Abstract
Vascular function assessment is useful for the evaluation of atherosclerosis severity, which may provide additional information for cardiovascular risk stratification. In addition, vascular function assessment is helpful for a better understanding of pathophysiological associations between vascular dysfunction and cardiometabolic disorders. In 2020 and 2021, although coronavirus disease 2019 (COVID-19) was still a worldwide challenge for health care systems, many excellent articles regarding vascular function were published in Hypertension Research and other major cardiovascular and hypertension journals. In this review, we summarize new findings on vascular function and discuss the association between vascular function and COVID-19, the importance of lifestyle modifications for the maintenance of vascular function, and the usefulness of vascular function tests for cardiovascular risk assessment. We hope this review will be helpful for the management of cardiovascular risk factors, including hypertension and cardiovascular diseases, in clinical practice.

Similar content being viewed by others
Introduction
The assessment of vascular function, including endothelial function, vascular smooth muscle function, and arterial stiffness, is performed to assess the severity of atherosclerosis, which may provide additional information for cardiovascular risk assessment and an opportunity for timely intervention to reduce the risk of cardiovascular events in patients with cardiovascular risk factors or a history of cardiovascular events [1, 2]. In addition, the assessment of vascular function may be helpful to understand the pathophysiology of cardiometabolic disorders.
The outbreak of coronavirus disease 2019 (COVID-19) caused by the highly pathogenic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a worldwide challenge for health care systems. Major complications of COVID-19 are viral pneumonia and acute respiratory distress syndrome, which can lead to respiratory failure [3]. However, accumulating evidence has shown that COVID-19 is also associated with thromboembolic complications such as venous thromboembolism, arterial thrombosis, and small-vessel thrombosis, which may contribute to the high morbidity and mortality in patients with COVID-19 [4,5,6]. Although the pathogenesis of thromboembolic complications in patients with COVID-19 has not been fully elucidated, vascular dysfunction, especially endothelial dysfunction, has been shown to be a potential contributor to thromboembolic events in patients with COVID-19 [7,8,9].
Many excellent articles regarding vascular function were published in 2020 and 2021. In this review, we summarize recent literature and discuss the associations of vascular function with COVID-19, lifestyle modifications, and cardiovascular risk assessment.
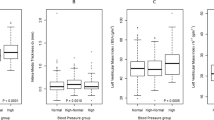
COVID-19 and vascular function
The acute effects of COVID-19 on vascular function have been investigated in several studies. Clinical studies have shown that flow-mediated vasodilation (FMD) of the brachial artery, an index of endothelial function, is significantly lower and that brachial-ankle pulse wave velocity (baPWV) and carotid-femoral pulse wave velocity (cfPWV), indices of arterial stiffness, are significantly higher in patients with COVID-19 than in control participants without COVID-19 in the acute phase of COVID-19 (Fig. 1) [10,11,12]. These findings indicate that vascular function is impaired in the acute phase of COVID-19. Although the precise mechanisms underlying endothelial dysfunction in patients with COVID-19 have not been fully elucidated, endothelial dysfunction may be caused by a combination of the direct effects of SARS-CoV-2 and the secondary effects of COVID-19-induced systemic inflammation on the vascular endothelium [7]. Several autopsy studies have revealed the presence of coronavirus-like particles in endothelial cells in multiple organs using electron microscopy analysis, the presence of SARS-CoV-2 spike proteins in capillary endothelial cells using immunohistochemistry, and the presence of SARS-CoV-2 RNA within the endothelium in multiple organs using in situ hybridization [13,14,15,16,17,18,19,20], and those findings have led to speculation that direct SARS-CoV-2 infection of endothelial cells contributes to the development of endothelial dysfunction in patients with COVID-19. Angiotensin-converting enzyme 2 (ACE2) is the main entry receptor for SARS-CoV-2 [21, 22]. However, it remains a matter of debate whether ACE2 is expressed in endothelial cells [21, 23,24,25,26]. Recently, Kaneko et al. reported that although the basal level of ACE2 gene expression