Abstract
The role of early growth in later health is controversial. We examined the associations of growth at different phases from birth to puberty with blood pressure and lipid profile at ~17.5 years. In the population-representative “Children of 1997” birth cohort, growth was measured as (i) weight-for-age z score (WAZ) at birth and WAZ gains from 0 to 2 and 2 to 8 years and (ii) body-mass-index-for-age z score (BAZ) and length/height-for-age z score (LAZ) at 3 months and BAZ and LAZ gains from 3 months to 3 years, 3 to 8 years and 8 to 14 years, based on the World Health Organization growth standards/references. Adjusted partial least squares regression was used to assess simultaneously the associations of growth with height-, age- and sex-specific systolic (SBPZ) and diastolic blood pressure z scores (DBPZ), low- (LDL) and high-density lipoprotein (HDL) and triglycerides (TG) at ~17.5 years. Among 3410 children, higher WAZ, BAZ and LAZ gains from initial size to 8 years were associated with higher SBPZ. Higher gains in WAZ and BAZ from 2 to 8 years were consistently associated with higher DBPZ, LDL and TG and lower HDL. Lower LAZ at 3 months and higher LAZ gain from 3 months to 3 years were associated with lower HDL and higher TG. Greater growth in weight, body mass index and length/height had negative associations with blood pressure and lipid profile at ~17.5 years, but the differences by growth measure, phase and outcome suggest a complex underlying process.
Similar content being viewed by others
Introduction
Growth is an important physical marker of child health and living conditions. Poor child growth or stunting, indicative of infections or malnutrition, especially in low-income settings, has been associated with adverse health outcomes, including poorer cognition and health in later life [1, 2]. This health concern has led to the implementation of child growth promotion programs from conception, consistent with the idea that poor early growth may result in “scarring” with lifelong health consequences, as in the hypothesis of Barker [3]. However, the evolutionary trade-off between growth and longevity raises the possibility that greater child growth could increase the risk of chronic diseases [4]. The empirically derived growth acceleration hypothesis also suggests that faster growth, especially during early life, may have long-term detrimental effects on health [5]. Growth at later phases may also be relevant since growth at different phases is correlated [6].
Given that cardiovascular disease is the leading cause of death worldwide [7], the associations of child growth, particularly in weight, with blood pressure and hypertension have been extensively investigated [8,9,10,11,12,13,14,15,16,17,18,19,20]. However, previous studies have mainly been conducted in Western populations, where higher socioeconomic position tends to be associated with higher birth weight and better health [8,9,10,11,12,13,14,15,16,17,18,19,20], making the results difficult to interpret. These studies have also often been restricted to a few growth periods defined by the availability of growth measurements and blood pressure during childhood, as well as being limited in their handling of correlated growth measurements [8,9,10,11,12,13,14,15,16,17,18,19,20]. Generally, these studies have found that lower birth weight is associated with higher blood pressure, and greater child growth in weight, body mass index or length/height are associated with higher blood pressure, but the studies differ in their identification of the period at which greater growth appears to be detrimental [8,9,10,11,12,13,14,15,16,17,18,19,20]. Furthermore, only a few growth studies have considered additional metabolic risk factors, such as lipid profile [9, 10, 14, 17, 20,21,22], which has frequently been linked to blood pressure [23]. A comparison of the role of growth in blood pressure and lipids may clarify the role of growth in metabolic health but it has rarely been undertaken.
We used Hong Kong’s population-representative Chinese “Children of 1997” birth cohort, with uniquely little social patterning of birth weight [24] and growth [25], to examine the associations of initial size and growth in weight, body mass index (BMI) and length/height at different phases from birth to puberty with systolic blood pressure (SBP) and diastolic blood pressure (DBP), low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol and triglycerides (TGs) at ~17.5 years. In this cohort, we have previously shown that greater height and BMI gains during middle childhood were positively associated with blood pressure at ~11 years [18], but whether these patterns persist after puberty is unknown. Given that sex hormones play a role during infancy and puberty [26] and are associated with lipid profile [27,28,29,30], we also assessed whether the associations differed by sex.
