to predict cardiovascular outcomes in patients with ASCVD, especially when the ratio is above 3.6 cm·m2/kg, which can be an easy, convenient, and useful tool for the clinical practice.
Although the World Health Organization defines obesity as abnormal or excessive fat accumulation that may impair health and suggest that BMI is only a rough guide to diagnose overweight and obesity, it is still widely used in epidemiological surveys and clinical practice due to its simplicity22,23. Association between BMI and first cardiovascular event and mortality in the general population have been confirmed by a large number of studies24,25,26,27. Therefore, BMI is widely used to predict cardiovascular outcomes in primary prevention at the population level. However, the ‘obesity paradox’ phenomenon of BMI6,7,8 in patients with established ASCVD could limit its application as an anthropometric tool for predicting cardiovascular outcomes. With the use of BMI in the present study, overweight ASCVD patients had the lowest risk for MACE, and the revealed U-shaped association is consistent with that of previous studies. The explanation of the obesity paradox may be the inherent limitations of clinical studies and the BMI as an obesity index28. The obesity paradox is observed by epidemiological studies, which could be biased by reverse causality, selection bias, inadequate follow-up periods, etc. BMI cannot distinguish between fat and lean mass, and it does not account for fat distribution, such as visceral fat or peripheral fat29,30,31. Individuals with similar BMI may have a different body fat percentage and fat distribution. Romeo-Corral et al. has demonstrated the poor diagnostic performance of BMI to discriminate between body fat and lean mass and to detect obesity in patients with CAD32. BMI is a crude measurement of total adiposity and does not seem to be a good clinical anthropometric tool for predicting CV outcome in ASCVD patients. A similar U-shaped association of BMI with prognosis has been also observed in patients with some other diseases, such as hypertension, heart failure, atrial fibrillation and chronic pulmonary disease although the reason might be not the same with that for ASCVD1.
Increased visceral adipose tissue is associated with the incidence of traditional cardiovascular risk factors, such as hypertension, hyperlipidemia, diabetes mellitus, and metabolic syndrome9,33,34. Besides, visceral adipose tissue plays an important role in the vascular inflammation. Image and autopsy studies demonstrated an association of abdominal visceral fat with coronary artery atherosclerosis35,36, the prevalent cardiovascular disease37,38, the severity of coronary artery disease39 and MACE40. Since regional adiposity is more important in ASCVD patients, a pertinent anthropometric measure is necessary for clinical use.
WC and WHR are thought to be better anthropometric measures than BMI to evaluate body fat distribution41 and can be surrogates for central or visceral fat adipose tissue42. Mounting evidence suggests that WC and WHR are associated with the risk of cardiovascular events and may be a better anthropometric measure to predict those events12,43,44. However, there is a lack of robust data about the relationship between central obesity and cardiovascular outcomes in patients with established ASCVD. One study demonstrated that central obesity was associated with adverse prognosis in patients with CAD, and highlighted the importance of central obesity in mortality risk assessment in this group of patients41. Our study showed that WC failed to predict cardiovascular outcome in patients with ASCVD. WC alone is theoretically unable to allow comparison between individuals with different body size and mass. Although the past studies showed that WC correlated well with BMI, a considerable variation in WC was noted for any given BMI value45,46. This means that individuals with the same BMI may have different WC, the different level of central obesity. One study has showed that patients with normal BMI but central obesity possess the worst cardiovascular outcome47. On the other hand, individuals with the same WC may have different BMI. Specifically, someone with lower BMI might have less lean mass but higher abdominal fat. Hence, individuals with the same WC might have different level of abdominal fat distribution. This implicated that WC should be interpreted in the context of BMI.
In this study, waist-to-BMI ratio was proposed to be a single and simple clinical anthropometric measure and adiposity index. Waist-to-BMI ratio incorporates the cardiovascular risk effect of regional adiposity WC with the application of BMI for normalization of body size and mass, which would be a better adiposity index for fat distribution or central obesity to predict cardiovascular outcomes in ASCVD patients. After normalizing WC by BMI, waist-to-BMI ratio was shown to have a significantly and consistently positive association with cardiovascular outcomes. This study also showed that the hazard of MACE increased positively with all range of ABSI, a recently proposed waist-based index, in the cubic spline regression analysis. With similar concept with waist-to-BMI ratio, ABSI was proposed to take body size and mass into account, and was designed to be independent of BMI base on the allometric power law analysis15. It has been shown to predict cardiovascular risk in some studies48,49,50. However, ABSI is too complicated to calculate for daily practice. The results of this study showed that waist-to-BMI ratio was not inferior, or even better, than ABSI in prediction of cardiovascular outcomes. This study demonstrated the waist-to-BMI ratio could be a good and simple anthropometric tool for predicting cardiovascular outcomes in established ASCVD patients, especially when the ratio is higher than 3.6 cm‧m2/kg.
