Abstract
Triple-negative breast cancer (TNBC) patients with residual disease (RD) after neoadjuvant systemic therapy (NAST) are at high risk for recurrence. Biomarkers to risk-stratify patients with RD could help individualize adjuvant therapy and inform future adjuvant therapy trials. We aim to investigate the impact of circulating tumor DNA (ctDNA) status and residual cancer burden (RCB) class on outcomes in TNBC patients with RD. We analyze end-of-treatment ctDNA status in 80 TNBC patients with residual disease who are enrolled in a prospective multisite registry. Among 80 patients, 33% are ctDNA positive (ctDNA+) and RCB class distribution is RCB-I = 26%, RCB-II = 49%, RCB-III = 18% and 7% unknown. ctDNA status is associated with RCB status, with 14%, 31%, and 57% of patients within RCB-I, -II, and -III classes demonstrating ctDNA+ status (P = 0.028). ctDNA+ status is associated with inferior 3-year EFS (48% vs. 82%, P < 0.001) and OS (50% vs. 86%, P = 0.002). ctDNA+ status predicts inferior 3-year EFS among RCB-II patients (65% vs. 87%, P = 0.044) and shows a trend for inferior EFS among RCB-III patients (13% vs. 40%, P = 0.081). On multivariate analysis accounting for T stage and nodal status, RCB class and ctDNA status independently predict EFS (HR = 5.16, P = 0.016 for RCB class; HR = 3.71, P = 0.020 for ctDNA status). End-of-treatment ctDNA is detectable in one-third of TNBC patients with residual disease after NAST. ctDNA status and RCB are independently prognostic in this setting.
Similar content being viewed by others
Introduction
Triple-negative breast cancer (TNBC) accounts for 15% of all breast cancers and is associated with higher rates of recurrence and death compared to non-triple-negative breast cancers1. Neoadjuvant systemic therapy (NAST) is commonly employed in TNBC, and residual disease after NAST is associated with a high risk of recurrence and death2,3. The addition of adjuvant chemotherapy with capecitabine in TNBC patients with residual disease has been shown to improve outcomes, though many patients still experience disease recurrence despite the addition of adjuvant chemotherapy, and this approach may lead to overtreatment in some patients since not all patients with residual disease experience a recurrence4,5. Thus, tools to further stratify the risk of recurrence in patients with residual disease can optimize the utilization of available adjuvant therapy and improve the efficiency of clinical trials investigating novel agents in this setting. One of these risk-stratifying tools, the residual cancer burden (RCB) classification, quantitates the extent of residual disease in the breast and axillary lymph nodes following neoadjuvant chemotherapy and adds prognostic value to the binary assessment of pathological complete response vs. residual disease in predicting long-term survival6,7.
Recent studies have shown that detectable cell-free circulating tumor DNA (ctDNA) after NAST is prognostic in TNBC patients with residual disease8,9,10. Because both RCB and ctDNA status are prognostic among patients with TNBC with residual disease, assessing the combined impact of both is of interest. Most TNBC patients with residual disease will receive adjuvant radiotherapy and/or chemotherapy, and recent work has shown that adjuvant therapy may influence ctDNA status in patients with residual disease11. Thus, ctDNA status at the completion of all definitive treatment is likely to be a good indicator of the efficacy of currently available curative therapy. The impact of end-of-treatment (EOT) ctDNA status on long-term prognosis and its ability to complement the prognostic utility of the RCB classification has not been investigated. The purpose of this study was to investigate the combined impact of EOT ctDNA status and RCB class on outcomes in TNBC patients with residual disease. We hypothesized that RCB class and ctDNA status may provide complementary prognostic information.
We detected ctDNA in 33% of TNBC patients with residual disease after NAST. ctDNA status is associated with RCB class, though these two biomarkers provide complementary but not completely overlapping prognostic information, particularly in patients with RCB-II disease. These findings, if confirmed in additional studies, could provide insights into the role of ctDNA in identifying patients who are most likely to benefit from adjuvant treatment intensification. Because of the complementary prognostic information provided by RCB class and ctDNA status, we suggest that future residual disease adjuvant therapy trials for TNBC patients consider both biomarkers for patient selection/stratification.