Methods
Study participants
Participants were from Hong Kong’s population-representative Chinese ‘Children of 1997’ birth cohort. The study was initially designed to investigate the effects of second-hand smoke exposure and breastfeeding on infant health service use [31]. The participants represent 88% (n = 8327) of those born between 1 April 1997 and 31 May 1997 and were recruited shortly after birth at all 49 governmental Maternal and Child Health Centres (MCHCs) in Hong Kong, which offer free preventive services, including immunizations and well-baby/child check-ups, from birth to 5 years of age. At the first MCHC visit (generally shortly after birth), maternal and family characteristics (i.e., birth place, education, age and gestational age) and infant sex were recorded using a self-administered questionnaire in Cantonese Chinese. Data on household income, housing type and occupation were also collected. Infant feeding was ascertained at regular visits (the recruitment visit, 3, 9 and 18 months of age) and classified into three groups (exclusively breastfed for at least 3 months, partially breastfed for any length of time or exclusively breastfed for less than 3 months, and never breastfed), as described elsewhere [32]. In 2005, we used record linkage to obtain routine measurements (weight at birth, and at 1, 3, 9, 12, 18, 24 and 36 months and annually from 6 to 15 years old; length/height at 3, 9 and 36 months and annually from 6 to 15 years old) taken by trained nurses at the MCHCs and the Student Health Service. During clinical follow-up from August 2013 to January 2016, i.e., at 17.5 ± 0.5 years, each participant’s weight and standing height were measured, and SBP and DBP (in mm Hg) were measured in standard conditions of position, rest and appropriate cuff size on the right arm using a sphygmomanometer (Kawamoto DM-3000, Japan). At the same visit, each participant’s overnight fasting blood sample was taken and assayed for lipids. LDL was estimated in mmol/L by the Friedewald equation (Roche Cobas C8000 System, Germany). HDL was measured in mmol/L using a homogeneous enzymatic colorimetric test with polyethylene glycol-coupled cholesterol esterase and cholesterol oxidase (Roche Cobas C8000 System, Germany). TG was quantitated in mmol/L by an enzymatic colorimetric method with glycerol and peroxidase (Roche Cobas C8000 System, Germany). Height and weight were used to calculate BMI as weight in kilograms divided by height in meters squared. Overweight status was based on the sex- and age-specific BMI cutoffs of the International Obesity Task Force criteria corresponding to worldwide definitions for overweight (BMI ≥ 25 kg/m2) and obesity (BMI ≥ 30 kg/m2) from the age of 18 years onwards [33]. The study was approved by the University of Hong Kong Hospital Authority–Hong Kong West Cluster Joint Institutional Review Board.
Growth changes and phases
Changes in the weight-for-age z score (WAZ), body-mass-index-for-age z score (BAZ), weight-for-length/height z score (WHZ) and length/height-for-age z score (LAZ) based on the World Health Organization (WHO) Child Growth Standards [34] and the WHO Growth Reference [35], 2007] were used to represent child growth. WAZ assesses underweight but not overweight status, while BAZ measures overweight and obesity status [36], given the strong correlation between BMI and body fat percentage at 3 to 7 years [37]. BAZ has also been suggested to assess growth among young children aged 0 to 2 years [38]. WHZ identifies wasting and overweight or obese status [36], but WHZ is not adjusted for age, unlike other growth indicators, and thus cannot assess growth over time. LAZ screens for stunting status due to prolonged undernutrition or repeated illness [36]. Here, we computed WAZ, BAZ and LAZ using routine weight and length/height measurements and calculated growth changes over time as the z score differences from a specific age to a later age.
Growth intervals were first selected based on the infancy–childhood–puberty model [39] rather than a parametric model such as the Count model, the Jenss–Bayley model or the Berkey–Reed model, which are more suitable for growth up to 6 years [40]. Based on the infancy–childhood–puberty model [39], growth phases for infancy, childhood and puberty were defined as birth to 2 years, 2 to 8 years and 8 to 14 years, respectively. Depending on data availability (i.e., weight at birth, and at 1, 3, 9, 12, 18, 24 and 36 months and annually from 6 to 15 years old; length/height at 3, 9 and 36 months and annually from 6 to 15 years old), we defined growth changes at three phases [39], which represent different physiological changes potentially driven by different factors, as follows: (i) WAZ in infancy (birth to 2 years) and childhood (2 to 8 years), and (ii) BAZ and LAZ in infancy (3 months to 3 years), childhood (3 to 8 years) and puberty (8 to 14 years). WAZ in puberty (8 to 14 years) was not analyzed because the WHO growth standards/references for weight are only available from birth to 10 years.