by endothelial cells in the human brain was low, ACE2 gene expression was increased by stimulation with fluid shear stress in both human umbilical vein endothelial cells (HUVECs) and human brain microvascular endothelial cells (HBMECs) within a three-dimensional printed vessel replica system [27]. In addition, ACE2 protein expression was increased by the stimulation of monolayer HUVECs and HBMECs with horizontal shear stress. They also reported that the susceptibility of brain endothelia to SARS-CoV-2 spike protein was facilitated by a flow-mediated increase in ACE2 expression. Unique gene expression patterns in human brain endothelial cells, such as an upregulation of complement component C3, were triggered by the binding of the SARS-CoV-2 spike protein [27]. These findings indicate that flow-dependent expression of ACE2 is associated with the susceptibility of endothelial cells to direct SARS-CoV-2 infection. In contrast, Urata et al. reported that HUVECs were infected with SARS-CoV-2 through endocytosis in an ACE2-independent manner [25]. Susceptibility to SARS-CoV-2 infection through endocytosis was more enhanced in senescent endothelial cells than in early-passage endothelial cells. They also reported that the expression of various genes associated with inflammation, the immune response, and coagulation cascades was affected by SARS-CoV-2 infection in endothelial cells [25]. Although further studies are needed to determine how SARS-CoV-2 infects endothelial cells, the results of previous studies indicate that SARS-CoV-2 may have the ability to directly infect endothelial cells and cause endothelial dysfunction, which can result in the exacerbation of inflammation and thrombosis in COVID-19.
The results of several longitudinal studies have demonstrated the possibility that the vascular dysfunction caused by SARS-CoV-2 infection partially improves but does not completely return to the baseline level, resulting in the persistence of vascular dysfunction after SARS-CoV-2 infection [28,29,30,31,32,33]. Oikonomou et al. longitudinally measured FMD in 73 patients with COVID-19 in the acute phase (between 24 and 72 h after hospitalization), in the mid-term phase (28 days after hospital discharge), and in the long-term phase (6 months after hospital discharge) [28]. They reported that FMD was significantly improved during the follow-up period in patients with COVID-19 (1.75 ± 2.19% in the acute phase, 4.23 ± 2.02% in the mid-term phase, and 5.24 ± 1.62% in the long-term phase, P = 0.001). However, FMD did not recover to the level of that in controls (6.48 ± 3.08%) in either the mid-term phase (P < 0.001) or the long-term phase (P = 0.01). Zanoli et al. longitudinally measured aortic pulse wave velocity (aPWV) in 90 individuals with a history of COVID-19 between 12 and 48 weeks after SARS-CoV-2 infection and at 27 weeks after the first measurement of aPWV [33]. They reported that aPWV was significantly improved during the follow-up period (P = 0.01). However, aPWV at 27 weeks after the first measurement was still significantly higher than that in matched controls (P = 0.04). Taken together, these findings show that the vascular dysfunction caused by COVID-19 may partially improve but does not completely recover to the baseline level, which can lead to the persistence of vascular dysfunction even after the resolution of acute infection. Further studies are needed to determine whether the persistence of vascular dysfunction is associated with an increased risk of cardiovascular events after the resolution of the acute infection or post-COVID-19 conditions such as persistent cardiovascular symptoms and exercise limitations (Fig. 1).
The results of a recent study showed that vascular function was not impaired in participants who had been vaccinated against COVID-19 but were infected with the Omicron variant of SARS-CoV-2 [34]. Skow et al. measured FMD and cfPWV in 23 vaccinated adults with mild-to-moderate COVID-19 (Omicron) who did not require hospitalization and 13 vaccinated healthy controls without a history of COVID-19 [34]. The average period from the diagnosis of SARS-CoV-2 infection to FMD measurements was 30 ± 9 days. They reported that there was no significant difference in FMD (6.1 ± 2.3% vs. 5.9 ± 2.8%, P = 0.544) or cfPWV (5.7 ± 0.8 m/s vs. 5.9 ± 0.6 m/s, P = 0.367) between vaccinated participants with COVID-19 during the Omicron wave and vaccinated healthy controls without a history of COVID-19 [34]. These findings suggest that vascular function is not impaired by infection with the Omicron variant of SARS-CoV-2 in vaccinated adults with mild-to-moderate COVID-19 who did not require hospitalization.