Results
Patient characteristics and univariate analysis of clinicopathologic features and survival
81 patients with residual disease and an available EOT plasma sample for ctDNA analysis were identified (see REMARK, Supplementary Fig. 1A). ctDNA sequencing was unsuccessful in one patient, so the final study cohort includes 80 patients. There was no difference in baseline disease characteristics between the EOT ctDNA available cohort (N = 80) and all patients with residual disease (N = 268) (data not shown). Similarly, there was no difference in survival outcomes between ctDNA-available patients and all patients with residual disease (3-year EFS 70% for ctDNA-available cohort vs. 70% for all residual disease patients, P = 0.782; 3-year OS 74% for ctDNA-available cohort vs. 77% for all residual disease patients, P = 0.520).
We evaluated lower boundary VAF thresholds from 1% to 5% (Supplementary Fig. 1B) and found that a lower boundary of 3% gave the best discrimination for EFS (Supplementary Fig. 1C), so this threshold was used to define ctDNA status. Thirteen patients (16%) had one or more mutations detected at 40–60% VAF (Fig. 1). Ten of these patients had a cfDNA mutation in BRCA1 or BRCA2, and 9/10 were confirmed to be germline from clinical genetic testing reports. The remaining patient with a detectable BRCA2 ctDNA mutation did not undergo germline genetic testing and had co-existing 40–60% VAF cfDNA mutations in SRSF2 and STAG2. One patient had a BRCA1 mutation with a VAF of 21%, but this was confirmed germline on clinical genetic testing, so this patient was classified as ctDNA−. Two patients had 40–60% VAF cfDNA mutations in genes that were not represented on their clinical genetic testing panels (NF1 and CDK12); one of these had co-existing cfDNA mutations that fell within the ≥3% and <40% range and therefore was classified as ctDNA+. Two patients had 40–60% VAF cfDNA mutations in TP53, and these mutations were not detected on clinical genetic testing panels that included TP53. Both of these patients had co-existing low-frequency cfDNA mutations that rendered them ctDNA+, so this did not impact their status. Using the ≥3% but <40% or >60% threshold, the median per-patient maximum VAF (excluding confirmed germline mutations) was 4.9% with an interquartile range of 3.9–7.0% (Fig. 1). Baseline patient and tumor characteristics for the study cohort are shown in Table 1: 14% of patients were Black, 40% of patients had node-positive disease, and 24% of patients had stage III disease at presentation. Median time from completion of curative treatment to EOT plasma sample collection was 113 days (range 0–180 days; Supplementary Fig. 1D), and ctDNA was detectable in 26/80 (33%) patients (Fig. 1). The frequency of ctDNA+ status did not differ by time to sample collection when analyzing in six 30-day bins (P = 0.300) or when partitioning by median (P = 0.635) (Supplementary Fig. 1D). Patients with detectable ctDNA (ctDNA+) had a higher TNM stage (P = 0.029), and this was driven by a trend toward higher rates of lymph node involvement (P = 0.079). The rate of ctDNA positivity was associated with RCB class, with ctDNA positivity rates of 14%, 31%, and 57% in RCB-I, -II, and -III classes, respectively (P = 0.028; Table 2). Distribution of age, menopausal status, race, ethnicity, germline BRCA1/2 mutation status, T stage, NAST regimen, receipt of neoadjuvant immunotherapy, and receipt of adjuvant systemic therapy were not significantly different between ctDNA+ and ctDNA− patients. 49% of patients received adjuvant chemotherapy, and no patient received adjuvant immunotherapy (Table 1).