Metabolic outcomes
Systolic and diastolic blood pressure at ~17.5 years were analyzed as sex-, age- and height-specific systolic (SBPZ) and diastolic blood pressure z scores (DBPZ) based on the United States National High Blood Pressure Education Group reference 2004 [41]. “High normal” blood pressure and hypertension were defined as SBPZ and/or DBPZ ≥90th percentile but <95th percentile and ≥95th percentile, respectively [41]. Lipid profile at ~17.5 years consisted of LDL, HDL and TG, but not total cholesterol, which is determined by LDL and HDL. An adverse lipid profile in adolescents was defined as LDL ≥130 mg/dL (or ≥3.36 mmol/L) or HDL <40 mg/dL (or <1.03 mmol/L) or TG ≥130 mg/dL (or ≥1.47 mmol/L) based on the 2011 Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents [42, 43].
Statistical analyses
Differences in baseline characteristics and growth between the excluded and included participants in the present study were compared using Cohen’s d and w effect sizes for continuous and categorical variables, respectively, and they were interpreted as small (0.2; 0.1), medium (0.5; 0.3) or large (0.8; 0.5) [44]. Associations of baseline characteristics with growth among the included participants were assessed using linear regression. Correlations between growth at different phases were assessed using Pearson's correlation.
Since growth at different phases cannot be considered together in an ordinary least squares regression model due to multicollinearity, the associations of initial size and growth at different phases with blood pressure and lipid profile were examined using partial least squares regression (PLSR) [45, 46]. The advantage of PLSR is that it reduces the number of dimensions to a minimum to decompose highly correlated exposures into components that have similar associations with outcome [45, 46]. The optimal number of principal components in the PLSR models was chosen using the 10-fold cross-validated root mean squared error of prediction, while ensuring estimates for the confounders were stabilized and additional components made little difference to the variance explained. Confidence intervals were estimated using bootstrapping. Potential confounders (i.e., common causes of growth and blood pressure or lipid profile) chosen were maternal characteristics (i.e., birth place, age), infant characteristics (i.e., breastfeeding status, gestational age), highest parental education and household income per person. We also examined whether the associations of growth with blood pressure and lipid profile varied by sex from the significance of interaction terms between sex and growth, allowing for confounding interactions by sex.
Missing data, especially for growth, are unavoidable in longitudinal studies. To avoid possible selection bias due to the exclusion of participants with incomplete data, missing exposures and confounders were predicted 50 times using multiple imputation with chained equations [47]. Separate analysis was performed in the 50 complete datasets, followed by summarizing the estimates into single estimated beta-coefficients with 95% confidence intervals (CIs), using Rubin’s rules. Inverse-probability weighting [48] was also used to account for potential differences between the included and excluded participants. The model predicting inclusion status was based on factors associated with being excluded, which were growth at different phases, maternal birth place and age, highest parental education, highest parental occupation, housing type, breastfeeding status, gestational age and household income per person.
All statistical analyses were performed using Stata 13.0 (StataCorp. 2013. Stata Statistical Software: Release 13. StataCorp LP, College Station, TX) and R 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study participants
As of December 2017, of the original 8327 recruited, 8298 (99.7%) remained in ‘Children of 1997’, and 29 had permanently withdrawn. At the clinical follow-up, 6850 participants were contactable, of whom 3460 participated at ~17.5 years. In the final sample, we analyzed 3410 singletons with at least one growth measurement and blood pressure or lipid profile. The reasons for exclusion were being a twin (n = 48) and missing blood pressure and lipid profile (n = 2) (Supplemental Figure 1). Only slight differences in parental and infant characteristics were observed between the included and excluded participants (Cohen’s d < 0.2 for continuous variables; Cohen’s w < 0.1 for categorical variables) (Supplemental Table 1).
