Abstract
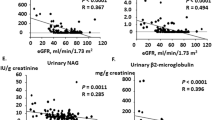
Individuals with primary aldosteronism (PA) exhibit glomerular hyperfiltration, which may conceal underlying kidney damage. This observational cohort study enrolled 760 coronary artery disease-naive patients diagnosed with PA between January 1, 2007 and December 31, 2018 (male, 45%; mean age, 52.3 ± 11.9 years). The baseline estimated glomerular filtration rate (eGFR) was calculated using the 2021 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, which includes serum creatinine and cystatin C but omits the race variable. During a mean follow-up of 5.8 ± 3.2 years, new-onset composite cardiovascular events (total death, non-fatal myocardial infarction, and coronary revascularization procedure) occurred at a crude incidence rate of 10.9 per 1,000 person-years. Multivariable Cox proportional hazards analysis showed that baseline eGFR was independently associated with composite cardiovascular events (hazard ratio [HR], 0.98 [95% CI, 0.97–0.99]). Penalized splines smoothing in multivariable regression analysis demonstrated that the risk of composite cardiovascular events increased negatively and linearly when patients had a baseline eGFR less than 85 mL/min/1.73 m2. Patients with baseline eGFR <85 mL/min/1.73 m2 were independently associated with higher risks of composite cardiovascular events (HR, 2.39 [95% CI, 1.16–4.93]), all-cause mortality (HR, 4.63 [95% CI, 1.59–13.46]), and adverse kidney events (sub-distribution HR, 5.96 [95% CI, 3.69–9.62], with mortality as a competing risk). Our data support baseline eGFR as a predictor for new-onset adverse cardiorenal events and emphasizes the importance of the early detection of kidney function impairment in hypertensive patients with PA. We also firstly validate the 2021 race-free CKD-EPI eGFR equation in Asian patents with PA.

Even with the glomerular hyperfiltration phenomenon, baseline eGFR in patients with primary aldosteronism is associated with subsequent cardiorenal outcomes. The results also firstly point to the validity of the 2021 race-free CKD-EPI eGFR equation in healthcare and clinical decision-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Takeda Y, Karashima S, Yoneda T. Primary aldosteronism, diagnosis and treatment in Japan. Rev Endocr Metab Disord. 2011;12:21–5.
Huang KH, Yu CC, Hu YH, Chang CC, Chan CK, Liao SC, et al. Targeted treatment of primary aldosteronism - the consensus of Taiwan Society of Aldosteronism. J Formos Med Assoc. 2019;118:72–82.
Xu Z, Yang J, Hu J, Song Y, He W, Luo T, et al. Primary aldosteronism in patients in China with recently detected hypertension. J Am Coll Cardiol. 2020;75:1913–22.
Yoon M, Hong N, Ha J, Lee CJ, Ku CR, Rhee Y, et al. Prevalence and clinical characteristics of primary aldosteronism in a tertiary-care center in Korea. Hypertens Res. 2022;45:1418–29.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, Williams GH, et al. The unrecognized prevalence of primary aldosteronism: a cross-sectional study. Ann Intern Med. 2020;173:10–20.
TAIPAI Study Group, Wu VC, Chueh SC, Chang HW, Lin LY, Liu KL, et al. Association of kidney function with residual hypertension after treatment of aldosterone-producing adenoma. Am J Kidney Dis. 2009;54:665–73.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168:80–5.
Reincke M, Fischer E, Gerum S, Merkle K, Schulz S, Pallauf A, et al. Observational study mortality in treated primary aldosteronism: the German Conn’s registry. Hypertension. 2012;60:618–24.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension. 2018;71:530–7.
Wu VC, Wang SM, Huang KH, Tsai YC, Chan CK, Yang SY, et al. Long-term mortality and cardiovascular events in patients with unilateral primary aldosteronism after targeted treatments. Eur J Endocrinol. 2022;186:195–205.