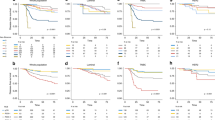
ctDNA status and RCB class are associated with survival
At a median follow-up of 31 months, there have been 21 events (4 local only, 17 distant) and 21 deaths, and the estimated 3-year EFS and OS for all patients were 70% and 74%, respectively. ctDNA+ status was significantly associated with inferior EFS (3-year EFS 48% in ctDNA+ vs. 82% in ctDNA−, log-rank P < 0.001; HR = 4.68, 95% CI 1.93–11.33, Cox proportional hazard P = 0.001) and OS (3-year OS 50% in ctDNA+ vs. 86% in ctDNA−, log-rank P = 0.002; HR = 3.57, 95% CI 1.50–8.50, Cox proportional hazard P = 0.004) (Fig. 2). There was no apparent association between the interval from surgery to ctDNA assessment and the interval from ctDNA assessment to EFS event in patients who experienced recurrence (Supplementary Fig. 1E). Among ctDNA+ patients who experienced an EFS event, the median time from ctDNA detection to the event was 4.7 months. Similarly, increasing RCB class was associated with significantly worse EFS and OS. Both 3-year EFS and OS for patients with RCB class I, II, and III were 100%, 79%, and 23%, respectively (log-rank P < 0.001 for both; Supplementary Fig. 2). On univariate analysis, higher presenting T stage (T3–T4 vs. T1–2), positive nodal status (node-positive vs. negative), and higher TNM stage (stage III vs. I) were also associated with significantly worse EFS and OS (Table 3).
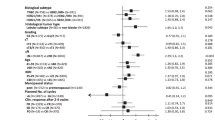
ctDNA complements RCB in prognosticating TNBC patients with residual disease
Since RCB is a validated measure of recurrence risk after NAST, we sought to examine the utility of classifying patients by both RCB class and ctDNA status to determine if dual classification provided additional prognostic information. There were no EFS or OS events in patients with RCB-I, so the prognostic impact of ctDNA in the RCB-I group could not be evaluated (Supplementary Fig. 2). In patients with RCB-II disease, ctDNA+ status was significantly associated with inferior EFS (3-year EFS 65% in ctDNA+ vs. 87% in ctDNA−, log-rank P = 0.044; HR = 4.17, 95% CI 0.92–18.79, Cox proportional hazard P = 0.063) and a trend toward inferior OS (3-year OS 61% for ctDNA+ vs. 76% for ctDNA−, log-rank P = 0.077; HR = 3.30, 95% CI: 0.82–13.33, Cox proportional hazard P = 0.094). In patients with RCB-III disease, ctDNA+ status was also associated with a trend toward inferior EFS (3-year EFS 13% for ctDNA+ vs. 40% for ctDNA−, log-rank P = 0.081; HR = 3.29, 95% CI: 0.81–13.37, Cox proportional hazard P = 0.096) and a trend toward inferior OS (3-year OS 13% for ctDNA+ vs. 40% for ctDNA−, log-rank P = 0.201; HR = 2.41, 95% CI: 0.60–9.60, Cox proportional hazard P = 0.214) (Fig. 3). In a multivariate Cox regression analysis (including T stage, nodal status, RCB class, and ctDNA status), RCB class and ctDNA status remained prognostic for EFS (HR = 5.16, 95% CI: 1.36–19.52, P = 0.016 (RCB class); HR = 3.71, 95% CI: 1.23–11.21, P = 0.020 (ctDNA status)). For OS, RCB class remained prognostic (HR = 3.53, 95% CI: 1.10–11.35, P = 0.034) and ctDNA status showed a prognostic trend (HR = 2.59, 95% CI: 0.87–7.77, P = 0.089) (Table 4).
Discussion
In this study, we examined EOT ctDNA status and its combined use with RCB class as prognostic markers in TNBC patients with residual disease after NAST. ctDNA positivity was noted in 33% of patients, and ctDNA status was highly correlated with RCB class. We examined the association of EOT ctDNA status with outcomes in TNBC patients with residual disease after NAST and evaluated the combined use of ctDNA status and RCB class in this population.