Lifestyle modifications and vascular function
Lifestyle modifications, including salt intake restriction, dietary pattern changes, the maintenance of a proper body weight, exercise therapy, alcohol restriction, and smoking cessation, are expected not only to lower blood pressure but also to enhance the blood pressure-lowering effects of antihypertensive drugs, which can prevent the development of overt hypertension in untreated individuals and lead to a reduction in the use or dose of antihypertensive drugs required for blood pressure control in medicated patients with hypertension (Fig. 2). Therefore, lifestyle modifications play an important role in the management of hypertension regardless of the presence or absence of antihypertensive drug treatment. Lifestyle modifications are also expected to improve vascular function in a blood pressure-dependent and blood pressure-independent manner, thereby preventing the progression of atherosclerosis (Fig. 2) [35,36,37,38]. Exercise training has been shown to reduce arterial stiffness in patients with hypertension. Lopes et al. conducted a systematic review and meta-analysis to determine the effect of exercise training on PWV in patients with hypertension [39]. They reported that PWV was significantly reduced by exercise interventions based on aerobic exercise, isometric exercise, and combined exercise in adult patients with hypertension. Subgroup analyses showed that the positive effects of exercise training on PWV were independent of antihypertensive drug treatment. In addition, similar reductions in PWV were observed in both participants with large blood pressure reductions and participants with small blood pressure reductions by exercise training. These findings suggest that exercise training improves arterial stiffness regardless of the type of exercise training and independent of antihypertensive drug treatment or the extent of blood pressure reduction. Yamaji et al. investigated the association between daily stair climbing activity and vascular function in patients with hypertension [40]. They reported that endothelial function assessed by FMD of the brachial artery and vascular smooth muscle function assessed by nitroglycerine-induced vasodilation of the brachial artery were significantly higher in patients who usually climbed stairs to the ≥3rd floor than in patients who did not climb stairs at all in daily life. Although a definitive causal relationship between daily stair climbing activity and vascular function was not established due to the cross-sectional design of the study, these findings suggest that daily stair climbing activity, which requires more muscle strength and more energy than walking on flat ground or downstairs, has beneficial effects on vascular function in patients with hypertension.
In addition to exercise, dietary patterns have acute and chronic effects on vascular function. Fryer et al. investigated the acute effects of a combination of prolonged uninterrupted sitting (180 min) and a high-saturated fat meal on arterial stiffness in 13 healthy nonsmoking males [41]. They reported that central arterial stiffness assessed by cfPWV and peripheral arterial stiffness assessed by PWVβ were more deteriorated by consuming a high-fat meal (61 g fat, 1066 kcal) prior to prolonged uninterrupted sitting than by consuming a low-fat meal (10 g fat, 601 kcal) prior to prolonged uninterrupted sitting. These findings suggest that a high-fat meal should be avoided before prolonged uninterrupted sitting for the prevention of arterial stiffening. The dietary approach to stop hypertension (DASH) diet is rich in vegetables, fruits, and low-fat dairy products and is low in fat, sugar, and sodium. The DASH diet has been shown to dramatically lower blood pressure compared with a standard Western diet in adult patients with hypertension [42]. Couch et al. investigated the effects of a 6-month DASH-focused behavioral nutrition intervention on blood pressure and endothelial function assessed by FMD in adolescents with elevated blood pressure in a randomized control trial [43]. Adolescents (n = 159) with newly diagnosed elevated blood pressure or stage 1 hypertension were randomly assigned to receive a DASH-focused behavioral nutrition intervention (n = 81) or routine care (n = 78). The DASH participants received a take-home manual, face-to-face counseling sessions with a dietitian regarding the DASH diet, monthly mailings, and weekly telephone calls focused on behavioral strategies to promote DASH adherence for 6 months, whereas the routine care participants received usual nutrition counseling with a dietitian. The authors reported that the DASH diet participants had greater improvements in systolic blood pressure (−2.7 mmHg, P = 0.03) and FMD (2.5%, P = 0.05) from baseline to 6 months and a greater improvement in FMD (3.1%, P = 0.03) from baseline to 18 months than the routine care participants. The improvement in FMD was independent of changes in blood pressure, weight, or physical activity from baseline to 18 months in the DASH diet participants. These findings indicate that the DASH diet not only lowers blood pressure but also improves endothelial function independent of blood pressure reductions in adolescents with elevated BP or stage 1 hypertension. In addition, the beneficial effects of the DASH-focused behavioral nutrition intervention on endothelial function may persist after the completion of intervention. Long-term adherence to the DASH-type dietary pattern may prevent the progression of atherosclerosis, which can lead to the prevention of future cardiovascular events in adolescents with elevated blood pressure. Funakoshi et al. investigated the association between eating before bed and the development of hypertension in 2930 participants without hypertension with an average follow-up period of 4.5 years [44]. They reported that eating within 2 h before going to sleep ≥three times per week was significantly associated with an increased risk of developing hypertension (odds ratio [OR]: 1.23, 95% confidence interval [CI]: 1.05–1.44) compared with eating within 2 h before going to sleep ≤two times per week. Taken together, these findings show that daily eating habits have profound effects on both blood pressure and vascular function.
