Abstract
Since its discovery nearly a century ago, over 100,000 studies of growth hormone (GH) have investigated its structure, how it interacts with the GH receptor and its multiple actions. These include effects on growth, substrate metabolism, body composition, bone mineral density, the cardiovascular system and brain function, among many others. Recombinant human GH is approved for use to promote growth in children with GH deficiency (GHD), along with several additional clinical indications. Studies of humans and animals with altered levels of GH, from complete or partial GHD to GH excess, have revealed several covert or hidden actions of GH, such as effects on fibrosis, cardiovascular function and cancer. In this Review, we do not concentrate on the classic and controversial indications for GH therapy, nor do we cover all covert actions of GH. Instead, we stress the importance of the relationship between GH and fibrosis, and how fibrosis (or lack thereof) might be an emerging factor in both cardiovascular and cancer pathologies. We highlight clinical data from patients with acromegaly or GHD, alongside data from cellular and animal studies, to reveal novel phenotypes and molecular pathways responsible for these actions of GH in fibrosis, cardiovascular function and cancer.
Key points
-
Growth hormone (GH) is important for growth and tissue remodelling, extracellular matrix formation and fibrosis.
-
Patients with acromegaly, which is characterized by excessive circulating levels of GH, have increased cardiovascular mortality that is associated with hypertension and heart failure.
-
Patients with GH deficiency have an increased risk of cardiovascular morbidity and mortality that is associated with cardiovascular risk factors and premature atherosclerosis.
-
GH actions in cancer are particularly implicated in mechanisms of therapy resistance; for example, active drug efflux, the epithelial-to-mesenchymal transition, apoptosis inhibition and development of a tumour-supportive microenvironment.
-
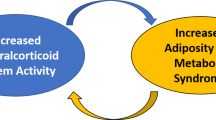
GH has a ‘Goldilocks effect’, where too little or too much can lead to poor clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Jorgensen, J. O. L., Johannsson, G. & Barkan, A. Should patients with adult GH deficiency receive GH replacement? Eur. J. Endocrinol. 186, D1–D15 (2021).
Ranke, M. B. & Wit, J. M. Growth hormone–past, present and future. Nat. Rev. Endocrinol. 14, 285–300 (2018).
Bernardo, A. & Houssay, M. D. The hypophysis and metabolism. N. Engl. J. Med. 214, 961–971 (1936).
Guevara-Aguirre, J. et al. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Sci. Transl Med. 3, 70ra13 (2011).
Aguiar-Oliveira, M. H. & Bartke, A. Growth hormone deficiency: health and longevity. Endocr. Rev. 40, 575–601 (2019).
Milman, S., Huffman, D. M. & Barzilai, N. The somatotropic axis in human aging: framework for the current state of knowledge and future research. Cell Metab. 23, 980–989 (2016).
Wynn, T. A. Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat. Rev. Immunol. 4, 583–594 (2004).
Householder, L. A. et al. Increased fibrosis: a novel means by which GH influences white adipose tissue function. Growth Horm. IGF Res. 39, 45–53 (2018).
Fruchtman, S. et al. Suppressor of cytokine signaling-2 modulates the fibrogenic actions of GH and IGF-I in intestinal mesenchymal cells. Am. J. Physiol. Gastrointest. Liver Physiol. 289, G342–G350 (2005).
Ong, L. K. et al. Growth hormone improves cognitive function after experimental stroke. Stroke 49, 1257–1266 (2018).
Yang, C. W., Striker, G. E., Chen, W. Y., Kopchick, J. J. & Striker, L. J. Differential expression of glomerular extracellular matrix and growth factor mRNA in rapid and slowly progressive glomerulosclerosis: studies in mice transgenic for native or mutated growth hormone. Lab. Invest. 76, 467–476 (1997).
Nielsen, R. H. et al. Chronic alterations in growth hormone/insulin-like growth factor-I signaling lead to changes in mouse tendon structure. Matrix Biol. 34, 96–104 (2014).
Doessing, S. et al. Growth hormone stimulates the collagen synthesis in human tendon and skeletal muscle without affecting myofibrillar protein synthesis. J. Physiol. 588, 341–351 (2010).
Gadelha, M. R., Kasuki, L., Lim, D. S. T. & Fleseriu, M. Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr. Rev. 40, 268–332 (2019).
Constantin, T. et al. Calcium and bone turnover markers in acromegaly: a prospective, controlled study. J. Clin. Endocrinol. Metab. 102, 2416–2424 (2017).
Arlien-Soborg, M. C. et al. Fibroblast activation protein is a GH target: a prospective study of patients with acromegaly before and after treatment. J. Clin. Endocrinol. Metab. 105, dgz033 (2020).
Nielsen, R. H. et al. GH receptor blocker administration and muscle-tendon collagen synthesis in humans. Growth Horm. IGF Res. 21, 140–145 (2011).
Holt, R. I. G. & Ho, K. K. Y. The use and abuse of growth hormone in sports. Endocr. Rev. 40, 1163–1185 (2019).
Coghlan, R. F. et al. A degradation fragment of type X collagen is a real-time marker for bone growth velocity. Sci. Transl Med. 9, eaan4669 (2017).
Antoniazzi, F. et al. GH in combination with bisphosphonate treatment in osteogenesis imperfecta. Eur. J. Endocrinol. 163, 479–487 (2010).
Randeva, H. S. et al. Growth hormone replacement decreases plasma levels of matrix metalloproteinases (2 and 9) and vascular endothelial growth factor in growth hormone-deficient individuals. Circulation 109, 2405–2410 (2004).
Karci, A. C., Canturk, Z., Tarkun, I. & Cetinarslan, B. Matrix metalloproteinase 2 (MMP-2) levels are increased in active acromegaly patients. Endocrine 57, 148–155 (2017).
Imanishi, R. et al. GH suppresses TGF-β-mediated fibrosis and retains cardiac diastolic function. Mol. Cell Endocrinol. 218, 137–146 (2004).
Zhang, Y. et al. TIMP3 modulates GHR abundance and GH sensitivity. Mol. Endocrinol. 30, 587–599 (2016).
