Abstract
Q fever is an infectious zoonotic disease, caused by the Gram-negative bacterium Coxiella burnetii. Transmission occurs from livestock to humans through inhalation of a survival form of the bacterium, the Small Cell Variant, often via handling of animal parturition products. Q fever manifests as an acute self-limiting febrile illness or as a chronic disease with complications such as vasculitis and endocarditis. The current preventative human Q fever vaccine Q-VAX poses limitations on its worldwide implementation due to reactogenic responses in pre-sensitized individuals. Many strategies have been undertaken to develop a universal Q fever vaccine but with little success to date. The mechanisms of the underlying reactogenic responses remain only partially understood and are important factors in the development of a safe Q fever vaccine. This review provides an overview of previous and current experimental vaccines developed for use against Q fever and proposes approaches to develop a vaccine that establishes immunological memory while eliminating harmful reactogenic responses.
Similar content being viewed by others
Brief history and background
The emergence of an unknown abattoir fever in Brisbane (Australia) preceded the discovery of Coxiella burnetii as the causative agent of this illness. In 1938 Derrick was assigned the task of unraveling the mystery behind an unknown febrile illness among abattoir workers in Brisbane. Despite its clinical resemblance to other known diseases, Derrick was convinced it was a new type of fever and denoted it “Q (for query) fever”. Despite his success in transmitting the disease to guinea pigs from blood and urine of infected patients, he was unable to isolate the pathogen and speculated that the causative agent was a virus1. The infected tissue containing the “Q fever virus” was sent to Burnet who determined its structure to be similar to a Rickettsia species. Concurrently Cox and Davis isolated an infectious agent from ticks in Montana (USA). They demonstrated that this agent was a minute Gram-negative pleomorphic Rickettsia-like organism2 and later demonstrated that it could grow in chicken embryo cultures3. The realization that these two discoveries involved the same organism dawned, when Dyer contracted the illness a few days after his stay at the Montana lab with Cox. Later, the organism was renamed “Coxiella burnetii” in honor of Cox and Burnets’ seminal work in identifying this infectious agent.
C. burnetii, the etiological agent of Q fever, causes a flu-like infectious zoonotic disease of worldwide importance4,5. C. burnetii reservoirs in ruminant livestock such as goats, sheep, and cattle who transmit the bacterium via their parturition products. Transmission occurs through direct contact with infected animals or their products of parturition via inhalation of the C. burnetii small cell variant (SCV). For this reason, people who reside in livestock areas and handle livestock are susceptible to Q fever, making it a disease of location and occupation5,6,7. Owing to its excellent environmental stability and low infectious dose, C. burnetii is considered to be a category B agent of bioterrorism by the Centre for Disease Control and Prevention8. The disease has been a substantial cause of morbidity in Australia, with New South Wales and Queensland reporting most cases9,10,11. Q fever is also reported worldwide, and the most notable epidemic was the major outbreak in the Netherlands from 2007–2010 involving 4026 cases12.
Coxiella burnetii
C. burnetii is a pleomorphic Gram-negative bacterium that belongs to the gamma-subgroup of the Proteobacteriacae, order Legionellales, family Coxiellaceae, genus Coxiella and species C. burnetii13. C. burnetii exhibits morphological and antigenic variation. The morphological forms arise from its biphasic developmental cycle and consist of the SCV and the large cell variant (LCV). The SCV is a short rod-shaped, non-replicative extracellular form of C. burnetii. Its structure enables survival under harsh environmental conditions and assists dissemination9,14. As the SCV, C. burnetii invades host cells and gradually develops into the LCV. LCVs are pleomorphic and the metabolically active forms that are capable of replication inside eukaryotic cells14,15.
The phase variations of C. burnetii include virulent phase I and avirulent phase II cells16. The difference between the two-phase variants lies in the structure of the lipopolysaccharide (LPS), a major component of the bacterial cell wall. The full-length LPS (smooth) of the phase I variant consists of Lipid A, inner and outer core with an O-antigen that contains two unique sugars, virenose and dihydrohydroxystreptose17. Upon serial passages in embryonated eggs, cell cultures, and synthetic media, phase I cells gradually transition to avirulent phase II, which consists of a truncated (rough) LPS that only retains the inner core of oligosaccharides and lipid A18,19,20. As C. burnetii is highly infectious, causes consistent disabilities, survives harsh environmental conditions, and can be mass-produced for aerosol transmission, it has been classified as a category B bioterrorist agent. This led to operation Whitecoat carried out by the U.S Army where defensive measures to Q fever, including vaccine candidates, were tested by exposing war-time conscientious objectors to the pathogen21. An aerosolization chamber was used to test volunteers vulnerability to aerosolized pathogens22. While some of the volunteers became sick, they all fully recovered and no death were reported. In the 1990s, a Japanese religious group that used sarin gas to attack Tokyo was known to develop C. burnetii for intentional release23.
Pathogenesis of Q fever
The pathogenesis of Q fever is a convergence of C. burnetii virulence with host cell resistance24. Following inhalation of SCVs, C. burnetii primarily targets alveolar macrophages. They are internalized by both phagocytotic and non-phagocytotic cells25,26. Phase I and phase II enter phagocytic cells through the engagement of different receptors. The uptake of C. burnetii by non-phagocytotic cells is through a “zippering” mechanism. The interaction of surface ligands with cognate receptors on host cells such as fibroblasts8 and HeLa cells27 passively encloses them in a zipper-like manner, accompanied by remodeling of the actin cytoskeleton25,27,28. Recent studies by multi-phenotypic high-content screening identify OmpA as an essential PAMP of C. burnetii that enables its entry into non-phagocytic cells28. Complement receptor CR3 and leukocyte response integrin (αvβ3) are receptors present on monocytes, involved in the uptake29. The avirulent variant is readily recognized by both CR3 and integrin receptors after which it is efficiently eliminated following phagocytosis. In contrast phase I uptake is mediated by αvβ3 alone29,30,31. This difference in receptor recognition lies in the LPS structure variation. The resistance of the phase I variant to serum complement-mediated attack32 suggests that steric hindrance provided by LPS might mask its opsonization by the complement system, hence the lack of recognition by its cognate CR3 receptor. Furthermore, impaired spatial rearrangement of CR3 outside membrane protrusions inhibits its essential crosstalk with the integrin receptor resulting in impaired uptake of phase I bacteria30. Internalization of phase I C. burnetii by the integrin receptor αvβ3, initiates extensive membrane ruffling through rearrangement of the filamentous (F)-actin cytoskeleton controlled by the Rho family of GTPases33,34. Once contained in the early phagosome, now referred to as a “Coxiella containing Vacuole” (CCV), it fuses with early endosomes. This process is similar to the usual canonical pathway and regulated by GTPase Rab5, which recruits early endosome antigen EEA1 that promotes the fusion of the endosome with the CCV35. The maturing CCV increases in size as it enters the late phagosome stage25,26. Rab7 replaces Rab5, while vacuolar ATPase on the CCV membrane pumps protons into the CCV reducing the pH to 5.5–6. Lysosome associated membrane glycoprotein (LAMP) LAMP1 and LAMP 2 are recruited to the late endosome stage35,36. The phagosomes that house phase II C. burnetii transition to a phagolysosome where it is destroyed by the action of lysosomal enzymes such as cathepsins and hydrolases7. Remarkably, studies with THP-1 cells demonstrate that vacuoles that shelter virulent C. burnetii do not acquire lysosomal markers and therefore do not transition to a phagolysosome, escaping their degradation37. Contradicting this theory, later studies reveal that fusion of CCV containing the virulent phase I with lysosome does occur but is halted due to its interaction with the autophagy pathway. The overexpression of the autophagic proteins GFP-LC3 or GFP-Rab24 increases CCV maturation after early infection38,39,40. The CCV membrane equips itself with LC3 markers a few minutes after infection41. The fusion of lysosome protein with CCV is further delayed by starvation-induced autophagy40. Autophagy is a homeostatic process that degrades and recycles molecular components of damaged organelles and proteins inside a cell. It involves the recruitment of Atg8 proteins such as LC3, which enclose the ubiquitinated cargo in the autophagosome. Fusion with the lysosome to generate the autophagolysosome mediates the degradation of the cargo by lysosomal enzymes42,43. The CCV is known to interfere with the host autophagic pathway44 to favor its enlargement and survival inside the host cell40. Diverted phagolysosomal maturation is speculated to provide time for the differentiation of metabolically inactive SCV inside the CCV to the metabolically active LCV form39,45 and the autophagy cargo acts as a source of nutrients to initiate replication and metabolic development to LCV26. The transition of SCV to LCV in mature CCVs halts the late CCV endosome maturation, retains the LC3 markers, and acquires the lysosomal glycoproteins LAMP1, and LAMP226. The acidic pH in the CCV lumen sustains their survival as acidity is required for the assimilation of nutrients required for the synthesis of nucleic acids and amino acids46. Homotypic fusions with multiple small CCVs and heterotypic fusions with autophagic vesicles result in a large parasitophorous vacuole (PV) that occupies half the volume of the cell. The PV is surrounded by a cholesterol-rich membrane and lipid raft proteins flotillin-1 and flotillin-2 that enables membrane fusions39 and is filled with LCV and SCV variants. Six days post-infection the LCV reverts back to the SCV form, retaining the features of late CCV25. The fate of the host cell at this point is exploited in two ways by C. burnetii: (1) it can inhibit apoptosis by actively inhibiting signaling pathways47 or (2) Induction of pro-survival factors such as the ERKI, ERK2, and AKT family48. The need for prolonged survival of host cells could be crucial for the establishment of chronic disease and continued survival of C. burnetii. Similarly, C. burnetii can also initiate apoptosis of invaded host cells in a caspase-independent pathway, disseminating replicating bacteria to infect other susceptible cells49.
Host immune responses
One characteristic of the facultative intracellular C. burnetii is its ability to survive and replicate in the acidic niche of phagocytes50. This makes them inaccessible to circulating antibodies and the complement system. Cell-mediated responses are required for the elimination and control of infection. While the acute infection is sometimes controlled by innate mechanisms, host responses to chronic infection require a more specific adaptive arm of the immune system51,52.