Wu VC, Kuo CC, Wang SM, Liu KL, Huang KH, Lin YH, et al. Primary aldosteronism: changes in cystatin C-based kidney filtration, proteinuria, and renal duplex indices with treatment. J Hypertens. 2011;29:1778–86.
Ogata H, Yamazaki Y, Tezuka Y, Gao X, Omata K, Ono Y, et al. Renal injuries in primary aldosteronism: quantitative histopathological analysis of 19 patients with primary adosteronism. Hypertension. 2021;78:411–21.
Monticone S, Sconfienza E, D’Ascenzo F, Buffolo F, Satoh F, Sechi LA, et al. Renal damage in primary aldosteronism: a systematic review and meta-analysis. J Hypertens. 2020;38:3–12.
Fernandez-Argueso M, Pascual-Corrales E, Bengoa Rojano N, Garcia Cano A, Jimenez Mendiguchia L, Araujo-Castro M. Higher risk of chronic kidney disease and progressive kidney function impairment in primary aldosteronism than in essential hypertension. Case-control study. Endocrine. 2021;73:439–46.
Ribstein J, Du Cailar G, Fesler P, Mimran A. Relative glomerular hyperfiltration in primary aldosteronism. J Am Soc Nephrol. 2005;16:1320–5.
Utsumi T, Kawamura K, Imamoto T, Nagano H, Tanaka T, Kamiya N, et al. Preoperative masked renal damage in Japanese patients with primary aldosteronism: identification of predictors for chronic kidney disease manifested after adrenalectomy. Int J Urol. 2013;20:685–91.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–81.
Zhang R, Zheng L, Sun Z, Zhang X, Li J, Hu D, et al. Decreased glomerular filtration rate is associated with mortality and cardiovascular events in patients with hypertension: a prospective study. PLoS ONE. 2011;6:e27359.
Wang X, Wang Y, Patel UD, Barnhart HX, Li Z, Li H, et al. Comparison of associations of reduced estimated glomerular filtration rate with stroke outcomes between hypertension and no hypertension. Stroke. 2017;48:1691–4.
Lees JS, Welsh CE, Celis-Morales CA, Mackay D, Lewsey J, Gray SR, et al. Glomerular filtration rate by differing measures, albuminuria and prediction of cardiovascular disease, mortality and end-stage kidney disease. Nat Med. 2019;25:1753–60.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension. 2018;72:658–66.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Vyas DA, Eisenstein LG, Jones DS. Hidden in plain sight - reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020;383:874–82.
Delgado C, Baweja M, Burrows NR, Crews DC, Eneanya ND, Gadegbeku CA, et al. Reassessing the inclusion of race in diagnosing kidney diseases: an interim report from the NKF-ASN Task Force. J Am Soc Nephrol. 2021;32:1305–17.
Gama RM, Kalyesubula R, Fabian J, Mahalingasivam V. NICE takes ethnicity out of estimating kidney function. BMJ. 2021;374:n2159.
Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N. Engl J Med. 2021;385:1737–49.
Delgado C, Baweja M, Crews DC, Eneanya ND, Gadegbeku CA, Inker LA, et al. A unifying approach for GFR estimation: recommendations of the NKF-ASN task force on reassessing the inclusion of race in diagnosing kidney disease. Am J Kidney Dis. 2022;79:268–88.e1.
Fu EL, Coresh J, Grams ME, Clase CM, Elinder CG, Paik J, et al. Removing race from the CKD-EPI equation and its impact on prognosis in a predominantly White European population. Nephrol Dial Transplant. 2023;38:119–28.
Hsu CY, Yang W, Parikh RV, Anderson AH, Chen TK, Cohen DL, et al. Race, genetic ancestry, and estimating kidney function in CKD. N Engl J Med. 2021;385:1750–60.
Wu VC, Hu YH, Wu CH, Kao CC, Wang CY, Yang WS, et al. Administrative data on diagnosis and mineralocorticoid receptor antagonist prescription identified patients with primary aldosteronism in Taiwan. J Clin Epidemiol. 2014;67:1139–49.