Our ctDNA positivity rate and 3-year EFS and OS are in line with previous studies8,9,10. Though we observed favorable 3-year EFS and OS in ctDNA− patients compared to ctDNA+ patients, the fact that approximately 15–20% of ctDNA− patients do experience an EFS event indicates that ctDNA status alone likely cannot be used to recommend against adjuvant therapy in TNBC patients with residual disease. The RCB model was originally developed on a cohort of 241 patients treated with neoadjuvant chemotherapy12, and it has since been validated in numerous independent cohorts as a robust measure of long-term recurrence risk in breast cancer patients treated with NAST6,7,13. RCB is highly prognostic in TNBC, with 5-year relapse-free survival rates of approximately 94%, 89%, 62%, and 26% in patients with RCB-0 (pathologic complete response (pCR)), RCB-I, RCB-II, and RCB-III disease, respectively6. Despite its excellent performance, RCB is not a perfect model for recurrence risk and can be improved upon to aid in personalized decisions for an individual patient. The distribution of RCB classes in our study is quite similar to the distribution among 1004 TNBC patients with residual disease that was recently reported by Yau et al.7. We show that for RCB II patients, incorporating ctDNA status can identify a group that has 3-year EFS > 90%, for whom escalation of adjuvant systemic therapy with additional investigational agents may not yield a clinically meaningful survival benefit. More than two-thirds of TNBC patients with the residual disease have RCB-I/II, so this observation, if validated in other studies, can have potential clinical implications for a large proportion of patients. Similarly, the observation that 50% of patients with RCB-III disease who were ctDNA- did not experience an EFS event suggests that even the presence of a large amount of residual disease is not an absolute indicator of the eventual development of metastatic disease. On the other hand, the presence of both RCB-III disease and ctDNA+ status was associated with very dismal outcomes. These hypothesis-generating findings from our study regarding complementary prognostic information of ctDNA status and RCB should be confirmed in other data sets.
The observation that 30–40% of TNBC patients with residual disease who receive adjuvant systemic therapy develop recurrent disease4,5 highlights the urgent need to develop more effective adjuvant treatments for high-risk patients. Robust prognostic and predictive biomarkers of individual patients’ recurrence risk and therapeutic vulnerabilities will enable risk-adapted and personalized adjuvant therapy approaches, thus maximizing the efficacy of therapy and minimizing both physical and financial toxicity from unnecessary or ineffective therapy. Assessing novel therapeutic agents in the adjuvant setting for TNBC patients with the residual disease is an active area of investigation, and our results suggest that incorporating RCB class and ctDNA status into the design of these trials may improve trial efficiency.
Two recent experiences have reported on the utility of ctDNA as a prognostic marker in TNBC patients with residual disease after NAST. Radovich et al. analyzed 196 patients who were prospectively enrolled in the BRE12-158 study that randomized TNBC patients with residual disease after NAST to treatment of physician’s choice versus genomically-directed therapy. This study noted detectable ctDNA in 64% of patients and demonstrated that the presence of detectable ctDNA in patients with residual disease after NAST was associated with significantly inferior disease-free survival, distant-disease-free survival, and OS9,14. Similarly, an analysis of 22 TNBC patients enrolled in the I-SPY2 trial demonstrated that post-NAST (but before surgery) ctDNA was detectable in 14% of patients and was associated with an increased risk of distant recurrence8. The significant difference in ctDNA positivity rates in these two studies, despite both being sampled after neoadjuvant systemic therapy, may be explained by differences in methodology and ctDNA assessment time-point. ctDNA assessment in BRE12–158 was via a standardized multiplex panel (FoundationACT or FoundationOne), while in I-SPY2 it was based on an assessment of 12–16 personalized somatic mutations detected in patients’ primary tumors. In both BRE12-158 and I-SPY2 experiences, ctDNA assessment was performed before patients had received all definitive therapy. A recent small study of 11 TNBC patients with residual disease after NAST who required adjuvant radiotherapy reported that 3/11 (27%) patients had detectable ctDNA prior to radiotherapy, and that detection of cancer-associated variant alleles in plasma decreased dramatically in 2/3 (67%) of these patients during and after radiotherapy11. Though the small size of this study precludes any definitive conclusions, it demonstrates that EOT ctDNA assessment may be fundamentally more informative than an assessment that occurs before patients have completed all definitive therapy. It is possible that standard-of-care adjuvant systemic therapy (i.e., capecitabine or pembrolizumab) may also influence ctDNA status, and ongoing studies are evaluating serial ctDNA status in early-stage TNBC patients receiving adjuvant capecitabine (NCT04768426). Our study differs from BRE12–158 and I-SPY2 in that we assessed patients at the end of all curative therapy. Importantly, 3-year EFS and OS for our study population are in line with what is expected for contemporary patients when all degrees of residual disease are considered.