Amor, C. et al. Senolytic CAR T cells reverse senescence-associated pathologies. Nature 583, 127–132 (2020).
Liu, R. M. & Liu, G. Cell senescence and fibrotic lung diseases. Exp. Gerontol. 132, 110836 (2020).
Baker, D. J. et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature 530, 184–189 (2016).
Stout, M. B. et al. Growth hormone action predicts age-related white adipose tissue dysfunction and senescent cell burden in mice. Aging 6, 575–586 (2014).
Matsumoto, R. et al. Accelerated telomere shortening in acromegaly; IGF-I induces telomere shortening and cellular senescence. PLoS ONE 10, e0140189 (2015).
Tran, D. et al. Insulin-like growth factor-1 regulates the SIRT1-p53 pathway in cellular senescence. Aging Cell 13, 669–678 (2014).
Chesnokova, V. & Melmed, S. GH and senescence: a new understanding of adult GH action. J. Endocr. Soc. 6, bvab177 (2022).
Thum, T. et al. Age-dependent impairment of endothelial progenitor cells is corrected by growth-hormone-mediated increase of insulin-like growth-factor-1. Circ. Res. 100, 434–443 (2007).
Luo, X. et al. Insulin-like growth factor-1 attenuates oxidative stress-induced hepatocyte premature senescence in liver fibrogenesis via regulating nuclear p53-progerin interaction. Cell Death Dis. 10, 451 (2019).
Henderson, N. C., Rieder, F. & Wynn, T. A. Fibrosis: from mechanisms to medicines. Nature 587, 555–566 (2020).
Freeth, J. S. et al. Human skin fibroblasts as a model of growth hormone (GH) action in GH receptor-positive Laron’s syndrome. Endocrinology 138, 55–61 (1997).
Guller, S., Sonenberg, M., Wu, K. Y., Szabo, P. & Corin, R. E. Growth hormone-dependent events in the adipose differentiation of 3T3-F442A fibroblasts: modulation of macromolecular synthesis. Endocrinology 125, 2360–2367 (1989).
Thorey, I. S. et al. Transgenic mice reveal novel activities of growth hormone in wound repair, angiogenesis, and myofibroblast differentiation. J. Biol. Chem. 279, 26674–26684 (2004).
Fan, M. H. et al. Fibroblast activation protein (FAP) accelerates collagen degradation and clearance from lungs in mice. J. Biol. Chem. 291, 8070–8089 (2016).
Wang, X. M. et al. Fibroblast activation protein and chronic liver disease. Front. Biosci. 13, 3168–3180 (2008).
Ben-Shlomo, A. & Melmed, S. Skin manifestations in acromegaly. Clin. Dermatol. 24, 256–259 (2006).
Lie, J. T. Pathology of the heart in acromegaly: anatomic findings in 27 autopsied patients. Am. Heart J. 100, 41–52 (1980).
dos Santos Silva, C. M. et al. Low frequency of cardiomyopathy using cardiac magnetic resonance imaging in an acromegaly contemporary cohort. J. Clin. Endocrinol. Metab. 100, 4447–4455 (2015).
Koutsou-Tassopoulou, A. et al. Hepatic steatosis in patients with acromegaly. Endocrinol. Diabetes Metab. 2, e00090 (2019).
Andrioli, M. et al. Thyroid nodules in acromegaly: the role of elastography. J. Ultrasound 13, 90–97 (2010).
Lai, N. B., Garg, D., Heaney, A. P., Bergsneider, M. & Leung, A. M. No benefit of dedicated thyroid nodule screening in patients with acromegaly. Endocr. Pract. 26, 16–21 (2020).
Jara, A. et al. Elevated systolic blood pressure in male GH transgenic mice is age dependent. Endocrinology 155, 975–986 (2014).
Munoz, M. C. et al. Downregulation of the ACE2/Ang-(1-7)/Mas axis in transgenic mice overexpressing GH. J. Endocrinol. 221, 215–227 (2014).
Jensen, E. A. et al. Growth hormone alters gross anatomy and morphology of the small and large intestines in age- and sex-dependent manners. Pituitary 25, 116–130 (2022).
List, E. O. et al. Adipocyte-specific GH receptor-null (AdGHRKO) mice have enhanced insulin sensitivity with reduced liver triglycerides. Endocrinology 160, 68–80 (2019).
List, E. O. et al. GH knockout mice have increased subcutaneous adipose tissue with decreased fibrosis and enhanced insulin sensitivity. Endocrinology 160, 1743–1756 (2019).
Yakar, S. & Isaksson, O. Regulation of skeletal growth and mineral acquisition by the GH/IGF-1 axis: lessons from mouse models. Growth Horm. IGF Res. 28, 26–42 (2016).
Dichtel, L. E. et al. The association between IGF-1 levels and the histologic severity of nonalcoholic fatty liver disease. Clin. Transl Gastroenterol. 8, e217 (2017).
Polyzos, S. A. et al. Targeted analysis of three hormonal systems identifies molecules associated with the presence and severity of NAFLD. J. Clin. Endocrinol. Metab. 105, e390–e400 (2020).
Nishizawa, H. et al. Nonalcoholic fatty liver disease in adult hypopituitary patients with GH deficiency and the impact of GH replacement therapy. Eur. J. Endocrinol. 167, 67–74 (2012).
Theiss, A. L. et al. Growth hormone reduces the severity of fibrosis associated with chronic intestinal inflammation. Gastroenterology 129, 204–219 (2005).
de Oliveira, G. V. et al. Growth hormone effects on hypertrophic scar formation: a randomized controlled trial of 62 burned children. Wound Repair Regen. 12, 404–411 (2004).
Breederveld, R. S. & Tuinebreijer, W. E. Recombinant human growth hormone for treating burns and donor sites. Cochrane Database Syst. Rev. 2014, CD008990 (2014).
Hu, Z. C. et al. Expression of insulin-like growth factor-1 receptor in keloid and hypertrophic scar. Clin. Exp. Dermatol. 39, 822–828 (2014).
