Abstract
There is substantial cognitive heterogeneity among patients with schizophrenia (SZ) and bipolar disorders (BD). More knowledge about the magnitude and clinical correlates of performance variability could improve our understanding of cognitive impairments. Using double generalized linear models (DGLMs) we investigated cognitive mean and variability differences between patients with SZ (n = 905) and BD spectrum disorders (n = 522), and healthy controls (HC, n = 1170) on twenty-two variables. The analysis revealed significant case-control differences on 90% of the variables. Compared to HC, patients showed larger intra-individual (within subject) variability across tests and larger inter-individual (between subject) variability in measures of fine-motor speed, mental processing speed, and inhibitory control (SZ and BD), and in verbal learning and memory and intellectual functioning (SZ). In SZ, we found that lager intra -and inter (on inhibitory control and speed functions) individual variability, was associated with lower functioning and more negative symptoms. Inter-individual variability on single measures of memory and intellectual function was additionally associated with disorganized and positive symptoms, and use of antidepressants. In BD, there were no within-subject associations with symptom severity. However, greater inter-individual variability (primarily on inhibitory control and speeded functions) was associated with lower functioning, more negative -and disorganized symptoms, earlier age at onset, longer duration of illness, and increased medication use. These results highlight larger individual differences in patients compared to controls on various cognitive domains. Further investigations of the causes and correlates of individual differences in cognitive function are warranted.
Similar content being viewed by others
Introduction
Cognitive dysfunction is a central feature of psychotic disorders. In schizophrenia (SZ), group-level performance within key cognitive domains has been reported to be 1-2 standard deviations (SD) below the healthy population1. The clinical relevance of cognitive functioning is considerable, and impaired cognition is associated with poor response to treatment, difficulties with social relationships and occupational functioning2. Patients with bipolar disorder (BD) show intermediate group level cognitive dysfunction compared to SZ and healthy controls3. Despite better performance compared to SZ, the pattern of cognitive profiles is similar and are associated with functional outcome also in BD4.
Cognitive deficits are often present from illness onset5 and remain relatively stable throughout the course of the illness6, implicating neurodevelopmental processes in both disorders5. Studies also show overlap in symptom dimensions7, genetic lability8, and brain morphology9, suggesting a continuum and common pathophysiological mechanisms across psychotic disorders. Still, the association between cognitive impairments and genetic risk appears to be somewhat different in the two disorders. While most risk alleles related to SZ also are associated with lower intelligence and neurodevelopmental processes, BD risk alleles are related to both higher and lower intelligence (although more to higher than lower)10.
Most individuals vary in their cognitive performance from one test to another, but also show some consistency in their responses. In SZ and BD, intra-individual responses on cognitive tasks are more variable, and mean differences are often accompanied by considerable inter-individual differences on the group level11. Previous studies have attempted to parse this cognitive variability by identifying patient sub-groups with differentially affected neurobiology and clinical and cognitive profiles11,12,13. Cognitive variability could reflect differential sensitivity to illness related processes, including clinical developmental paths and vulnerability to environmental factors and genetic susceptibility. Furthermore, cognitive domains show differential trajectories through the lifespan14. Complex executive functions, including fluid skills, show protracted development through early adulthood. Processing speed peaks in the early twenties and thereafter steadily declines. Working memory performance is relatively stable in the twenties and starts to decline in the early thirties, while inhibitory control declines from the mid-thirties. Other functions involving acquired knowledge (such as intellectual functioning) continue to improve into middle age and senescence. Consequently, the individual pattern of cognitive dysfunctions is likely to reflect the age period in which a patient experiences illness.
Neuroimaging has revealed case-control differences in several brain structural characteristics in severe mental disorders15,16, but the individual differences are substantial17 and the anatomical overlap is low18, suggesting that group-level differences may disguise considerable heterogeneity, with clinical relevance. Although substantial individual differences in cognitive function among patients with SZ and BD have been shown, there is a lack of studies simultaneously investigating differences within (intra-individual) and between individuals (inter-individual) on single tests. This is important since cognitive sub-domains showing homogeneous deficits could reflect common pathological features. Higher heterogeneity in patients on the other hand, could indicate disease subtypes or cognitive domains that are particularly sensitive to individual trajectories, and to illness and environmental perturbations19. Although previous studies often show lager standard deviations around the means on cognitive tests in SZ and BD compared to HC3,20, no one has explicitly tested the variability difference between these populations previously. Some tests or functions may be more sensitive to variability differences than others. Accordingly, quantifying performance variability is important to identify common mechanisms of cognitive dysfunction and to detect markers of cognitive subtypes17,19.
The aim of the current study was to test for mean and variability (intra -and inter-individual) differences between patients with SZ and BD spectrum disorders and HC within several cognitive domains. Intra-individual variability reflects the individual standard deviation of variation across cognitive tests. Inter-individual variability reflects the average deviation from the group-level predicted mean value or slope on a single test. Here the extent of variability in patients compared to HC can be interpreted as reflecting level of performance heterogeneity in the relevant cognitive domain. Using double generalized linear models (DGLM), which allows for simultaneous modeling of the mean and the variance, we investigated whether patients with severe mental disorders show higher or lower variability at the group-level compared to HC. Further, we investigated whether the magnitude of variability in cognitive performance is related to clinical severity, i.e. if the range of performance is associated with illness severity in the patient group.
