Abstract
The aim of the present study was to describe the characteristics of infections with Staphylococcus aureus with reduced vancomycin susceptibility (SARVS) including vancomycin-intermediate S. aureus (VISA) in South Korea, using data from the national sentinel surveillance system during 2014–2016. A total of 66 patients infected or colonized with SA-RVS were reported using the sentinel surveillance system. Among them, VISA was confirmed in 14 isolates (21.2%) and no vancomycin-resistant S. aureus (VRSA) was detected. Most of patients had any kind of indwelling devices (81.8%, 54/66) and underwent surgical procedures in the previous 6 months (84.8%, 56/66). Patients who admitted to an intensive care unit (ICU) in the previous 3 months were 68.2% (45/66). Furthermore, patients who used vancomycin or had MRSA in the previous 1 month were 54.5% (36/66) and 59.1% (39/66), respectively. Upon review of the medical records, 54.5% (36/66) of patients were classified as having SA-RVSassociated infection and 30-day mortality was 19.4% (7/36). Our findings revealed that there was no VRSA in South Korea. SA-RVS including VISA existed particularly in patients who had indwelling devices, history of surgical procedure, and history of ICU admission.
Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR) is an emerging global crisis and a present threat to public health1. Multidrug-resistant organisms (MDROs) increase mortality rate, length of hospital stay, and health care costs2. Medical costs attributable to infections caused by MDROs are estimated to range from $18,588 to $29,069 per patient in the United States3. In addition, potential cost savings have been estimated at $1,948 per patient if MDRO infection rates were reduced by 3.5%4. MDRO-related illness sometimes leads to legal conflicts as well5.
Unfortunately, MDROs are widespread throughout South Korea. According to the Korean Antimicrobial Resistance Monitoring System (KARMS), the proportions of methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus faecium, and carbapenem-resistant Acinetobacter baumannii were 66%, 30%, and 85%, respectively, in 20156. Moreover, there have been substantial increases in the incidence of infections due to some MDROs, such as fluoroquinolone-resistant Enterobacteriaceae, vancomycin-resistant E. faecium, carbapenem-resistant A. baumannii, and carbapenem-resistant Enterobacteriaceae6,7. Consequently, some medical institutions in South Korea have experienced MDRO outbreaks8,9.
Among MDROs, vancomycin-intermediate S. aureus (VISA) is under special consideration by the Korea Centers for Disease Control and Prevention (KCDC). This is because infections caused by such pathogens leave clinicians with few therapeutic options for treatment.
The aim of the present study was to describe the characteristics of infections with S. aureus with reduced vancomycin susceptibility (SA-RVS) including VISA in South Korea, using data from Korea’s National Sentinel Surveillance System for VISA during 2014–2016.
Material and Methods
National Sentinel Surveillance for VISA
The KCDC started National Sentinel Surveillance for vancomycin-resistant S. aureus (VRSA) in 2000, and surveillance was expanded to SA-RVS in 2012.
All cases of S. aureus with vancomycin minimum inhibitory concentration (MIC) > 2 µg/mL using agar dilution, broth microdilution, or E-test, isolated at sentinel medical institutions, are mandatorily reported to the KCDC through the National Surveillance System for VISA. At the same time, sentinel medical institutions are required to send all isolates to the National Institute of Health (NIH) for further analysis. The sentinel medical institutions consist of all tertiary care hospitals (n = 44), all public hospitals (n = 39), and some hospitals with ≥200 beds (n = 17 in 2014 and 2015; n = 32 in 2016). These hospitals are distributed throughout the Korean Peninsula.
The KCDC performed in-depth surveillance for analysis of the current status of VISA dissemination from January 1, 2014 to December 31, 2016. On notification, the Epidemic Intelligence Service Officer of the KCDC (JW Park) reviewed the relevant medical records and gathered the following patient data: (i) demographic data, (ii) regional distribution, (ii) underlying comorbidities, (iii) risk factors for VISA acquisition, (iv) clinical features, (v) mortality, and (vi) admission history to other medical institutions. All cases were reviewed by staff of the KCDC department of Healthcare-Associated Infection Control and confirmed by the head of the department (H Lee). Both colonization and infection cases were included in this study.