Wu VC, Yang SY, Lin JW, Cheng BW, Kuo CC, Tsai CT, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta. 2011;412:1319–25.
Wu VC, Hu YH, Er LK, Yen RF, Chang CH, Chang YL, et al. Case detection and diagnosis of primary aldosteronism - The consensus of Taiwan Society of Aldosteronism. J Formos Med Assoc. 2017;116:993–1005.
Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367:20–9.
Wu VC, Wu CH, Huang TM, Wang CY, Lai CF, Shiao CC, et al. Long-term risk of coronary events after AKI. J Am Soc Nephrol. 2014;25:595–605.
Iwakura Y, Morimoto R, Kudo M, Ono Y, Takase K, Seiji K, et al. Predictors of decreasing glomerular filtration rate and prevalence of chronic kidney disease after treatment of primary aldosteronism: renal outcome of 213 cases. J Clin Endocrinol Metab. 2014;99:1593–8.
Moore DF. Applied survival analysis using R. Switzerland: Springer; 2016.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74.
Meng Y, Chen K, Xie A, Liu Y, Huang J. Screening for unilateral aldosteronism should be combined with the maximum systolic blood pressure, history of stroke and typical nodules. Medicine. 2022;101:e31313.
Puar TH, Loh WJ, Lim DS, Loh LM, Zhang M, Foo RS, et al. Aldosterone-potassium ratio predicts primary aldosteronism subtype. J Hypertens. 2020;38:1375–83.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Wu VC, Chan CK, Chueh JS, Chen YM, Lin YH, Chang CC, et al. Markers of kidney tubular function deteriorate while those of kidney tubule health improve in primary aldosteronism after targeted treatments. J Am Heart Assoc. 2023;12:e028146.
Rothenbacher D, Rehm M, Iacoviello L, Costanzo S, Tunstall-Pedoe H, Belch JJF, et al. Contribution of cystatin C- and creatinine-based definitions of chronic kidney disease to cardiovascular risk assessment in 20 population-based and 3 disease cohorts: the BiomarCaRE project. BMC Med. 2020;18:300.
Sechi LA, Novello M, Lapenna R, Baroselli S, Nadalini E, Colussi GL, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA. 2006;295:2638–45.
Sechi LA, Di Fabio A, Bazzocchi M, Uzzau A, Catena C. Intrarenal hemodynamics in primary aldosteronism before and after treatment. J Clin Endocrinol Metab. 2009;94:1191–7.
Fu Y, Hall JE, Lu D, Lin L, Manning RD Jr., Cheng L, et al. Aldosterone blunts tubuloglomerular feedback by activating macula densa mineralocorticoid receptors. Hypertension. 2012;59:599–606.
Chen CW, Tsai CH, Hung CS, Tsai IJ, Chiu YW, Chang CC, et al. Comparison of cystatin C-based and creatinine-based glomerular filtration rate in the prediction of postoperative residual hypertension in aldosterone-producing adenoma patients after adrenalectomy. Clin Chim Acta. 2021;520:147–53.
Wuerzner G, Pruijm M, Maillard M, Bovet P, Renaud C, Burnier M, et al. Marked association between obesity and glomerular hyperfiltration: a cross-sectional study in an African population. Am J Kidney Dis. 2010;56:303–12.
Stefansson VT, Schei J, Jenssen TG, Melsom T, Eriksen BO. Central obesity associates with renal hyperfiltration in the non-diabetic general population: a cross-sectional study. BMC Nephrol. 2016;17:172.
Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Kucuksumer ZS, Ortiz A, et al. Renal hyperfiltration defined by high estimated glomerular filtration rate: A risk factor for cardiovascular disease and mortality. Diabetes Obes Metab. 2019;21:2368–83.
Penno G, Orsi E, Solini A, Bonora E, Fondelli C, Trevisan R, et al. Renal hyperfiltration is independently associated with increased all-cause mortality in individuals with type 2 diabetes: a prospective cohort study. BMJ Open Diabetes Res Care. 2020;8:e001481.
