Abstract
Whilst involvement of the motor cortex in the phenomenon of freezing in Parkinson’s disease has been previously suggested, few empiric studies have been conducted to date. We investigated motor cortex (M1) excitability in eleven right-handed Parkinson’s disease patients (aged 69.7 ± 9.6 years, disease duration 11.2 ± 3.9 years, akinesia-rigidity type) with verified gait freezing using a single-pulse transcranial magnetic stimulation (TMS) repetitive finger tapping paradigm. We delivered single TMS pulses at 120% of the active motor threshold at the ‘ascending (contraction)’ and ‘descending (relaxation)’ slope of the tap cycle during i) regular tapping, ii) the transition period of the three taps prior to a freeze and iii) during freezing of upper limb movement. M1 excitability was modulated along the tap cycle with greater motor evoked potentials (MEPs) during ‘ascending’ than ‘descending’. Furthermore, MEPs during the ‘ascending’ phase of regular tapping, but not during the transition period, were greater compared to the MEPs recorded throughout a freeze. Neither force nor EMG activity 10–110 s before the stimulus predicted MEP size. This piloting study suggests that M1 excitability is reduced during freezing and the transition period preceding a freeze. This supports that M1 excitability is critical to freezing in Parkinson’s disease.
Similar content being viewed by others
Introduction
Freezing phenomena in idiopathic Parkinson’s disease (PD) represent a significant source of disease-related disability1,2,3. More than 60% of PD patients experience some form of freezing with disease progression, and the incomplete understanding of the pathophysiology and circuit mechanisms limits effective treatment4,5. Freezing most commonly occurs while walking (FoG) but also during swallowing6, speech3, and particularly during repetitive movements of the upper limbs (ULF)7,8,9. Like FoG, ULF significantly impairs daily activities such as handwriting, tooth brushing, typing, or bimanual coordination1,10,11. The similar spatiotemporal characteristics of FoG and ULF12 prompted research interest in ULF to generate neurophysiological hypotheses on FoG and freezing phenomena in general.
Ultimately, ULF represents the failure to produce an intended movement sequence effectively2,13,14. The production of internally generated movement strongly depends on movement planning in frontostriatal projections to M115. The desynchronization of sensorimotor beta-band oscillatory activity during the acceleration phase of a repetitive movement cycle has previously been related to activity across the subthalamic nucleus, the primary motor cortex (M1), and prefrontal areas8,16. Furthermore, impaired movement-related modulation of beta-band activity over the sensorimotor area has been associated with freezing behaviour14,17,18,19, and can be observed for up to three taps before a freeze8. Combined EEG-TMS studies have established a direct pathophysiological link between oscillatory activity and M1 excitability, showing that M1 excitability was enhanced during beta-band desynchronization but reduced during beta-band synchronization20,21.
Here, we studied M1 excitability in PD freezers during regular tapping, transitions, and ULF. Specifically, we investigated the transitions between regular tapping and episodes of ULF using single-pulse TMS time-locked to the tap cycle. Based on the available neurophysiological evidence, we hypothesized that M1 excitability would be modulated throughout the tap cycle with higher excitability during the contraction (ascending) phase and lower excitability during the relaxation (descending) phase. Secondly, we hypothesized that M1 excitability would be reduced during ULF episodes compared to ascending periods of regular tapping. Finally, we anticipated that M1 excitability during the transition period between regular tapping and freezing would show reduced excitability in ascending compared to freezing and lower difference of M1 excitability between ascending and descending.
Results
Behavioural findings
On average, all patients completed 15 tapping blocks (SD = 5) with a mean tapping frequency of 2.53 Hz (SD = 1.29). Within these blocks, we detected 237 freezing episodes across all patients, lasting on average 0.83 s (SD = 0.13). In two patients, no TMS pulse coincided with a freezing episode (Table 1) and the data from these patients were excluded from statistical analyses concerning ULF.
Overall, 1,067 single pulses were delivered. Of these, 505 were applied during the ascending slope (mean = 27.84% of the tap cycle, SD = 9.81), 447 during regular tapping (rTasc; median force = 1.44 N, IQR = 0.67), and 58 during the transition phase (TRANSasc; median force 1.44 N, IQR = 0.58). For the descending slope, 503 pulses were triggered (mean 75.19%, SD = 8.06), 425 during regular tapping (rTdesc; median force 1.48 N, IQR = 0.62), and 78 during the transition phase (TRANSdesc; median force=1.51 N, IQR = 0.56). Another 59 pulses coincided with ULF (median force=1.39 N, IQR = 0.76). Finally, 123 of the pulses (36 ascending (29.27%), 80 descending (65%), 7 ULF (5.69%)) did not evoke a MEP (<200µV) and were thus set to value zero.