Innate responses to C. burnetii
Innate responses are mediated by monocytes, macrophages and natural killer (NK) cells. Monocytes and macrophages, which are the primary targets, have differential responses depending on the variant that invades the cell. Invasion by phase II can be readily controlled by innate phagocytic function, whereas phase I C. burnetii requires the combined forces of innate and cell-mediated responses to eliminate them50,53.
Monocytes and macrophages
The interaction of C. burnetii with macrophages and monocytes induces their polarization into the M1 or M2 macrophage phenotype. During acute infection, circulating monocytes polarize toward the M1 phenotype, which secretes the cytokines IFN-γ, IL-6, IL-12, and expresses CCR754. The upregulated expression of nitric oxide synthase (NOS) catalyzes the conversion of L-arginine to citrulline to produce reactive nitrogen species (RNS) that are microbicidal and contribute to the control of infection54,55,56. Tissue-resident macrophages are directed toward an atypical M2 phenotype that is characterized by the expression of the chemokine receptor CXCL8 and cytokines such as TGF-β1 and IL-6. The arginine pathway in the M2 phenotype is directed by the upregulated expression of arginase to ornithine and urea which are precursors for proline and polyamine synthesis and are involved in tissue repair56.This antagonistic phenotype acts to “heal and fix” without killing the harboring C. burnetii promoting their survival and replication. During chronic infection, macrophages significantly reprogram toward the M2 phenotype. Although there is no conclusive evidence as to how this occurs, it is speculated that apoptosis of leukocytes in endocarditis results in their uptake by macrophages promoting the M2 phenotype that exhibits anti-inflammatory and immunosuppressive responses through the release of IL-10 and TGF-β57,58 facilitating the replication and dissemination of C. burnetii. M1 and M2 macrophages alleviate their specific responses, by directing T cells to differentiate into TH1 or TH2 lineage, respectively. The IL-4 and IL-10 cytokines produced by the M2 phenotype leads to the TH2 response, while IFN-γ and IL-12 produced by the M1 phenotype leads to the TH1 response. Subsequently, T cells continue to produce their respective cytokines, further driving macrophage effector functions in a positive feedback loop55. Macrophages derived from phase I immunized guinea pigs effectively degraded phase I C. burnetii even in the absence of immune serum59. Increased phagocytic activity without the involvement of antibodies indicates T cell-dependent activation. Macrophages, in addition to their role as phagocytes, present antigens in the form of peptide MHC-II complex for T cell activation60. The significance of this mechanism was underscored by the absence of protection in phase I-vaccinated mice lacking MHC-II molecules when subjected to C. burnetii infection61. Furthermore, the potent activation of macrophages commences with Toll-like receptor (TLR) recognition of pathogenic components, inducing transcription pathways that release mediators to prime adaptive immune responses. Studies on TLR2-deficient mice have demonstrated defective production of pro-inflammatory cytokines, such as TNF-α and IL-12 upon C. burnetii infection62. IL-12 promotes T cell differentiation to TH1 cells and exhibits synergistic effects with TNF-α for IFN-γ mediated killing of C. burnetii63. Hence, the protective mechanisms mediated by macrophages during C. burnetii infection and vaccination are a combined effort of the innate and cell-mediated immune responses.
Neutrophils
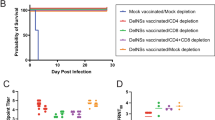
As first responders to infection, they can recognize, ingest, and kill pathogens without adaptive responses. Phase I and II strains of C. burnetii infect neutrophils at a lower infection rate and infected neutrophils can further replicate and invade macrophages during apoptosis clearance of neutrophils64. An aerosolized infection model of SCID mice demonstrated delayed neutrophil influx at the infection site. This delay was explained by the reduction in pro-inflammatory cytokines attributed to C. burnetii immune evasion64. Neutrophil-depleted mice showed reduced body weight, increased splenomegaly, and increased bacterial burden upon infection with C. burnetii. This indicated their role in clinical disease reduction and bacterial clearance65. In contrast, phase I vaccinated and neutrophil-depleted mice displayed reduced body weight and splenomegaly with no difference in bacterial clearance compared to control mice. This suggests neutrophils play a role in vaccine-induced reduction of clinical signs, and not in bacterial clearance65.
Dendritic cells
Dendritic cells (DC) or “alarm cells” are the immune sentinels that bridge the innate and adaptive immune responses. Their ability to acquire antigens and present them in the form of peptide MHC complexes to T cells orchestrates the cell-mediated responses to infections. In vitro studies with C. burnetii have shown that virulent phase I interferes with DC maturation. Human DCs infected with phase I expressed low levels of maturation markers such as MHC class II, CD80, CD86, CD83, and CD40 compared to the increased expression in phase II-infected DCs66,67. This study also demonstrated that phase II-induced DC maturation is TLR4-independent with increased production of IL-12 and TNF-α67. Contradicting this finding, Grovel et al. demonstrated the partial maturation of C. burnetii infected DCs with downregulated expression of TLR4, TLR3, STAT1, and interferon response genes68. This observation is further supported by a recent study in which, phase II infected DCs showed downregulated MHC expression with impaired maturation. However, the administration of IFN-γ reversed the inhibitory effects of phase II on DCs69. Many of these studies utilized monocyte-derived dendritic cells which have the disadvantage of poor IL-12p70 production, a heterodimer required for the activation and differentiation of TH1 cells70. Investigating the effect of different variants on DC subsets such as conventional DCs might shed more light on infection induced DC responses to C. burnetii. Several studies in murine models have shown the importance of DCs in vaccine-induced immunity. The chemokine receptor CCR7 directs DCs to lymph nodes for initiation of T cell responses71. The termination of phase I WCV induced cellular responses in Ccr7−/− mice, highlights the importance of DC trafficking to lymph nodes for initiation of cell-mediated responses66. In mice, the administration of phase II WCV-pulsed bone marrow-derived dendritic cells (BMDCs) led to a decrease in bacterial burden, demonstrating the protective role of antigen-activated BMDCs. This was linked to an increase in the proliferation of TH1 CD4+ helper T cells, skewed enhancement of TH17 cells, and a suppression of regulatory T cells72. T-bet is a transcription factor that is expressed in both lymphoid and myeloid lineages. T-bet is required by DCs for the production of IFN-γ, TNF-α, and activation of antigen-specific T cells73,74. T-bet knock out (KO) mice exhibited significant body weight loss and splenomegaly compared to phase I-vaccinated wild-type mice, indicating the essential role of DCs in initiating T cell-mediated responses75.
Cell-mediated responses
The adaptive arm of immune defense marks the final defeat of the invading intracellular pathogens. Cell-mediated responses are primarily important for the clearance and control of C. burnetii, as they directly augment infected cells to boost their microbicidal activity (Fig. 1). Because of the intracellular nature of C. burnetii it is inaccessible to the effects of the humoral response51. Consequently, T cell-mediated killing of infected cells provides an important mechanism to prevent C. burnetii infection. The indispensable role of T cells in inducing cellular effector functions is demonstrated by the inability of severe combined immunodeficiency (SCID) mice to clear the infection with Nine Mile phase I (NMI) and phase II (NMII) strain76. Adoptive transfer of CD4+ and CD8+ T cells alone to infected SCID mice was sufficient to eliminate infection, conversely wild-type (WT) mice depleted of both T cells were susceptible to infection, whereas depletion of only one type of T cell, controlled infection77. SCID mice that received splenocytes and T cells from phase I immunized mice prevented splenomegaly and splenic bacterial burdens upon challenge, in addition to protection against the development of clinical disease and loss of body weight78. The initiation of the cellular cascade begins when C. burnetii is taken up by antigen-presenting cells at the site of infection. Dendritic cells in the mucosal airways are key mediators in shuttling C. burnetii from the site of infection (lungs) to the nearest lymphoid tissue to initiate T cell responses. In addition, C. burnetii can be disseminated to draining lymph nodes following infection79. Once in the mature and draining lymph nodes, activated and mature DCs present antigens in the form of an MHC class II peptide complex to naïve T cells. Upon infection with NMI, MHC II deficient mice exhibited translational loss in body weight, compared with WT mice61. Vaccination with inactivated NMI failed to reduce the bacterial load in MHC II KO and alum immunized mice75. Antigen-specific T cells proliferate and differentiate into effector CD4+ T cells. CD4+ T cells differentiate to the TH1 subset, which is largely determined by cytokines secreted by innate immune cells encountering an antigen. IFN-γ and IL-2 are characteristic cytokines produced by TH1 cells and are also the cytokines that drive their differentiation to TH1 subset. Individuals vaccinated with inactivated whole-cells exhibited lymphoproliferation and IFN-γ production suggesting a TH1 type response78,80,81. Upon encountering an infected macrophage, TH1 cells activate them to become more potent in their microbicidal functions. This classical activation is mediated by IFN-γ and co-stimulatory signals through the interaction of CD40L with CD40 on macrophages. IFN-γ activates the transcription factor STAT1, and CD40 signals activate nuclear factor-kappa beta (NF-κB). Together these induce lysosomal enzymes and the expression of phagocyte oxidase and inducible nitric oxide synthase (iNOS) enzymes that produce reactive oxygen (ROI) and nitrogen intermediates (RNI) respectively25,26,82. All these potent microbicidal agents help to kill C. burnetii, thus preventing their replication inside macrophages. The inability of iNOS−/− and p47phox−/− mice to control infection, upon challenge with C. burnetii, supports the role of RNI in host control of infection83. The vital role of IFN-γ in bacterial clearance has been demonstrated in IFN-γ−/− mice models, and high-dose infection with NMI results in bacteremia and mortality during the early phase of infection76. In vitro studies with NMI infected THP-1 monocytes have revealed the ability of IFN-γ to reinstate the impairment of phagosome maturation47 and promote vacuolar alkalinization37. Infection of mouse L-292 cells with C. burnetii upregulates IFN- γ production, which augments iNOS expression46. Furthermore, IFN-γ activated macrophages from iNOS−/− and p47phox−/− mice were able to impede bacterial replication, indicating the potential of IFN-γ to activate iNOS- independent bacteriostatic mechanisms83. Although CD4+ T cell-dependent mechanisms have demonstrated their importance in C. burnetii clearance, Ledbetter et al. reported that CD4+-independent mechanisms play a more critical role in C. burnetii clearance in NMI-vaccinated mice66. The reduction in body weight, splenomegaly, and bacterial burden in MHC-I-deficient (β2m KO) mice compared to MHC II KO mice, indicates that protection by MHC I CD8+ T cells is crucial for C. burnetii clearance61. Furthermore, SCID mice reconstituted with CD4+ T cells alone exhibited increased bacterial burden and splenomegaly compared to mice reconstituted with CD8+ T cells77. This is likely due to the cytolytic activity of effector CD8+ T cells, which kill infected cells through the release of cytolytic compounds and induction of apoptosis in infected cells. While T cells are important for the primary clearance of C. burnetii, the role of B cells and their effector antibodies remains unclear. Antibody-mediated immunity includes, opsonization, complement-mediated killing and antibody‐dependent cellular cytotoxicity (ADCC)84,85. These effector functions are extracellular; hence, the role of antibodies for intracellular bacteria such as C. burnetii becomes crucial for the duration of time they are in the extracellular phase before inhabiting their target cells85. Vaccine-induced protection depends on B cell immunity, as indicated by increased splenomegaly and spleen bacterial loads in B cell-deficient mice compared to those in WT mice. This immunity is dependent on T cell-independent IgM, which inhibits C. burnetii infection in vivo86. Furthermore, this study demonstrated that antibody-mediated immunity is complement and FcR receptor-independent. This hypothesis is supported by a recent study in which FcR-KO, complement deficient, and WT mice were equally protected following passive immunization with mouse immune serum87. Previous findings where C. burnetii specific anti-serum added to macrophages failed to control their intracellular replication88 and the inability of macrophages to control antibody opsonized C. burnetii87 indicate a role for antibodies in initial clinical stages but not for clearance or elimination of infection. Schoenlaub et al. demonstrated that a population of B cells, B1a cells, might play a role in regulating the inflammatory response during C. burnetii infection. C. burnetii infected B1a cells induced high levels of IL-10 and TNF-α in vitro, whereas in vivo mice deficient in B1a cells (BTKxid) exhibited increased spleen inflammation, reduced IgM titers, and reduced levels of TNF-α89. However, these contradictory observations suggest that population of B cells might have a regulatory role in vitro, although this is insignificant in vivo.