Laboratory procedures
At the laboratory of the NIH, confirmatory testing was performed for vancomycin MIC using agar dilution, broth microdilution, and E-test for all S. aureus isolates sent to the NIH. All isolates had MIC > 2 µg/mL by at least one of those methods and additional antimicrobial susceptibility testing and molecular typing were performed for them.
Antimicrobial susceptibility tests were conducted for penicillin, oxacillin, gentamicin, ciprofloxacin, clindamycin, erythromycin, telithromycin, linezolid, teicoplanin, tetracycline, tigecycline, nitrofurantoin, rifampicin, and trimethoprim/sulfamethoxazole, using the Vitek 2 (Biomérieux, Marcy I’Etoile, France). S. aureus ATCC 29213 was used as the quality control strain. For daptomycin susceptibility, an E-test was performed.
For molecular typing, genomic DNA was extracted using a Wizard Genomic DNA Purification Kit (Promega, Madison, WI, USA). According to the manufacturer’s protocol for bacterial cells, we added lysostaphin at a final concentration of 30 µg/mL in lysis buffer and incubated it at 37 °C for 1 h. Multilocus sequence typing (MLST) was carried out using polymerase chain reaction (PCR) amplification and sequencing of seven housekeeping genes (arc, aroE, glpF, gmk, pta, tpi, and yqiL) using primer pairs as previously described10. The allelic profiles and sequence types (STs) were assigned using the MLST website (http://saureus.mlst.net/). Staphylococcal Cassette Chromosome mec (SCCmec) types were identified with the multiplex PCR method11. Strains COL, N315, NCCP13860, and MW2 were included as controls for SCCmec types I, II, III, and IV, respectively. Amplification of the spa repeat region was performed using primers spa-1113f (5′-AAGACGATCCTTCGGTGAGC-3′) and spa-1514r (5′-CAGCAGTAGTGCCGTTTGCTT-3′). PCR products were sequenced and the spa types were determined using the Ridom SpaServer12,13. Gene responsible for the vanA or vanB were determined using PCR and DNA sequencing method as described previously14,15.
Classification of S. aureus according to vancomycin MIC
Following the definition of the Clinical and Laboratory Standards Institute (CLSI), S. aureus isolates with vancomycin MIC 4–8 µg/mL were classified as VISA, and those with MIC ≥ 16 µg/mL were classified as VRSA16. The remaining reported S. aureus isolates, which showed vancomycin MIC between 2 and 4 µg/mL, were defined as non-VISA SA-RVS.
Classification of patients with VISA or VRSA according to origin of the pathogen
Patients with VISA or VRSA were categorized as cases of “cross-transmission,” “present on admission,” or “sporadic” according to exposure history for the potential origin of the pathogen. A description of each category follows.
Cross-transmission
Isolation of VISA or VRSA which was identical with isolates from another patient who was hospitalized in the same ward within the 2 weeks. Isolates were considered to be genetically identical if the patterns of antibiogram, SCCmec type, ST, and spa type were identical13.
Present on admission
Isolation of VISA or VRSA within 48 hours of admission from patients who were transferred from other medical institutions.
Sporadic
isolation of VISA or VRSA within 48 hours of admission, and the category Cross-transmission or Present on admission was not applicable.
Comparison between patients with VISA or VRSA and non-VISA SA-RVS
We performed a case-control study to identify differences in the characteristics of patients with VISA or VRSA compared to those with non-VISA SA-RVS, according to demographic data, regional distribution, underlying comorbidities, risk factors for VISA/VRSA acquisition, clinical categories, and mortality.
As for clinical categories, we defined patients who had compatible infectious signs and symptoms (such as bloodstream infection, urinary tract infection, pneumonia, surgical site infection, and so on) as having “SA-RVS-associated infection” based on the US Centers for Disease Control and Prevention/National Healthcare Safety Network (CDC/NHSN) surveillance definition of healthcare-associated infection17; the remaining cases were classified as “colonization with SA-RVS”.