Doi, T. et al. Progressive glomerulosclerosis develops in transgenic mice chronically expressing growth hormone and growth hormone releasing factor but not in those expressing insulinlike growth factor-1. Am. J. Pathol. 131, 398–403 (1988).
Bengtsson, B. A., Eden, S., Ernest, I., Oden, A. & Sjogren, B. Epidemiology and long-term survival in acromegaly. A study of 166 cases diagnosed between 1955 and 1984. Acta Med. Scand. 223, 327–335 (1988).
Dal, J. et al. Acromegaly incidence, prevalence, complications and long-term prognosis: a nationwide cohort study. Eur. J. Endocrinol. 175, 181–190 (2016).
Colao, A., Grasso, L. F. S., Di Somma, C. & Pivonello, R. Acromegaly and heart failure. Heart Fail. Clin. 15, 399–408 (2019).
Thuesen, L. et al. Increased myocardial contractility following growth hormone administration in normal man. An echocardiographic study. Dan. Med. Bull. 35, 193–196 (1988).
Thuesen, L. et al. Short and long-term cardiovascular effects of growth hormone therapy in growth hormone deficient adults. Clin. Endocrinol. 41, 615–620 (1994).
Napoli, R. et al. Acute effects of growth hormone on vascular function in human subjects. J. Clin. Endocrinol. Metab. 88, 2817–2820 (2003).
Kamenicky, P., Mazziotti, G., Lombes, M., Giustina, A. & Chanson, P. Growth hormone, insulin-like growth factor-1, and the kidney: pathophysiological and clinical implications. Endocr. Rev. 35, 234–281 (2014).
Moller, J., Jorgensen, J. O., Frandsen, E., Laursen, T. & Christiansen, J. S. Body fluids, circadian blood pressure and plasma renin during growth hormone administration: a placebo-controlled study with two growth hormone doses in healthy adults. Scand. J. Clin. Lab. Invest. 55, 663–669 (1995).
Thuesen, L., Christensen, S. E., Weeke, J., Orskov, H. & Henningsen, P. A hyperkinetic heart in uncomplicated active acromegaly. Explanation of hypertension in acromegalic patients? Acta Med. Scand. 223, 337–343 (1988).
Ikkos, D., Luft, R. & Sjogren, B. Body water and sodium in patients with acromegaly. J. Clin. Invest. 33, 989–994 (1954).
Moller, N. et al. Basal- and insulin-stimulated substrate metabolism in patients with active acromegaly before and after adenomectomy. J. Clin. Endocrinol. Metab. 74, 1012–1019 (1992).
Bolfi, F., Neves, A. F., Boguszewski, C. L. & Nunes-Nogueira, V. S. Mortality in acromegaly decreased in the last decade: a systematic review and meta-analysis. Eur. J. Endocrinol. 181, L5–L6 (2019).
Jaffrain-Rea, M. L. et al. Impact of successful transsphenoidal surgery on cardiovascular risk factors in acromegaly. Eur. J. Endocrinol. 148, 193–201 (2003).
Maison, P., Tropeano, A. I., Macquin-Mavier, I., Giustina, A. & Chanson, P. Impact of somatostatin analogs on the heart in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 92, 1743–1747 (2007).
Yuen, K. C. J. et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of growth hormone deficiency in adults and patients transitioning from pediatric to adult care. Endocr. Pract. 25, 1191–1232 (2019).
Hammarstrand, C. et al. Higher glucocorticoid replacement doses are associated with increased mortality in patients with pituitary adenoma. Eur. J. Endocrinol. 177, 251–256 (2017).
Klose, M. et al. Central hypothyroidism and its replacement have a significant influence on cardiovascular risk factors in adult hypopituitary patients. J. Clin. Endocrinol. Metab. 98, 3802–3810 (2013).
Tomlinson, J. W. et al. Association between premature mortality and hypopituitarism. West Midlands Prospective Hypopituitary Study Group. Lancet 357, 425–431 (2001).
Abe, S. Y. et al. Metabolic syndrome and its components in adult hypopituitary patients. Pituitary 23, 409–416 (2020).
Rosen, T. & Bengtsson, B. A. Premature mortality due to cardiovascular disease in hypopituitarism. Lancet 336, 285–288 (1990).
Isgaard, J., Wahlander, H., Adams, M. A. & Friberg, P. Increased expression of growth hormone receptor mRNA and insulin-like growth factor-I mRNA in volume-overloaded hearts. Hypertension 23, 884–888 (1994).
Ratku, B. et al. Effects of adult growth hormone deficiency and replacement therapy on the cardiometabolic risk profile. Pituitary 25, 211–228 (2022).
Johannsson, G. & Ragnarsson, O. Growth hormone deficiency in adults with hypopituitarism — What are the risks and can they be eliminated by therapy? J. Intern. Med. 290, 1180–1193 (2021).
Moller, N. & Jorgensen, J. O. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr. Rev. 30, 152–177 (2009).
Zierler, K. L. & Rabinowitz, D. Roles of insulin and growth hormone, based on studies of forearm metabolism in man. Medicine 42, 385–402 (1963).
Press, M., Notarfrancesco, A. & Genel, M. Risk of hypoglycaemia with alternate-day growth hormone injections. Lancet 1, 1002–1004 (1987).
Johansson, J. O., Fowelin, J., Landin, K., Lager, I. & Bengtsson, B. A. Growth hormone-deficient adults are insulin-resistant. Metabolism 44, 1126–1129 (1995).
Hew, F. L. et al. Insulin resistance in growth hormone-deficient adults: defects in glucose utilization and glycogen synthase activity. J. Clin. Endocrinol. Metab. 81, 555–564 (1996).
Berryman, D. E., Glad, C. A., List, E. O. & Johannsson, G. The GH/IGF-1 axis in obesity: pathophysiology and therapeutic considerations. Nat. Rev. Endocrinol. 9, 346–356 (2013).
Boger, R. H. et al. Nitric oxide may mediate the hemodynamic effects of recombinant growth hormone in patients with acquired growth hormone deficiency. A double-blind, placebo-controlled study. J. Clin. Invest. 98, 2706–2713 (1996).