Dupuis ME, Nadeau-Fredette AC, Madore F, Agharazii M, Goupil R. Association of glomerular hyperfiltration and cardiovascular risk in middle-aged healthy individuals. JAMA Netw Open. 2020;3:e202377.
Wen CP, Cheng TY, Tsai MK, Chang YC, Chan HT, Tsai SP, et al. All-cause mortality attributable to chronic kidney disease: a prospective cohort study based on 462 293 adults in Taiwan. Lancet. 2008;371:2173–82.
Lu YC, Liu KL, Wu VC, Wang SM, Lin YH, Chueh SJ, et al. Factors associated with renal function change after unilateral adrenalectomy in patients with primary aldosteronism. Int J Urol. 2022;29:831–7.
Reincke M, Rump LC, Quinkler M, Hahner S, Diederich S, Lorenz R, et al. Risk factors associated with a low glomerular filtration rate in primary aldosteronism. J Clin Endocrinol Metab. 2009;94:869–75.
Brem AS, Morris DJ, Gong R. Aldosterone-induced fibrosis in the kidney: questions and controversies. Am J Kidney Dis. 2011;58:471–9.
Chen YY, Lin YH, Huang WC, Chueh E, Chen L, Yang SY, et al. Adrenalectomy improves the long-term risk of end-stage renal disease and mortality of primary aldosteronism. J Endocr Soc. 2019;3:1110–26.
Acknowledgements
The authors thank Miss Fang-Yu Yeh for her assistant in statistical analysis. The authors also thank the staff of the Second and Seventh Core Labs, Department of Medical Research at National Taiwan University Hospital for technical assistance. The authors express sincere gratitude to all staffs of the Taiwan Clinical Trial Consortium (TCTC).
the TAIPAI study group
Vin-Cent Wu1,3, Tai-Shuan Lai1, Jeff S. Chueh4, Shao-Yu Yang1, Kao-Lang Liu5, Chin-Chen Chang5, Bo-Ching Lee5, Shuo-Meng Wang4, Kuo-How Huang4, Po-Chih Lin2, Yen-Hung Lin2,3, Chi-Sheng Hung2, Lian-Yu Lin2,6, Shih-Cheng Liao5, Ching-Chu Lu5, Chieh-Kai Chan7, Leay-Kiaw Er8, Ya-Hui Hu8, Che-Hsiung Wu8, Yao-Chou Tsai8, Zheng-Wei Chen6, Chien-Ting Pan6, Che-Wei Liao9, Cheng-Hsuan Tsai2, Yi-Yao Chang10, Chen-Hsun Ho11, Wei-Chieh Huang12, Ying-Ying Chen13
Funding
This work was supported by the National Science and Technology Council, Taiwan (110-2314-B-002-239, 110-2314-B-002-241); National Health Research Institutes, Taiwan (PH 102-SP-09); National Taiwan University Hospital (109-S4634, UN109-041, UN110-030); Ministry of Health and Welfare, Taiwan (110-TDU-B-212-124005); Mrs. Hsiu-Chin Lee Kidney Research Fund. The funds played no role in the study design, data collection, analysis and interpretation, manuscript writing or in the decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
JSC and VCW conceptualized and design the study; YHL, KHH, and VCW were responsible for investigation; CFL, YHL, and VCW were responsible for data curation; CFL and VCW were responsible for methodology; CFL and VCW were responsible for formal analysis; CFL and VCW were responsible for visualization; JSC was responsible for resources; JSC provided supervision; CFL and VCW wrote the original draft; and YHL, KHH, and JSC reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lai, CF., Lin, YH., Huang, KH. et al. Kidney function predicts new-onset cardiorenal events and mortality in primary aldosteronism: approach of the 2021 race-free eGFR equation. Hypertens Res 47, 233–244 (2024). https://doi.org/10.1038/s41440-023-01400-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01400-0