T cell responses are initiated upon peptide-MHC recognition by T cell receptor. Activated T cells differentiate to CD4+ helper T cells that secrete cytokines that activate B cells, macrophages, and inflammation. Activated B cells differentiate to plasma cell that produce antibodies. Antibody effector mechanisms include opsonization and Fc receptor mediated phagocytosis and complement activation.
Q fever vaccine development: hits and misses
Since the discovery of the pathogen, many approaches have been taken to develop vaccines against Q fever, but no fully safe and effective vaccine has been developed to date. The only licensed vaccine currently available is Q-VAX, an inactivated whole cell vaccine derived from the Henzerling phase I strain. This vaccine is licensed for use only in Australia, and its worldwide administration is limited because of its reactogenic nature. Therefore, a pre-screening test including a skin test and serology is mandatory before administration. Owing to its restricted availability and safety, attempts to develop a safe vaccine are still an ongoing race with limited success. No vaccine has proven efficacy or afforded protection equivalent in humans to that of Q-VAX. To develop a successful vaccine, it is crucial to target, the concise immune effectors that are required to eliminate the pathogen and induce immunological memory to combat the pathogen in subsequent encounters without the establishment of disease. Most Q fever vaccines developed to date induce an immunological response but fail to confer protective immunity. These Q fever vaccine candidates can be categorized as whole cell vaccines or subunit vaccines and are summarized in Table 1.
Whole-cell vaccines
Whole-cell vaccines (WCV) can either be live attenuated or killed inactivated.
-
(1)
Live attenuated vaccines: one of the early vaccines developed for Q fever was the live attenuated vaccine M-44, which was used in Russia during the 1960s. This vaccine contains the Grita strain of C. burnetii, which was made avirulent by repeated passaging in embryonated yolk sacs90. Mass immunization of humans with live vaccine demonstrated mild reactogenicity following subcutaneous administration91. However, complications such as myocarditis, hepatitis, necrosis, and granuloma formation were identified 8 days post-infection in immunized guinea pigs, questioning its safety92. The use of avirulent viable NMII C. burnetii as a potential vaccine candidate was assessed in mouse models. This study demonstrated that intranasal immunization with NMII induced protection against NMI challenge, However, no information regarding reactogenicity was provided93.
-
(2)
Inactivated vaccines: to develop a refined Q fever vaccine, two inactivated vaccines derived from the Dyer or Henzerling strains were introduced in the 1980s. These vaccines are composed of formaldehyde-inactivated C. burnetii strains obtained from infected yolk tissues94. Evaluation of their efficacy in guinea pigs revealed a mortality rate of 40–80% in unvaccinated guinea pigs compared to 1–6% in vaccinated guinea pigs. When tested in humans, 3 out of 28 individuals developed mild systemic reactions, such as fever, anorexia, and malaise, with no serious reactions94. In mid-1981, clinical trials of inactivated Henzerling strains were conducted among abattoir workers and high-risk groups in South Australia to control Q fever95. At 18 months after vaccination, no Q fever cases were reported among 924 vaccinated subjects, whereas 34 cases were reported among 1349 unvaccinated subjects96. The trial revealed that vaccine conferred 100% protection in humans that lasted for at least 5 years. Assessment of cellular and humoral immunity revealed 80–82% seroconversion following vaccination, and lymphoproliferative responses in 85–95% of vaccinees95,97. The formalin-inactivated Henzerling strain vaccine; Q-VAX is currently approved for use only in Australia. The unsuccessful worldwide implementation is due to the occurrence of adverse effects in pre-sensitized individuals, primarily at the site of injection98,99. Data on adverse effects following immunization for Q-VAX were collected from clinical trials in abattoir workers95,97 and a mass vaccination program in the Netherlands following a Q fever outbreak100. These surveys revealed common reactions to vaccination such as erythema or induration at the injection site, with infrequent fever and transient headaches95,96,100. However, more severe reactions, such as delayed-type hypersensitivity reactions (DTH) were reported in individuals with prior exposure to C. burnetii99,101,102. For this reason, a pre-vaccination screening prior to vaccination is performed to determine pre-existing cellular or humoral immunity against C. burnetii. Recently, genetic engineering of whole-cell pathogens has been used, in which gene knockouts selectively remove the gene required for the pathogenicity of the organism rendering it avirulent and suitable for use as an attenuated vaccine. This also eliminates the risk of the organism reverting to its original virulent form. Based on this theory, a recent study assessed the immunogenicity and reactogenicity of a mutant version of the NMI strain in a guinea pig model. A 32 kb region encompassing 23 genes of the dot/icm system was deleted while retaining the phase I LPS. The resultant Δdot/icm mutant was avirulent in a guinea pig challenge model but demonstrated protective immunity following C. burnetii challenge with Δdot/icm sensitized guinea pigs. However, this vaccine displayed altered reactogenicity suggesting that the C. burnetii type IVB secretion system (T4BSS) is indispensable for vaccine-induced immunity but is a factor of post-vaccination hypersensitivity20. To further mitigate reactogenicity, whole-cell extracts of C. burnetii were explored for their potential as vaccines. In 1982 a chloroform-methanol extraction was used to extract the components of phase I Ohio strain. The extraction yielded a soluble phase consisting of lipids and a chloroform-methanol residue (CMR) composed of phase I LPS, proteins, and peptidoglycan103. When tested as a vaccine the CMR demonstrated good efficacy at a lower dose than Q-VAX in mice, and a dose four times higher than that of Q-VAX in guinea pigs, and a similar dose to Q-VAX in primates, but at the cost of local reactions104,105,106. A trichloroacetic acid (TCA) extract containing phase I antigenic components demonstrated more than 90% protection in C. burnetii challenged guinea pigs102,107. However, local reactions post-vaccination, such as transient erythema and local pain for several days at the site of injection have been reported with no severe abscesses102. Detergent extraction to obtain soluble antigens from the NMII avirulent strain yielded a soluble extract vaccine. When formulated with CpG adjuvant, this vaccine induced protective immunity in mice and guinea pigs against C. burnetii challenge with reduced erythema and induration at the site of injection compared to the whole-cell vaccine108.
Reactogenicity associated with WCVs is a result of innate and adaptive immune activation109. The recognition of conserved bacterial ligands called “pattern associated molecular patterns” (PAMPs) by pattern recognition receptors (PRRs) present on immune cells induces the production of inflammatory mediators that drive the adaptive response. During the initial exposure to C. burnetii this concomitant stimulation is favorable for pathogen clearance. However, during subsequent exposure in the form of vaccination or re-infection, the activation of adaptive responses together with innate recognition leads to an injurious cytokine-mediated inflammation called DTH reactions, which are mainly mediated by CD4+ T cells110. This reaction manifests as induration and swelling and occurs 24–48 h after antigen exposure. Clinical evaluation of guinea pig models following sensitization and immunization with C. burnetii showed a type IV hypersensitivity reaction101,111. With WCVs, there should be a fine balance between safety and immunogenicity, and the pathogen in the formulation should be virulent enough to induce immunological memory but less reactogenic to not elicit DTH reactions during subsequent exposure in the form of infection or vaccination.