Descriptive study of fatal cases of SA-RVS-associated infection
To identify clinical characteristics of deaths caused by SA-RVS-associated infection, we performed a descriptive study. Demographic data, diagnosis on admission, risk factors for VISA or VRSA acquisition, and treatment regimen for SA-RVS-associated infections were summarized.
Statistical analysis
All statistical analyses were conducted using SPSS version 21.0 for Windows (IBM Corp., Armonk, NY, USA). Categorical variables were analyzed using the chi-square test or Fisher’s extract test, as appropriate. Continuous variables were analyzed by independent t-tests. A two-tailed P-value of <0.05 was considered statistically significant.
Ethics statement
The study protocol was approved by the Institutional Review Boards of the KCDC (2018-02-04-PE-A). The requirement for written informed consent from patients was waived due to the retrospective nature of the study and its impracticability.
Results
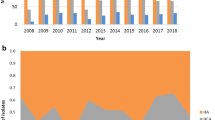
A total of 66 patients infected or colonized with SA-RVS were reported using the sentinel surveillance system (11 in 2014, 28 in 2015, and 27 in 2016) (Fig. 1). The largest proportion of patients with SA-RVS was identified in Seoul (54.5%, 36/66), followed by Busan (18.2%, 12/66), Chungcheongnam-do (15.1%, 10/66), Gyeonggi-do (10.6%, 7/66), and Jeollabuk-do (1.5%, 1/66). No cases were identified in the other provinces (Fig. 2). As a result of confirmatory testing for vancomycin MIC, VISA was confirmed in 14 isolates (21.2%); no VRSA was detected. The MIC of the remaining 52 SA-RVS isolates (78.8%) was <4 µg/mL and their MIC were 3 µg/mL by E-test. Among VISA cases, 12 (85.7%, 12/14) were classified as “sporadic” cases, two (14.3%, 2/14) were classified as “present on admission,” and there were no cases of “cross-transmission”.
Characteristics of patients carrying SA-RVS
Table 1 shows the characteristics of patients carrying SA-RVS. The mean age of patients was 62.3 ± 20.6 years and male sex predominated (72.7%, 48/66).
A 45.5% (30/66) of patients had diabetes and 22.7% (15/66) of them had any malignancy. Patients who had liver diseases and renal diseases were 12.1% (8/66) and 15.1% (10/66), respectively. Most of patients had any kind of indwelling devices (81.8%, 54/66) and underwent surgical procedures in the previous 6 months (84.8%, 56/66). Patients who admitted to an intensive care unit (ICU) in the previous 3 months were 68.2% (45/66). Furthermore, patients who used vancomycin or had MRSA in the previous 1 month were 54.5% (36/66) and 59.1% (39/66), respectively.
Upon review of the medical records, 54.5% (36/66) of patients were classified as having SA-RVS-associated infection. The most common infections were pneumonia (27.3%, 18/66), followed by bloodstream infection (12.1%, 8/66) and surgical site infection (12.1%, 8/66). Among patients with SA-RVS associated infection, 13 (36.1%, 13/36) patients died during admission and 30-day mortality was 19.4% (7/36).
When compared patients with VISA and patients with non-VISA SA-RVS, there was no significant difference in most parameters, except admission history to an ICU in the previous 3 months. It was significantly higher in patients with non-VISA SA-RVS than in patients with VISA (76.9% vs. 35.7%, P = 0.009).
As for clinical outcomes, there were no deaths among patients with VISA; however, 13 (43.3%, 13/30) patients with non-VISA SA-RVS died during admission; this difference was not statistically significant (P = 0.680).
Deaths attributed to SA-RVS-associated infection
We analyzed patients who died within 30 days of hospital admission owing to SA-RVS-associated infections (Table 2). As shown in the table, all deaths occurred among patients with non-VISA SA-RVS.
The median patient age was 70 years, and five (71.4%, 5/7) patients were male. Among them, three patients (patient numbers 3, 4, and 7) had malignancies. Most patients (85.7%, 6/7) died owing to pneumonia. Nearly all patients had a history of admission to a medical institution in the previous 3 months (100.0%, 7/7), use of an indwelling device (100.0%, 7/7), and admission to an ICU in the previous 3 months (85.7%, 6/7). Two patients (28.6%, 2/7) had undergone a surgical procedure in the previous 6 months. Linezolid was administered to three patients for treatment of SA-RVS infection.