Based on studies reviewed above3,19, we hypothesized that patients with SZ would show lower mean performance compared to HC but display larger variability. Based on Vaskinn and colleagues12, we anticipated a similar pattern but of smaller magnitude in BD when compared to HC. Since cognitive heterogeneity has been linked to clinical characteristics12,21, we further hypothesized that larger variability in performance among patients would be associated with higher clinical severity, age at onset and duration of illness.
Results
Demographic, clinical and cognitive characteristics
Sample characteristics are summarized in Table 1. In brief, patients with BD and HC were older than SZ patients. There was a higher proportion of females in the BD group and males in the SZ group. Furthermore, the HC group had significantly longer education and higher intellectual functioning compared to both patient groups, while BD patients had more education and higher intellectual functioning compared to the SZ group. As reported earlier in a subsample of the presented data (Vaskinn et al., 2020), patients with SZ presented with more positive, negative, disorganized and excited symptoms, worse psychosocial functioning (GAF-S,GAF-F, SFS) and reported higher drug use than patients with BD, while the BD group reported higher alcohol consumption than the SZ and HC groups.
Mean and variability differences
Mean and variability (dispersion) differences for all groups are summarized in Table 2 and Fig. 1. Compared to HC, patients with SZ had significantly lower mean scores across most cognitive measures. Patients with SZ also had significantly larger intra-individual variability compared to HC. Furthermore, DGLM revealed significantly larger inter-individual variability among patients with SZ compared to HC on measures of intellectual functioning, mental processing speed, learning and memory, inhibitory control fine-motor speed, and the cognitive composite score (Fig. 2). Additionally, SZ displayed larger dispersion on the intra-individual variability score compared to HC, indicating increased between subject variability for SZ compared to HC, in the 90th percentile (supplementary). The model revealed no significant inter-individual variability differences in psychomotor processing speed, semantic fluency, working memory, or on two measures of verbal learning and memory.
Presented are effect sizes (beta values, standardized regression coefficients) for significant (Bonferroni corrected (α = 0.05/48 tests = p < 0.000104)) mean and variability (dispersion) differences between groups across all cognitive tests, adjusted for age and sex. The more negative beta value the poorer the patient group performed compared to HC and more positive beta values indicate increased dispersion in patients compared to HC. Note, NDH Non-Dominant Hand, DH Dominant Hand, HC Healthy controls, SZ Schizophrenia, BD Bipolar disorder.
A Marginal distributions of z-normalized cognitive scores in SZ and HC (adjusted for age and sex) for Inhibition (the remaining tests distributions are presented in the online supplement). The black vertical lines show deciles in each group, and the orange lines indicate decile-matched differences (shifts) between the two distributions. B Case-control difference plotted as a function of the distribution among HC. A sloped line indicates different dispersions for the two groups, beyond a simple mean shift. Number in the orange boxes indicate the case-control difference (z-scores) for the corresponding deciles within each group. The largest case-control differences are found in the lower deciles indicating a longer tail for lower performance individuals for patients compared to controls, with 4.4 times larger case-control difference in performance at the 10th percentile of the distribution for inhibitory control compared to the 90th percentile. SZ Schizophrenia, HC healthy controls.
Compared to HC, patients with BD showed significantly lower mean scores on most measures with the exception of premorbid intellectual functioning and two measures of verbal learning and memory. Patients with BD also displayed significantly larger intra-individual variability compared to HC. Further, the model predicted significantly larger inter-individual variability among patients with BD compared to HC on one measure of mental processing speed, in inhibitory control, fine-motor speed, and on the cognitive composite score. There was also a significant difference in dispersion on the intra-individual variability score, where BD (like SZ), displayed larger between-subject variation at the higher end of within-subject variability compared to HC. There were no significant dispersion differences in intellectual functioning, psychomotor processing speed, verbal learning and memory, semantic fluency, or on any of the working memory measures.
Lastly, compared to BD, patients with SZ displayed significantly lower mean cognitive performance on all measures except one measure of verbal learning and inhibitory control, and two measures of working memory. Moreover, SZ had significantly larger intra-individual variability across tests compared to BD and larger inter-individual variability on the composite score. There were however no significant inter-individual variability differences on any of the other cognitive measures between these groups.