Subunit vaccines
Subunit vaccines are composed of immunodominant antigenic components that can be recombinantly produced or purified from microbes112. They offer the advantages of reduced reactogenicity and cost-effective production over traditional WCVs113. To augment immunogenicity, they are fused with a carrier or formulated with an appropriate adjuvant and administered in a multi-dose regimen113,114,115. A subunit vaccine composed of the outer membrane protein of C. burnetii; Com1 antigen formulated with TLR triagonist was evaluated for immunogenicity and reactogenicity in a mouse model. Although it induced a strong IgG2c skewed response it only conferred partial protection against C. burnetii compared to Q-VAX116. Fratzke et al. designed a subunit vaccine using six C. burnetii antigens formulated with multiple TLR agonists. Of the various vaccine formulations with different TLR agonists, only one vaccine containing TLR4, TLR7, and TLR9 agonists as triagonists demonstrated reduced reactogenicity and comparable bacterial burden to WCVs117. The findings from these studies emphasize the use of an appropriate adjuvant for subunit vaccine development to induce the desired immune response required for C. burnetii clearance. Phase I LPS (LPSI) of C. burnetii is considered a virulent determinant and most studies have explored LPS I as a vaccine candidate. The immune response induced by LPSI reduced C. burnetii loads in the spleen of intraperitoneally challenged mice but remained high in the spleens of mice after aerosol challenge103. An LPSI mimetic peptide m1E41920 screened using an LPSI monoclonal antibody (1E4) was conjugated to keyhole limpet hemocyanin (KLH) and tested in a mouse model. Although this combination induced transferable humoral responses, its protective efficacy was less than that of LPSI-immunized mice118. Recently a human T cell-directed epitope vaccine based on human leukocyte antigen (HLA) Class II T cell epitopes of C. burnetii was designed and evaluated in three animal models. Although the vaccine candidates induced a non-reactogenic response in a sensitized guinea pig model, the immune response elicited in mice was skewed toward a single epitope, which was deficient in conferring protection against C. burnetii challenge81. In addition, a tetanus toxoid carrier conjugated to a polysaccharide derived from phase I C. burnetii was recently developed as an alternative vaccine to Q-VAX. This vaccine demonstrated reduced febrile responses with reduced body weight loss in vaccinated guinea pigs post challenge with C. burnetii. Assessment of C. burnetii loads in the liver, spleen and kidney showed a significant reduction in vaccinated guinea pigs compared to unvaccinated controls18. One drawback of subunit vaccines is inadequate protective responses required for C. burnetii clearance. Identification of immunodominant antigens and selection of epitopes are crucial factors in designing subunit vaccines and require more knowledge beyond immunoinformatics.
Moving forward: immunological targets for a better Q fever vaccine?
The current hurdle in Q fever vaccine development is the failure to generate long-lived immunological protection that prevents re-infection or disease severity. A vaccine that is equally efficacious, but less reactogenic than Q-VAX, remains the benchmark for developing an ideal Q fever vaccine. Approaches to implement this objective require an understanding of the precise immune mechanisms involved in the clearance of C. burnetii and the development of vaccines that elicit such responses at a certain threshold. Owing to its ability to build an intracellular niche C. burnetii requires T cell-driven adaptive responses for control and clearance. The induction of long-lived immunological memory requires the generation of memory T cells (both CD4+ and CD8+) and plasma B cells that secrete high affinity antibodies. To this end, we focused on vaccine strategies that warrant the induction of antigen-specific effector memory T or B cells, for better Q fever vaccine development.
Programming T-cell responses
The three phases of T cell response include activation, differentiation, and induction of memory. Immunological memory depends on the quantity and quality of memory T cells, which in turn depend on the magnitude of T cell expansion induced by a vaccine. The clonal expansion of T cells is modulated by T cell activation which is a collective effect of antigenic stimulation, co-stimulation, and polarizing cytokines released by innate mechanisms. These parameters can be influenced by the different forms of vaccination. During the activation phase, antigen recognition by TCR occurs through interaction with the peptide-MHC complex. Designing vaccines that effectively provide the unprocessed antigen to mature dendritic cells for exogenous or endogenous processing, and presentation to T cells via MHC molecules is an approach for targeted antigen delivery required for the activation phase (Fig. 2). Targeted delivery can be achieved by coupling antigens with immunomodulators that target the antigen-presenting cells. Approaches include linking antigens with antibodies against specific receptors present on APCs, for example, administration of anti-CD205 with antigens, induces CD205+(DEC-205) DCs a specific subset of cross-presenting DCs present in the spleen119. Additionally, antigen cross-presentation can be enhanced by co-delivery of anti-CLEC9A antibodies that target CLEC9A, a C-type lectin expressed exclusively by conventional dendritic cells120,121. Furthermore, the co-delivery of anti-CD40 promotes DC maturation through the interaction of CD40L on T cells. This interaction recruits the antigen-presenting cell to enhance expression of co-stimulatory molecules (B7-1, B7-2) and T cell differentiating cytokines such as IL-12, which further promotes potent activation of cognate T cell122. Adjuvants are an alternative form of immunomodulators that induce innate effectors to supplement adaptive responses. The use of PAMPs as adjuvants in vaccine formulations enables innate recognition of antigens, by PRRs123, resulting in the production of inflammatory cytokines that create an appropriate cytokine milieu for the activation and phenotypic differentiation of T cells. This approach has been explored in recent studies and has demonstrated protective immunity post-challenge with C. burnetii116,117,124. The incorporation of cytokines as adjuvants125 has yet to be explored as a vaccine approach for Q fever. A recent study revealed that IL-12 loaded nano-vaccine induced Hepatitis B virus-specific CD4+ and CD8+ T cell responses with long-term memory responses126. The incorporation of cytokines such as IL-12 or IFN-γ along with C. burnetii antigens as DNA vaccines could be explored as a promising Q fever vaccine. Collectively, these approaches trigger robust activation of T cells, which eventually become programmed for clonal expansion, followed by the contraction phase once the pathogen is cleared and eventually goes into induction of memory phase, the ultimate goal of a successful vaccine.
a Administration of anti-CD205 or CLEC9A with antigens, induces DC maturation and enhanced cross-presentation. b Anti-CD40 induces DC maturation, expression of costimulatory molecules and cytokines for T cell differentiation. c Co-delivery of TLR ligands with antigens: TLR9 present on the endosomal membrane detects unmethylated CpG DNA, TLR4 present on the cell membrane detects bacterial LPS. This innate recognition by pattern recognition receptors, in conjunction with antigen stimulation drives T cell activation.
Programming B-cell responses
Although intracellular C. burnetii remains inaccessible to antibodies, the role of humoral response in C. burnetii clearance and control becomes beneficial during the initial extracellular phase of C. burnetii. High affinity antibodies are produced in the germinal centers of lymphoid follicles during affinity maturation a process that selectively picks B cells with high affinity B-cell receptors (BCRs)127. B cell activation drives the germinal center (GC) reaction consisting of somatic hypermutation, affinity maturation, isotype switching, and generation of memory B cells128. Memory B cells upon subsequent antigen exposure, rapidly induce a secondary response, present antigens to memory T cells, and generate plasma cells within days feasibly before C. burnetii homes inside macrophages or monocytes129,130. Effective B cell stimulation requires antigen recognition and co-stimulation from cognate T cells. Activation of antigen-specific B cells is initiated by binding of antigen to BCR, which is internalized and presented as peptide-MHC complex to cognate T cells. In addition, it has been shown that APCs present antigens to B cells131,132. Targeted delivery of antigens to APCs can drive B cell activation similar to T cells, and this has been discussed in the previous section. Antigen valency is another factor that impacts B cell activation133. Multivalent antigens have demonstrated potent B cell signal transduction via BCR clustering compared to monovalent antigens134,135. Multiple antigens can be delivered by particulate carriers, which can also be fine-tuned to unload the antigen cargo in the lymphoid organs136,137. Targeting complement activation for antigen delivery to follicular dendritic cells (FDC) in the GC is an effective approach to drive GC reactions138. Glycosylated nanoparticles were shown to activate the complement system through mannose-binding lectin (MBL) pathway and subsequently deliver the antigen load to FDCs expressing complement receptors139,140. The FDCs present the antigens to B cells driving their affinity maturation during GC reaction. The various approaches are summarized in Fig. 3.
a Multivalent antigens cause B cell receptor clustering that initiates signal transduction, which combined with costimulation from cognate T cells, amplifies B cell activation. b Nanocarriers help to unload antigen cargo in lymph nodes, they can be bioengineered for controlled release of antigens; glycosylated antigens activate the mannose-binding lectin complement pathway, that produces C3b, for antigen opsonization, which eventually binds to complement receptors in follicular dendritic cells. These cells display the antigens for recognition by B cells during the process of affinity maturation in the germinal centers.
Eliminating vaccine-associated hypersensitivity
Threshold of activation
It has been described that CD4+ and CD8+ T cells have preferential requirements of co-stimulatory activation and distinct mechanisms in developing into effector T cells. CD8+ requires a lower threshold for activation as a consequence of universal MHC I. In contrast, CD4+ requires a high threshold of activation owing to the restricted expression of MHC class II and the need for co-stimulation by intrinsic ligands141,142,143. The DTH reactions induced in previously sensitized Q-VAX recipients are mediated by CD4+ T cells111. Induction of such responses during a secondary response in the form of vaccination depends on the supply and length of antigen exposure. Taking into consideration the high threshold of CD4+ activation, a WCV fulfills the antigen requirement for elicitation of high-frequency DTH CD4+ T cell responses. Switching the complete pathogen cargo in the form of the WCV to immunodominant antigens as subunit or particulate vaccines might mitigate the amplitude of aggressive CD4+ T cell responses while sustaining a sufficient threshold for CD4+ T activation137,144,145.The subcutaneous route of administration is known to retain antigens at the site of injection, which amplifies the recruitment of CD4+ T cells and cytokines to the site of injection. As C. burnetii transmission occurs by inhalation of SCV, induction of mucosal immunity by intranasal routes of administration paves an alternative approach to eliminating hypersensitivity reactions. This route could also prevent C. burnetii entry to cells through IgA-mediated effector functions146,147.
Vaccine components
Post-vaccination hypersensitivity reactions can result from individual vaccine components, including egg proteins, additives, and inactivators110. The use of formaldehyde to chemically inactivate C. burnetii may also contribute to Q-VAX-associated hypersensitivity. Although formaldehyde is removed from vaccines through purification processes, traces remain in the end-product148,149. It has been shown that formaldehyde-treated vaccines can cause reactive carbonyl groups to form on proteins, resulting in the development of novel immune-triggering epitopes or the unmasking of hidden immunogens that elevate non-specific immune responses150,151. Formaldehyde specific dermatitis have been reported following vaccination with Hepatitis B and influenza vaccines152,153. It is possible to eliminate formalin-associated hypersensitivity using alternate inactivation processes when considering a whole-cell vaccine for Q fever. Another probable factor contributing to hypersensitivity may stem from egg proteins present after purification of C. burnetii from chicken yolk tissues154. Studies on influenza vaccines have examined the safety of vaccines containing egg proteins, and indicates that vaccination of egg-allergic children with influenza vaccines does not pose a greater risk of allergic reactions155. However, not much data is available for egg-derived C. burnetii-based vaccines.