Sverrisdottir, Y. B., Elam, M., Herlitz, H., Bengtsson, B. A. & Johannsson, G. Intense sympathetic nerve activity in adults with hypopituitarism and untreated growth hormone deficiency. J. Clin. Endocrinol. Metab. 83, 1881–1885 (1998).
Moller, J., Frandsen, E., Fisker, S., Jorgensen, J. O. & Christiansen, J. S. Decreased plasma and extracellular volume in growth hormone deficient adults and the acute and prolonged effects of GH administration: a controlled experimental study. Clin. Endocrinol. 44, 533–539 (1996).
Maison, P. et al. Impact of growth hormone (GH) treatment on cardiovascular risk factors in GH-deficient adults: a metaanalysis of blinded, randomized, placebo-controlled trials. J. Clin. Endocrinol. Metab. 89, 2192–2199 (2004).
Sverrisdottir, Y. B. et al. The effect of growth hormone (GH) replacement therapy on sympathetic nerve hyperactivity in hypopituitary adults: a double-blind, placebo-controlled, crossover, short-term trial followed by long-term open GH replacement in hypopituitary adults. J. Hypertens. 21, 1905–1914 (2003).
Evans, L. M. et al. The effect of GH replacement therapy on endothelial function and oxidative stress in adult growth hormone deficiency. Eur. J. Endocrinol. 142, 254–262 (2000).
Aguiar-Oliveira, M. H. & Salvatori, R. Disruption of the GHRH receptor and its impact on children and adults: the Itabaianinha syndrome. Rev. Endocr. Metab. Disord. 22, 81–89 (2021).
Johannsson, G., Sverrisdottir, Y. B., Ellegard, L., Lundberg, P. A. & Herlitz, H. GH increases extracellular volume by stimulating sodium reabsorption in the distal nephron and preventing pressure natriuresis. J. Clin. Endocrinol. Metab. 87, 1743–1749 (2002).
Kamenicky, P. et al. Body fluid expansion in acromegaly is related to enhanced epithelial sodium channel (ENaC) activity. J. Clin. Endocrinol. Metab. 96, 2127–2135 (2011).
Moller, J. et al. Blockade of the renin-angiotensin-aldosterone system prevents growth hormone-induced fluid retention in humans. Am. J. Physiol. 272, E803–E808 (1997).
Yokota, N., Bruneau, B. G., Kuroski de Bold, M. L. & de Bold, A. J. Atrial natriuretic factor significantly contributes to the mineralocorticoid escape phenomenon. Evidence for a guanylate cyclase-mediated pathway. J. Clin. Invest. 94, 1938–1946 (1994).
Moller, J., Jorgensen, J. O., Marqversen, J., Frandsen, E. & Christiansen, J. S. Insulin-like growth factor I administration induces fluid and sodium retention in healthy adults: possible involvement of renin and atrial natriuretic factor. Clin. Endocrinol. 52, 181–186 (2000).
Widdowson, W. M. & Gibney, J. The effect of growth hormone replacement on exercise capacity in patients with GH deficiency: a metaanalysis. J. Clin. Endocrinol. Metab. 93, 4413–4417 (2008).
Jorgensen, J. O. et al. Beneficial effects of growth hormone treatment in GH-deficient adults. Lancet 1, 1221–1225 (1989).
Johannsson, G., Grimby, G., Sunnerhagen, K. S. & Bengtsson, B. A. Two years of growth hormone (GH) treatment increase isometric and isokinetic muscle strength in GH-deficient adults. J. Clin. Endocrinol. Metab. 82, 2877–2884 (1997).
Amato, G. et al. Body composition, bone metabolism, and heart structure and function in growth hormone (GH)-deficient adults before and after GH replacement therapy at low doses. J. Clin. Endocrinol. Metab. 77, 1671–1676 (1993).
Hansson, G. K. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 352, 1685–1695 (2005).
Rudling, M. et al. Importance of growth hormone for the induction of hepatic low density lipoprotein receptors. Proc. Natl Acad. Sci. USA 89, 6983–6987 (1992).
Sharma, V. M. et al. Growth hormone acts along the PPARγ-FSP27 axis to stimulate lipolysis in human adipocytes. Am. J. Physiol. Endocrinol. Metab. 316, E34–E42 (2019).
Elam, M. B., Wilcox, H. G., Solomon, S. S. & Heimberg, M. In vivo growth hormone treatment stimulates secretion of very low density lipoproteins by the perfused rat liver. Endocrinology 131, 2717–2722 (1992).
Beentjes, J. A., van Tol, A., Sluiter, W. J. & Dullaart, R. P. Effect of growth hormone replacement therapy on plasma lecithin:cholesterol acyltransferase and lipid transfer protein activities in growth hormone-deficient adults. J. Lipid Res. 41, 925–932 (2000).
Rosén, T., Bosaeus, I., Tölli, J., Lindstedt, G. & Bengtsson, B.-Å. Increased body fat mass and decreased extracellular fluid volume in adults with growth hormone deficiency. Clin. Endocrinol. 38, 63–71 (1993).
Cuneo, R. C., Salomon, F., Wiles, C. M., Hesp, R. & Sönksen, P. H. Growth hormone treatment in growth hormone-deficient adults. II. Effects on exercise performance. J. Appl. Physiol. 70, 695–700 (1991).
Olivecrona, H., Ericsson, S., Berglund, L. & Angelin, B. Increased concentrations of serum lipoprotein (a) in response to growth hormone treatment. BMJ 306, 1726–1727 (1993).
Ridker, P. M., Hennekens, C. H., Buring, J. E. & Rifai, N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Engl. J. Med. 342, 836–843 (2000).
Leonsson, M. et al. Increased Interleukin-6 levels in pituitary-deficient patients are independently related to their carotid intima-media thickness. Clin. Endocrinol. 59, 242–250 (2003).
Sesmilo, G. et al. Effects of growth hormone administration on inflammatory and other cardiovascular risk markers in men with growth hormone deficiency. A randomized, controlled clinical trial. Ann. Intern. Med. 133, 111–122 (2000).
Franco, C. et al. Growth hormone treatment reduces abdominal visceral fat in postmenopausal women with abdominal obesity: a 12-month placebo-controlled trial. J. Clin. Endocrinol. Metab. 90, 1466–1474 (2005).