Microbiological characteristics of VISA and non-VISA SA-RVS isolates
The vanA and vanB genes were not detected in any isolates. Regarding sample type, the largest proportion of SA-RVS was isolated from sputum (47.0%, 31/66), followed by nasopharyngeal swabs (16.7%, 11/66), and blood (10.6%, 7/66).
Table 3 shows the microbiological characteristics of VISA and non-VISA SA-RVS. The antimicrobial susceptibility of S. aureus isolates from patients with VISA to most antibiotics was similar to the susceptibility of isolates from patients with non-VISA SA-RVS. Both groups demonstrated high rates of susceptibility to linezolid, tigecycline, nitrofurantoin, and trimethoprim/sulfamethoxazole. VISA isolates were more susceptible than non-VISA SA-RVS isolates to penicillin (VISA: 14.3% vs. non-VISA SA-RVS: 0%, P = 0.042) and oxacillin (VISA: 14.3% vs. non-VISA SA-RVS: 0%, P = 0.042). On the other hand, the susceptibility rates of VISA isolates to teicoplanin (VISA: 69.2% vs. non-VISA SA-RVS: 94.2%, P = 0.025) and daptomycin (VISA: 85.7% vs. non-VISA SA-RVS: 100.0%, P = 0.042) were lower than those of non-VISA SA-RVS isolates.
All isolates were either SCCmec type II or IV; SCCmec type II was the predominant isolate in both groups (VISA: 92.9% vs. non-VISA SA-RVS: 90.4%, P = 1.000). Compared with SCCmec type IV isolates, SCCmec type II isolates had significantly lower rates of susceptibility to gentamicin (type II: 30%, 18/60; type IV: 83.3%, 5/6; P = 0.030), ciprofloxacin (type II: 0.0%, 0/60; type IV: 66.7%, 4/6; P < 0.001), clindamycin (type II: 3.3%, 2/60; type IV: 83.3%, 5/6; P < 0.001), tetracycline (type II: 6.7%, 4/60; type IV: 83.3%, 5/6; P < 0.001), and rifampicin (type II: 48.3%, 29/60; type IV: 100.0%, 6/6; P = 0.039) (Table 4).
As for MLST, most isolates were ST5, comprising 92.8% (13/14) and 90.4% (47/52) of isolates from patients with VISA and non-VISA SA-RVS, respectively. The remaining isolates were ST72 (VISA: 7.1%, 1/14; non-VISA SA-RVS: 7.7%, 4/52; P = 1.000) and ST632 (VISA: 0.0%, 0/14; non-VISA SA-RVS: 1.9%, 1/52; P = 1.000).
As for spa typing, 9 known spa types were detected, with t2460 being the most prevalent (VISA: 50.0%, 7/14; non-VISA SA-RVS: 59.6%, 31/52; P = 0.518).
Discussion
Herein, we report the characteristics of patients carrying SA-RVS including VISA in South Korea. Notably, no VRSA has been isolated in South Korea. The main mechanism for the occurrence of VRSA is via the presence of the vanA gene, which could be transferred from vancomycin-resistant enterococci to S. aureus via plasmids15,18. We found that no S. aureus isolates identified via the National Surveillance System for VISA had the vanA or vanB gene.
The presence of a thickened cell wall with an increased number of peptidoglycan layers is mostly applicable mechanism of reduced susceptibility to vancomycin among VISA19. The gene mutation that changes the pattern of the cell wall and/or reduces the expression of penicillin-binding proteins in S. aureus is triggered by long-term vancomycin usage20,21. In fact, the majority of VISA strains have emerged in patients with MRSA undergoing prolonged vancomycin therapy19,20.
Identified risk factors associated with VISA in previous studies include prolonged vancomycin use, previous MRSA colonization, hemodialysis dependence, and use of indwelling devices19,22. Furthermore, an observational study in the US revealed that prior vancomycin exposure within 30 days and residence in an ICU were predictors of SA-RVS presence in patients with S. aureus bacteremia23. Concordant with previous studies, we found that the majority of patients with SA-RVS used an indwelling device during hospitalization, had history of surgical procedures within 6 months, and admitted to ICU within 3 months.
