Abstract
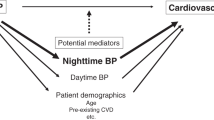
There is some evidence that nighttime blood pressure varies between seasons. In the present analysis, we investigated the seasonal variation in ambulatory nighttime blood pressure and its associations with target organ damage. In 1054 untreated patients referred for ambulatory blood pressure monitoring, we performed measurements of urinary albumin-to-creatinine ratio (ACR, n = 1044), carotid-femoral pulse wave velocity (cfPWV, n = 1020) and left ventricular mass index (LVMI, n = 622). Patients referred in spring (n = 337, 32.0%), summer (n = 210, 19.9%), autumn (n = 196, 18.6%) and winter (n = 311, 29.5%) had similar 24-h ambulatory systolic/diastolic blood pressure (P ≥ 0.25). However, both before and after adjustment for confounding factors, nighttime systolic/diastolic blood pressure differed significantly between seasons (P < 0.001), being highest in summer and lowest in winter (adjusted mean values 117.0/75.3 mm Hg vs. 111.4/71.1 mm Hg). After adjustment for confounding factors, nighttime systolic/diastolic blood pressure were significantly and positively associated with ACR, cfPWV and LVMI (P < 0.006). In season-specific analyses, statistical significance was reached for all the associations of nighttime blood pressure with target organ damage in summer (P ≤ 0.02), and for some of the associations in spring, autumn and winter. The association between nighttime systolic blood pressure and ACR was significantly stronger in patients examined in summer than those in winter (standardized β, 0.31 vs 0.11 mg/mmol, P for interaction = 0.03). In conclusion, there is indeed seasonality in nighttime blood pressure level, as well as in its association with renal injury in terms of urinary albumin excretion.

Our study shows that there is indeed seasonal variability in nighttime blood pressure, highest in summer and lowest in winter, and its association with renal injury in terms of urinary albumin excretion varies between summer and winter as well.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, et al. Seasonal variation in blood pressure: Evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2020;38:1235–43.
Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S. Seasonal variations in office, home and 24 h ambulatory blood pressure in patients with essential hypertension. J Hypertens. 1996;14:1421–5.
Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessi-Fulgheri P, Sarzani R. Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J Hypertens. 2012;30:1392–8.
Kollias A, Kyriakoulis KG, Stambolliu E, Ntineri A, Anagnostopoulos I, Stergiou GS. Seasonal blood pressure variation assessed by different measurement methods: systematic review and meta-analysis. J Hypertens. 2020;38:791–8.
Kario K, Hoshide S, Mizuno H, Kabutoya T, Nishizawa M, Yoshida T, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP Study. Circulation 2020;142:1810–20.
Cuspidi C, Facchetti R, Bombelli M, Sala C, Negri F, Grassi G, et al. Nighttime blood pressure and new-onset left ventricular hypertrophy: findings from the Pamela population. Hypertension. 2013;62:78–84.
Cheng D, Tang Y, Li HY, Li YP, Sang HQ. Nighttime blood pressure decline as a predictor of renal injury in patients with hypertension: a population-based cohort study. Aging-Us. 2019;11:4310–22.
Yang WY, Melgarejo JD, Thijs L, Zhang ZY, Boggia J, et al. Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019;322:409–20.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008;51:55–61.
Huang QF, Cheng YB, Guo QH, Liu CY, Kang YY, Sheng CS, et al. Clinic and ambulatory blood pressure in relation to the interaction between plasma advanced glycation end products and sodium dietary intake and renal handling. Hypertens Res. 2022;45:665–74.
Kang YY, Cheng YB, Guo QH, Sheng CS, Huang QF, Xu TY, et al. Renal sodium handling in relation to environmental and genetic factors in untreated Chinese. Am J Hypertens. 2021;34:394–403.
Sheng CS, Cheng YB, Wei FF, Yang WY, Guo QH, Li FK, et al. Diurnal blood pressure rhythmicity in relation to environmental and genetic cues in untreated referred patients. Hypertension. 2017;69:128–35.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55:613–8.
Expert Committee on the D, Classification of Diabetes M. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26:S5–20.
Narita K, Hoshide S, Fujiwara T, Kanegae H, Kario K. Seasonal variation of home blood pressure and its association with target organ damage: the J-HOP study (Japan morning surge-home blood pressure). Am J Hypertens. 2020;33:620–8.
Narita K, Hoshide S, Kanegae H, Kario K. Seasonal variation in masked nocturnal hypertension: The J-HOP Nocturnal Blood Pressure Study. Am J Hypertens. 2021;34:609–18.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, et al. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155–61.
Suzuki M, Taniguchi T, Furihata R, Yoshita K, Arai Y, Yoshiike N, et al. Seasonal changes in sleep duration and sleep problems: A prospective study in Japanese community residents. PLoS One. 2019;14:e0215345.
Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, et al. Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension. 2013;61:908–14.
Del Giorno R, Troiani C, Gabutti S, Stefanelli K, Puggelli S, Gabutti L. Impaired daytime urinary sodium excretion impacts nighttime blood pressure and nocturnal dipping at older ages in the general population. Nutrients. 2020;12:2013.
Bankir L, Bochud M, Maillard M, Bovet P, Gabriel A, Burnier M. Nighttime blood pressure and nocturnal dipping are associated with daytime urinary sodium excretion in African subjects. Hypertension. 2008;51:891–8.
Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013;61:278–83.
Acknowledgements
We acknowledge all patients for their commitment to the study. We also appreciate the technical assistance of Bei-Wen Lv, Jun-Wei Li and Yi Zhou.
Funding
This work was supported by the Chinese National Natural Science Foundation (82270452, 82070432, 82070435, 82270469), the Shanghai Municipal Health Commission (Grant for Leading Academics 2022LJ022) and the Shanghai Talent Development Fund (2021087).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, Y., Sheng, CS., Huang, JF. et al. Seasonality in nighttime blood pressure and its associations with target organ damage. Hypertens Res 46, 1433–1441 (2023). https://doi.org/10.1038/s41440-023-01201-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01201-5
Keywords
This article is cited by
-
Seasonal variation in blood pressure and its impact on target organ damage and cardiovascular disease incidence
Hypertension Research (2023)
-
Topics 2023 in Hypertension Research leading to guidelines in Asia
Hypertension Research (2023)