The goal of adjuvant treatment intensification is to eradicate occult micrometastatic disease. In our study, the median interval from detecting ctDNA to an EFS event was 4.7 months and most of the EFS events (81%) involved distant recurrence, suggesting that ctDNA positivity is a harbinger of rapid clinical disease recurrence. Our observation is similar to findings recently reported from the c-TRAK TN trial, which identified that ctDNA positivity was associated with a 4.1-month lead time until clinical detection of recurrence10. This is a clinically meaningful observation, as it has implications for the sequence of adjuvant systemic and local therapies and the design of trials incorporating adjuvant systemic therapy for TNBC patients with residual disease. Most patients in the CREATE-X trial4 completed radiotherapy before initiating capecitabine, and the current National Comprehensive Cancer Network (NCCN) guidelines indicate that capecitabine should be given after completion of radiotherapy (NCCN Version 2.2022). The short interval between the detection of ctDNA and clinical recurrence suggests that the window of opportunity for adjuvant systemic therapy to eradicate non-locoregional micrometastatic disease may be very small. The findings from our study and the cTRAK TN trial suggest that future investigations might consider swift initiation of adjuvant systemic therapy prior to radiotherapy in patients at a very high risk of distant recurrence, as that risk might significantly outweigh the risk of locoregional recurrence.
Our study has several limitations. First, ctDNA status was assessed retrospectively in archival plasma samples, though the collection of all blood and clinical follow-up data was performed prospectively as part of our ongoing registry (PROGECT; NCT02302742). We also did not have radiographic staging performed concurrently with plasma collection, and recent data suggest that many patients with detectable ctDNA, especially those with residual nodal disease after NAST, may have overt metastatic disease10. An additional limitation is that the ctDNA assessment was only performed at a single time point, and this occurred over a period of six months. ctDNA status may be a dynamic biomarker, with ctDNA+ patients converting to ctDNA- as a consequence of adjuvant therapy11, or ctDNA− patients converting to ctDNA+ on later assessments10. We also did not have comprehensive germline sequencing available for these patients, though we were able to corroborate the majority of 40–60% VAF cfDNA mutations as germline, and/or the presence of a 40–60% VAF cfDNA mutation did not change their status, since nearly all of those patients had co-existing low-frequency cfDNA mutation(s) that otherwise met the criteria for ctDNA+ status. Interestingly, in the single patient with a detectable 40–60% VAF cfDNA BRCA2 mutation who did not undergo germline genetic testing, we also found co-existing 40–60% VAF cfDNA mutations in SRSF2 and STAG2. Both mutations are seen commonly in patients with myelodysplastic syndrome (MDS)15,16, and this patient did receive a subsequent diagnosis of MDS. We suspect that this patient carried a germline mutation in BRCA2, which is known to increase the risk of myeloid malignancy17, and that the SRSF2 and STAG2 cfDNA mutations were arising from dysplastic myeloblasts rather than her TNBC.