MEPs during regular tapping, freezes, and transitions
We found that during regular tapping, ascending MEPs were greater compared with descending MEPs (U = 71402, P < 0.001) and greater compared with ULF (U = 8904, P = 0.007) (Fig. 1). In contrast, MEPs during the descending phase did not differ from ULF (U = 11954, P = 0.562). During the transition phase, MEPs during the ascending cycle were still greater than for descending (U = 1772, P = 0.031) but no longer differed from periods of ULF (U = 1520, P = 0.298).
Overview of all conducted Mann-Whitney U tests: we compared normalized MEP sizes (ascending slope vs. descending slope) during regular tapping (rTasc vs. rTdesc), the transition (TRANSasc vs. TRANSdesc), and regular tapping ascending (rTasc) with ULF. MEP sizes were greater at ascending (downward press) compared to descending (upward release) during both regular tapping and transition (see Methods for definition of transition). MEPs evoked at rTasc (successful motor output) were also greater than during ULF (unsuccessful motor output), but overall MEP size variability increased when freezing (ULF). X-axis: % change from block average as median ± 95%-confidence interval; Y-axis: motor behavioural state.
As expected, right FDI EMG activity outside the MEPs of both regular and transition time segments was modulated across the tap cycle and was slightly greater for ascending (44.28 ± 6.81µV (mean ± SEM) compared to descending (28.27 ± 6.09µV; Z = −2.045, P = 0.041) phases (Fig. 2). However, EMG activity did not differ between ascending and ULF (32.76 ± 5.10µV; Z = −1.689, P = 0.091) or descending and ULF (Z = −1.423; P = 0.155) contrasts.
a Average EMG activity over all single taps of all patients (all data). Black line shows mean EMG activity, grey area shows SEM. A real-time signal processing algorithm (based on Simulink Real-Time Version R2016a, MathWorks Inc., USA) triggered single TMS pulses aimed at 25% tap cycle (=ascending), or 75% tap cycle (=descending), respectively, with an interstimulus interval of >2.5 s. Arrows show the mean percentage of tap cycle at the actual time of TMS (asc: mean = 27.84, SD = 9.81; desc: mean = 75.19, SD = 8.06). b Histogram of tapping force levels (N) at the time of TMS. There was no significant statistical difference between force levels at the time of TMS. Please note, that ascending and descending each contain both, data from the transition and regular tapping.
Secondary analyses to control for potential effects of force and EMG pre-stimulus activity
There was no correlation EMG activity 110–10 ms before a single TMS pulse and MEP size. This held true for both normalized and un-normalized MEP size (Fig. 3). Additionally, force levels at stimulation did not differ between the ascending and descending phases of regular tapping (U = 89944, P = 0.175), or for transition (ascending vs. descending, U = 2002, P = 0.254), or between regular tapping ascending and ULF (U = 10178, P = 0.19).
Spearman’s rho correlation analysis between background EMG activity 110–10 ms before stimulation (RMS, root mean square) and MEP size. a. Correlation with raw MEPs before normalization (r = −0.0267, 95% CI −0.0861–0.0329, p = 0.3651). b Correlation with normalized MEPs (r = 0.056, 95% CI −0.0032–0.1155, p = 0.056).
Nevertheless, to further exclude any confounding effects of pre-stimulus EMG activity or force on MEP size, we added a linear regression analysis with MEP size as dependent, and behavioural state, EMG activity, and force as independent variables (refer methods for details). Overall, the model showed predictive value on MEP size (R2 = 0.03692, F(4.928)=8.894, P = 4.764e-07), as expected. However, this was driven by the differences in the behavioural state between “regular tapping ascending” vs. “descending” (P < 0.001) and “regular tapping ascending” vs. “freezing” (P = 0.0374). However, neither EMG activity (P = 0.511) nor force (P = 0.883) were predictive in this model.