There was no significant difference in most parameters including 30-day mortality between patients with VISA and patients with non-VISA SA-RVS. A previous study in the US suggested that patients with non-VISA SA-RVS infection had similar clinical characteristics compared to those with VISA infection22. Although elevated vancomycin MIC levels in patients with S. aureus infection may cause antibiotic therapy less effective, the association between vancomycin MIC and mortality is still controversial. Some previous meta-analyses have addressed association between vancomycin MIC and worse outcome24,25. On the contrary, no statistically significant difference in the mortality between patients with SA-RVS and those with non-SA-RVS were observed in the recent studies26,27. A prospective cohort study proposed that reduced vancomycin susceptibility might be linked to reduced disease severity in S. aureus infection27. Further studies are necessary to clarify this issue.
As for antimicrobial susceptibility, the SA-RVS strains appeared to have retained high susceptibility to linezolid, tigecycline, nitrofurantoin, and trimethoprim/sulfamethoxazole. Fortunately, these agents are available in South Korea and could be treatment options for SA-RVS-associated infections. When comparing VISA isolates with non-VISA SA-RVS isolates, the VISA strains were significantly less susceptible to teicoplanin. A previous report revealed that VISA is well correlated with lower response to teicoplanin because teicoplanin is a glycopeptide and has mechanisms similar to those of vancomycin28. Interestingly, two VISA isolates were resistant to daptomycin, which is not available in South Korea. Previous studies have revealed that increased vancomycin MIC in VISA isolates is associated with daptomycin resistance29,30. Sakoulas et al. suggested that exposure of S. aureus to vancomycin may affect daptomycin resistance31. In our study, two daptomycin-resistant VISA isolates had vancomycin MIC of 4 µg/mL. Another interesting finding was that two VISA isolates were susceptible to oxacillin whereas no non-VISA isolates were susceptible to this agent; both of these isolates carried SCCmec type II. Previous in vitro studies showed that decreased vancomycin susceptibility is associated with increased sensitivity to beta-lactams32. Based on such findings, the combination of vancomycin and beta-lactams has been suggested for treatment of SA-RVS infection33.
A recent retrospective study demonstrated that the molecular epidemiology of S. aureus is changing in Korea: a community-genotype MRSA strain, ST72, has emerged as a nosocomial pathogen34. Typically, SCCmec type II and ST5 strains are correlated with hospital-associated MRSA whereas SCCmec type IV and ST72 are correlated with community-acquired MRSA35,36. Despite the changing molecular epidemiology, SCCmec type II and ST5 remain predominant among SA-RVS strains in South Korea. Considering that most of our patients had risk factors for acquisition of SA-RVS, most SA-RVS strains might originate in health-care settings in South Korea.
Our study had some limitations. First, we could not acquire sufficient information about antibiotic usage. Basically, the in-depth surveillance in this study was mainly focused on the possibility of cross-transmission within medical institutions, and patients’ medical records from previous facilities were not fully available. Thus, we could not draw any conclusions about the relationship between the amount of vancomycin consumption and elevated vancomycin MIC in S. aureus. Second, most of the sentinel medical institutions are tertiary care hospitals and public hospitals. Therefore, the results of the present study are not generalizable to small- or medium-sized hospitals, including long-term care hospitals. Third, confirmatory testing for vancomycin MIC was performed by a variety of methods. E-test tends to yield higher numeric values for MIC than either broth or agar dilution and some isolates showed vancomycin MIC > 2 µg/mL only by E-test. It may have influenced data. Finally, the control group with fully vancomycin susceptible S. aureus was absent, which limits the ability to draw conclusions regarding clinical risk factors for VISA or SA-RVS acquisition.
Despite these limitations, the overall data of this study likely represent a reasonable approximation of the true values, and our findings may represent well the national status of SA-RVS in South Korea.
Conclusion
Our findings revealed that there was no VRSA in South Korea. However, SA-RVS including VISA existed particularly in patients who had indwelling devices, history of surgical procedure, and history of ICU admission. Because only few therapeutic options exist and showing high mortality rate for infections caused by such pathogens, proper preventive strategies for further spread are indispensable. Implementing strict infection-control strategies and antimicrobial stewardship practices in each hospital is required in South Korea.