Associations between symptoms and variability in cognitive performance
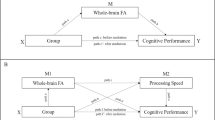
Figure 3A, B summarizes results from DGLMS testing for associations between clinical symptoms and intra -and inter-individual variability in test performance. Among patients with SZ, GAF-S and GAF-F scores were negatively associated and PANSS negative symptoms positively associated with intra-individual variability, indicating larger individual variation in test performance among patients with lower function and more negative symptoms. Regarding between subject variation on single domains/tests, GAF-S and GAF-F were similarly negatively associated with inter-individual variability in inhibitory control, GAF (S/F) and SFS were negatively associated with inter-individual variability in mental processing speed, while GAF-F was negatively associated with inter-individual variability on memory and fine-motor speed, also indicating larger between subject differences among patients with lower function on these particular domains. Furthermore, PANSS negative symptoms were positively associated with inter-individual variability in measures of inhibitory control, fine-motor speed, and mental processing speed, indicating higher more variable performance for these cognitive functions for patients with more negative symptoms. Lastly, disorganized symptoms were positively associated with inter-individual variability on measures of inhibitory control, memory and intellectual functioning, and the use of antidepressant medication was positively associated inter-variability in memory, indicating that increasing disorganized symptoms and use of antidepressant medication, are related to the larger variance found in these domains.
Shows the associations between clinical characteristics and cognitive dispersion in schizophrenia (A) and bipolar (B) spectrum disorders, respectively. Each cell represents a DGLM dispersion effect, showing how clinical severity scores are associated with intra and inter-individual variability in cognition. Orange/red colors indicate positive associations and blue colors indicate negative associations. Note, AAO Age at onset, PANSS Positive and Negative Syndrome Scale, GAF Global Assessment of Functioning scale, YMRS Young Mania Rating Scale, DOI Duration of illness, DUP Duration of untreated psychosis, AUDIT/DUDIT Alcohol/Drug Use Disorder Identification Tests.
In summary, the results indicate larger variability (both within and between patients) in cognitive function among SZ patients with more severe compared to less severe clinical burden.
Among patients with BD, SFS and GAF (S/F) were negatively associated with inter-individual variability in measures of inhibitory control and mental processing speed. Additionally, GAF-F was negatively associated with overall cognitive functioning (cognitive composite). These results indicate that poorer social and global functioning is related to larger between-subject variability in these functions.
Furthermore, use of antipsychotic medications and total medication use were positively associated with inter-individual variability in fine-motor speed as well as in premorbid functioning, indicating that higher medication use is related to higher motor variability and more variable premorbid intellectual functioning. Also, there were negative associations between inter-individual variability in working memory and use of antipsychotic medications and between a measure of verbal learning and drug use, possibly reflecting that participants with higher drug use or using more antipsychotic medication, when considered jointly, are cognitively more homogeneous.
Regarding predicted variability on the inhibitory control function, disorganized symptoms and DOI were positively associated, and AAO was negatively associated with inter-individual variability in this function, indicating larger individual differences in inhibitory control among patients with early onset, longer duration of illness and more disorganized symptoms.
There were no associations between intra-individual variability in cognitive function and clinical symptoms.
Discussion
The main finding of the present study was distinct patterns of significant mean and variability differences in cognitive domains in SZ and BD spectrum disorders compared to HC. We found larger intra-individual variability in patients with SZ and BD compared to HC, and in SZ compared to BD, when investigating the within-subject SD across cognitive performance scores. Further, we found larger inter-individual variability in several cognitive measures among patients with SZ and BD compared to HC. Specifically, we found larger inter-individual variability in measures of intellectual functioning, mental processing speed, verbal learning and memory, inhibitory control, and in fine-motor speed function, in SZ compared to HC, partly in agreement with our hypothesis. Among patients with BD, we found larger inter-variability in one measure of mental processing speed (color naming), in measures of inhibitory control and in fine-motor speed function compared to HC. There were no differences in inter-subject variability in any of the cognitive tests between the two patient groups. However, on the cognitive composite score patients with SZ had larger inter-individual variability compared to BD patients. We also replicated previous findings of lower mean cognitive scores across most tasks in SZ and BD compared to HC3, and in SZ compared to BD5.
Although, previous studies have shown that patients are less stable in their individual performance, to our knowledge, no studies have systematically investigated and shown that both within-subject and between-subject variability is higher among patients with SZ and BD compared to HC. This implies that the observed intra-individual variability in cognitive performance in patients coexists with a high degree of inter-individual variability on single constructs when compared to a healthy population. Nevertheless, this did not apply for all functions. There was no between-subject variability in working memory, semantic fluency or in psychomotor processing speed, in either patient group compared to HC.
The speeded component is a common element for the observed inter-variability in mental processing speed, inhibitory control and fine-motor speed in SZ and BD. The largest variability deviance appears to be in the lower end of the test-distributions, possibly pointing towards a disease subtype with specific speed challenges. Psychomotor slowing is frequently observed in SZ22, BD23, and across SZ and BD subgroups12, and is expressed as slowed initiation and execution of responses and movement. Psychomotor slowing overlaps with clinical features such as negative symptoms, catatonia and extrapyramidal symptoms24, and is a common side effect of some medications25. Psychomotor slowing is related to worsening in negative symptoms and disability and has been suggested as an independent predictor of functional outcome in BD and SZ spectrum disorders26. Thus, one might speculate that the observed variability on speeded tests is related to such clinical and functional characteristics. This was partly confirmed by our follow-up analysis, showing increased intra and inter-individual variability among patients (although most pronounced in SZ) with more negative symptoms and worse social and functional outcome. This implies that both within- and between-individual variability differences in speeded functions are related to similar clinical outcomes, which strengthen our findings on a single test level.