In this study, half of participants were boys (n = 1711, 50.2%), and the household income per capita was equally distributed across quintiles. The majority of the participants were formula-fed (n = 1733, 52.8%), had parents whose highest education level was grade 10–11 (n = 1470, 43.3%) and had mothers from Hong Kong (1980, 58.4%). At birth, the mean age of participants’ mothers was 30.5 ± 4.6 years, and participants had a mean gestational age of 39.4 ± 1.6 weeks, a mean birth weight of 3.2 ± 0.4 kg, a mean length at 3 months of 60.78 ± 2.09 cm and a mean BMI of 17.08 ± 1.50 kg/m2. At ~17.5 years, participants had a mean BMI of 21.95 ± 3.52 kg/m2, a mean systolic blood pressure of 110.88 ± 12.25 mm Hg, a mean diastolic blood pressure of 68.44 ± 8.85 mm Hg, a mean TG of 0.80 ± 0.40 mmol/L, a mean LDL of 2.14 ± 0.65 mmol/L and a mean HDL of 1.55 ± 0.34 mmol/L. The prevalence of overweight and obesity was 12.8%, while the prevalence of “high normal” blood pressure and hypertension was 5.5 and 7.1%, respectively, and the prevalence of an adverse lipid profile was 12.5%. Overweight and obese participants were more likely to have “high normal” blood pressure (9.0 vs 5.0%), hypertension (21.2 vs 5.0%) (Cohen’s w = 0.222) and an adverse lipid profile (32.9 vs 9.6%) (Cohen’s w = 0.235) than normal-weight participants.
Table 1 shows the associations of selected potential confounders with growth at different phases. Only a few parental and infant characteristics were consistently associated with growth. Higher parental education was associated with higher WAZ gain from birth to 2 years and lower WAZ gain from 2 to 8 years. Higher gestational age was associated with lower WAZ gains from birth to 2 years and 2 to 8 years, as well as lower BAZ gains from 3 to 8 years and 8 to 14 years. Children of Hong Kong–born mothers had lower LAZ gain from 3 to 8 years and higher LAZ gain from 8 to 14 years. Partially breastfed and formula-fed children had higher LAZ gain from 3 months to 3 years and 8 to 14 years but lower LAZ gain from 3 to 8 years. As shown in Supplementary Table 2, WAZ, BAZ and LAZ gains at different phases were negatively correlated, and moderate correlations were seen between initial size and growth during infancy.
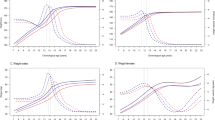
Growth and blood pressure
The associations of initial size and growth with blood pressure did not consistently vary by sex. Table 2 shows the adjusted associations of initial size and growth at different phases with SBPZ and DBPZ. Greater WAZ gains from birth to 2 years and 2 to 8 years and greater BAZ gains from 3 months to 3 years and 3 to 8 years were associated with higher SBPZ. WAZ gain from 2 to 8 years and BAZ gains from 3 months to 3 years and 3 to 8 years were positively associated with DBPZ. Greater LAZ gains from 3 to 8 years and 8 to 14 years were associated with higher SBPZ. No associations of birth weight, BMI or length at 3 months with SBPZ or DBPZ were observed.
Growth and lipid profile
Table 2 shows the adjusted associations of initial size and growth at different phases with LDL, HDL and TG. Higher WAZ gain from 2 to 8 years and BAZ gain from 3 to 8 years were associated with higher LDL and TG and lower HDL, while WAZ at birth was unrelated to lipid profile. Sex differences were consistently found in the associations of WAZ gain from 2 to 8 years and BAZ gain from 3 to 8 years with TG (P values < 0.001). Higher WAZ gain from 2 to 8 years (adjusted β = 0.047 mmol/L, 95% CI = 0.027, 0.067) and BAZ gain from 3 to 8 years (adjusted β = 0.046 mmol/L, 95% CI = 0.021, 0.071) were associated with higher TG in boys, but not in girls (WAZ gain: adjusted β = 0.007 mmol/L, 95% CI = −0.017, 0.031; BAZ gain: adjusted β = 0.009 mmol/L, 95% CI = −0.011, 0.029). Higher LAZ at 3 months was associated with higher HDL and lower TG, whereas higher LAZ gain from 3 months to 3 years was associated with lower HDL and higher TG.
Discussion
In this Chinese population-representative birth cohort from a developed non-Western setting, with little social patterning of birth weight or growth [24, 25], our findings are consistent with the hypothesis that accelerated growth may be detrimental [5] and the theory that growth may trade-off against long-term health [4]. Specifically, birth weight was unrelated to blood pressure and lipids, but shorter length at 3 months was linked to an adverse lipid profile in HDL and TG. However, greater weight, BMI and length gains in infancy were associated with higher blood pressure. Greater length gain in infancy was also associated with a more adverse lipid profile in terms of TG and HDL. Greater weight, BMI and length gains in childhood were associated with higher blood pressure, while greater weight and BMI gain in childhood were also associated with a more adverse lipid profile, especially in TG among boys.