Further considerations for effective Q fever vaccine development
In addition to identifying immunological targets and eliminating reactogenicity, it is imperative to consider other aspects of vaccine development for an improved Q fever vaccine, including (1) identification and selection of antigens, (2) vaccine delivery systems, (3) safety and scalability of antigen production, (4) screening for reactogenicity and (5) route of administration.
Identification and selection of antigens
In recent years, the use of reverse vaccinology has enabled the identification of potential antigenic determinants in the C. burnetii genome. Many studies have focused on evaluating predicted antigens and epitopes as vaccine candidates in various animal models. Several immunoproteomic and protein microarrays have revealed sero-reactive C. burnetii antigens in murine and human sera148,149,150,151,152. Based on these findings, the identified antigens were screened for HLA class I and class II epitopes using bioinformatic analysis153. These epitopes were able to induce IFN-γ recall responses in HLA-DR3 transgenic mice and individuals exposed to a Q fever outbreak. The class II HLA epitopes identified in this study demonstrated robust T cell responses in patients with chronic Q fever as measured by direct ELISPOT, and these responses were comparable to those of convalescents154. Furthermore, another study evaluated the T cell epitopes of C. burnetii immunodominant antigens based on their MHC class II binding capacity and assessed their potential as T cell vaccines in mice155. Although protection was only established in mice immunized with a cocktail of epitopes, this study emphasizes the need for T cell epitopes to be present in vaccine candidates for the induction of protective immunity. A viral vector vaccine expressing concatemers of selected HLA class II epitopes demonstrated a single epitope-specific response in mice, whereas a broad range of epitope-specific responses was induced in cynomolgus macaques81. These findings emphasize the need to select antigens that elicit immune responses in a wide range of species. Besides protein antigens, C. burnetii phase I LPS has also been evaluated as a potential Q fever vaccine antigen118. Based on previous observations that LPS plays a major role in WCV-induced protection, LPS based vaccine candidates were recently developed and mediated significant reduction in clinical signs and bacterial burden implicating the involvement of phase I LPS in C. burnetii protective immune responses18,156. Xiong et al. reported novel MHC Class I epitopes from C. burnetii Type IV secretion system (T4SS) none of which were identified as immunodominant antigens through antibody-based methods157. These peptides were able to induce robust CD8+ T-cell recall responses in infected mice and conferred measurable protection when tested as potential antigen candidates via the Listeria monocytogenes vaccine vector. Alternatively, a recent study reported that the Type IVB secretion system (T4BSS) of C. burnetii is dispensable for vaccine -induced immunity but may contribute to vaccine-induced hypersensitivity20. Despite significant advances, the fact that similar systems of C. burnetii induce different responses in hosts reveals gaps in our understanding of C. burnetti antigens.
Vaccine delivery systems
Delivery systems enable the targeted and controlled release of antigens to the site of the immune response. These systems can also be effectively tailored to induce the desired immune response by altering their physical characteristics such as size, geometry, and surface charge158,159,160. Delivery systems currently in use include biopolymers, liposomes, immune-stimulating complexes (ISCOMs), virus like particles (VLPs), and bacterial and viral vectors. A few studies have investigated the use of viral and bacterial vectors to incorporate C. burnetii antigens and have demonstrated the potential of these delivery systems to elicit cell-mediated responses81,157. Biopolymer-based vaccines have been evaluated as vaccine platforms for intracellular pathogens and have demonstrated the ability to elicit antigen-specific cellular responses that confer protective immunity against infection161. These studies are promising and encourage the use of delivery systems as an improved Q fever vaccine approach to eliminate reactogenicity and to boost desirable immune responses.
Safety and scalability of antigen production
The laborious production of conventional WCVs carries the risk of handling C. burnetii which poses a threat to laboratory personnel and limits the scalability of production. Modern advancements have surmounted this barrier with alternative vaccine approaches, including nucleic acid-based vaccines, subunit vaccines, and gene knockout WCVs. C. burnetii protein production using recombinant technology has significantly reduced safety concerns. Protein expression systems, such as e.g., using safe Escherichia. coli as production host, have enabled scalable production of biopolymer- and protein-based vaccines136,137,162. These strategies provide alternative paths for the safe, cost-effective, and scalable production of Q fever vaccines.
Screening for reactogenicity
The current approach for reactogenicity screening of experimental vaccines involves a sensitized animal model. Guinea pigs appear to be the primary model because of their physiological resemblance to human disease, while mice and non-human primates serve as complementary models163. The use of non-mammalian models, such as the Galleria mellonella insect model, has also been explored and overcomes the ethical and high cost limitations of mammalian models164. The complexity of the immune response coupled with a lack of understanding of the correlates of infection and vaccine-induced protection makes it difficult to define an ideal model for reactogenicity screening. Telemetric measurements to monitor systemic side effects of vaccination have been reported to be more useful than conventional clinical scoring methods165. Identification of potential biomarkers of vaccine induced responses can serve as predictors of systemic reactogenicity166,167. Immune markers such as C-reactive protein (CRP), IL-6, IFN-γ, IP-10, and MCP-2 were associated with systemic symptoms in individuals vaccinated with AS01B—Hepatitis B surface antigen168. Alternative approaches include metabolomics and transcriptomics, which can be used to predict markers of vaccine reactogenicity and accelerate the clinical testing of Q fever candidates169.
Route of administration
C. burnetii whole-cell vaccines have traditionally been administered subcutaneously, and this route may be responsible for reactogenicity, even though it triggered protective immune responses. It would be worthwhile to explore other routes that might enhance or retain immunogenicity while reducing reactogenicity. As with subcutaneous routes, intramuscular routes induce similar responses, but with fewer local reactions109 The intramuscular route proved to be less adverse for whole-cell formulations with alum than the subcutaneous route. The CDC recommends the intramuscular route for inactivated vaccines formulated with adjuvants because it causes less inflammation and granulomas170,171. However, no studies have reported the intramuscular administration of C. burnetii WCVs with adjuvants; hence, the reactogenicity associated with this route remains unclear. Infectious diseases that spread through airborne transmission are well-suited for mucosal vaccines172,173. The induction of mucosal immunity leads to secretory IgA responses that neutralize pathogens at the point of entry173,174. This route has proven effective in subunit CMR vaccines, with no data on reactogenicity175. Depending on the vaccine platform, it is important to choose an ideal route that induces the maximum response without causing local or systemic reactions.
The primary goal is to develop a universal preventative Q fever vaccine. The ideal vaccine to combat this biological warfare agent is one that prevents infection and ultimately disease development. Therefore, a pre-infection vaccine that prevents acute infection and progression to a chronic state should be considered. From an immunological perspective, a pre-infection Q fever vaccine evokes a pre-existing immune response that intervenes in the pathogenesis of C. burnetii that occurs upon exposure. The chronic state of Q fever occurs due to the inability of the immune system to clear C. burnetii76,77. This is probably due to the delayed onset of the T cell response, which is initiated much later owing to the immune evasion mechanisms of C. burnetii5,176. The presence of pre-existing C. burnetii-specific CD4+ T cells, in combination with pre-existing antibodies at the time of exposure is a valid strategy to counteract evasion mechanisms. Additionally, an effective vaccine should evoke an efficacious response that confers protection upon subsequent exposure. To this end, future Q fever vaccine development efforts should consider a prevention of infection vaccine that induces long-lasting and memory immune responses in order to reduce the rate of disease transmission and thus control of disease among populations.
Concluding remarks
Although extensive studies aiming at the development of non-reactogenic Q fever vaccines have been conducted, such a vaccine remains elusive. The current knowledge of immunology underpinning protective immunity against C. burnetii indicates that both humoral and cell-mediated immune responses are required for Q fever prevention. However, there are still certain knowledge gaps that must be addressed with regard to the development of a Q fever vaccine. An in-depth analysis of Q fever prevalence across different populations and regions is crucial to assess heterologous protection against different strains. There is still limited understanding of the pathogenesis and immune mechanisms induced by C. burnetii, which makes it difficult to elucidate correlates of protection required for vaccine development. Identifying optimal antigenic determinants as vaccine targets is central to vaccine discovery, and information in this area remains obscure despite advancements in bioinformatics. Furthermore, to date, no studies have reported the long-term durability and longevity of responses following vaccination. A comprehensive approach to these research questions should provide useful information for precise engineering of future Q fever vaccines.
References
Derrick, E. “Q” fever, a new fever entity: clinical features, diagnosis and laboratory investigation. Med. J. Aust. 2, 281–299 (1937).
Davis, G. E. et al. A filter-passing infectious agent isolated from ticks. Public Health Rep. 53, 2259–2311 (1938).
Cox, H. R. & Beli, E. J. The cultivation of Rickettsia diaporica in tissue culture and in the tissues of developing chick embryos. Public Health Rep. 54, 2171–2178 (1939).
Cutler, S. J. Bacteria: Coxiella burnetii. In Encyclopedia of Food Safety (ed. Motarjemi, Y.) 410–416 (Academic Press, 2014).
Dragan, A. L. & Voth, D. E. Coxiella burnetii: international pathogen of mystery. Microbes Infect. 22, 100–110 (2020).
Ullah, Q. et al. Q fever—a neglected zoonosis. Microorganisms 10, 1530 (2022).
Eldin, C. et al. From Q fever to Coxiella burnetii Infection: a paradigm change. Clin. Microbiol. Rev. 30, 115–190 (2017).
Moos, A. & Hackstadt, T. Comparative virulence of intra-and interstrain lipopolysaccharide variants of Coxiella burnetii in the guinea pig model. Infect. Immun. 55, 1144–1150 (1987).
Million, M. & Raoult, D. Recent advances in the study of Q fever epidemiology, diagnosis and management. J. Infect. 71, S2–S9 (2015).
Gidding, H. F. et al. Seroprevalence of Q fever among metropolitan and non-metropolitan blood donors in New South Wales and Queensland, 2014-2015. Med. J. Aust. 210, 309–315 (2019).
Garner, M. G. et al. A review of Q fever in Australia 1991–1994. Aust. N.Z. J. Public Health 21, 722–730 (1997).
Schimmer, B. et al. Low seroprevalence of Q fever in the Netherlands prior to a series of large outbreaks. Epidemiol. Infect. 140, 27–35 (2012).
Shaw, E. I. & Voth, D. E. Coxiella burnetii: a pathogenic intracellular acidophile. Microbiology 165, 1–3 (2019).