Discussion
We used adaptive single-pulse TMS to study M1 excitability in PD freezers during the ascending (contraction) and descending (relaxation) cycles of regular finger tapping, the transition period, and actual freezing episodes. As expected, cortical excitability fluctuations in M1 were preserved during regular tapping and transitions depending on the movement phase. However, M1 excitability was reduced during freezing compared to the ascending phase of regular tapping, despite the intention to move. During ascending transition taps, M1 excitability was no longer increased compared to freezing and pointed to a premonitory abnormality of M1 in increasing excitability.
In our experiment, background EMG was slightly higher comparing the ascending to the descending slope of tapping, whereas the force levels did not differ between conditions22. In control analysis, we did not find a correlation of background EMG with MEP size, nor did we find predictive value of force or EMG background activity when we included these variables to a multiple regression model. However, the effect of behavioural state (regular tapping ascending / descending, freezing) persisted. Thus, it is unlikely that background EMG or force explained our findings23. Instead, phase-specific modulation of corticospinal responsiveness has been observed during lower24 and upper limb cyclic movements23 in younger, healthy subjects, and our findings support that such excitability fluctuations aligned to the movement cycle are preserved in PD freezers. However, PD freezers were impaired when increasing cortical excitability during the freeze and the transition period. In the light of previous research, the insufficient increase of M1 excitability of the Parkinsonian M1 does not necessarily constitute a general abnormality but rather emerges during voluntary movement. Whereas the PD resting motor thresholds were found to be mostly similar to those reported in healthy controls25, the Parkinsonian M1 has shown reduced cortical excitability increases during isometric contraction and in reaction time tasks. This was reflected by flattened input-output curves in incremental isometric contractions26, and by abnormalities in pre-movement facilitation in a reaction time motor task, such that the Parkinsonian M1 showed an earlier but lower excitability increase prior to externally cued voluntary movements27,28. Our findings suggest that the freezing phenomenon may critically depend on such rapid and sufficient adjustments of cortical excitability to stabilize repetitive movement sequences. In turn, failure of these excitability adjustments – as observed during the transition period – may give rise to freezing, which could represent a generalized pathophysiologic mechanism common to the symptoms observed in upper and lower limbs and speech. Indeed, motor deterioration in our experiment became first kinematically visible during freezing but was neurophysiologically measurable in the transition phase already, when cortical excitability decreased. This may have been related to increasing performance difficulties and reflect a “timing problem” when modulating M1 excitability over the tap cycle. In this sense, increasing demands on motor performance such as fatigue or high tapping speed9 might have deranged the physiological time course of excitability modulations and preparation of M1 to increase excitability when needed16.
In general, M1 excitability and successful motor output rely heavily on afferent inputs from diverse cortical and subcortical areas to M129. Particularly the generation of self-initiated sequential (finger) movements – movement most susceptible to freezing – depends on intact signal transmission from the frontoparietal executive control network30 and the BG-thalamic-motor loop, involving the supplementary motor area, M1, putamen, globus pallidus, and ventrolateral thalamus31. In PD, reduced effective connectivity between these areas and the loss of automaticity32 lead to compensatory over-reliance on the cognitive striatum for effective movement production. The competition for limited processing resources with increasing motor task difficulty is then believed to cause transient striatal dysfunction and STN overactivity, ultimately resulting in freezing33.
As such, our observations are compatible with existing pathophysiological models of freezing that have postulated a ‘dysexecutive’ communication failure between frontostriatal and primary motor areas with a paroxysmal failure to produce effective motor output2,15,28. These models embedded M1 and other gait-related structures in an “inhibited” or “hypoactive” state33 and indeed, we found that M1 was less excitable such that the insufficient “facilitation” of M1 excitability paralleled the freeze. From the present experiment, however, we cannot infer if M1 was actively inhibited or lacked afferent input (or both). This distinction is pathophysiologically meaningful since inhibition versus facilitation of M1 rely on different intracortical circuits and neurotransmitters, which both reflect separate active processes34,35. We found that excitability during freezing did not differ significantly from excitability during the transition. In fact, M1 excitability was lowest overall at relaxation during the transition – when motor output was still intact. Motor arrest during freezing, however, occurred involuntarily, suggesting that the abnormally excited M1 may indeed result from activation failure (lack of excitatory afferences) rather than active inhibition. Even though this observation is based on a relatively small sample, we believe it is still worth noting since it highlights the importance of the underlying movement intention (voluntary vs. involuntary motor stops) and the reliance on the cognitive control network to compensate for deficiencies in internal movement generation and motor automaticity15. Nonetheless, it remains for future studies to investigate inhibitory plasticity measures during a freeze.