All patients in our study had residual disease so we are unable to report on the impact of ctDNA status on prognosis in patients with pCR. Neoadjuvant treatment among the 80 patients in our series varied, with most patients receiving standard chemotherapy treatment of physician’s choice, and some patients (23%) receiving chemotherapy plus immunotherapy on a clinical trial (NCT03639948). Though this heterogeneous treatment and 6-month collection period limit the interpretation of our results in the context of a defined systemic therapy regimen or defined post-treatment timepoint, they reflect real-world practice. The number of patients who received neoadjuvant immunotherapy is small and precludes a subset analysis of ctDNA status within this population, but the inclusion of these patients is relevant given the recent approval of neoadjuvant pembrolizumab with chemotherapy in high-risk early-stage TNBC patients18. It is important to interpret our findings accordingly, since most TNBC patients will now receive immunotherapy in the neoadjuvant and adjuvant setting, and data suggest that ctDNA dynamics during treatment with pembrolizumab are prognostic in breast cancer19. Lastly, we used a non-personalized sequencing methodology that assesses mutations in 275 cancer-related genes, and we dichotomized ctDNA status based on an internally optimal lower boundary VAF threshold. This leads to inherent bias and highlights the need to validate our methodology in an independent dataset. Tumor-informed approaches that interrogate ctDNA for discrete alterations that are known to exist in the primary tumor may lead to improved sensitivity and specificity. Despite the limitations of our study, we demonstrate that end-of-treatment ctDNA status is highly prognostic and that its combined use with RCB class provides better prognostication than either biomarker alone.
Methods
Patients and samples
The study population included patients with stage I-III TNBC (defined as estrogen receptor (ER) ≤ 10%, progesterone receptor (PR) ≤ 10%, and negative for human epidermal growth factor receptor 2 (HER2) by ASCO-CAP criteria20) who were enrolled on an IRB-approved multisite prospective registry (PROGECT; NCT02302742) between 2011 and 2020 and had residual disease after NAST with available EOT plasma samples. EOT plasma samples were collected 1–6 months after completion of all curative treatment (surgery, chemotherapy, and/or radiotherapy, whichever ended last). RCB was calculated using defined clinicopathologic features as previously described12. Demographic, clinical, pathologic, and treatment information was collected (Table 1), and participants were prospectively followed for recurrence and survival. Patients received systemic and locoregional treatment as per the recommendations of their treating physicians. All patients provided written informed consent, and the study was approved by the institutional review board at the University of Kansas Medical Center.
Blood collection, processing, and storage
Blood was collected into acid-citrate dextrose (ACD) blood tubes and processed within four hours of collection using standard blood processing methods. Briefly, whole blood was centrifuged once at 1300 × g for 10 min in a swinging bucket centrifuge with the brakes turned off. The upper plasma was collected without disrupting the buffy coat layer, aliquoted (1 mL/aliquot) into prelabeled cryovials, and stored frozen at −80 °C. Cell-free DNA was isolated from 2 mL of ACD plasma using the QIAamp Circulating Nucleic Acid kit (Qiagen) following the manufacturer’s protocol for the vacuum manifold method and then sequenced.
ctDNA sequencing
ctDNA quality was assessed by TapeStation (Agilent) and then concentrated approximately three-fold using a Savant DNA SpeedVac on the no-heat setting. Libraries were prepared from concentrated ctDNA using the QIAseq Targeted DNA Human Comprehensive Cancer Panel (Qiagen) which targets exons of 275 genes. The quality and concentration of the prepared libraries were assessed by TapeStation. Equimolar libraries were pooled (~16–19 samples/pool) and 151-cycle paired-end sequencing was performed on an Illumina NextSeq 550 instrument using a high-output flow cell. Raw sequence data in FASTQ format were processed through CLC Genomics Workbench (Qiagen) against GRCh37 to generate variant call format (vcf) files as well as sequencing quality metrics. Patients with mutations only in DNMT3A, TET2, ASXL1, or JAK2 were classified as ctDNA- as these mutations likely arise from clonal hematopoiesis of indeterminate potential (CHIP)21. Patients with detectable pathogenic or likely pathogenic variants (variant allelic frequency (VAF) ≥ 3.0% but <40% or >60%) were considered ctDNA+. When possible, mutations detected with a frequency of ≥40% were corroborated as germline by referencing clinical genetic testing reports. Patients with one or more mutation(s) detected at 40–60% frequency, confirmed or unconfirmed germline, without any mutation(s) detected in the ≥3.0% but <40% or >60% range were classified as ctDNA−. Patients with one or more mutation(s) detected in the ≥3.0% but <40% or >60% range were classified as ctDNA+ (unless all confirmed germline), regardless of whether additional mutations at 40–60% were detected.