Sireci, G. et al. Recent advances on the innate immune response to Coxiella burnetii. Front. Cell Infect. Microbiol. 11, 754455 (2021).
Park, D. et al. Developmental transitions coordinate assembly of the Coxiella burnetii Dot/Icm type IV secretion system. Infect. Immun. 90, e0041022 (2022).
Andoh, M. et al. Comparative virulence of phase I and II Coxiella burnetii in immunodeficient mice. Ann. N. Y. Acad. Sci. 1063, 167–170 (2005).
Cross, A. R. et al. Spinning sugars in antigen biosynthesis: characterization of the Coxiella burnetii and Streptomyces griseus TDP-sugar epimerases. J. Biol. Chem. 298, 101903 (2022).
Graves, S. R. et al. An O-specific polysaccharide/tetanus toxoid conjugate vaccine induces protection in guinea pigs against virulent challenge with Coxiella burnetii. Vaccines 10, 1393 (2022).
Beare, P. A. et al. Genetic mechanisms of Coxiella burnetii lipopolysaccharide phase variation. PLoS Pathog. 14, e1006922 (2018).
Long, C. M. et al. Contributions of lipopolysaccharide and the type IVB secretion system to Coxiella burnetii vaccine efficacy and reactogenicity. NPJ Vaccines 6, 38 (2021).
Ruiz, S. & Wolfe, D. N. Vaccination against Q fever for biodefense and public health indications. Front. Microbiol. 5, 726 (2014).
Miller, J., Shaw, E. & Thompson, H. Coxiella burnetii, Q fever, and bioterrorism. In Microorganisms and Bioterrorism (eds Anderson, B., Friedman, H. & Bendinelli, M.). 181–208 (Springer, 2006).
Noah, D. L. et al. The history and threat of biological warfare and terrorism. Emerg. Med. Clin. 20, 255–271 (2002).
Burette, M. et al. Modulation of innate immune signaling by a Coxiella burnetii eukaryotic-like effector protein. Proc. Natl Acad. Sci. USA 117, 13708–13718 (2020).
van Schaik, E. J. et al. Molecular pathogenesis of the obligate intracellular bacterium Coxiella burnetii. Nat. Rev. Microbiol. 11, 561–573 (2013).
Voth, D. E. & Heinzen, R. A. Lounging in a lysosome: the intracellular lifestyle of Coxiella burnetii. Cell Microbiol. 9, 829–840 (2007).
Rosales, E. M. et al. Cortactin is involved in the entry of Coxiella burnetii into non-phagocytic cells. PLoS ONE 7, e39348 (2012).
Martinez, E. et al. Identification of OmpA, a Coxiella burnetii protein involved in host cell invasion, by multi-phenotypic high-content screening. PLoS Pathog. 10, e1004013 (2014).
Capo, C. et al. Subversion of monocyte functions by Coxiella burnetii: impairment of the cross-talk between αvβ3 integrin and CR3. J. Immunol. 163, 6078–6085 (1999).
Capo, C. et al. Coxiella burnetii avoids macrophage phagocytosis by interfering with spatial distribution of complement receptor 3. J. Immunol. 170, 4217–4225 (2003).
Waag, D. M. Coxiella burnetii: host and bacterial responses to infection. Vaccine 25, 7288–7295 (2007).
Vishwanath, S. & Hackstadt, T. Lipopolysaccharide phase variation determines the complement-mediated serum susceptibility of Coxiella burnetii. Infect. Immun. 56, 40–44 (1988).
Salinas, R. P. et al. Coxiella burnetii phagocytosis is regulated by GTPases of the Rho family and the RhoA effectors mDia1 and ROCK. PLoS ONE 10, e0145211 (2015).
Kinchen, J. M. & Ravichandran, K. S. Phagosome maturation: going through the acid test. Nat. Rev. Mol. Cell Biol. 9, 781–795 (2008).
Uribe-Querol, E. & Rosales, C. Phagocytosis: our current understanding of a universal biological process. Front. Immunol. 11, 1066 (2020).
Fairn, G. D. & Grinstein, S. How nascent phagosomes mature to become phagolysosomes. Trends Immunol. 33, 397–405 (2012).
Ghigo, E. et al. Coxiella burnetii survival in THP-1 monocytes involves the impairment of phagosome maturation: IFN-gamma mediates its restoration and bacterial killing. J. Immunol. 169, 4488–4495 (2002).
Gutierrez, M. G. et al. Autophagy induction favours the generation and maturation of the Coxiella-replicative vacuoles. Cell Microbiol. 7, 981–993 (2005).
Howe, D. & Heinzen, R. A. Coxiella burnetii inhabits a cholesterol-rich vacuole and influences cellular cholesterol metabolism. Cell Microbiol. 8, 496–507 (2006).
Romano, P. S. et al. The autophagic pathway is actively modulated by phase II Coxiella burnetii to efficiently replicate in the host cell. Cell Microbiol. 9, 891–909 (2007).
Beron, W. et al. Coxiella burnetii localizes in a Rab7-labeled compartment with autophagic characteristics. Infect. Immun. 70, 5816–5821 (2002).
Levine, B., Mizushima, N. & Virgin, H. W. Autophagy in immunity and inflammation. Nature 469, 323–335 (2011).
Kohler, L. J. et al. Effector protein Cig2 decreases host tolerance of infection by directing constitutive fusion of autophagosomes with the coxiella-containing vacuole. mBio 7, e01127-16 (2016).
Mansilla Pareja, M. E. et al. Alterations of the Coxiella burnetii replicative vacuole membrane integrity and interplay with the autophagy pathway. Front. Cell Infect. Microbiol. 7, 112 (2017).
Swanson, M. S. & Fernandez‐Moreia, E. A microbial strategy to multiply in macrophages: the pregnant pause. Traffic 3, 170–177 (2002).
Howe, D. et al. Nitric oxide inhibits Coxiella burnetii replication and parasitophorous vacuole maturation. Infect. Immun. 70, 5140–5147 (2002).
Voth, D. E., Howe, D. & Heinzen, R. A. Coxiella burnetii inhibits apoptosis in human THP-1 cells and monkey primary alveolar macrophages. Infect. Immun. 75, 4263–4271 (2007).
Voth, D. E. & Heinzen, R. A. Sustained activation of Akt and Erk1/2 is required for Coxiella burnetii antiapoptotic activity. Infect. Immun. 77, 205–213 (2009).
Zhang, Y. et al. Coxiella burnetii induces apoptosis during early stage infection via a caspase-independent pathway in human monocytic THP-1 cells. PLoS ONE 7, e30841 (2012).
Ganesan, S. et al. Syntaxin 11 contributes to the interferon-inducible restriction of Coxiella burnetii intracellular infection. Mbio 14, e03545-22 (2023).
Peters, N. C., Khan, N. & Mody, C. H. Novel approaches to preventing phagosomal infections: timing is key. Trends Immunol. 44, 22–31 (2022).
Rayamajhee, B. et al. Acanthamoeba, an environmental phagocyte enhancing survival and transmission of human pathogens. Trends Parasitol. 38, 975–990 (2022).
Fisher, J. R. et al. Pattern recognition receptors in innate immunity to obligate intracellular bacteria. Zoonoses 1, 10 (2021).
Benoit, M., Desnues, B. & Mege, J. L. Macrophage polarization in bacterial infections. J. Immunol. 181, 3733–3739 (2008).
Ka, M. B. et al. Phenotypic diversity and emerging new tools to study macrophage activation in bacterial infectious diseases. Front. Immunol. 5, 500 (2014).
Rath, M. et al. Metabolism via arginase or nitric oxide synthase: two competing arginine pathways in macrophages. Front. Immunol. 5, 532 (2014).
Savill, J. et al. A blast from the past: clearance of apoptotic cells regulates immune responses. Nat. Rev. Immunol. 2, 965–975 (2002).
Benoit, M. et al. The uptake of apoptotic cells drives Coxiella burnetii replication and macrophage polarization: a model for Q fever endocarditis. PLoS Pathog. 4, e1000066 (2008).
Kishimoto, R. et al. Cell-mediated immune responses of guinea pigs to an inactivated phase I Coxiella burnetii vaccine. Infect. Immun. 19, 194–198 (1978).
Muntjewerff, E. M., Meesters, L. D. & van den Bogaart, G. Antigen cross-presentation by macrophages. Front. Immunol. 11, 1276 (2020).
Buttrum, L. et al. Both major histocompatibility complex class I (MHC-I) and MHC-II molecules are required, while MHC-I appears to play a critical role in host defense against primary Coxiella burnetii infection. Infect. Immun. 86, e00602-17 (2018).
Meghari, S. et al. TLR2 is necessary to inflammatory response in Coxiella burnetii infection. Ann. N. Y. Acad. Sci. 1063, 161–166 (2005).
Arango Duque, G. & Descoteaux, A. Macrophage cytokines: involvement in immunity and infectious diseases. Front. Immunol. 5, 491 (2014).
Elliott, A., Peng, Y. & Zhang, G. Coxiella burnetii interaction with neutrophils and macrophages in vitro and in SCID mice following aerosol infection. Infect. Immun. 81, 4604–4614 (2013).
Elliott, A. et al. Neutrophils play an important role in protective immunity against Coxiella burnetii infection. Infect. Immun. 83, 3104–3113 (2015).
Chen, C. et al. Chemokine receptor 7 is essential for Coxiella burnetii whole-cell vaccine-induced cellular immunity but dispensable for vaccine-mediated protective immunity. J. Infect. Dis. 220, 624–634 (2019).
Shannon, J. G., Howe, D. & Heinzen, R. A. Virulent Coxiella burnetii does not activate human dendritic cells: role of lipopolysaccharide as a shielding molecule. Proc. Natl Acad. Sci. 102, 8722–8727 (2005).
Gorvel, L. et al. Intracellular bacteria interfere with dendritic cell functions: role of the type I interferon pathway. PLoS ONE 9, e99420 (2014).
Matthiesen, S. et al. TGF-β/IFN-γ antagonism in subversion and self-defense of phase II Coxiella burnetii-infected dendritic cells. Infect. Immun. 91, e00323-22 (2023).
Boullart, A. C. et al. Maturation of monocyte-derived dendritic cells with Toll-like receptor 3 and 7/8 ligands combined with prostaglandin E2 results in high interleukin-12 production and cell migration. Cancer Immunol. Immunother. 57, 1589–1597 (2008).