Finally, our findings parallel clinical observations made on freezing of gait, in which TMS protocols increasing M1 excitability have led to an improvement in symptoms, i.e., 10 Hz repetitive TMS of M136, or combined stimulation of the dorsolateral prefrontal cortex and M1 with anodal transcranial direct current stimulation37 and further corroborate the notion of an hypoactive M1 during freezing.
There are a few points to consider when interpreting our results. First, the presented data of our pilot study is based on a small sample size, which naturally increases variability and may limit statistical power. Hence, we used a statistical approach focusing not on individual patients but on the pooled number of evoked MEPs per experimental condition. This enabled us to collect sufficient data (regular tapping asc (447 MEPs)/desc (425 MEPs), transition asc (58 MEPs)/desc (78 MEPs), freezing (59 MEPs)) to perform meaningful analyses.
Second, as healthy controls do not freeze, we did not add a healthy control group, even though the logical foundation of our experiment is based on available literature on repetitive movements in health. We know from healthy subjects, for example, that MEP size is modulated along cyclic upper and lower limb movements23,24 and combined TMS-EEG studies showed that beta-band desynchronization over the sensorimotor area related to increased M1 excitability and greater MEP size20,21,38. In PD patients, our work8 and the work of other groups16 found that during repetitive finger tapping beta activity modulation was preserved and modulated along the tap cycle in a similar fashion albeit differences have been observed regarding peak beta amplitudes16,17,18,19. Thus, we concluded that modulation of M1 excitability relative to the tap cycle would be preserved in PD patients, and this is indeed one finding of the present study.
Third, we chose to study patients in the off-medication state only as it allowed to observe the genuine disease-related pathophysiology of freezing and L-Dopa withdrawal significantly increases freezing likelihood39. On-state freezing, on the other hand, would have provided heterogeneity in terms of L-Dopa resistant freezing vs. paradoxical on-freezes, both of which are considered different phenomena40. Also, previous TMS experiments found no meaningful differences in MEP amplitudes (during isometric contraction) before and after L-Dopa intake25,26,41,42 and particularly during finger tapping, cortical beta band modulations did not differ between medication on- and off-states in an EEG experiment with PD patients43.
In conclusion, freezing reflects an episodic event of ineffective motor output. Our findings suggest that the Parkinsonian M1 is impaired in increasing excitability during a freeze and, critically, already during the transition phase preceding a freeze. Therapeutic interventions modulating M1 should be investigated as a treatment approach to ameliorate freezing phenomena in Parkinson’s disease.
Methods
Patients
We studied eleven right-handed patients with akinetic-rigid iPD and clinically verified FoG44 (Table 1). Exclusion criteria were a Mini-Mental State Examination score <22/30, TMS safety concerns45, and neurological (ataxia, spasticity, epilepsy) or psychiatric disorders (major depression, substance abuse) that would impact interpretability, performance, and/or compliance. Patients participated with written informed consent and the study protocol followed the Declaration of Helsinki, which was approved by the ethics committee of the University of Tübingen (protocol number: 916/2018BO1).
Study design
Patients were investigated during their “medication off” state having withdrawn overnight from their dopaminergic medication. Preparation included the mounting of the EMG electrodes, identification of the individual motor hotspot46, and determination of the individual active motor threshold (aMT) following standardized procedures published elsewhere47. The EMG was recorded from the right first dorsal interosseus (FDI) in the belly-tendon montage (5 kHz sampling rate, 0.16 Hz–1.25 kHz bandpass filter, 24-bit amplifier). Patients placed their right index finger on a force sensor and were instructed to perform internally generated taps as fast and accurately as possible up to a 2 N peak maximum while keeping the finger in permanent contact with the sensor. Real-time visual feedback was provided on tapping force and accuracy. A tapping block lasted 30 s, followed by a 20 s pause to prevent fatigue. Overall, one session included ten blocks of continuous, self-paced tapping or more, if possible.