Cigarette smoking is one of the major risk factors for cardiovascular mortality in Japan [45]. Fukumoto et al. reported that FMD was significantly improved (3.80 ± 2.24% to 4.60 ± 2.55%, P = 0.013) in 58 smokers who succeeded with smoking cessation 20 weeks after treatment initiation in the smoking cessation outpatient department, but there was no significant change in FMD (4.41 ± 2.01% to 4.43 ± 2.26%, P = 0.98) in 21 age- and sex-matched continued smokers [46]. The use of electronic (e)-cigarettes and heat-not-burn cigarettes is an emerging trend, especially among the younger generation. The results of recent experimental and clinical studies have shown that endothelial function is impaired by e-cigarette smoking and heat-not-burn cigarette smoking. Carnevale et al. measured the FMD of the brachial artery in 40 healthy participants just before and within 30 min after smoking. They reported that FMD was decreased by both traditional tobacco cigarette smoking and e-cigarette smoking, but a significant difference in FMD between participants who smoked traditional tobacco cigarettes and participants who smoked e-cigarettes was not observed [47]. They also reported that oxidative stress markers were increased and that NO bioavailability and vitamin E levels were decreased by e-cigarette smoking. Kuntic et al. investigated the effects of short-term e-cigarette vapor exposure on endothelial function and oxidative stress in mice. They reported that endothelial dysfunction, oxidative stress, inflammation, and lipid oxidation were induced by e-cigarette vapor exposure [48]. Biondi-Zacai et al. measured FMD in 20 smokers just before and after smoking and reported that FMD was significantly decreased by traditional tobacco cigarette smoking, e-cigarette smoking, and heat-not-burn cigarette smoking. E-cigarette smoking and heat-not-burn cigarette smoking tended to have a less deleterious effect than traditional tobacco cigarette smoking on FMD [49]. Taken together, these findings suggest that although both e-cigarettes and heat-not-burn cigarettes may be less harmful than traditional tobacco cigarettes to endothelial function, endothelial function is deteriorated by the use of both e-cigarettes and heat-not-burn cigarettes. Therefore, neither e-cigarettes nor heat-not-burn cigarettes should be labeled as safe for the cardiovascular system.
Taken together, these findings show that lifestyle modifications are strongly recommended in daily practice not only to lower blood pressure but also to improve or augment vascular function to prevent the progression of atherosclerosis and the development of cardiovascular events (Fig. 2).