Our study extends previous studies [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] by having a longer duration of follow-up, until ~17.5 years, when growth is almost complete, and a larger sample size than most of the previous studies (n = 139–2285) [8,9,10,11,12,13, 15,16,17, 20, 22] While previous studies mostly examined the effect of growth over shorter periods [8,9,10,11,12,13,14, 16, 17, 20,21,22], we concomitantly considered multicollinearity and growth at more phases to avoid ascribing effects of growth at an unmeasured stage, such as infancy, to factors with more readily available proxy measurements, such as birth weight. We defined growth periods based on the infancy–childhood–puberty model [39] rather than on data availability as in previous studies, which may increase chance findings. Furthermore, we considered weight, BMI and length/height, as well as two distinct metabolic outcomes, to provide more insight into the overall role of child growth in health. Our findings were only adjusted for confounders in the PLSR model, which allows simultaneous consideration of correlated growth measures, but not for mediators, as in some previous studies. Unlike previous studies, which suggested that the role of later child growth in blood pressure predominated [15, 18, 19], the present study highlights that growth, especially in weight, BMI and length, during infancy and childhood has an important role in blood pressure and lipid profile. Our observations are unlikely affected by the measures of blood pressure at older ages, since our previous study [18] and the present study agree that growth in BMI and height during childhood were positively associated with systolic blood pressure at ~11 and ~17 years, respectively.
The exact mechanisms underlying our findings are unclear. However, our findings of different associations of growth in weight, BMI and length/height with blood pressure and lipid profile suggest that there may be specific growth-related factors influencing metabolic risk factors [18] and that the factors affecting blood pressure and lipids may not be limited to adiposity [18]. Additionally, our findings of sex differences in the associations of weight and BMI gains in childhood with TG may suggest the possible involvement of sex hormones, which are increasingly recognized as affecting lipids [27,28,29,30]. Notably, infancy includes the period of mini-puberty. Whether growth rates in infancy and their effects are a reflection of the drivers of mini-puberty is a possibility that has not been examined, although growth in infancy is associated with pubertal timing [49]. Childhood growth is largely driven by growth hormone, which is not known to adversely affect blood pressure or lipids, suggesting some other mechanisms could be relevant. Further, the associations of higher LAZ at 3 months and LAZ gain from 3 months to 3 years with better and poorer lipid profile, respectively, may be relevant to the capacity-load model [50], which suggests early physiological conditions determine long-term capacity for homeostasis, while environmental factors and lifestyle in later life may challenge the homeostasis. Alternatively, these differences could be due to the influence of mini-puberty in the earlier period.
Child growth promotion is undoubtedly beneficial for short-term survival and cognitive development, but consideration should also be given as to whether it is detrimental to metabolic health. Further studies are needed to define optimal growth patterns in Hong Kong and other regions that do not experience poor growth caused by malnutrition or repeated infections. With the advent of “big data”, such studies are now possible, using study designs such as Mendelian randomization, but require genetic characterization of growth trajectories in a suitable population. Whether child growth promotion, especially in low-income settings, to attain a favored final stature or body size, maximizes long-term health also requires investigation.
This study has several strengths, such as a large sample size, regular growth measurements, a longitudinal analysis of growth from infancy to puberty, use of PLSR to handle multicollinearity of growth and minimal confounding by socioeconomic position, which increase the reliability of our findings. Inevitably, longitudinal studies will have missing data. Nonetheless, we showed that the included and excluded participants in these analyses were similar. We also used multiple imputation and inverse probability weighting to further minimize selection bias. BMI and length at birth were absent in this study, which may have affected our findings, but we used strong proxies, i.e., BMI and length at 3 months, respectively, in the analyses. We did not perform subgroup analysis by preterm or small-for-gestational-age status because these groups represented <10% of our cohort. Other limitations in this study include the lack of data on body composition at different phases, which would have improved our understanding of our findings, but we analyzed several indicators of growth that represented different underlying factors.