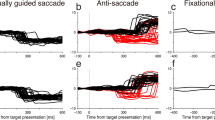
Single-pulse TMS was applied over the hand representation of the left M1 using a figure-of-eight coil (Magstim D70, 70 mm winding; Magstim Ltd., UK) at 120% aMT stimulus intensity46. A custom-made real-time signal processing algorithm based on Simulink Real-Time (Version R2016a, MathWorks Inc., USA) was used to trigger single TMS pulses in response to specific pressure sensor force conditions during the tap cycle. We phase-locked the pulses to 25% (ascending) and 75% (descending) of the tap cycle (NeurOne Tesla with Digital-Out Option, Bittium, Finland) in randomized order (Fig. 4). An interstimulus interval of ≥2.5 s was maintained to prevent induction of neural plasticity from repetitive stimulation48,49. Transitions or freezes were thus only hit by chance as a reliable real-time prediction based on the kinematic time series has not yet been established for these time segments. Transition segments could only be identified in post-hoc analysis.
Top panels show sections of kinematic data, that is, continuous tapping (Force, (N)) over time (s) and the time point of the TMS pulse (grey vertical lines). Bottom panels show the corresponding MEP (Amplitude, (µV); 20–40 ms after TMS pulse) recorded over the right first dorsal interosseus (rFDI). For the sake of clarity, different time scales have been chosen for kinematic and MEP panels, but overlay at time ‘0’, i.e. TMS pulse. a regular tapping ascending (rTasc), b regular tapping descending (rTdesc), c transition period ascending (TRANSasc), d transition period descending (TRANSdesc), e freezing (ULF).
Data segmentation and processing
Preprocessing was done with FieldTrip open-source toolbox50 and customized MATLAB® scripts (Mathworks Ltd, USA, R2017a). Each patient’s kinematic data was segmented into single taps and ULF episodes using MATLAB function ‘findpeaks.m’. One tap cycle consisted of a downward press (trough to peak) and an upward release (peak to trough). A trough-peak-trough section was considered a full tap if it lasted <2 s and if its amplitude deflection from trough-to-peak and peak-to-trough was ≥1 N (50%)8. We then calculated mean tapping frequencies (per patient, overall) and average EMG activity (freezing, regular tapping). ULF episodes were detected visually based on the following criteria: (i) reduction of amplitude deflection >50%, (ii) Freezing Index (FI) > 1, and (iii) duration ≥0.5 s11,51.
Peak-to-peak MEPs were extracted from the EMG signal 20–40 ms after the TMS pulse and stored for analysis if >200 µV47. Lower amplitudes were set to 0 µV and considered ‘no MEP’ for statistical analyses. The mean MEP size per individual and tapping block served as reference for normalization to account for intra- and interpersonal drifts in cortical excitability52. MEPs were classified as either ‘ascending’ or ‘descending’ during regular tapping and in the transition period, which was taken as the last three taps preceding a freeze8. MEPs during freezing episodes were not divided into ascending or descending due to the lack of effective motor output when freezing.
It is known that force levels and background EMG activity at or just before single-pulse TMS may influence MEP size22,53,54,55. Therefore, we deliberately chose the right FDI muscle to record MEPs due to its partial agonist activity during finger tapping to reduce the magnitude of these influences.
Statistical analysis
This piloting study aimed to investigate real-time cortical excitability in PD patients during repetitive finger movements, transitions and freezing. We decided on an exploratory strategy, as (i) recording time and adherence of PD patients in “medication off” was limited and (ii) the number of freezes and transitions that could be recorded in the laboratory setting and with it the number of MEPs evoked per condition could not be predicted. This also meant that we planned to perform non-parametric pairwise comparisons between contrasts of interest as introduced above, i.e. we had neurophysiological hypothesis as introduced above comparing regular ascending vs. descending, regular ascending vs. ULF, transition ascending vs descending, and transition ascending vs. ULF.
Further, we used a linear multiple regression model to predict MEP size from different independent variables, i) behavioural state (regular tapping ascending, regular tapping descending, freezing), ii) background EMG activity (rooted mean square 10–110 ms prior to stimulation) and force at the time of stimulation. MEP size was treated as dependent outcome variable to ensure that EMG activity and MEP sizes were not linearly related23.