Furthermore, increased use of antipsychotic medication and total medication use were associated with increased variability in fine-motor speed in BD, assumingly reflecting individuals with a more severe type of illness. In SZ, there were no such associations. However, as > 83% of the SZ sample currently were taking antipsychotic medications it is difficult to parse out these effects, since medication use often follows the severity of illness.
During normal development, the speed in which one is able to name colors, words and visual objects has been shown to improve from childhood and adolescence to adulthood27. Following this, individual illness-related factors such as age at onset, duration of illness, and severity may impact these processes differentially, creating wider ranges of performance within patients than in healthy individuals. In BD earlier onset and longer duration of illness were related to increased variability in inhibitory control, potentially reflecting disrupted neurodevelopment in some patients. Previous studies have shown that poor inhibitory control is related to mania28, neuronal dysregulation29, and genetic liability30 in BD. Since cognitive controls functions develop into adulthood, they might be particularly vulnerable to late-maturational changes such as illness onset in BD, which include onset of manic symptoms.
Studies have reported heterogeneity in verbal memory31, intellectual functioning11, as well as in intellectual trajectories12 and “at risk” stages of psychotic disorders32. However, it is not clear whether this reflects individual sensitivity to illness-related mechanisms. We found increased variability primarily in SZ, indicating some underlying mechanisms magnifying individual differences in verbal learning and memory -and intellectual outcomes in this group. It has been speculated that SZ is a progressive neurodevelopmental disorder, and that cognitive reserve (higher premorbid intellect) is related to protective compensatory mechanisms33. Patients with BD showed no difference in a measure of premorbid intellectual functioning compared to HC, supporting normal-range levels of premorbid functioning3. Current intellectual functioning and verbal learning and memory were however affected in BD compared to HC, although not to the same extent as in SZ. Intellectual variability has previously been linked to symptom severity and different functional outcomes in SZ and BD12. In line with this, we found that larger variability in intellectual function was related to having more disorganized symptoms in SZ, and increased medication use in BD, potentially reflecting illness severity in both groups. Increased medication use is likely to reflect a more severe illness type and disorganized symptoms have been linked to severity in schizophrenia34.
In healthy neurodevelopment, processes involving acquired knowledge and crystallized intelligence develop into late adulthood35 and are continuously shaped by exposure to new information through education, work and social relationships. Thus, disrupted opportunities for social and cognitive maturation due to lower education and work achievements, and difficulties maintaining social relationships in SZ, could additionally be related to the increased variability reported here.
We did not find variability differences in working memory, semantic fluency or psychomotor processing speed. In these functions, the two patient groups seemed similarly affected when compared to HC, supporting a common disease mechanism23. However, we found that increased performance on these tests (as well as most others) predicts less between-subject variability and more homogeneous performance on speeded tests (supplementary material). This could indicate that general cognitive performance, including functioning in complex and compound functions such as semantic fluency and psychomotor processing speed, is important when predicting variability in speeded functions23. Further, overall performance (cognitive composite) was the strongest predictor for intra-individual variability in BD. In SZ there was no such association and measures of intellectual function were the strongest predictors (supplementary). Regardless, intra-individual variability predicts inter-individual variability in all other tests in all groups, except for working memory in BD (supplementary). Taken together these results suggest that variability differences in BD and SZ are overlapping but also different and influenced by diverse factors. Intra-individual variability seems to capture between-subject variability in single tests in a satisfactory manner. However, it may not be sensitive to capture relevant clinical information in better functioning patients, such as BD. Speed appears to be particularly sensitive to inter-individual variation, particular among subjects with more compromised functioning. Thus, identifying patients with specific speed challenges, beyond the general speed impairment found in the majority of patients is important to achieve personalized treatment.
Strengths and weaknesses
There are some strengths and weaknesses in the study that warrant mentioning. This is the first study to explicitly investigate patient-control differences in cognitive variability. Further we present data from a large sample, covering multiple cognitive functions and clinical characteristics.
One study limitation is that we did not investigate single-task psychometrics. Cognitive tests likely differ in their sensitivity to individual differences at the extreme ends of the distribution, which could differentially affect our ability to detect diagnosis-based differences in inter-individual variability across cognitive tests. Thus, one possible confounder could be that the increased variance in patients reflects poor test psychometrics rather than “true” heterogeneity, as there were subjects performing more than 3 SD below the average. Therefore, we re-run all analyses with a cut-off of 3 SD to show that the above reported variability differences are not driven by extreme values (supplementary material). Nevertheless, these tests are commonly used when assessing heterogenous populations like SZ and BD, thus more knowledge about sensitivity to variability and how it relates to different clinical factors is important. Our result shows that individual variation in cognition relates to different clinical factors, and that the precision of a cognitive mean is dependent on symptoms, beyond simply covarying for them in a mean-model.
Environmental factors and experience may be important contributors to the observed variability in the patient groups. Unfortunately, we did not have data on environmental factors such as trauma, social deprivation, living situation etc., and this remains an important follow-up for future work investigating variability in these patients.