References
Spellberg, B. et al. The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 46, 155–164 (2008).
Cosgrove, S. E. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis. 42, S82–S89 (2006).
Giske, C. G., Monnet, D. L., Cars, O. & Carmeli, Y. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother. 52, 813–821 (2008).
Roberts, R. R. et al. Hospital and societal costs of antimicrobial-resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin infect Dis. 49, 1175–1184 (2009).
Song, J.-H. & Joo, E.-J. The crisis of antimicrobial resistance: current status and future strategies. J Korean Med Assoc. 53, 999–1005 (2010).
Kim, D. et al. Increasing Resistance to Extended-Spectrum Cephalosporins, Fluoroquinolone, and Carbapenem in Gram-Negative Bacilli and the Emergence of Carbapenem Non-Susceptibility in Klebsiella pneumoniae: Analysis of Korean Antimicrobial Resistance Monitoring System (KARMS) Data From 2013 to 2015. Ann Lab Med. 37, 231–239, https://doi.org/10.3343/alm.2017.37.3.231 (2017).
Korea Centers for Disease Control and Prevention. 2015 annual report from Korean antimicrobial resistance monitoring system [cited 2018 February 14], http://cdc.go.kr/CDC/cms/cmsFileDownload.jsp?fid=76&cid=71295&fieldName=attachGrp&index=2 (2015).
Lee, J. Y. et al. Outbreak of Imipenemase-1-Producing Carbapenem-Resistant Klebsiella pneumoniae in an Intensive Care Unit. Korean J Crit Care Med. 32, 29–38 (2016).
Kim, M.-N., Hwang, S. H., Pyo, Y.-J., Mun, H.-M. & Pai, C. H. Clonal spread of Staphylococcus aureus heterogeneously resistant to vancomycin in a university hospital in Korea. J Clin Microbiol. 40, 1376–1380 (2002).
Enright, M. C., Day, N. P., Davies, C. E., Peacock, S. J. & Spratt, B. G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones ofStaphylococcus aureus. J Clin Microbiol. 38, 1008–1015 (2000).
Oliveira, D. C. & de Lencastre, H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 46, 2155–2161 (2002).
Harmsen, D. et al. Typing of methicillin-resistant Staphylococcus aureus in a university hospital setting by using novel software for spa repeat determination and database management. J Clin Microbiol. 41, 5442–5448 (2003).
Koreen, L. et al. spa typing method for discriminating among Staphylococcus aureus isolates: implications for use of a single marker to detect genetic micro-and macrovariation. J Clin Microbiol. 42, 792–799 (2004).
Sievert, D. M. et al. Vancomycin-resistant Staphylococcus aureus in the United States, 2002–2006. Clin Infect Dis. 46, 668–674 (2008).
Kos, V. N. et al. Comparative genomics of vancomycin-resistant Staphylococcus aureus strains and their positions within the clade most commonly associated with Methicillin-resistant S. aureus hospital-acquired infection in the United States. MBio 3, e00112–00112 (2012).
Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. 15th informational supplement. CLSI document M100-S15 [cited 2018 February 14], http://www.facm.ucl.ac.be/intranet/CLSI/CLSI-2017-M100-S27.pdf (2017).
Horan, T. C., Andrus, M. & Dudeck, M. A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J Inf Control 36, 309–332 (2008).
Chang, S. et al. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Eng J Med. 348, 1342–1347, https://doi.org/10.1056/NEJMoa025025 (2003).
Cosgrove, S. E., Carroll, K. C. & Perl, T. M. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infec Dis. 39, 539–545, https://doi.org/10.1086/422458 (2004).
Gardete, S. & Tomasz, A. Mechanisms of vancomycin resistance in Staphylococcus aureus. J Clin Invest. 124, 2836 (2014).
Walsh, T. R. & Howe, R. A. The prevalence and mechanisms of vancomycin resistance in Staphylococcus aureus. Ann Rev Microbiol. 56, 657–675 (2002).