Sample size and statistical analysis
Baseline characteristics were compared across groups by chi-squared or Fisher’s exact tests, with Mann–Whitney U test used for continuous variables. Event-free survival (EFS) and overall survival (OS) were estimated according to the Kaplan-Meier method and compared across groups by log-rank test, followed by Cox regression analysis. EFS was defined as the time from diagnosis to first recurrence (invasive ipsilateral breast, invasive local/regional, or distant), or to death from breast cancer. OS was defined as the time from diagnosis to death from any cause. Patients were censored on the date of last contact if an event had not been observed. All reported P values and confidence intervals (CI) are from two-sided tests. P values <0.05 were considered statistically significant. All analyses were conducted using SPSS Statistics version 27 (IBM Corporation).
With an anticipated ctDNA positivity rate of 50% and 3-year event-free survival of 55% in ctDNA+ patients and 80% in ctDNA− patients based on previously published data8,9, we projected that we would need a minimum sample size of 60 patients to have 86% power to detect this 25% difference in 3-year EFS between ctDNA− and ctDNA+ negative and positive patients with a one-sided α = 0.05. Because of the uncertainty in the ctDNA positivity rate and effect size, we elected to sequence 80 samples to ensure adequate statistical power.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to them containing information that could compromise research participant privacy. Additionally, explicit consent to deposit participant-level data was not obtained from participants, and many participants are deceased or lost to follow-up, which precludes obtaining consent for the data deposition. However, a limited set of de-identified data can be made available by the corresponding author (P.S.) upon reasonable request.
References
Li, X. et al. Triple-negative breast cancer has worse overall survival and cause-specific survival than non-triple-negative breast cancer. Breast Cancer Res. Treat. 161, 279–287 (2017).
Liedtke, C. et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J. Clin. Oncol. 26, 1275–1281 (2008).
Spring, L. M. et al. Pathologic complete response after neoadjuvant chemotherapy and impact on breast cancer recurrence and survival: a comprehensive meta-analysis. Clin. Cancer Res. 26, 2838–2848 (2020).
Masuda, N. et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N. Engl. J. Med. 376, 2147–2159 (2017).
Mayer, I. A. et al. Randomized phase III postoperative trial of platinum-based chemotherapy versus capecitabine in patients with residual triple-negative breast cancer following neoadjuvant chemotherapy: ECOG-ACRIN EA1131. J. Clin. Oncol. 39, 2539–2551 (2021).
Symmans, W. F. et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J. Clin. Oncol. 35, 1049–1060 (2017).
Yau, C. et al. Residual cancer burden after neoadjuvant chemotherapy and long-term survival outcomes in breast cancer: a multicentre pooled analysis of 5161 patients. Lancet Oncol. 23, 149–160 (2022).
Magbanua, M. J. M. et al. Circulating tumor DNA in neoadjuvant-treated breast cancer reflects response and survival. Ann. Oncol. 32, 229–239 (2021).
Radovich, M. et al. Association of circulating tumor DNA and circulating tumor cells after neoadjuvant chemotherapy with disease recurrence in patients with triple-negative breast cancer: preplanned secondary analysis of the BRE12-158 randomized clinical trial. JAMA Oncol. 6, 1410–1415 (2020).
Turner, N. et al. in San Antonio Breast Cancer Symposium.
Kim, H. et al. Dynamics of circulating tumor DNA during postoperative radiotherapy in patients with residual triple-negative breast cancer following neoadjuvant chemotherapy: a prospective observational study. Breast Cancer Res. Treat. 189, 167–175 (2021).
Symmans, W. F. et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J. Clin. Oncol. 25, 4414–4422 (2007).
Symmans, W. F. et al. Assessment of residual cancer burden and event-free survival in neoadjuvant treatment for high-risk breast cancer: an analysis of data from the I-SPY2 randomized clinical trial. JAMA Oncol. 7, 1654–1663 (2021).
Schneider, B. P. et al. BRE12-158: a postneoadjuvant, randomized phase II trial of personalized therapy versus treatment of physician’s choice for patients with residual triple-negative breast cancer. J. Clin. Oncol. https://doi.org/10.1200/JCO.21.01657 (2021).