Conclusions
Cognitive and clinical heterogeneity represents an important challenge and opportunity for research and for developing personalized treatments in mental health services. Here we extend previous reports by explicitly modeling the case-control variability-difference in addition to the average differences, by combining a case-control design with DGLM analyses. Further, we show that cognitive variability is related to clinical characteristics in patients, supporting the clinical relevance of cognitive diversity in patients.
Our results also indicate that intra-individual variability in patients coexists with a lot of inter-individual variability in single constructs. Consequently, it is important to differentiate the specific tests contributions from other causes of individual variability in future studies. Increased variability in measures with a speeded component, appears to be particularly clinically relevant, as these were associated with more negative symptoms and worse functional outcome. These results imply that “cognitive speed” should be a treatment target in BD and SZ subgroups with poor functioning24.
Furthermore, we find that younger age at onset and increased duration of illness were related to increased variability in inhibitory control in BD. This suggest that early treatment approaches, such as cognitive remediation, should be prioritized and evaluated for particularly impaired subgroups of younger BD patients within the early illness phase, to support the development of cognitive control functions.
Methods
The cross-sectional study is part of the ongoing Thematically Organized Psychosis (TOP) study at the University of Oslo and Oslo University Hospital, approved by the Regional Committee for Medical Research Ethics and the Norwegian Data Protection Authority, and conducted in accordance with the Helsinki declaration.
Sample
The sample included a total of 1427 patients (age range 18-65) recruited from psychiatric departments and outpatient clinics in Norway, primarily in the Oslo region. Diagnoses (Dx) were set by trained psychologists or physicians using the Structured Clinical Interview for DSM- IV axis 1 disorders (SCID- I)36 and included schizophrenia (n = 524), schizoaffective (n = 126), schizophreniform (n = 51), psychosis not otherwise specified (NOS, n = 204), bipolar I (n = 312), bipolar II (n = 182) and bipolar NOS (n = 28) disorders. The diagnoses were grouped into broad spectrum SZ (n = 905) and BD (n = 522) disorders. Patients recruited to the current study (both BD and SZ) were evaluated during a stable phase (e.g., patients that were too symptomatic were not able to participate). Healthy controls in the same age range were randomly invited (using national population records Statistics Norway) from the same catchment area (n = 1170) and screened for current or previous history of mental disorder before participation. All participants were recruited in the period between 2004 and 2019, informed about the study and provided written consent before participation. Study exclusion criteria were IQ below 70 (n = 64), previous severe head injury (requiring hospitalization including amnesia/loss of consciousness), or a neurological disease interfering with brain functioning.
Clinical measures
Current positive, negative, disorganized, excited and depressive symptoms37 were assessed using the Positive and Negative Syndrome Scale (PANSS)38. Although PANSS primarily is used for assessing symptom severity in SZ, there are studies showing suitability for use in BD disorder samples39,40. Manic symptoms were assessed using the Young Mania Rating Scale (YMRS)41. Global functioning was assessed using the split version of the Global Assessment of Functioning scale (GAF)42, including separate scores for symptoms (GAF-S), and function (GAF-F). Social functioning was assessed using the Social Functioning Scale (SFS)43,44. Substance use was reported using the alcohol and drug use disorder identification tests (AUDIT/DUDIT)45,46. Medication use was reported using defined daily dose (DDD) of psychopharmacological treatment (including, antipsychotics, antidepressants, antiepileptics, lithium and total use) and estimated according to guidelines from the World Health Organization (https://www.whocc.no/atc_ddd_index). Age at onset (AAO) was calculated as the age of the first SCID-verified psychotic/manic/hypomanic episode. Additionally, we calculated AAO Depression, for first SCID-verified depressive episode. Duration of illness (DOI) was calculated subtracting AAO from current age. See Table 1 for clinical characteristics.
Cognitive domains
Psychologists or personnel trained in standardized neuropsychological assessment administered the cognitive assessment. The following cognitive domains (cursive) were included (tests in bold): Premorbid intellectual functioning was assessed using the National Adult Reading Test (NART)47 and current Intellectual functioning using the Matrix Reasoning and Vocabulary subtests of the Wechsler Abbreviated Scale of Intelligence (WASI)48. Processing speed was sub-divided into psychomotor processing speed assessed using two different versions of the Digit-symbol-coding test (Symbol coding), from the Brief Assessment of Cognition in Schizophrenia (BACS)49 and the Wechsler Adult Intelligence Scale (WAIS-III)50 respectively, and mental processing speed (without a motor component), assessed using the Color naming and Reading subtests from the Color-Word Interference test, Delis Kaplan Executive Functioning System (D-KEEFS)51. Verbal learning and memory were assessed using the learning (List Learning), delayed recall (List Recall), and recognition (List Recognition) subtests of the Californian Verbal Learning Test (CVLT)52 or the Hopkins Verbal Learning Test (HVLT)53 and using the Immediate Recall and Thematic Recall sub-scores of the Logical Memory test from the Wechsler Memory Scale (WMS)54. Semantic fluency was measured using the Category Fluency subtest from the Verbal Fluency tests, D-KEEFS51 and or the MATRICS Consensus Cognitive Battery (MCCB)55,56. Inhibitory control was assessed using the Inhibition, Inhibition Switching and the accompanying error conditions from the Color-Word Interference Test, D-KEFS51. Working memory was measured using three sub-scores from the Digit Span test, including Digit Span Forward, Digit Span Backward and the Digit Span Total score from WAIS-III50, and using the total score from two different versions of the Letter Number Sequencing tests (MCCB and WAIS, respectively)50,56. Finally, to measure fine-motor speed, the two sub-scores from the Grooved Pegboard test, dominant hand (Grooved Pegboard DH) and non-dominant hand (Grooved Pegboard NDH) were used57. As some tests measuring the same skill were slightly different, we calculated standardized (not normalized) scores for each test, using the control group means and standard deviations as reference. Then, using standardized test scores, we calculated a cognitive composite score based on the average of the standardized scores and an intra-individual variance in performance score, using the standard deviations across the scores for each individual. A more detailed description of the tests (including descriptive statistics and number of valid cases per test) can be found in the online supplement.