Our study found that greater weight, BMI and length gains in infancy or childhood are associated with higher blood pressure and poorer lipid profile. These findings suggest that the underlying mechanisms of the pathogenesis of hypertension and dyslipidemia may differ. Long-term health effects of different growth patterns should be identified to inform policy and practice.
References
Hoddinott J, Behrman JR, Maluccio JA, Melgar P, Quisumbing AR, Ramirez-Zea M, et al. Adult consequences of growth failure in early childhood. Am J Clin Nutr. 2013;98:1170–8.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60.
Barker DJP. Fetal origins of cardiovascular disease. Ann Med. 1999;31:3–6.
Wells JCK, Nesse RM, Sear R, Johnstone RA, Stearns SC. Evolutionary public health: Introducing the concept. Lancet. 2017;390:500–9.
Singhal A. Long-term adverse effects of early growth acceleration or catch-up growth. Ann Nutr Metab. 2017;70:236–40.
Luo ZC, Karlberg J. Critical growth phases for adult shortness. Am J Epidemiol. 2000;152:125–31.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
Kagura J, Adair LS, Munthali RJ, Pettifor JM, Norris SA. Association between early life growth and blood pressure trajectories in Black South African children. Hypertension. 2016;68:1123–31.
Lurbe E, Garcia-Vicent C, Torro MI, Aguilar F, Redon J. Associations of birth weight and postnatal weight gain with cardiometabolic risk parameters at 5 years of age. Hypertension. 2014;63:1326–32.
Hulst AV, Barnett TA, Paradis G, Roy-Gagnon MH, Gomez-Lopez L, Henderson M. Birth weight, postnatal weight gain, and childhood adiposity in relation to lipid profile and blood pressure during early adolescence. J Am Heart Assoc. 2017;6:e006302.
Ramoshaba N, Monyeki K, Hay L. Components of height and blood pressure among Ellisras rural children: Ellisras longitudinal study. Int J Environ Res Public Health. 2016;13:E856.
Regnault N, Kleinman KP, Rifas-Shiman SL, Langenberg C, Lipshultz SE, Gillman MW. Components of height and blood pressure in childhood. Int J Epidemiol. 2014;43:149–59.
de Beer M, Vrijkotte TG, Fall CH, van Eijsden M, Osmond C, Gemke RJ. Correction: Associations of infant feeding and timing of weight gain and linear growth during early life with childhood blood pressure: findings from a prospective population based cohort study. PLoS ONE. 2016;11:e0168920.
Marinkovic T, Toemen L, Kruithof CJ, Reiss I, van Osch-Gevers L, Hofman A, et al. Early infant growth velocity patterns and cardiovascular and metabolic outcomes in childhood. J Pediatr. 2017;186:57–63.e54.
Aris IM, Bernard JY, Chen LW, Tint MT, Lim WY, Soh SE, et al. Postnatal height and adiposity gain, childhood blood pressure and prehypertension risk in an Asian birth cohort. Int J Obes (Lond). 2017;41:1011–7.
Taine M, Stengel B, Forhan A, Carles S, Botton J, Charles MA, et al. Rapid early growth may modulate the association between birth weight and blood pressure at 5 years in the Eden cohort study. Hypertension. 2016;68:859–65.
Antonisamy B, Vasan SK, Geethanjali FS, Gowri M, Hepsy YS, Richard J, et al. Weight gain and height growth during infancy, childhood, and adolescence as predictors of adult cardiovascular risk. J Pediatr. 2017;180:53–61.e53.
Heys M, Lin SL, Lam TH, Leung GM, Schooling CM. Lifetime growth and blood pressure in adolescence: Hong Kong's "Children of 1997" birth cohort. Pediatrics. 2013;131:e62–72.
Tilling K, Davies N, Windmeijer F, Kramer MS, Bogdanovich N, Matush L, et al. Is infant weight associated with childhood blood pressure? Analysis of the Promotion of Breastfeeding Intervention Trial (PROBIT) cohort. Int J Epidemiol. 2011;40:1227–37.
Fujita Y, Kouda K, Nakamura H, Iki M. Association of rapid weight gain during early childhood with cardiovascular risk factors in Japanese adolescents. J Epidemiol. 2013;23:103–8.