Pappachan, J. M., Raskauskiene, D., Kutty, V. R. & Clayton, R. N. Excess mortality associated with hypopituitarism in adults: a meta-analysis of observational studies. J. Clin. Endocrinol. Metab. 100, 1405–1411 (2015).
Drake, C. J. Embryonic and adult vasculogenesis. Birth Defects Res. C. Embryo Today 69, 73–82 (2003).
Bouloumie, A., Schini-Kerth, V. B. & Busse, R. Vascular endothelial growth factor up-regulates nitric oxide synthase expression in endothelial cells. Cardiovasc. Res. 41, 773–780 (1999).
Brunet-Dunand, S. E. et al. Autocrine human growth hormone promotes tumor angiogenesis in mammary carcinoma. Endocrinology 150, 1341–1352 (2009).
Walsh, M. F. et al. Insulin-like growth factor I diminishes in vivo and in vitro vascular contractility: role of vascular nitric oxide. Endocrinology 137, 1798–1803 (1996).
Setola, E. et al. Effects of growth hormone treatment on arginine to asymmetric dimethylarginine ratio and endothelial function in patients with growth hormone deficiency. Metabolism 57, 1685–1690 (2008).
Lilien, M. R., Schroder, C. H., Levtchenko, E. N. & Koomans, H. A. Growth hormone therapy influences endothelial function in children with renal failure. Pediatr. Nephrol. 19, 785–789 (2004).
Lanes, R. et al. Endothelial function, carotid artery intima-media thickness, epicardial adipose tissue, and left ventricular mass and function in growth hormone-deficient adolescents: apparent effects of growth hormone treatment on these parameters. J. Clin. Endocrinol. Metab. 90, 3978–3982 (2005).
Ishikawa, M. et al. Role of growth hormone signaling pathways in the development of atherosclerosis. Growth Horm. IGF Res. 53–54, 101334 (2020).
Maffei, P., Dassie, F., Wennberg, A., Parolin, M. & Vettor, R. The endothelium in acromegaly. Front. Endocrinol. 10, 437 (2019).
Messias de Lima, C. F., Dos Santos Reis, M. D., da Silva Ramos, F. W., Ayres-Martins, S. & Smaniotto, S. Growth hormone modulates in vitro endothelial cell migration and formation of capillary-like structures. Cell Biol. Int. 41, 577–584 (2017).
Rymaszewski, Z., Cohen, R. M. & Chomczynski, P. Human growth hormone stimulates proliferation of human retinal microvascular endothelial cells in vitro. Proc. Natl Acad. Sci. USA 88, 617–621 (1991).
Speakman, J. S. et al. Pituitary ablation for diabetic retinopathy. Can. Med. Assoc. J. 94, 627–635 (1966).
Smith, L. E. et al. Essential role of growth hormone in ischemia-induced retinal neovascularization. Science 276, 1706–1709 (1997).
Steenfos, H. H. & Jansson, J. O. Growth hormone stimulates granulation tissue formation and insulin-like growth factor-I gene expression in wound chambers in the rat. J. Endocrinol. 132, 293–298 (1992).
Isgaard, J., Arcopinto, M., Karason, K. & Cittadini, A. GH and the cardiovascular system: an update on a topic at heart. Endocrine 48, 25–35 (2015).
Santini, M. P. et al. Enhancing repair of the mammalian heart. Circ. Res. 100, 1732–1740 (2007).
Jara, A. et al. Cardiac-specific disruption of GH receptor alters glucose homeostasis while maintaining normal cardiac performance in adult male mice. Endocrinology 157, 1929–1941 (2016).
Kim, J. et al. Insulin-like growth factor I receptor signaling is required for exercise-induced cardiac hypertrophy. Mol. Endocrinol. 22, 2531–2543 (2008).
Imrie, H. et al. Novel role of the IGF-1 receptor in endothelial function and repair: studies in endothelium-targeted IGF-1 receptor transgenic mice. Diabetes 61, 2359–2368 (2012).
Abbas, A. et al. The insulin-like growth factor-1 receptor is a negative regulator of nitric oxide bioavailability and insulin sensitivity in the endothelium. Diabetes 60, 2169–2178 (2011).
Liang, M. et al. Protective role of insulin-like growth factor-1 receptor in endothelial cells against unilateral ureteral obstruction-induced renal fibrosis. Am. J. Pathol. 185, 1234–1250 (2015).
Higashi, Y. et al. Insulin-like growth factor-1 receptor deficiency in macrophages accelerates atherosclerosis and induces an unstable plaque phenotype in apolipoprotein E-deficient mice. Circulation 133, 2263–2278 (2016).
Spadaro, O. et al. Growth hormone receptor deficiency protects against age-related NLRP3 inflammasome activation and immune senescence. Cell Rep. 14, 1571–1580 (2016).
Nehra, S., Gumina, R. J. & Bansal, S. S. Immune cell dilemma in ischemic cardiomyopathy: to heal or not to heal. Curr. Opin. Physiol. 19, 39–46 (2021).
Moon, H. D., Simpson, M. E., Li, C. H. & Evans, H. M. Neoplasms in rats treated with pituitary growth hormone; pulmonary and lymphatic tissues. Cancer Res. 10, 297–308 (1950).
Chesnokova, V. et al. Local non-pituitary growth hormone is induced with aging and facilitates epithelial damage. Cell Rep. 37, 110068 (2021).
Harvey, S., Aramburo, C. & Sanders, E. J. Extrapituitary production of anterior pituitary hormones: an overview. Endocrine 41, 19–30 (2012).
Basu, R. & Kopchick, J. J. The effects of growth hormone on therapy resistance in cancer. Cancer Drug Resist. 2, 827–846 (2019).
Waters, M. J. & Conway-Campbell, B. L. The oncogenic potential of autocrine human growth hormone in breast cancer. Proc. Natl Acad. Sci. USA 101, 14992–14993 (2004).
Chesnokova, V. & Melmed, S. Growth hormone in the tumor microenvironment. Arch. Endocrinol. Metab. 63, 568–575 (2019).