Statistical analyses
Statistical analyses were performed with R (version 3.5.3) and the R-package “dglm” (https://CRAN.R-project.org/package=dglm), and SPSS version 25.
Group differences in demographic and clinical data were assessed in SPSS using independent t-tests and analysis of variance (ANOVA) for continuous variables and chi- square statistics for categorical data.
In the main analyses we simultaneously estimated mean and between-subject variability (dispersion) parameters using DGLM, which iterates between the mean and dispersion sub-models until overall convergence. For each of the 24 cognitive variables, we used the following model specifications (1) Y ~ Age + Sex + Dx, (2) ~ Age + Sex + Dx. Here (1) is the mean model specification, and (2) is the dispersion model specification, and Y represents the cognitive outcome variables for the first GLM and the dispersion of the mean GLM (the residual scores) for the second GLM. For the group comparison we then obtain an estimate of the mean difference between groups, as well as an estimate of the difference in dispersion around the mean between SZ/HC, BD/HC, and SZ/BD for all the cognitive variables, including the precalculated composite and intra-individual variability scores.
All effects were corrected for multiple testing using the Bonferroni method (α = 0.005/48 tests ~ log10(p) =3.98, or p < 0.000104).
To investigate the degree to which the range of individual variability in cognitive performance is associated with disease severity within SZ or BD group, we added symptom measures (Sx) as additional independent variables in the dGLMs (Y ~ Age + Sex + Sx, (2) ~ Age + Sex + Sx). For these analyses we adjusted the false discovery rate58 using the R-function “p.adjust”, with q = 0.05 and method = ”BH”(https://www.jstor.org/stable/2346101), this was done across all tests and group-comparisons. The statistical threshold for q = 0.05 was set to log10(p) = 2.03, or p < 0.009.
Reanalysis of the mean and dispersion models with outlier removal (3 SD cut-off on all cognitive measures) can be found in the supplementary material (Fig. S2). There are also association analyses between mean performance on one test and the dispersion of the other (Fig. S3), to check whether performance on one task is related to cognitive heterogeneity in another, i.e. if higher performance on one test is related to higher or lower variability on another.
Data availability
The dataset used in the current study are not publicly available due to privacy or ethical restrictions. Anonymized data can be made available from the authors on reasonable request and with permission of Norwegian Center for Mental Disorders Research.
References
Keefe, R. S. & Fenton, W. S. How should DSM-V criteria for schizophrenia include cognitive impairment? Schizophr Bull. 33, 912–920 (2007).
Lepage, M., Bodnar, M. & Bowie, C. R. Neurocognition: clinical and functional outcomes in schizophrenia. Can. J. Psychiatry 59, 5–12 (2014).
Simonsen, C. et al. Neurocognitive dysfunction in bipolar and Schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophrenia Bull. 37, 73–83 (2009).
Baune, B. T. & Malhi, G. S. A review on the impact of cognitive dysfunction on social, occupational, and general functional outcomes in bipolar disorder. Bipolar Disord. 17, 41–55 (2015).
Bora, E. & Pantelis, C. Meta-analysis of cognitive impairment in first-episode bipolar disorder: comparison with first-episode Schizophrenia and healthy controls. Schizophr Bull. 41, 1095–1104 (2015).
Bora, E. & Özerdem, A. Meta-analysis of longitudinal studies of cognition in bipolar disorder: comparison with healthy controls and schizophrenia. Psychol. Med. 47, 2753–2766 (2017).
Keshavan, M. S. et al. A dimensional approach to the psychosis spectrum between bipolar disorder and schizophrenia: the Schizo-Bipolar Scale. Schizophr Res. 133, 250–254 (2011).
Bipolar Disorder and Schizophrenia Working Group of the Psychiatric Genomics Consortium. Genomic dissection of bipolar disorder and schizophrenia, including 28 subphenotypes. Cell 173, 1705–1715.e1716 (2018).
Brandt, C. L. et al. Working memory networks and activation patterns in schizophrenia and bipolar disorder: comparison with healthy controls. Br. J. Psychiatry 204, 290–298 (2014).