Leon, B. & Lund, F. E. Compartmentalization of dendritic cell and T-cell interactions in the lymph node: anatomy of T-cell fate decisions. Immunol. Rev. 289, 84–100 (2019).
Wei, Y. et al. Coxiella burnetii antigen-stimulated dendritic cells mediated protection against Coxiella burnetii in BALB/c mice. J. Infect. Dis. 203, 283–291 (2011).
Lazarevic, V., Glimcher, L. H. & Lord, G. M. T-bet: a bridge between innate and adaptive immunity. Nat. Rev. Immunol. 13, 777–789 (2013).
Mezouar, S. et al. T-Bet controls susceptibility of mice to Coxiella burnetii infection. Front. Microbiol 11, 1546 (2020).
Ledbetter, L. et al. Major histocompatibility complex class II-Restricted, CD4+ T cell-dependent and-independent mechanisms are required for vaccine-induced protective immunity against Coxiella burnetii. Infect. Immun. 88, e00824-19 (2020).
Andoh, M. et al. T cells are essential for bacterial clearance, and gamma interferon, tumor necrosis factor alpha, and B cells are crucial for disease development in Coxiella burnetii infection in mice. Infect. Immun. 75, 3245–3255 (2007).
Read, A. J., Erickson, S. & Harmsen, A. G. Role of CD4+ and CD8+ T cells in clearance of primary pulmonary infection with Coxiella burnetii. Infect. Immun. 78, 3019–3026 (2010).
Zhang, G. et al. Mechanisms of vaccine-induced protective immunity against Coxiella burnetii infection in BALB/c mice. J. Immunol. 179, 8372–8380 (2007).
Nash, A. A., Dalziel, R. G. & Fitzgerald, J. R. Early stages of infection after pathogen entry. In Mims’ Pathogenesis of Infectious Disease (ed. Fitzgerald, J. R.) 51–65 (Academic Press, 2015).
Izzo, A., Marmion, B. & Hackstadt, T. Analysis of the cells involved in the lymphoproliferative response to Coxiella burnetii antigens. Clin. Exp. Immunol. 85, 98–108 (1991).
Sluder, A. E. et al. Evaluation of a human T cell-targeted multi-epitope vaccine for Q fever in animal models of Coxiella burnetii immunity. Front. Immunol. 13, 901372 (2022).
Dresler, J. et al. Quantitative proteome profiling of Coxiella burnetii reveals major metabolic and stress differences under axenic and cell culture cultivation. Front. Microbiol. 10, 2022 (2019).
Brennan, R. E. et al. Both inducible nitric oxide synthase and NADPH oxidase contribute to the control of virulent phase I Coxiella burnetii infections. Infect. Immun. 72, 6666–6675 (2004).
Casadevall, A. & Pirofski, L.-A. Antibody-mediated regulation of cellular immunity and the inflammatory response. Trends Immunol. 24, 474–478 (2003).
Casadevall, A. & Pirofski, L. A. A reappraisal of humoral immunity based on mechanisms of antibody‐mediated protection against intracellular pathogens. Adv. Immunol. 91, 1–44 (2006).
Zhang, G. et al. Formalin-inactivated Coxiella burnetii phase I vaccine-induced protection depends on B cells to produce protective IgM and IgG. Infect. Immun. 81, 2112–2122 (2013).
Shannon, J. G. et al. Antibody-mediated immunity to the obligate intracellular bacterial pathogen Coxiella burnetii is Fc receptor- and complement-independent. BMC Immunol. 10, 26 (2009).
Hinrichs, D. J. & Jerrells, T. R. In vitro evaluation of immunity to Coxiella burnetii. J. Immunol. 117, 996–1003 (1976).
Schoenlaub, L. et al. Role of B cells in host defense against primary Coxiella burnetii infection. Infect. Immun. 83, 4826–4836 (2015).
Robinson, D. M. & Hasty, S. E. Production of a potent vaccine from the attenuated M-44 strain of Coxiella burneti. Appl. Microbiol. 27, 777–783 (1974).
Genig, V. et al. Experience on the mass immunization of humans with the M-44 live vaccine against Q-fever. I. Subcutaneous method of immunization. Vopr. Virusol. 3, 319–323 (1966).
Johnson, J. W. et al. Lesions in guinea pigs infected with Coxiella burnetii strain M-44. J. Infect. Dis. 135, 995–998 (1977).
Kumaresan, V. et al. The feasibility of using Coxiella burnetii avirulent nine mile phase II viable bacteria as a live attenuated vaccine against Q fever. Front. Immunol. 12, 754690 (2021).
Smadel, J. E., Snyder, M. J. & Robbins, F. C. Vaccination against Q fever. Am. J. Hyg. 47, 71–81 (1948).
Marmion, B. et al. Vaccine prophylaxis of abattoir-associated Q fever: eight years’ experience in Australian abattoirs. Epidemiol. Infect. 104, 275–287 (1990).
Marmion, B. et al. Vaccine prophylaxis of abattoir-associated Q fever. Lancet 324, 1411–1414 (1984).
Ackland, J. R., Worswick, D. A. & Marmion, B. P. Vaccine prophylaxis of Q fever: a follow‐up study of the efficacy of Q‐Vax (CSL) 1985‐1990. Med. J. Aust. 160, 704–708 (1994).
Sellens, E. et al. Frequency of adverse events following Q fever immunisation in young adults. Vaccines 6, 83 (2018).
Bell, J. F. et al. Recurrent reaction at site of Q fever vaccination in a sensitized person. Mil. Med. 129, 591–595 (1964).
Schoffelen, T. et al. Adverse events and association with age, sex and immunological parameters of Q fever vaccination in patients at risk for chronic Q fever in the Netherlands 2011. Vaccine 32, 6622–6630 (2014).
Fratzke, A. P. et al. Coxiella burnetii whole cell vaccine produces a Th1 delayed-type hypersensitivity response in a novel sensitized mouse model. Front. Immunol. 12, 754712 (2021).
Kazar, J. et al. Immunogenicity and reactogenicity of a Q fever chemovaccine in persons professionally exposed to Q fever in Czechoslovakia. Bull. World Health Organ. 60, 389 (1982).
Williams, J. C. et al. Vaccines against coxiellosis and Q fever. Development of a chloroform:methanol residue subunit of phase I Coxiella burnetti for the immunization of animals. Ann. N. Y. Acad. Sci. 653, 88–111 (1992).
Waag, D. M. et al. Comparative efficacy and immunogenicity of Q fever chloroform: methanol residue (CMR) and phase I cellular (Q-Vax) vaccines in cynomolgus monkeys challenged by aerosol. Vaccine 20, 2623–2634 (2002).
Waag, D. M., England, M. J. & Pitt, M. L. M. Comparative efficacy of a Coxiella burnetii chloroform: methanol residue (CMR) vaccine and a licensed cellular vaccine (Q-Vax) in rodents challenged by aerosol. Vaccine 15, 1779–1783 (1997).
Fries, L., Waag, D. & Williams, J. Safety and immunogenicity in human volunteers of a chloroform-methanol residue vaccine for Q fever. Infect. Immun. 61, 1251–1258 (1993).
Anacker, R. et al. Conversion of the phase I antigen of Coxiella burnetii to hapten by phenol treatment. J. Bacteriol. 85, 1165–1170 (1963).
Gregory, A. E. et al. Soluble antigens derived from Coxiella burnetii elicit protective immunity in three animal models without inducing hypersensitivity. Cell Rep. Med. 2, 100461 (2021).
Herve, C. et al. The how’s and what’s of vaccine reactogenicity. npj Vaccines 4, 39 (2019).
McNeil, M. M. & DeStefano, F. Vaccine-associated hypersensitivity. J. Allergy Clin. Immunol. 141, 463–472 (2018).
Fratzke, A. P., van Schaik, E. J. & Samuel, J. E. Immunogenicity and reactogenicity in Q fever vaccine development. Front. Immunol. 13, 886810 (2022).
Heidary, M. et al. A comprehensive review of the protein subunit vaccines against COVID-19. Front. Microbiol. 13, 927306 (2022).
Moyle, P. M. & Toth, I. Modern subunit vaccines: development, components, and research opportunities. ChemMedChem 8, 360–376 (2013).
Vartak, A. & Sucheck, S. J. Recent advances in subunit vaccine carriers. Vaccines 4, 12 (2016).
Chen, S. et al. Precision-engineering of subunit vaccine particles for prevention of infectious diseases. Front. Immunol. 14, 1131057 (2023).
Gilkes, A. P. et al. Tuning subunit vaccines with novel TLR triagonist adjuvants to generate protective immune responses against Coxiella burnetii. J. Immunol. 204, 611–621 (2020).
Fratzke, A. P. et al. Subunit vaccines using TLR triagonist combination adjuvants provide protection against Coxiella burnetii while minimizing reactogenic responses. Front. Immunol. 12, 653092 (2021).
Peng, Y. et al. Development of a lipopolysaccharide-targeted peptide mimic vaccine against Q fever. J. Immunol. 189, 4909–4920 (2012).
Feng, Y. et al. DEC-205 receptor targeted poly(lactic-co-glycolic acid) nanoparticles containing Eucommia ulmoides polysaccharide enhances the immune response of foot-and-mouth disease vaccine in mice. Int. J. Biol. Macromol. 227, 576–589 (2023).
Belz, G. T. et al. CD8alpha+ dendritic cells selectively present MHC class I-restricted noncytolytic viral and intracellular bacterial antigens in vivo. J. Immunol. 175, 196–200 (2005).
Schreibelt, G. et al. The C-type lectin receptor CLEC9A mediates antigen uptake and (cross-)presentation by human blood BDCA3+ myeloid dendritic cells. Blood 119, 2284–2292 (2012).
Ceglia, V. et al. Anti-CD40 antibody fused to CD40 ligand is a superagonist platform for adjuvant intrinsic DC-targeting vaccines. Front. Immunol. 12, 786144 (2021).
Ong, G. H. et al. Exploration of pattern recognition receptor agonists as candidate adjuvants. Front. Cell Infect. Microbiol. 11, 745016 (2021).
Kaur, A. et al. Toll-like receptor (TLR) agonists as a driving force behind next-generation vaccine adjuvants and cancer therapeutics. Curr. Opin. Chem. Biol. 70, 102172 (2022).