Lincoln, D. T., Singal, P. K. & Al-Banaw, A. Growth hormone in vascular pathology: neovascularization and expression of receptors is associated with cellular proliferation. Anticancer Res. 27, 4201–4218 (2007).
Dos Santos Reis, M. D., Dos Santos, Y. M. O., de Menezes, C. A., Borbely, K. S. C. & Smaniotto, S. Resident murine macrophage migration and phagocytosis are modulated by growth hormone. Cell Biol. Int. 42, 615–623 (2018).
Kopchick, J. J., Berryman, D. E., Puri, V., Lee, K. Y. & Jorgensen, J. O. L. The effects of growth hormone on adipose tissue: old observations, new mechanisms. Nat. Rev. Endocrinol. 16, 135–146 (2020).
Lee, S. W., Kim, S. H., Kim, J. Y. & Lee, Y. The effect of growth hormone on fibroblast proliferation and keratinocyte migration. J. Plast. Reconstr. Aesthet. Surg. 63, e364–e369 (2010).
Hua, H., Kong, Q., Yin, J., Zhang, J. & Jiang, Y. Insulin-like growth factor receptor signaling in tumorigenesis and drug resistance: a challenge for cancer therapy. J. Hematol. Oncol. 13, 64 (2020).
Pollak, M. Insulin and insulin-like growth factor signalling in neoplasia. Nat. Rev. Cancer 8, 915–928 (2008).
Basu, R. et al. Growth hormone upregulates melanocyte-inducing transcription factor expression and activity via JAK2-STAT5 and SRC signaling in GH receptor-positive human melanoma. Cancers 11, 1352 (2019).
Chesnokova, V. et al. Growth hormone is a cellular senescence target in pituitary and nonpituitary cells. Proc. Natl Acad. Sci. USA 110, E3331–E3339 (2013).
Ben-Shlomo, A. et al. DNA damage and growth hormone hypersecretion in pituitary somatotroph adenomas. J. Clin. Invest. 130, 5738–5755 (2020).
Chesnokova, V. et al. Excess growth hormone suppresses DNA damage repair in epithelial cells. JCI Insight 4, e125762 (2019).
Chesnokova, V. et al. Growth hormone is permissive for neoplastic colon growth. Proc. Natl Acad. Sci. USA 113, E3250–E3259 (2016).
Podlutsky, A. et al. The GH/IGF-1 axis in a critical period early in life determines cellular DNA repair capacity by altering transcriptional regulation of DNA repair-related genes: implications for the developmental origins of cancer. Geroscience 39, 147–160 (2017).
Dominick, G., Bowman, J., Li, X., Miller, R. A. & Garcia, G. G. mTOR regulates the expression of DNA damage response enzymes in long-lived Snell dwarf, GHRKO, and PAPPA-KO mice. Aging Cell 16, 52–60 (2017).
Menashe, I. et al. Pathway analysis of breast cancer genome-wide association study highlights three pathways and one canonical signaling cascade. Cancer Res. 70, 4453–4459 (2010).
Kleinberg, D. L. & Barcellos-Hoff, M. H. The pivotal role of insulin-like growth factor I in normal mammary development. Endocrinol. Metab. Clin. North Am. 40, 461–471 (2011).
Lombardi, S. et al. Growth hormone is secreted by normal breast epithelium upon progesterone stimulation and increases proliferation of stem/progenitor cells. Stem Cell Rep. 2, 780–793 (2014).
Boulter, L., Bullock, E., Mabruk, Z. & Brunton, V. G. The fibrotic and immune microenvironments as targetable drivers of metastasis. Br. J. Cancer 124, 27–36 (2021).
Piersma, B., Hayward, M. K. & Weaver, V. M. Fibrosis and cancer: a strained relationship. Biochim. Biophys. Acta Rev. Cancer 1873, 188356 (2020).
Chakraborty, D. et al. Activation of STAT3 integrates common profibrotic pathways to promote fibroblast activation and tissue fibrosis. Nat. Commun. 8, 1130 (2017).
Tandon, M. et al. Prolactin promotes fibrosis and pancreatic cancer progression. Cancer Res. 79, 5316–5327 (2019).
Sun, W. et al. Regulation of the IGF1 signaling pathway is involved in idiopathic pulmonary fibrosis induced by alveolar epithelial cell senescence and core fucosylation. Aging 13, 18852–18869 (2021).
Duran-Ortiz, S. et al. Growth hormone receptor gene disruption in mature-adult mice improves male insulin sensitivity and extends female lifespan. Aging Cell 20, e13506 (2021).
Ikeno, Y. et al. Reduced incidence and delayed occurrence of fatal neoplastic diseases in growth hormone receptor/binding protein knockout mice. J. Gerontol. A Biol. Sci. Med. Sci. 64, 522–529 (2009).
Bougen, N. M. et al. Autocrine human GH promotes radioresistance in mammary and endometrial carcinoma cells. Endocr. Relat. Cancer 19, 625–644 (2012).
Basu, R., Baumgaertel, N., Wu, S. & Kopchick, J. J. Growth hormone receptor knockdown sensitizes human melanoma cells to chemotherapy by attenuating expression of ABC drug efflux pumps. Horm. Cancer 8, 143–156 (2017).
Qian, Y. et al. Growth hormone upregulates mediators of melanoma drug efflux and epithelial-to-mesenchymal transition in vitro and in vivo. Cancers 12, 3640 (2020).
Arumugam, A. et al. Silencing growth hormone receptor inhibits estrogen receptor negative breast cancer through ATP-binding cassette sub-family G member 2. Exp. Mol. Med. 51, 1–13 (2019).
Lantvit, D. D. et al. Mammary tumors growing in the absence of growth hormone are more sensitive to doxorubicin than wild-type tumors. Endocrinology 162, bqab013 (2021).
Begicevic, R. R. & Falasca, M. ABC transporters in cancer stem cells: beyond chemoresistance. Int. J. Mol. Sci. 18, 2362 (2017).