Cardiovascular risk assessment by vascular function tests
The results of a previous individual participant data meta-analysis of prospective cohort studies conducted in Japan showed that baPWV was an independent predictor of cardiovascular events and could provide additional information for cardiovascular risk stratification in individuals without a history of cardiovascular disease, indicating the usefulness of baPWV in the primary prevention of cardiovascular disease [50]. Sang et al. conducted a systematic review and meta-analysis to evaluate the associations of baPWV with cardiovascular events, cardiovascular mortality, and all-cause mortality in patients with a history of atherosclerotic cardiovascular disease (ASCVD) [51]. They reported that higher baPWV was independently associated with an increased risk of cardiovascular events, cardiovascular mortality, and all-cause mortality in patients with a history of ASCVD, indicating the usefulness of baPWV assessment in the secondary prevention of cardiovascular disease. These findings indicate that baPWV is useful in cardiovascular risk assessment regardless of the presence or absence of a history of cardiovascular disease. Our group investigated the usefulness of baPWV for predicting cardiovascular events based on blood pressure control in medicated hypertensive patients with a history of coronary heart disease (CHD) [52]. We reported that baPWV was an independent predictor of cardiovascular events in medicated hypertensive patients with CHD who had blood pressure <130/80 mmHg, but there was no significant association between baPWV and cardiovascular events in those who had blood pressure ≥130/80 mmHg. These findings suggest that baPWV is useful for cardiovascular risk assessment in patients with well-controlled blood pressure, whereas baPWV is less useful for cardiovascular risk assessment in patients with inadequate blood pressure control among medicated hypertensive patients with a history of CHD.
The ankle-brachial index (ABI) has been used not only for the screening of lower extremity arterial disease (LEAD) but also for cardiovascular risk assessment. The results of a meta-analysis have shown that cardiovascular risk increases as ABI decreases [53]. Occasionally, however, the ABI value is falsely elevated and maintained within the normal range despite the presence of occlusive arterial lesions in the lower extremities in patients with noncompressible lower limb arteries, which can lead to incorrect cardiovascular risk assessment. Therefore, information other than the ABI value should be combined for precise cardiovascular risk assessment. Tsai et al. reported that a combination of an ABI < 0.9 and an interleg ABI difference ≥0.17 was more useful than an ABI < 0.9 alone for predicting all-cause mortality and cardiovascular mortality [54]. Paying attention to an interleg ABI difference may prevent missed diagnoses of LEAD, which may result in an improvement in the accuracy of the ABI method for predicting cardiovascular mortality.
The results of recent studies have shown that attention should be given to the burden of LEAD. When ABI is determined by measuring systolic blood pressure in each arm and each ankle using the Doppler method, four ABIs that correspond to the four ankle arteries, including the anterior (or dorsalis pedis) and posterior tibial arteries of each leg, can be calculated. The highest ABI in each leg is used for the diagnosis of LEAD, and the lowest ABI between the two legs is used for cardiovascular risk assessment as a vascular marker. Therefore, patients with normal ABI in both legs can be categorized into two groups: patients with four normal ABIs and patients with discordant ABIs. Patients with discordant ABIs include those who have one low ABI (<1.00) and three normal ABIs and those who have one low ABI and one normal ABI in both legs. Firth et al. reported that patients with discordant ABIs had increased risks of myocardial infarction (hazard ratio [HR]: 1.31, 95% CI: 1.10–1.56), ischemic stroke (HR: 1.53, 95% CI: 1.37–1.72), and all-cause mortality (HR: 1.27, 95% CI: 1.16–1.39) compared with patients with four normal ABIs among patients with normal ABIs in both legs (1.00–1.39) [55]. These findings suggest that the presence of an occlusive lesion in even one infrapopliteal artery is associated with an increased risk of cardiovascular morbidity and mortality. Unkart et al. investigated the associations of the burden of LEAD with all-cause mortality, cardiovascular events, and cardiovascular mortality in individuals without a history of cardiovascular disease [56]. They reported that the risk of all-cause mortality, cardiovascular events, and cardiovascular mortality increased as the number of low ABIs (≤0.9) (0, 1, 2, 3, and 4) or the number of legs with a low ABI (none, unilateral low ABI, and bilateral low ABI) increased. These findings indicate that attention should be given not only to the ABI value but also to the burden of LEAD for more precise cardiovascular risk assessment.
Conclusions
In this article, we reviewed the recent literature and summarized new findings on vascular function. The results of recent studies have indicated that vascular function tests are useful for a better understanding of the pathophysiology of cardiovascular diseases, more precise cardiovascular risk assessment, and the evaluation of therapeutic intervention effects on atherosclerosis. Further accumulation of data regarding vascular function would enable us to draw more specific conclusions concerning the role of vascular function in cardiovascular disease.