Alpatova, N. A. et al. Adjuvant properties of cytokines in vaccination (Review). Pharm. Chem. J. 53, 991–996 (2020).
Zhao, H. et al. Chitosan nanovaccines as efficient carrier adjuvant system for IL-12 with enhanced protection against HBV. Int. J. Nanomed. 16, 4913–4928 (2021).
Mesin, L. et al. Restricted clonality and limited germinal center reentry characterize memory B cell reactivation by boosting. Cell 180, 92–106.e11 (2020).
Laidlaw, B. J. & Ellebedy, A. H. The germinal centre B cell response to SARS-CoV-2. Nat. Rev. Immunol. 22, 7–18 (2022).
Zhang, Y. et al. Recycling of memory B cells between germinal center and lymph node subcapsular sinus supports affinity maturation to antigenic drift. Nat. Commun. 13, 2460 (2022).
Moran, I. et al. Memory B cells are reactivated in subcapsular proliferative foci of lymph nodes. Nat. Commun. 9, 3372 (2018).
Lindquist, R. L. et al. Visualizing dendritic cell networks in vivo. Nat. Immunol. 5, 1243–50 (2004).
Carrasco, Y. R. & Batista, F. D. B cells acquire particulate antigen in a macrophage-rich area at the boundary between the follicle and the subcapsular sinus of the lymph node. Immunity 27, 160–171 (2007).
Hinke, D. M. et al. Antigen bivalency of antigen-presenting cell-targeted vaccines increases B cell responses. Cell Rep. 39, 110901 (2022).
Kato, Y. et al. Multifaceted effects of antigen valency on B cell response composition and differentiation in vivo. Immunity 53, 548–563.e8 (2020).
Volkmann, C. et al. Molecular requirements of the B-cell antigen receptor for sensing monovalent antigens. EMBO J. 35, 2371–2381 (2016).
Chen, S. et al. Ambient temperature stable, scalable COVID-19 polymer particle vaccines induce protective immunity. Adv. Health. Mater. 11, e2102089 (2022).
Chen, S. et al. Assembly of immunogenic protein particles toward advanced synthetic vaccines. Small 19, e2205819 (2022).
Luo, W. & Yin, Q. B cell response to vaccination. Immunol. Invest. 50, 780–801 (2021).
Tokatlian, T. et al. Innate immune recognition of glycans targets HIV nanoparticle immunogens to germinal centers. Science 363, 649–654 (2019).
Singh, A. Eliciting B cell immunity against infectious diseases using nanovaccines. Nat. Nanotechnol. 16, 16–24 (2021).
This, S. et al. What’s self got to do with it: sources of heterogeneity among naive T cells. Semin. Immunol. 65, 101702 (2023).
van Gisbergen, K. & Gerlach, C. No-shows in T-cell responses are frequent for clones of low T-cell receptor affinity. Eur. J. Immunol. 53, e2250305 (2023).
Kaech, S. M., Wherry, E. J. & Ahmed, R. Effector and memory T-cell differentiation: implications for vaccine development. Nat. Rev. Immunol. 2, 251–262 (2002).
González-Miró, M. et al. Design and biological assembly of polyester beads displaying pneumococcal antigens as particulate vaccine. ACS Biomater. Sci. Eng. 4, 3413–3424 (2018).
Gonzaga, Z. J. C., Zhang, J. & Rehm, B. H. Intranasal delivery of antigen-coated polymer particles protects against Pseudomonas aeruginosa infection. ACS Infect. Dis. 8, 744–756 (2022).
Teng, Z. et al. Bridging nanoplatform and vaccine delivery, a landscape of strategy to enhance nasal immunity. J. Control Release 351, 456–475 (2022).
Su, F. et al. Induction of mucosal immunity through systemic immunization: phantom or reality? Hum. Vaccin. Immunother. 12, 1070–1079 (2016).
Vigil, A. et al. Profiling the humoral immune response of acute and chronic Q fever by protein microarray. Mol. Cell Proteom. 10, M110.006304 (2011).
Jiao, J. et al. Serological characterization of surface-exposed proteins of Coxiella burnetii. Microbiology 160, 2718–2731 (2014).
Beare, P. A. et al. Candidate antigens for Q fever serodiagnosis revealed by immunoscreening of a Coxiella burnetii protein microarray. Clin. Vaccin. Immunol. 15, 1771–1779 (2008).
Xiong, X. et al. Potential serodiagnostic markers for Q fever identified in Coxiella burnetii by immunoproteomic and protein microarray approaches. BMC Microbiol. 12, 35 (2012).
Vigil, A. et al. Genome-wide profiling of humoral immune response to Coxiella burnetii infection by protein microarray. Proteomics 10, 2259–2269 (2010).
Scholzen, A. et al. Promiscuous Coxiella burnetii CD4 epitope clusters associated with human recall responses are candidates for a novel T-cell targeted multi-epitope Q fever vaccine. Front. Immunol. 10, 207 (2019).
Scholzen, A. et al. Coxiella burnetii epitope-specific T-cell responses in patients with chronic Q fever. Infect. Immun. 87, e00213-19 (2019).
Xiong, X. et al. Exploratory study on Th1 epitope-induced protective immunity against Coxiella burnetii infection. PLoS ONE 9, e87206 (2014).
Dold, C. et al. Immunisation with purified Coxiella burnetii phase I lipopolysaccharide confers partial protection in mice independently of co-administered adenovirus vectored vaccines. Vaccine 41, 3047–3057 (2023).
Xiong, X. et al. Identification of Coxiella burnetii CD8+ T-cell epitopes and delivery by attenuated listeria monocytogenes as a vaccine vector in a C57BL/6 mouse model. J. Infect. Dis. 215, 1580–1589 (2017).
Bachmann, M. F. & Jennings, G. T. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nat. Rev. Immunol. 10, 787–796 (2010).
Wibowo, D. et al. Polymeric nanoparticle vaccines to combat emerging and pandemic threats. Biomaterials 268, 120597 (2021).
Baranov, M. V. et al. Modulation of immune responses by particle size and shape. Front. Immunol. 11, 607945 (2020).
Chen, S. et al. Particulate mycobacterial vaccines induce protective immunity against tuberculosis in mice. Nanomaterials 11, 2060 (2021).
Chen, S. et al. Innovative antigen carrier system for the development of tuberculosis vaccines. FASEB J. 33, 7505–7518 (2019).
Tesfamariam, M., Binette, P. & Long, C. M. Preclinical animal models for Q fever vaccine development. Front. Cell Infect. Microbiol. 12, 828784 (2022).
Norville, I. H. et al. Galleria mellonella as an alternative model of Coxiella burnetii infection. Microbiology 160, 1175–1181 (2014).
Arras, M. et al. Multiparameter telemetry as a sensitive screening method to detect vaccine reactogenicity in mice. PLoS ONE 7, e29726 (2012).
Weiner, J. et al. Characterization of potential biomarkers of reactogenicity of licensed antiviral vaccines: randomized controlled clinical trials conducted by the BIOVACSAFE consortium. Sci. Rep. 9, 20362 (2019).
Chan, C. Y. et al. Early molecular correlates of adverse events following yellow fever vaccination. JCI Insight 2, e96031 (2017).
Burny, W. et al. Inflammatory parameters associated with systemic reactogenicity following vaccination with adjuvanted hepatitis B vaccines in humans. Vaccine 37, 2004–2015 (2019).
Gonzalez-Dias, P. et al. Methods for predicting vaccine immunogenicity and reactogenicity. Hum. Vaccin. Immunother. 16, 269–276 (2020).
Zhang, L., Wang, W. & Wang, S. Effect of vaccine administration modality on immunogenicity and efficacy. Expert Rev. Vaccines 14, 1509–23 (2015).
Frieden, T. R. Public health then and now: celebrating 50 years of MMWR at CDC: foreward. (2011).
Holmgren, J. & Czerkinsky, C. Mucosal immunity and vaccines. Nat. Med. 11, S45–S53 (2005).
Mettelman, R. C., Allen, E. K. & Thomas, P. G. Mucosal immune responses to infection and vaccination in the respiratory tract. Immunity 55, 749–780 (2022).
Price, G. E. et al. Mucosal immunization with a candidate universal influenza vaccine reduces virus transmission in a mouse model. J. Virol. 88, 6019–6030 (2014).
Feng, J. et al. Enhanced protection against Q fever in BALB/c mice elicited by immunization of chloroform-methanol residue of Coxiella burnetii via intratracheal inoculation. Vaccine 37, 6076–6084 (2019).
Benoit, M. et al. Coxiella burnetii, the agent of Q fever, stimulates an atypical M2 activation program in human macrophages. Eur. J. Immunol. 38, 1065–70 (2008).
Williams-Macdonald, S. E. et al. Efficacy of phase I and phase II Coxiella burnetii bacterin vaccines in a pregnant Ewe challenge model. Vaccines 11, 511 (2023).
Tomaiuolo, S. et al. QuilA(R) adjuvanted Coxevac(R) sustains Th1-CD8(+)-type immunity and increases protection in Coxiella burnetii-challenged goats. npj Vaccines 8, 17 (2023).
Waag, D. M. et al. Low-dose priming before vaccination with the phase I chloroform-methanol residue vaccine against Q fever enhances humoral and cellular immune responses to Coxiella burnetii. Clin. Vaccin. Immunol. 15, 1505–1512 (2008).
Acknowledgements
This work is supported by the Griffith Institute for Drug Discovery, Griffith University (Australia) and the Centre for Cell Factories and Biopolymers, Griffith University (Australia) and the Australian Rickettsial Reference Laboratory (Australia). B.H.A.R. acknowledges financial support from awards of the Australian Research Council (ARC) Discovery Projects (DP200100874 and DP220102236) and the ARC Linkage Infrastructure, Equipment and Facilities (LE200100140). All figures were created using Biorender.com.
Author information
Authors and Affiliations
Contributions
G.S. and B.H.A.R. wrote the manuscript, J.S. and S.R.G. edited and provided feedback.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sam, G., Stenos, J., Graves, S.R. et al. Q fever immunology: the quest for a safe and effective vaccine. npj Vaccines 8, 133 (2023). https://doi.org/10.1038/s41541-023-00727-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-023-00727-6