Chen, Y. J. et al. Autocrine human growth hormone promotes invasive and cancer stem cell-like behavior of hepatocellular carcinoma cells by STAT3 dependent inhibition of CLAUDIN-1 expression. Int. J. Mol. Sci. 18, 1274 (2017).
Wang, J. J. et al. Autocrine hGH stimulates oncogenicity, epithelial-mesenchymal transition and cancer stem cell-like behavior in human colorectal carcinoma. Oncotarget 8, 103900–103918 (2017).
Subramani, R., Nandy, S. B., Pedroza, D. A. & Lakshmanaswamy, R. Role of growth hormone in breast cancer. Endocrinology 158, 1543–1555 (2017).
Subramani, R. et al. Growth hormone receptor inhibition decreases the growth and metastasis of pancreatic ductal adenocarcinoma. Exp. Mol. Med. 46, e117 (2014).
Basu, R., Wu, S. & Kopchick, J. J. Targeting growth hormone receptor in human melanoma cells attenuates tumor progression and epithelial mesenchymal transition via suppression of multiple oncogenic pathways. Oncotarget 8, 21579–21598 (2017).
Yang, J. et al. Guidelines and definitions for research on epithelial-mesenchymal transition. Nat. Rev. Mol. Cell Biol. 21, 341–352 (2020).
Brittain, A. L., Basu, R., Qian, Y. & Kopchick, J. J. Growth hormone and the epithelial-to-mesenchymal transition. J. Clin. Endocrinol. Metab. 102, 3662–3673 (2017).
Mukhina, S. et al. Phenotypic conversion of human mammary carcinoma cells by autocrine human growth hormone. Proc. Natl Acad. Sci. USA 101, 15166–15171 (2004).
Shafiei, F. et al. DNMT3A and DNMT3B mediate autocrine hGH repression of plakoglobin gene transcription and consequent phenotypic conversion of mammary carcinoma cells. Oncogene 27, 2602–2612 (2008).
Zhang, W. et al. Autocrine/paracrine human growth hormone-stimulated microRNA 96-182-183 cluster promotes epithelial-mesenchymal transition and invasion in breast cancer. J. Biol. Chem. 290, 13812–13829 (2015).
Chien, C. H., Lee, M. J., Liou, H. C., Liou, H. H. & Fu, W. M. Growth hormone is increased in the lungs and enhances experimental lung metastasis of melanoma in DJ-1 KO mice. BMC Cancer 16, 871 (2016).
Chandler, C., Liu, T., Buckanovich, R. & Coffman, L. G. The double edge sword of fibrosis in cancer. Transl Res. 209, 55–67 (2019).
Leslie, M. Genetics and disease. Growth defect blocks cancer and diabetes. Science 331, 837 (2011).
Steuerman, R., Shevah, O. & Laron, Z. Congenital IGF1 deficiency tends to confer protection against post-natal development of malignancies. Eur. J. Endocrinol. 164, 485–489 (2011).
Boguszewski, C. L. & Boguszewski, M. Growth hormone’s links to cancer. Endocr. Rev. 40, 558–574 (2019).
Lu, M., Flanagan, J. U., Langley, R. J., Hay, M. P. & Perry, J. K. Targeting growth hormone function: strategies and therapeutic applications. Signal Transduct. Target. Ther. 4, 3 (2019).
Basu, R. et al. A novel peptide antagonist of the human growth hormone receptor. J. Biol. Chem. 296, 100588 (2021).
Wang, H. et al. Inhibition of experimental small-cell and non-small-cell lung cancers by novel antagonists of growth hormone-releasing hormone. Int. J. Cancer 142, 2394–2404 (2018).
Paisley, A. N., Trainer, P. & Drake, W. Pegvisomant: a novel pharmacotherapy for the treatment of acromegaly. Expert Opin. Biol. Ther. 4, 421–425 (2004).
Basu, R., Qian, Y. & Kopchick, J. J. Mechanisms in endocrinology: lessons from growth hormone receptor gene-disrupted mice: are there benefits of endocrine defects? Eur. J. Endocrinol. 178, R155–R181 (2018).
Cohen, P., Clemmons, D. R. & Rosenfeld, R. G. Does the GH-IGF axis play a role in cancer pathogenesis? Growth Horm. IGF Res. 10, 297–305 (2000).
Chesnokova, V., Zonis, S., Barrett, R. J., Gleeson, J. P. & Melmed, S. Growth hormone induces colon DNA damage independent of IGF-1. Endocrinology 160, 1439–1447 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT00976508 (2013).
Hermansen, K., Bengtsen, M., Kjaer, M., Vestergaard, P. & Jorgensen, J. O. L. Impact of GH administration on athletic performance in healthy young adults: a systematic review and meta-analysis of placebo-controlled trials. Growth Horm. IGF Res. 34, 38–44 (2017).
Lupu, F., Terwilliger, J. D., Lee, K., Segre, G. V. & Efstratiadis, A. Roles of growth hormone and insulin-like growth factor 1 in mouse postnatal growth. Dev. Biol. 229, 141–162 (2001).
Wang, Z. et al. Disruption of growth hormone signaling retards early stages of prostate carcinogenesis in the C3(1)/T antigen mouse. Endocrinology 146, 5188–5196 (2005).
Zhang, X. et al. Inhibition of estrogen-independent mammary carcinogenesis by disruption of growth hormone signaling. Carcinogenesis 28, 143–150 (2007).
Swanson, S. M. & Unterman, T. G. The growth hormone-deficient Spontaneous Dwarf rat is resistant to chemically induced mammary carcinogenesis. Carcinogenesis 23, 977–982 (2002).
Bugni, J. M., Poole, T. M. & Drinkwater, N. R. The little mutation suppresses DEN-induced hepatocarcinogenesis in mice and abrogates genetic and hormonal modulation of susceptibility. Carcinogenesis 22, 1853–1862 (2001).
Snibson, K. J., Bhathal, P. S. & Adams, T. E. Overexpressed growth hormone (GH) synergistically promotes carcinogen-initiated liver tumour growth by promoting cellular proliferation in emerging hepatocellular neoplasms in female and male GH-transgenic mice. Liver 21, 149–158 (2001).