There are some limitations in this study that should be considered. First, this study did not evaluate the effect of cardiorespiratory fitness. Increasing evidence showed cardiorespiratory fitness is a strong prognostic factor in CVD, which may interact with the prediction power of anthropometric measures30,51. Second, the follow-up time was not long. Third, the sample size of this study was moderate, and the study sample was limited to Asian population. Further study with a larger sample size, and extended to other ethnic groups are required to address this issue.
In conclusion, this is the first study to examine waist-to-BMI ratio as an anthropometric measure to predict CV outcome. We found waist-to-BMI ratio to be a better positive predictor for MACE in established ASCVD patients than traditional anthropometric parameters. Our finding provided an easy, convenient, and useful anthropometric tool in patients with ASCVD in daily clinical practice.
References
Elagizi, A. et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 61, 142–150 (2018).
Hubert, H. B., Feinleib, M., McNamara, P. M. & Castelli, W. P. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study. Circulation 67, 968–977 (1983).
Wilson, P. W., D’Agostino, R. B., Sullivan, L., Parise, H. & Kannel, W. B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 162, 1867–1872 (2002).
Haslam, D. W. & James, W. P. Obesity. Lancet 366, 1197–1209 (2005).
Lavie, C. J., Arena, R., Alpert, M. A., Milani, R. V. & Ventura, H. O. Management of cardiovascular diseases in patients with obesity. Nat. Rev. Cardiol. 15, 45–56 (2018).
Romero-Corral, A. et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet 368, 666–678 (2006).
Angerås, O. et al. Evidence for obesity paradox in patients with acute coronary syndromes: A report from the Swedish Coronary Angiography and Angioplasty Registry. Eur. Heart J. 34, 345–353 (2013).
Das, S. R. et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J. Am. Coll. Cardiol. 58, 2642–2650 (2011).
Alexopoulos, N., Katritsis, D. & Raggi, P. Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis 233, 104–112 (2014).
Luna-Luna, M. et al. Adipose tissue in metabolic syndrome: Onset and progression of atherosclerosis. Arch. Med. Res. 46, 392–407 (2015).
Kamel, E. G. et al. Measurement of abdominal fat by magnetic resonance imaging, dual-energy X-ray absorptiometry and anthropometry in non-obese men and women. Int. J. Obes. Relat. Metab. Disord. 23, 686–692 (1999).
de Koning, L., Merchant, A. T., Pogue, J. & Anand, S. S. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: Meta-regression analysis of prospective studies. Eur. Heart J. 28, 850–856 (2007).
Thomas, D. M. et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 21, 2264–2271 (2013).
Maessen, M. F. et al. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS ONE 9, e107212 (2014).
Krakauer, N. Y. & Krakauer, J. C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 7, e39504 (2012).
Bertoli, S. et al. Association of Body Shape Index (ABSI) with cardio-metabolic risk factors: A cross-sectional study of 6081 Caucasian adults. PLoS ONE 12, e0185013 (2017).
Christakoudi, S. et al. A Body Shape Index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: Results from a large European cohort. Sci. Rep. 10, 14541 (2020).
Yin, W. H., Wu, C. C. & Chen, J. W. Registry of lipid control and the use of lipid-lowering drugs for secondary prevention of cardiovascular events in patients with established atherosclerotic disease in Taiwan: Rationality and methods. Int. J. Gerontol. 6, 241–246 (2012).
Consultation WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163 (2004).
Therneau, T. M. & Grambsch, P. M. Modeling Survival Data: Extending the Cox Model (Springer, 2000).
Klebanoff, M. A. & Cole, S. R. Use of multiple imputation in the epidemiologic literature. Am. J. Epidemiol. 168, 355–357 (2008).
WHO. Obesity, fact sheet, obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Gadde, K. M., Martin, C. K., Berthoud, H. R. & Heymsfield, S. B. Obesity: Pathophysiology and management. J. Am. Coll. Cardiol. 71, 69–84 (2018).
Khan, S. S. et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 3, 280–287 (2018).
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 373, 1083–1096 (2009).
Ortega, F. B., Sui, X., Lavie, C. J. & Blair, S. N. Body mass index, the most widely used but also widely criticized index: Would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality?. Mayo Clin. Proc. 91, 443–455 (2016).
Twig, G. et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 374, 2430–2440 (2016).
Antonopoulos, A. S. & Tousoulis, D. The molecular mechanisms of obesity paradox. Cardiovasc. Res. 2017(113), 1074–1086 (2017).
Oliveros, E., Somers, V. K., Sochor, O., Goel, K. & Lopez-Jimenez, F. The concept of normal weight obesity. Prog. Cardiovasc. Dis. 56, 426–433 (2014).
Xia, J. Y., Lloyd-Jones, D. M. & Khan, S. S. Association of body mass index with mortality in cardiovascular disease: New insights into the obesity paradox from multiple perspectives. Trends Cardiovasc. Med. 29, 220–225 (2019).