Statistical analyses were performed with SPSS® version 25 (IBM), Prism 8 (GraphPad), and Matlab® (Mathworks 2017a Ltd, USA); graphs were created with Prism 8. MEP amplitudes were not normally distributed (Shapiro-Wilk test) and thus all statistical tests were two-tailed nonparametric (Mann-Whitney U, Wilcoxon signed ranks test, Spearman’s rho), and a p-value of < 0.05 was considered statistically significant. MEPs are presented as percent (%) change from the block average.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data related to the analysis and findings of this study can be provided to interested researchers upon reasonable request from the principal authors of this study (Marlene Topka and Daniel Weiss). Data are locally stored on the archiving system of the Hertie-Institute for Clinical Brain Research. Since the MEP data and clinical metadata of this study stem from human beings, we consider controlled access to these data under privacy, ethical, and legal issues.
Code availability
Code related to the analysis and findings of this study can be provided to interested researchers upon reasonable request from the principal authors of this study (Marlene Topka and Daniel Weiss). Code is locally stored on the archiving system of the Hertie-Institute for Clinical Brain Research.
References
Nemanich, S. T., McNeely, M. E., Earhart, G. M., Norris, S. A. & Black, K. J. A case of apparent upper-body freezing in parkinsonism while using a wheelchair. Front Neurol. 8, 205 (2017).
Weiss D. et al. Freezing of gait: understanding the complexity of an enigmatic phenomenon. Brain. Published online October 24, 2019:awz314.
Moreau, C. et al. Oral festination in Parkinson’s disease: Biomechanical analysis and correlation with festination and freezing of gait. Mov. Disord. 22, 1503–1506 (2007).
Shine, J. M. et al. Freezing of gait in Parkinson’s disease is associated with functional decoupling between the cognitive control network and the basal ganglia. Brain 136, 3671–3681 (2013).
Ehgoetz Martens, K. A. et al. The functional network signature of heterogeneity in freezing of gait. Brain 141, 1145–1160 (2018).
Maetzler, W. et al. Freezing of Swallowing. Mov. Disord. Clin. Pr. 3, 490–493 (2016).
Naismith, S. L. & Lewis, S. J. G. A novel paradigm for modelling freezing of gait in Parkinson’s disease. J. Clin. Neurosci. 17, 984–987 (2010).
Scholten, M. et al. Transitions between repetitive tapping and upper limb freezing show impaired movement-related beta band modulation. Clin. Neurophysiol. 131, 2499–2507 (2020).
Heremans, E. et al. When motor control gets out of hand: Speeding up triggers freezing in the upper limb in Parkinson’s disease. Parkinsonism Relat. Disord. 64, 163–168 (2019).
Heremans, E. et al. Handwriting impairments in people with Parkinson’s disease and freezing of gait. Neurorehabil Neural Repair 30, 911–919 (2016).
Vercruysse, S. et al. The Neural Correlates of Upper Limb Motor Blocks in Parkinson’s Disease and Their Relation to Freezing of Gait. Cereb. Cortex 24, 3154–3166 (2014).
Vercruysse, S. et al. Freezing beyond gait in Parkinson’s disease: A review of current neurobehavioral evidence. Neurosci. Biobehav Rev. 43, 213–227 (2014).
Scholten, M. et al. Neuromuscular correlates of subthalamic stimulation and upper limb freezing in Parkinson’s disease. Clin. Neurophysiol. 127, 610–620 (2016).
Scholten, M. et al. Cortical correlates of susceptibility to upper limb freezing in Parkinson’s disease. Clin. Neurophysiol. 127, 2386–2393 (2016).
Hallett, M. The intrinsic and extrinsic aspects of freezing of gait. Mov. Disord. 23, S439–S443 (2008).
Stegemöller, E. L., Allen, D. P., Simuni, T. & MacKinnon, C. D. Motor cortical oscillations are abnormally suppressed during repetitive movement in patients with Parkinson’s disease. Clin. Neurophysiol. 127, 664–674 (2016).
Fischer, P. et al. Alternating Modulation of Subthalamic Nucleus Beta Oscillations during Stepping. J. Neurosci. 38, 5111–5121 (2018).
Seeber, M., Scherer, R. & Müller-Putz, G. R. EEG Oscillations Are Modulated in Different Behavior-Related Networks during Rhythmic Finger Movements. J. Neurosci. 36, 11671–11681 (2016).
Androulidakis, A. G. et al. Amplitude modulation of oscillatory activity in the subthalamic nucleus during movement. Eur. J. Neurosci. 27, 1277–1284 (2008).
Hussain, S. J., Cohen, L. G. & Bönstrup, M. Beta rhythm events predict corticospinal motor output. Sci. Rep. 9, 18305 (2019).