Emerald, B. S. et al. αCP1 mediates stabilization of hTERT mRNA by autocrine human growth hormone. J. Biol. Chem. 282, 680–690 (2007).
Snibson, K. J., Bhathal, P. S., Hardy, C. L., Brandon, M. R. & Adams, T. E. High, persistent hepatocellular proliferation and apoptosis precede hepatocarcinogenesis in growth hormone transgenic mice. Liver 19, 242–252 (1999).
Zhang, X. et al. Human growth hormone-regulated HOXA1 is a human mammary epithelial oncogene. J. Biol. Chem. 278, 7580–7590 (2003).
Zhu, T. et al. Oncogenic transformation of human mammary epithelial cells by autocrine human growth hormone. Cancer Res. 65, 317–324 (2005).
Ma, Y. et al. Dysregulation and functional roles of miR-183-96-182 cluster in cancer cell proliferation, invasion and metastasis. Oncotarget 7, 42805–42825 (2016).
Mertani, H. C. et al. Autocrine human growth hormone (hGH) regulation of human mammary carcinoma cell gene expression. Identification of CHOP as a mediator of hGH-stimulated human mammary carcinoma cell survival. J. Biol. Chem. 276, 21464–21475 (2001).
Chen, Y. J. et al. Autocrine human growth hormone stimulates the tumor initiating capacity and metastasis of estrogen receptor-negative mammary carcinoma cells. Cancer Lett. 365, 182–189 (2015).
Divisova, J. et al. The growth hormone receptor antagonist pegvisomant blocks both mammary gland development and MCF-7 breast cancer xenograft growth. Breast Cancer Res. Treat. 98, 315–327 (2006).
Kaulsay, K. K. et al. Autocrine stimulation of human mammary carcinoma cell proliferation by human growth hormone. Exp. Cell Res. 250, 35–50 (1999).
Takahara, K. et al. Human prostate cancer xenografts in lit/lit mice exhibit reduced growth and androgen-independent progression. Prostate 71, 525–537 (2011).
Recouvreux, M. V. et al. Androgen receptor regulation of local growth hormone in prostate cancer cells. Endocrinology 158, 2255–2268 (2017).
Friend, K. E., Radinsky, R. & McCutcheon, I. E. Growth hormone receptor expression and function in meningiomas: effect of a specific receptor antagonist. J. Neurosurg. 91, 93–99 (1999).
McCutcheon, I. E. et al. Antitumor activity of the growth hormone receptor antagonist pegvisomant against human meningiomas in nude mice. J. Neurosurg. 94, 487–492 (2001).
Yan, H. Z. et al. GHR is involved in gastric cell growth and apoptosis via PI3K/AKT signalling. J. Cell Mol. Med. 25, 2450–2458 (2021).
Evans, A., Jamieson, S. M., Liu, D. X., Wilson, W. R. & Perry, J. K. Growth hormone receptor antagonism suppresses tumour regrowth after radiotherapy in an endometrial cancer xenograft model. Cancer Lett. 379, 117–123 (2016).
Wu, X. et al. Growth hormone receptor overexpression predicts response of rectal cancers to pre-operative radiotherapy. Eur. J. Cancer 42, 888–894 (2006).
Wu, X. Y. et al. Growth hormone protects colorectal cancer cells from radiation by improving the ability of DNA damage repair. Mol. Med. Rep. 10, 486–490 (2014).
Minoia, M. et al. Growth hormone receptor blockade inhibits growth hormone-induced chemoresistance by restoring cytotoxic-induced apoptosis in breast cancer cells independently of estrogen receptor expression. J. Clin. Endocrinol. Metab. 97, E907–E916 (2012).
Zatelli, M. C. et al. Growth hormone excess promotes breast cancer chemoresistance. J. Clin. Endocrinol. Metab. 94, 3931–3938 (2009).
Bougen, N. M., Yang, T., Chen, H., Lobie, P. E. & Perry, J. K. Autocrine human growth hormone reduces mammary and endometrial carcinoma cell sensitivity to mitomycin C. Oncol. Rep. 26, 487–493 (2011).
Gentilin, E. et al. Growth hormone differentially modulates chemoresistance in human endometrial adenocarcinoma cell lines. Endocrine 56, 621–632 (2017).
Bogazzi, F. et al. Growth hormone inhibits apoptosis in human colonic cancer cell lines: antagonistic effects of peroxisome proliferator activated receptor-gamma ligands. Endocrinology 145, 3353–3362 (2004).
Arnold, R. E. & Weigent, D. A. The inhibition of apoptosis in EL4 lymphoma cells overexpressing growth hormone. Neuroimmunomodulation 11, 149–159 (2004).
Acknowledgements
J.J.K. acknowledges the support of the State of Ohio’s Eminent Scholar Program that includes a gift from Milton and Lawrence Goll, NIH-R01AG059779, the AMVETS and the Edison Biotechnology Institute at Ohio University. D.E.B. acknowledges the support of ASPIRE funding from Pfizer, NIH-R01AG059779 and the Heritage College of Osteopathic Medicine at Ohio University. V.P. acknowledges the support of funds from Osteopathic Heritage Foundation’s Vision 2020 to Heritage College of Osteopathic Medicine at Ohio University, R01HL140836, R01MD012579 and RO1DK124126. The authors acknowledge J. Young, L. Householder, S. Zhu and A. Jara (Ohio University) for their assistance with the original version of Fig. 1.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks César Boguszewski and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kopchick, J.J., Basu, R., Berryman, D.E. et al. Covert actions of growth hormone: fibrosis, cardiovascular diseases and cancer. Nat Rev Endocrinol 18, 558–573 (2022). https://doi.org/10.1038/s41574-022-00702-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-022-00702-6
This article is cited by
-
NETs: an extracellular DNA network structure with implication for cardiovascular disease and cancer
Hypertension Research (2024)
-
Disease control of acromegaly does not prevent excess mortality in the long term: results of a nationwide survey in Italy
Journal of Endocrinological Investigation (2024)
-
Analysis of the development of gastric cancer after resecting colorectal lesions using large-scale health insurance claims data
Journal of Gastroenterology (2023)