Smeland, O. B. et al. Genome-wide analysis reveals extensive genetic overlap between schizophrenia, bipolar disorder, and intelligence. Mol. Psychiatry 25, 844–853 (2020).
Van Rheenen, T. E. et al. Characterizing cognitive heterogeneity on the schizophrenia-bipolar disorder spectrum. Psychol Med. 47, 1848–1864 (2017).
Vaskinn, A. et al. Cognitive heterogeneity across Schizophrenia and bipolar disorder: A cluster analysis of intellectual trajectories. J. Int. Neuropsychol. Soc. 1-13 (2020).
Weinberg, D. et al. Cognitive sbtypes of Schizophrenia characterized by differential brain volumetric reductions and cognitive decline. JAMA Psychiatry 73, 1251–1259 (2016).
Ferguson, H. J., Brunsdon, V. E. A. & Bradford, E. E. F. The developmental trajectories of executive function from adolescence to old age. Sci Rep. 11, 1382 (2021).
Hibar, D. P. et al. Cortical abnormalities in bipolar disorder: An MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Molecular Psychiatry 23, 932–942 (2018).
van Erp, T. G. M. et al. Cortical brain abnormalities in 4474 individuals with Schizophrenia and 5098 control subjects via the enhancing neuro imaging genetics through meta analysis (ENIGMA) consortium. Biol. Psychiatry 84, 644–654 (2018).
Alnæs, D. et al. Brain heterogeneity in schizophrenia and its association with polygenic riskbrain heterogeneity in schizophrenia and polygenic riskbrain heterogeneity in Schizophrenia and polygenic risk. JAMA Psychiatry 76, 739–748 (2019).
Wolfers, T. et al. Mapping the heterogeneous phenotype of Schizophrenia and bipolar disorder using normative models. JAMA Psychiatry 75, 1146–1155 (2018).
Carruthers, S. P., Van Rheenen, T. E., Gurvich, C., Sumner, P. J. & Rossell, S. L. Characterising the structure of cognitive heterogeneity in schizophrenia spectrum disorders. A systematic review and narrative synthesis. Neurosci. Biobehav. Rev. 107, 252–278 (2019).
Haatveit, B. C. et al. The validity of d prime as a working memory index: results from the “Bergen n-back task”. J. Clin. Exp. Neuropsychol. 32, 871–880 (2010).
Wells, R. et al. The impact of premorbid and current intellect in schizophrenia: cognitive, symptom, and functional outcomes. npj Schizophrenia 1, 15043 (2015).
Dickinson, D., Ramsey, M. E. & Gold, J. M. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch. Gen. Psychiatry 64, 532–542 (2007).
Robinson, L. J. et al. A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. J. Affect. Disord. 93, 105–115 (2006).
Osborne, K. J., Walther, S., Shankman, S. A. & Mittal, V. A. Psychomotor slowing in Schizophrenia: Implications for endophenotype and biomarker development. Biomarkers Neuropsychiatry 2, 100016 (2020).
Morrens, M., Hulstijn, W. & Sabbe, B. Psychomotor slowing in Schizophrenia. Schizophrenia Bull. 33, 1038–1053 (2007).
Lee, R. S. et al. Neuropsychological and functional outcomes in recent-onset major depression, bipolar disorder and schizophrenia-spectrum disorders: A longitudinal cohort study. Transl. Psychiatry 5, e555 (2015).
van den Bos, K. P., Zijlstra, B. J. H. & lutje Spelberg, H. C. Life-span data on continuous-naming speeds of numbers, letters, colors, and pictured objects, and word-reading speed. Sci. Stud. Reading 6, 25–49 (2002).
Strakowski, S. M. et al. Characterizing impulsivity in mania. Bipolar Disord. 11, 41–51 (2009).
Breukelaar, I. A. et al. Investigating the neural basis of cognitive control dysfunction in mood disorders. Bipolar Disord. 22, 286–295 (2020).
Hıdıroğlu, C. et al. Response inhibition and interference control in patients with bipolar I disorder and first-degree relatives. Bipolar Disord. 17, 781–794 (2015).
Heinrichs, R. W., Parlar, M. & Pinnock, F. Normal-range verbal-declarative memory in schizophrenia. Neuropsychology 31, 778–786 (2017).
Reichenberg, A. et al. Premorbid intra-individual variability in intellectual performance and risk for schizophrenia: a population-based study. Schizophr Res. 85, 49–57 (2006).
Van Rheenen, T. E. et al. Widespread volumetric reductions in Schizophrenia and schizoaffective patients displaying compromised cognitive abilities. Schizophr Bull. 44, 560–574 (2018).
Ortiz, B. B. et al. Disorganized symptoms predicted worse functioning outcome in Schizophrenia patients with established illness. Clin. Schizophrenia Related Psychoses 11, 151–155 (2017).
Hartshorne, J. K. & Germine, L. T. When does cognitive functioning peak? The asynchronous rise and fall of different cognitive abilities across the life span. Psychol. Sci. 26, 433–443 (2015).