Future perspectives
FMD of the brachial artery and reactive hyperemia peripheral artery tonometry (RH-PAT) have been used frequently for the assessment of endothelial function. However, repeated measurements of FMD or RH-PAT examinations are difficult to perform in clinical practice, partly due to their relatively cumbersome procedures. Several new approaches for the assessment of endothelial function have been under development for clinical use [57,58,59]. The development of a noninvasive, simple, and operator-independent endothelial function test with high reproducibility would enable routine assessment of endothelial function in clinical practice, which may lead to improvements in cardiovascular morbidity and mortality through more precise cardiovascular risk assessment and timely intervention.
References
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circulation J: Off J Jpn Circulation Soc. 2009;73:411–8.
Tanaka A, Tomiyama H, Maruhashi T, Matsuzawa Y, Miyoshi T, Kabutoya T, et al. Physiological diagnostic criteria for vascular failure. Hypertension. 2018;72:1060–71.
Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020;323:1239–42.
Wichmann D. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020;173:1030.
Thomas W, Varley J, Johnston A, Symington E, Robinson M, Sheares K, et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thrombosis Res. 2020;191:76–7.
Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020;20:1135–40.
Maruhashi T, Higashi Y. Pathophysiological Association of endothelial dysfunction with fatal outcome in COVID-19. Int J Mol Sci. 2021;22:5131.
Six I, Guillaume N, Jacob V, Mentaverri R, Kamel S, Boullier A, et al. The Endothelium and COVID-19: an increasingly clear link brief title: endotheliopathy in COVID-19. Int J Mol Sci. 2022;23:6196.
Saeed S, Mancia G. Arterial stiffness and COVID-19: a bidirectional cause-effect relationship. J Clin Hypertension. 2021;23:1099–103.
Oliveira MR, Back GD, da Luz Goulart C, Domingos BC, Arena R, Borghi-Silva A. Endothelial function provides early prognostic information in patients with COVID-19: a cohort study. Respiratory Med. 2021;185:106469.
Ratchford SM, Stickford JL, Province VM, Stute N, Augenreich MA, Koontz LK, et al. Vascular alterations among young adults with SARS-CoV-2. Am J Physiol Heart Circulatory Physiol. 2021;320:H404–10.
Schnaubelt S, Oppenauer J, Tihanyi D, Mueller M, Maldonado-Gonzalez E, Zejnilovic S, et al. Arterial stiffness in acute COVID-19 and potential associations with clinical outcome. J Intern Med. 2021;290:437–43.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl J Med. 2020;383:120–8.
Dittmayer C, Meinhardt J, Radbruch H, Radke J, Heppner BI, Heppner FL, et al. Why misinterpretation of electron micrographs in SARS-CoV-2-infected tissue goes viral. Lancet. 2020;396:e64–5.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8.
Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, Xu H, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396:320–32.
Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77:198–209.
Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol. 2020;92:699–702.
Colmenero I, Santonja C, Alonso-Riano M, Noguera-Morel L, Hernandez-Martin A, Andina D, et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br J Dermatol. 2020;183:729–37.
Bhatnagar J, Gary J, Reagan-Steiner S, Estetter LB, Tong S, Tao Y, et al. Evidence of SARS-CoV-2 replication and tropism in the lungs, airways and vascular endothelium of patients with fatal COVID-19: an autopsy case-series. J Infect Dis. 2021. https://doi.org/10.1093/infdis/jiab039.
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7.
Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–92.e286.
Kuriakose J, Montezano AC, Touyz RM. ACE2/Ang-(1-7)/Mas1 axis and the vascular system: vasoprotection to COVID-19-associated vascular disease. Clin Sci. 2021;135:387–407.
McCracken IR, Saginc G, He L, Huseynov A, Daniels A, Fletcher S, et al. Lack of evidence of angiotensin-converting enzyme 2 expression and replicative infection by SARS-CoV-2 in human endothelial cells. Circulation. 2021;143:865–8.
Urata R, Ikeda K, Yamazaki E, Ueno D, Katayama A, Shin-Ya M, et al. Senescent endothelial cells are predisposed to SARS-CoV-2 infection and subsequent endothelial dysfunction. Sci Rep. 2022;12:11855.