Fridkin, S. K. et al. Epidemiological and microbiological characterization of infections caused by Staphylococcus aureus with reduced susceptibility to vancomycin, United States, 1997–2001. Clin Infect Dis. 36, 429–439 (2003).
Lodise, T. P. et al. Predictors of high vancomycin MIC values among patients with mehticillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother 62, 1138–1141 (2008).
Jacob, J. T. & DiazGranados, C. A. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistnat Staphylococcus aureus infections: a meta-analysis. Int J Infect Dis 17, e93–e100 (2013).
van Hal, S. J., Lodise, T. P. & Paterson, D. L. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-anaylsis. Clin Infect Dis 54, 755–771 (2012).
Kalil, A. C., Van Schooneveld, T. C., Fey, P. D. & Rupp, M. E. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. Jama 312, 1552–1564 (2014).
Kim, T. et al. Clinical and microbiological factors associated with early patient mortality from methicillin-resistant Staphylococcus aureus bacteremia. Korean J Intern Med 34, 184–194 (2019).
Hiramatsu, K. Vancomycin-resistant Staphylococcus aureus: a new model of antibiotic resistance. Lancet Infect Dis. 1, 147–155 (2001).
Kelley, P. G., Gao, W., Ward, P. B. & Howden, B. P. Daptomycin non-susceptibility in vancomycin-intermediate Staphylococcus aureus (VISA) and heterogeneous-VISA (hVISA): implications for therapy after vancomycin treatment failure. J Antimicrob Chemother. 66, 1057–1060 (2011).
Cui, L., Tominaga, E., Neoh, H.-M. & Hiramatsu, K. Correlation between reduced daptomycin susceptibility and vancomycin resistance in vancomycin-intermediate Staphylococcus aureus. Antimicrob Agents Chemother. 50, 1079–1082 (2006).
Sakoulas, G., Alder, J., Thauvin-Eliopoulos, C., Moellering, R. C. & Eliopoulos, G. M. Induction of daptomycin heterogeneous susceptibility in Staphylococcus aureus by exposure to vancomycin. Antimicrob Agents Chemother. 50, 1581–1585 (2006).
Sieradzki, K., Roberts, R. B., Haber, S. W. & Tomasz, A. The development of vancomycin resistance in a patient with methicillin-resistant Staphylococcus aureus infection. N Engl J Med. 340, 517–523 (1999).
Climo, M. W., Patron, R. L. & Archer, G. L. Combinations of vancomycin and β-lactams are synergistic against staphylococci with reduced susceptibilities to vancomycin. Antimicrob Agents Chemother. 43, 1747–1753 (1999).
Joo, E.-J. et al. Emergence of Community-Genotype Methicillin-Resistant Staphylococcus aureus in Korean Hospitals: Clinical Characteristics of Nosocomial Infections by Community-Genotype Strain. Infect Chemother. 49, 109–116 (2017).
Trindade, P. D. A. et al. Prevalence of SCCmec type IV in nosocomial bloodstream isolates of methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 43, 3435–3437 (2005).
Vandenesch, F. et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis. 9, 978 (2003).
Acknowledgements
The authors thank all medical staff in sentinel medical institutions for their cooperation in collecting data. This work was supported by the research fund of Hanyang University (HY-2018).
Author information
Authors and Affiliations
Contributions
P.J.W. and K.B. designed the study. P.J.W. and L.H. collected the data. P.J.W. and K.J.W. analyzed and interpreted the data. P.J.W. and K.B. wrote the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, J.W., Lee, H., Kim, J.W. et al. Characterization of Infections with Vancomycin-Intermediate Staphylococcus aureus (VISA) and Staphylococcus aureus with Reduced Vancomycin Susceptibility in South Korea. Sci Rep 9, 6236 (2019). https://doi.org/10.1038/s41598-019-42307-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42307-6
This article is cited by
-
Characterization of Brazilian green propolis as a photosensitizer for LED light-induced antimicrobial photodynamic therapy (aPDT) against methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-intermediate Staphylococcus aureus (VISA)
Photochemical & Photobiological Sciences (2023)
-
MWCNT-oxazolidinone conjugates with antibacterial activity
Journal of Nanoparticle Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.