First, M., Spitzer, R., Gibbon, M., & Williams, J. B. W. Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (SCID-P), Version 2. New York: New York State Psychiatric Institute, Biometrics Research (1995).
Wallwork, R. S., Fortgang, R., Hashimoto, R., Weinberger, D. R. & Dickinson, D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr Res. 137, 246–250 (2012).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative symptome scale (PANSS) for schizophrenia. Schizophrenia Bull. 13, 261–276 (1987).
Lindenmayer, J. P., Bossie, C. A., Kujawa, M., Zhu, Y. & Canuso, C. M. Dimensions of psychosis in patients with bipolar mania as measured by the positive and negative syndrome scale. Psychopathology 41, 264–270 (2008).
Daneluzzo, E. et al. PANSS factors and scores in schizophrenic and bipolar disorders during an index acute episode: a further analysis of the cognitive component. Schizophrenia Res. 56, 129–136 (2002).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435 (1978).
Pedersen, G., Hagtvet, K. A. & Karterud, S. Generalizability studies of the global assesment of functioning-split version. Comprehensive Psychiatry 48, 88–94 (2007).
Birchwood, M., Smith, J., Cochrane, R., Wetton, S. & Copestake, S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br. J. Psychiatry 157, 853–859 (1990).
Hellvin, T. et al. Validation of the Norwegian version of the Social Functioning Scale (SFS) for schizophrenia and bipolar disorder. Scand. J. Psychol 51, 525–533 (2010).
Berman, A. H., Bergman, H., Palmstierna, T. & Schlyter, F. Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur. Addict. Res. 11, 22–31 (2005).
Saunders, J. B., Aasland, O. G., Babor, T. F., De la Fuente, J. R. & Grant, M. Development of the alcohol use disorders identification test (AUDIT). WHO collaborative project on early detection of persons with harmful alcohol consumption-II. ADDICTION-ABINGDON- 88, 791–791 (1993).
Sundet, K. & Vaskinn, A. Estimating premorbid IQ. J. Norwegian Psychol. Assoc. 45, 1108–1115 (2008).
Wechsler, D. Wechsler Abbreviated Scale of Intelligence (WASI) Retrieved from Stockholm (2007a).
Keefe, R. S. E. et al. Brief Assessment of Cognition in Schizophrenia (BACS). APA PsycTests (2004).
Wechsler, D. Wechsler adult intelligence scale - third edition (WAIS-III). In Norwegian manual. Stockholm: Pearson assessment (2003).
Delis, D. C., Kaplan, E., & Kramer, J. H. Delis - Kaplan Executive Function System (D-KEFS) Norwegian Manual. In. Stockholm: Pearson Assessment (2005).
Delis DCKJ, K. E., Ober B. A. California Verbal Learning Test: CVLT-II. Stockholm, Sweden: Pearson Assessment (2004).
Benedict, R. H., Schretlen, D., Groninger, L. & Brandt, J. Hopkins verbal learning test–revised: normative data and analysis of inter-form and test-retest reliability. Clin. Neuropsychol. 12, 43–55 (1998).
Wechsler, D. WMS-III: Wechsler memory scale administration and scoring manual: Psychological Corporation (1997).
Mohn, C., Sundet, K. & Rund, B. R. The Norwegian standardization of the MATRICS (Measurement and Treatment Research to Improve Cognition in Schizophrenia) Consensus Cognitive Battery. J. Clin. Exp. Neuropsychol 34, 667–677 (2012).
Nuechterlein, K. H. et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am. J. Psychiatry 165, 203–213 (2008).
Klove, H. CLINICAL NEUROPSYCHOLOGY. Med. Clin. North Am. 47, 1647–1658 (1963).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B (Methodological) 57, 289–300 (1995).
Acknowledgements
We would like to thank all the participants who volunteered in the study for their time and effort. Additionally, we would like to thank the clinician, nurses and psychologist who contributed with patient recruitment. This work was funded by the Research Council of Norway (#223273), the KG Jebsen Stiftelsen, the European Research Council under the European Union’s Horizon 2020 research and Innovation program (ERC StG, Grant 802998), and South-Eastern Norway Regional Health Authority (grants 2019107 and 2020086).
Author information
Authors and Affiliations
Contributions
B.H., D.A., L.T.W. and T.U. took part in designing the study. B.H. and D.A. undertook the statistical analyses. Author B.H. managed the literature search and wrote the first draft of the manuscript. All authors have contributed to interpretation of data, critically revising and final approval of the completed version, and are accountable for all aspects of the work. Authors D.A. and T.U. contributed equally to this work.
Corresponding author
Ethics declarations
Competing interests
A.V. has received honorarium from VeraSci. O.A.A. has received speaker’s honorarium from Lundbeck and Sunovion and is a consultant to HealthLytix. The other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haatveit, B., Westlye, L.T., Vaskinn, A. et al. Intra- and inter-individual cognitive variability in schizophrenia and bipolar spectrum disorder: an investigation across multiple cognitive domains. Schizophr 9, 89 (2023). https://doi.org/10.1038/s41537-023-00414-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00414-4