Wagner JUG, Bojkova D, Shumliakivska M, Luxan G, Nicin L, Aslan GS, et al. Increased susceptibility of human endothelial cells to infections by SARS-CoV-2 variants. Basic Res Cardiol. 2021;116:42.
Kaneko N, Satta S, Komuro Y, Muthukrishnan SD, Kakarla V, Guo L, et al. Flow-mediated susceptibility and molecular response of cerebral endothelia to SARS-CoV-2 infection. Stroke. 2021;52:260–70.
Oikonomou E, Souvaliotis N, Lampsas S, Siasos G, Poulakou G, Theofilis P, et al. Endothelial dysfunction in acute and long standing COVID-19: a prospective cohort study. Vasc Pharmacol. 2022;144:106975.
Lambadiari V, Mitrakou A, Kountouri A, Thymis J, Katogiannis K, Korakas E, et al. Association of COVID-19 with impaired endothelial glycocalyx, vascular function and myocardial deformation 4 months after infection. Eur J Heart Fail. 2021;23:1916–26.
Gao YP, Zhou W, Huang PN, Liu HY, Bi XJ, Zhu Y, et al. Persistent endothelial dysfunction in coronavirus disease-2019 survivors late after recovery. Front Med. 2022;9:809033.
Ikonomidis I, Lambadiari V, Mitrakou A, Kountouri A, Katogiannis K, Thymis J, et al. Myocardial work and vascular dysfunction are partially improved at 12 months after COVID-19 infection. Eur J Heart Fail. 2022;24:727–9.
Szeghy RE, Stute NL, Province VM, Augenreich MA, Stickford JL, Stickford ASL, et al. Six-month longitudinal tracking of arterial stiffness and blood pressure in young adults following SARS-CoV-2 infection. J Appl Physiol. 2022;132:1297–309.
Zanoli L, Gaudio A, Mikhailidis DP, Katsiki N, Castellino N, Lo Cicero L, et al. Vascular dysfunction of COVID-19 is partially reverted in the long-term. Circulation Res. 2022;130:1276–85.
Skow RJ, Nandadeva D, Grotle AK, Stephens BY, Wright AN, Fadel PJ. Impact of breakthrough COVID-19 cases during the omicron wave on vascular health and cardiac autonomic function in young adults. Am J Physiol Heart Circulatory Physiol. 2022;323:H59–64.
Harrison DG, Coffman TM, Wilcox CS. Pathophysiology of hypertension: the mosaic theory and beyond. Circulation Res. 2021;128:847–63.
Hall ME, Cohen JB, Ard JD, Egan BM, Hall JE, Lavie CJ, et al. Weight-loss strategies for prevention and treatment of hypertension: a scientific statement from the American Heart Association. Hypertension. 2021;78:e38–50.
Barone Gibbs B, Hivert MF, Jerome GJ, Kraus WE, Rosenkranz SK, Schorr EN, et al. Physical activity as a critical component of first-line treatment for elevated blood pressure or cholesterol: Who, What, and How?: A scientific statement from the American Heart Association. Hypertension. 2021;78:e26–37.
Maruhashi T, Higashi Y. Cardiovascular risk in patients receiving antihypertensive drug treatment from the perspective of endothelial function. Hypertension Res: Off J Jpn Soc Hypertension. 2022;45:1322–33.
Lopes S, Afreixo V, Teixeira M, Garcia C, Leitao C, Gouveia M, et al. Exercise training reduces arterial stiffness in adults with hypertension: a systematic review and meta-analysis. J Hypertension. 2021;39:214–22.
Yamaji T, Harada T, Hashimoto Y, Nakano Y, Kajikawa M, Yoshimura K, et al. Stair climbing activity and vascular function in patients with hypertension. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:1274–82.
Fryer S, Stone K, Paterson C, Brown M, Faulkner J, Lambrick D, et al. Central and peripheral arterial stiffness responses to uninterrupted prolonged sitting combined with a high-fat meal: a randomized controlled crossover trial. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:1332–40.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl J Med. 1997;336:1117–24.