Thota, S. et al. Genetic alterations of the cohesin complex genes in myeloid malignancies. Blood 124, 1790–1798 (2014).
Wu, S. J. et al. The clinical implication of SRSF2 mutation in patients with myelodysplastic syndrome and its stability during disease evolution. Blood 120, 3106–3111 (2012).
Friedenson, B. The BRCA1/2 pathway prevents hematologic cancers in addition to breast and ovarian cancers. BMC Cancer 7, 152 (2007).
Schmid, P. et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 382, 810–821 (2020).
Bratman, S. V. et al. Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nat. Cancer 1, 873–881 (2020).
Wolff, A. C. et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. Arch. Pathol. Lab. Med. 142, 1364–1382 (2018).
Buscarlet, M. et al. DNMT3A and TET2 dominate clonal hematopoiesis and demonstrate benign phenotypes and different genetic predispositions. Blood 130, 753–762 (2017).
Acknowledgements
We acknowledge the University of Kansas Cancer Center’s Biospecimen Repository Core Facility and staff, including Michele Park, Alex Webster, and Lauren Dimartino who are supported, in part, by the NIH/NCI Cancer Center Support Grant P30CA168524. We also acknowledge support from P30CA168524 (Cancer Center Support Grant; University of Kansas Cancer Center), P20GM130423 (Kansas Institute for Precision Medicine COBRE; SRS), KL2TR002367 (KL2 Mentored Career Development Award; SRS). A.K.G. is the Chancellor’s Distinguished Chair in Biomedical Sciences Endowed Professor. P.S. is the Chancellor’s Chair of Therapeutics Cancer Treatment Endowed Professor. These data were presented in part at the 2021 San Antonio Breast Cancer Symposium.
Author information
Authors and Affiliations
Contributions
Concept and design: S.R.S., A.K.G., and P.S. Acquisition, analysis, or interpretation of data: S.R.S., B.F.K., R.Y., K.S., J.M.S., Q.J.K., A.P.O., L.E.N., M.E., J.H., T.H., S.H., K.I., H.B.P., A.K.G., and P.S. Drafting of the manuscript: S.R.S., R.Y., and P.S. Critical revision of the paper for important intellectual content: S.R.S., B.F.K., R.Y., K.S., J.M.S., Q.J.K., A.P.O., L.E.N., M.E., J.H., T.H., S.H., K.I., H.B.P., A.K.G., and P.S. Statistical analysis: S.R.S., B.F.K., and R.Y. Administrative, technical, or material support: T.H., S.H., K.I., H.B.P., and A.K.G. Supervision: S.R.S., A.K.G., and P.S.
Corresponding author
Ethics declarations
Competing interests
A.P.O.: Consulting honoraria from Pfizer, Puma Biotechnology, Novartis, Daiichi Sankyo, Astra Zeneca, and Seattle Genetics; A.K.G.: Co-founder of Sinochips Diagnostics, serves as a scientific advisory board member to Biovica, Clara Biotech, and Sinochips Diagnostics, and receives research funding from Predicine and VITRAC Therapeutics; P.S.: Research funding from Novartis, Merck, Gilead, and BMS; serves as a consultant/advisor to AstraZeneca, Novartis, Merck, GSK, Pfizer, Sanofi, and Genzyme; and receives royalties from UpToDate. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stecklein, S.R., Kimler, B.F., Yoder, R. et al. ctDNA and residual cancer burden are prognostic in triple-negative breast cancer patients with residual disease. npj Breast Cancer 9, 10 (2023). https://doi.org/10.1038/s41523-023-00512-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-023-00512-7
This article is cited by
-
Circulating tumour mutation detection in triple-negative breast cancer as an adjunct to tissue response assessment
npj Breast Cancer (2024)
-
Use of Circulating Tumor DNA (ctDNA) for Early Molecular Detection of Breast Cancer Relapse in Patients with Triple-Negative Breast Cancer (TNBC)
Current Breast Cancer Reports (2023)