Ferreri, F., Vecchio, F., Ponzo, D., Pasqualetti, P. & Rossini, P. M. Time-varying coupling of EEG oscillations predicts excitability fluctuations in the primary motor cortex as reflected by motor evoked potentials amplitude: An EEG-TMS study: EEG Coupling and Cortical Excitability. Hum. Brain Mapp. 35, 1969–1980 (2014).
Hess, C. W., Mills, K. R. & Murray, N. M. Responses in small hand muscles from magnetic stimulation of the human brain. J. Physiol. 388, 397–419 (1987).
Nomura Y., Jono Y., Tani K., Chujo Y., Hiraoka K. Corticospinal modulations during bimanual movement with different relative phases. Front Hum Neurosci. 10, 0095 (2016).
Sidhu, S. K., Hoffman, B. W., Cresswell, A. G. & Carroll, T. J. Corticospinal contributions to lower limb muscle activity during cycling in humans. J. Neurophysiol. 107, 306–314 (2012).
Lefaucheur, J. P. Motor cortex dysfunction revealed by cortical excitability studies in Parkinson’s disease: influence of antiparkinsonian treatment and cortical stimulation. Clin. Neurophysiol. 116, 244–253 (2005).
Valls-Solé, J. et al. Abnormal facilitation of the response to transcranial magnetic stimulation in patients with Parkinson’s disease. Neurology 44, 735–735 (1994).
Pascual-Leone, A., Valls-Sole, J., Brasil-Neto, J. P., Cohen, L. G. & Hallett, M. Akinesia in Parkinson’s disease. I. Shortening of simple reaction time with focal, single-pulse transcranial magnetic stimulation. Neurology 44, 884–884 (1994).
Rothwell, J. C. & Edwards, M. J. Parkinson’s disease. Handb. Clin. Neurol. 116, 535–542 (2013).
Udupa K., Chen R. Motor Cortical Plasticity in Parkinson’s Disease. Front Neurol. 4, 128 (2013).
Wu, T. et al. Effective connectivity of brain networks during self-initiated movement in Parkinson’s disease. NeuroImage 55, 204–215 (2011).
Taniwaki, T. et al. Reappraisal of the Motor Role of Basal Ganglia: A Functional Magnetic Resonance Image Study. J. Neurosci. 23, 3432–3438 (2003).
Wu, T., Hallett, M. & Chan, P. Motor automaticity in Parkinson’s disease. Neurobiol. Dis. 82, 226–234 (2015).
Lewis, S. J. G. & Shine, J. M. The next step: A common neural mechanism for freezing of gait. Neuroscientist 22, 72–82 (2016).
Begum, T. et al. Cortical mechanisms of unilateral voluntary motor inhibition in humans. Neurosci. Res 53, 428–435 (2005).
Kato, K., Vogt, T. & Kanosue, K. Brain activity underlying muscle relaxation. Front Physiol. 10, 1457 (2019).
Lee, S. Y. et al. Effects of repetitive transcranial magnetic stimulation on freezing of gait in patients with Parkinsonism. Restor. Neurol. Neurosci. 32, 743–753 (2014).
Dagan, M. et al. Multitarget transcranial direct current stimulation for freezing of gait in Parkinson’s disease: Multitarget tDCS for freezing of gait in PD. Mov. Disord. 33, 642–646 (2018).
Torrecillos, F. et al. Motor Cortex Inputs at the Optimum Phase of Beta Cortical Oscillations Undergo More Rapid and Less Variable Corticospinal Propagation. J. Neurosci. 40, 369–381 (2020).
Koehler, P. J., Nonnekes, J. & Bloem, B. R. Freezing of gait before the introduction of levodopa. Lancet Neurol. 20, 97 (2021).
Espay, A. J. et al. “On” state freezing of gait in Parkinson disease: A paradoxical levodopa-induced complication. Neurology 78, 454–457 (2012).
Cantello, R. Transcranial magnetic stimulation and Parkinson’s disease. Brain Res Rev. 38, 309–327 (2002).
Ni, Z. & Chen, R. Transcranial magnetic stimulation to understand pathophysiology and as potential treatment for neurodegenerative diseases. Transl. Neurodegener. 4, 22 (2015).
Stegemöller, E. L., Allen, D. P., Simuni, T. & MacKinnon, C. D. Altered premotor cortical oscillations during repetitive movement in persons with Parkinson’s disease. Behav. Brain Res 317, 141–146 (2017).