Ma, W. Q. et al. Does body mass index truly affect mortality and cardiovascular outcomes in patients after coronary revascularization with percutaneous coronary intervention or coronary artery bypass graft? A systematic review and network meta-analysis. Obes. Rev. 19, 1236–1247 (2018).
Romero-Corral, A. et al. Diagnostic performance of body mass index to detect obesity in patients with coronary artery disease. Eur. Heart J. 28, 2087–2093 (2007).
Finelli, C., Sommella, L., Gioia, S., La Sala, N. & Tarantino, G. Should visceral fat be reduced to increase longevity?. Ageing Res. Rev. 12, 996–1004 (2013).
Mathieu, P., Poirier, P., Pibarot, P., Lemieux, I. & Després, J. P. Visceral obesity: The link among inflammation, hypertension, and cardiovascular disease. Hypertension 53, 577–584 (2009).
Nishizawa, A. et al. Morphometric measurements of systemic atherosclerosis and visceral fat: Evidence from an autopsy study. PLoS ONE 12, e0186630 (2017).
Ohashi, N. et al. Association between visceral adipose tissue area and coronary plaque morphology assessed by CT angiography. JACC Cardiovasc. Imaging 3, 908–917 (2010).
Mahabadi, A. A. et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur. Heart J. 30, 850–856 (2009).
Marques, M. D. et al. Relation between visceral fat and coronary artery disease evaluated by multidetector computed tomography. Atherosclerosis 209, 481–486 (2010).
Lee, Y. H. et al. Visceral adiposity and the severity of coronary artery disease in middle-aged subjects with normal waist circumference and its relation with lipocalin-2 and MCP-1. Atherosclerosis 213, 592–597 (2010).
Britton, K. A. et al. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J. Am. Coll. Cardiol. 62, 921–925 (2013).
Coutinho, T. et al. Central obesity and survival in subjects with coronary artery disease: A systematic review of the literature and collaborative analysis with individual subject data. J. Am. Coll. Cardiol. 57, 1877–1886 (2011).
Cameron, A. J., Magliano, D. J. & Söderberg, S. A systematic review of the impact of including both waist and hip circumference in risk models for cardiovascular diseases, diabetes and mortality. Obes. Rev. 14, 86–94 (2013).
Yusuf, S. et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet 366, 1640–1649 (2005).
Iliodromiti, S. et al. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: A cohort study of 296535 adults of white European descent. Eur. Heart J. 39, 1514–1520 (2018).
Despres, J. P. et al. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler. Thromb. Vasc. Biol. 28, 1039–1049 (2008).
Balkau, B. et al. International Day for the Evaluation of Abdominal Obesity (IDEA): A study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation 116, 1942–1951 (2007).
Coutinho, T. et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: Role of “normal weight central obesity”. J. Am. Coll. Cardiol. 61, 553–560 (2013).
Dhana, K. et al. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J. Epidemiol. Community Health. 70, 90–96 (2016).
Wang, F., Chen, Y., Chang, Y., Sun, G. & Sun, Y. New anthropometric indices or old ones: Which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc. Disord. 18, 14 (2018).
Krakauer, N. Y. & Krakauer, J. C. Untangling waist circumference and hip circumference from body mass index with a body shape index, hip index, and anthropometric risk indicator. Metab. Syndr. Relat. Disord. 16, 160–165 (2018).
De Schutter, A., Lavie, C. J. & Milani, R. V. The impact of obesity on risk factors and prevalence and prognosis of coronary heart disease-the obesity paradox. Prog. Cardiovasc. Dis. 56, 401–408 (2014).
Acknowledgements
The Taiwan Consortium of Lipid and Atherosclerosis is sponsored by Taiwan Society of Lipids & Atherosclerosis since 2009 and Taiwan Ministry of Science and Technology since 2012 (Project code: NRPB-TR11: 100-2325-B-002-075, 102-2325-B-002-097, 104-2325-B-002-036, 105-2325-B-002-035, 106-2321-B-002-029, 107-2321-B-002-035, 108-2321-B-002-043, and 109-2321-B-002 -039).
Author information
Authors and Affiliations
Consortia
Contributions
C.-F.H., F.-J.L., W.-H.Y. and C.-C.W. conceptualized and designed the study. T.-L.L., W.-K.T. and Y.-W.W. collected data. C.-F.H., F.-J.L. and C.-C.W. analyzed data. C.-F.H., F.-J.L., T.-L.L., K.-C.Y. and C.-C.W. interpreted data. C.-F.H. and F.-J.L. prepared the origional manuscript. K.-C.Y., W.-H.Y., H.-I.Y., J.-W.C. and C.-C.W revised the manuscript. All authors reviewed and approved the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsuan, CF., Lin, FJ., Lee, TL. et al. The waist-to-body mass index ratio as an anthropometric predictor for cardiovascular outcome in subjects with established atherosclerotic cardiovascular disease. Sci Rep 12, 804 (2022). https://doi.org/10.1038/s41598-021-04650-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04650-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.