Couch SC, Saelens BE, Khoury PR, Dart KB, Hinn K, Mitsnefes MM, et al. Dietary approaches to stop hypertension dietary intervention improves blood pressure and vascular health in youth with elevated blood pressure. Hypertension. 2021;77:241–51.
Funakoshi S, Satoh A, Maeda T, Kawazoe M, Ishida S, Yoshimura C, et al. Eating before bed and new-onset hypertension in a Japanese population: the Iki city epidemiological study of atherosclerosis and chronic kidney disease. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:1662–7.
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, Noda M, et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med. 2012;9:e1001160.
Fukumoto K, Takemoto Y, Norioka N, Takahashi K, Namikawa H, Tochino Y, et al. Predictors of the effects of smoking cessation on the endothelial function of conduit and digital vessels. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:63–70.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150:606–12.
Kuntic M, Oelze M, Steven S, Kroller-Schon S, Stamm P, Kalinovic S, et al. Short-term e-cigarette vapour exposure causes vascular oxidative stress and dysfunction: evidence for a close connection to brain damage and a key role of the phagocytic NADPH oxidase (NOX-2). Eur Heart J. 2020;41:2472–83.
Biondi-Zoccai G, Sciarretta S, Bullen C, Nocella C, Violi F, Loffredo L, et al. Acute effects of heat-not-burn, electronic vaping, and traditional tobacco combustion cigarettes: the Sapienza University of rome-vascular assessment of proatherosclerotic effects of smoking (SUR - VAPES) 2 randomized trial. J Am Heart Assoc. 2019;8:e010455.
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, et al. Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension. 2017;69:1045–52.
Sang T, Lv N, Dang A, Cheng N, Zhang W. Brachial-ankle pulse wave velocity and prognosis in patients with atherosclerotic cardiovascular disease: a systematic review and meta-analysis. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:1175–85.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Increased arterial stiffness and cardiovascular risk prediction in controlled hypertensive patients with coronary artery disease: post hoc analysis of FMD-J (Flow-mediated Dilation Japan) Study A. Hypertension Res: Off J Jpn Soc Hypertension. 2020;43:781–90.
Ankle Brachial Index C, Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. Jama. 2008;300:197–208.
Tsai WC, Lee WH, Chen YC, Liu YH, Chang CT, Hsu PC, et al. Combination of low ankle-brachial index and high ankle-brachial index difference for mortality prediction. Hypertension Res: Off J Jpn Soc Hypertension. 2021;44:850–7.
Firth C, Tseng AS, Abdelmalek M, Girardo M, Atwal D, Cooper L, et al. Discordant values in lower extremity physiologic studies predict increased cardiovascular risk. J Am Heart Assoc. 2020;9:e015398.
Unkart JT, Allison MA, Araneta MRG, Ix JH, Matsushita K, Criqui MH. Burden of peripheral artery disease on mortality and incident cardiovascular events. Am J Epidemiol. 2020;189:951–62.
Idei N, Ukawa T, Kajikawa M, Iwamoto Y, Fujimura N, Maruhashi T, et al. A novel noninvasive and simple method for assessment of endothelial function: enclosed zone flow-mediated vasodilation (ezFMD) using an oscillation amplitude measurement. Atherosclerosis. 2013;229:324–30.
Morimoto H, Kajikawa M, Oda N, Idei N, Hirano H, Hida E, et al. Endothelial function assessed by automatic measurement of enclosed zone flow-mediated vasodilation using an oscillometric method is an independent predictor of cardiovascular events. J Am Heart Association. 2016;5:e004385.
Matsui S, Kajikawa M, Maruhashi T, Hashimoto H, Kihara Y, Chayama K, et al. New assessment of endothelial function measured by short time flow-mediated vasodilation: comparison with conventional flow-mediated vasodilation measurement. Int J Cardiol. 2018;265:24–9.
Acknowledgements
We thank Megumi Wakisaka, Miki Kumiji, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maruhashi, T., Higashi, Y. Current topic of vascular function in hypertension. Hypertens Res 46, 630–637 (2023). https://doi.org/10.1038/s41440-022-01147-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01147-0
Keywords
This article is cited by
-
Vascular function: a key player in hypertension
Hypertension Research (2023)