Snijders, A. H., Haaxma, C. A., Hagen, Y. J., Munneke, M. & Bloem, B. R. Freezer or non-freezer: Clinical assessment of freezing of gait. Parkinsonism Relat. Disord. 18, 149–154 (2012).
Rossi, S. et al. Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: Expert guidelines. Clin. Neurophysiol. 132, 269–306 (2021).
Rossini, P. M. et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: Basic principles and procedures for routine clinical and research application. An updated report from an I.F.C.N. Committee. Clin. Neurophysiol. 126, 1071–1107 (2015).
Rothwell J. C. et al. Magnetic stimulation: Motor evoked potentials. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin. Neurophysiol. (1999).
Fitzgerald, P., Fountain, S. & Daskalakis, Z. A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition. Clin. Neurophysiol. 117, 2584–2596 (2006).
Ziemann, U. et al. Consensus: Motor cortex plasticity protocols. Brain Stimul. 1, 164–182 (2008).
Oostenveld R., Fries P., Maris E., Schoffelen J. M. FieldTrip: Open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput Intell Neurosci. Published online 2011:1–9.
Moore, S. T., MacDougall, H. G. & Ondo, W. G. Ambulatory monitoring of freezing of gait in Parkinson’s disease. J. Neurosci. Methods 167, 340–348 (2008).
Bergmann, T. O., Lieb, A., Zrenner, C. & Ziemann, U. Pulsed facilitation of corticospinal excitability by the sensorimotor μ-alpha rhythm. J. Neurosci. 39, 10034–10043 (2019).
Carroll, T. J., Baldwin, E. R. L., Collins, D. F. & Zehr, E. P. Corticospinal excitability is lower during rhythmic arm movement than during tonic contraction. J. Neurophysiol. 95, 914–921 (2006).
Godfrey, S. B., Lum, P. S., Chan, E. & Harris-Love, M. L. Cortical effects of repetitive finger flexion- vs. extension-resisted tracking movements: a TMS study. J. Neurophysiol. 109, 1009–1016 (2013).
Mitchell, W. K., Baker, M. R. & Baker, S. N. Muscle responses to transcranial stimulation in man depend on background oscillatory activity: Spontaneous oscillations affect responses to transcranial stimulation. J. Physiol. 583, 567–579 (2007).
Acknowledgements
DW was supported by a grant from the German Research Foundation (WE5375/1-3). We would like to thank Prof. Peter Martus (Institute for Clinical Epidemiology and Applied Biometry, University of Tübingen, Germany) for statistical advice.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
M.T.: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B; M.S.: 1A, 1B, 1C, 2A, 2B, 2C, 3B; C.Z.: 1B, 1C, 3B; P.B.: 1B, 1C, 3B; U.Z.: 1A, 2A, 2C, 3B; D.W.: 1A, 1B, 1C, 2A, 2C, 3A, 3B. (1. Research project: 1.A. Conception, 1.B. Organization, 1.C. Execution 2. Statistical Analysis: 2.A. Design, 2.B. Execution, 2.C. Review and Critique 3. Manuscript Preparation: 3.A. Writing of the first draft, 3.B. Review and Critique).
Corresponding author
Ethics declarations
Competing interests
Marlene Topka, Marlieke Schneider, Paolo Belardinelli report no conflicts of interest. Christoph Zrenner reports stock ownership in a University of Tübingen spin-off start-up, sync2brain GmbH, commercializing real-time biosignal analysis hardware; Ulf Ziemann received grants from the German Ministry of Education and Research (BMBF), European Research Council (ERC), German Research Foundation (DFG), Janssen Pharmaceuticals NV and Takeda Pharmaceutical Company Ltd., and consulting fees from Bayer Vital GmbH, Pfizer GmbH, and CorTec GmbH, all not related to this work. Daniel Weiss received consulting fees, traveling, and research grants from the Abbott, Abbvie, Bial, Boston Scientific, Medtronic, Kyowa Kirin, Stadapharm, and research grants from the German Research Foundation (WE5375/1-3) and Michael J Fox Foundation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Topka, M., Schneider, M., Zrenner, C. et al. Motor cortex excitability is reduced during freezing of upper limb movement in Parkinson’s disease. npj Parkinsons Dis. 8, 161 (2022). https://doi.org/10.1038/s41531-022-00420-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-022-00420-w