Haack RL, Horta BL, Gigante DP, Barros FC, Oliveira I, Silveira VM. Hypertriglyceridemic waist phenotype: effect of birthweight and weight gain in childhood at 23 years old. PLoS ONE. 2015;10:e0134121.
Fujita Y, Kouda K, Nakamura H, Iki M. Inverse association between height increase and LDL cholesterol during puberty: a 3-year follow-up study of the Fukuroi city. Am J Hum Biol. 2016;28:330–4.
Borghi C, Rodriguez-Artalejo F, De Backer G, Dallongeville J, Medina J, Guallar E, et al. The association between blood pressure and lipid levels in Europe: European Study on Cardiovascular Risk Prevention and Management in Usual Daily Practice. J Hypertens. 2016;34:2155–63.
Leung JY, Leung GM, Schooling CM. Socioeconomic disparities in preterm birth and birth weight in a non-Western developed setting: evidence from Hong Kong's 'Children of 1997' birth cohort. J Epidemiol Community Health. 2016;70:1074–81.
Schooling CM, Yau C, Cowling BJ, Lam TH, Leung GM. Socio-economic disparities of childhood body mass index in a newly developed population: evidence from Hong Kong's 'Children of 1997' birth cohort. Arch Dis Child. 2010;95:437–43.
Schooling CM. Tachykinin neurokinin 3 receptor antagonists: a new treatment for cardiovascular disease? Lancet. 2017;390:709–11.
Zhao J, Jiang C, Lam TH, Liu B, Cheng KK, Xu L, et al. Genetically predicted testosterone and cardiovascular risk factors in men: a Mendelian randomization analysis in the Guangzhou Biobank Cohort Study. Int J Epidemiol. 2014;43:140–8.
Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, et al. Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med. 2011;8:272–83.
Casanova G, Bossardi Ramos R, Ziegelmann P, Spritzer PM. Effects of low-dose versus placebo or conventional-dose postmenopausal hormone therapy on variables related to cardiovascular risk: a systematic review and meta-analyses of randomized clinical trials. J Clin Endocrinol Metab. 2015;100:1028–37.
Au Yeung SL, Cheng KK, Zhao J, Zhang W, Jiang C, Lam TH, et al. Genetically predicted 17beta-estradiol and cardiovascular risk factors in women: a Mendelian randomization analysis using young women in Hong Kong and older women in the Guangzhou Biobank Cohort Study. Ann Epidemiol. 2016;26:171–5.
Schooling CM, Hui LL, Ho LM, Lam TH, Leung GM. Cohort profile: 'Children of 1997': a Hong Kong Chinese Birth Cohort. Int J Epidemiol. 2012;41:611–20.
Kwok MK, Schooling CM, Lam TH, Leung GM. Does breastfeeding protect against childhood overweight? Hong Kong's 'Children of 1997' birth cohort. Int J Epidemiol. 2010;39:297–305.
Cole TJ, Lobstein T. Extended International (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94.
World Health Organization, Department of Nutrition. WHO Child Growth Standards. Geneva: World Health Organization; 2006.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
World Health Organization. Training course on child growth assessment, WHO Child Growth Standards, C Interpreting growth indicators. Geneva: Department of Nutrition for Health and Development; 2008.
Sijtsma A, Bocca G, L'Abee C, Liem ET, Sauer PJ, Corpeleijn E. Waist-to-height ratio, waist circumference and BMI as indicators of percentage fat mass and cardiometabolic risk factors in children aged 3-7 years. Clin Nutr. 2014;33:311–5.
Furlong KR, Anderson LN, Kang H, Lebovic G, Parkin PC, Maguire JL, et al. BMI-for-age and weight-for-length in children 0 to 2 years. Pediatrics. 2016;138:e20153809.
Karlberg J. A biologically-oriented mathematical model (ICP) for human growth. Acta Paediatr Scand Suppl. 1989;350:70–94.
Beath KJ. Infant growth modelling and assessment of growth. In Preedy VR (ed), Handbook of growth and growth monitoring in health and disease, Vol. 1. Springer Science & Business Media: New York, USA, 2011, 3045–56.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
M Bibiloni Mdel, Salas R, Novelo HI, Villarreal JZ, Sureda A, Tur JA. Serum lipid levels and dyslipidaemia prevalence among 2–10 year-old Northern Mexican children. PLoS ONE. 2015;10:e0119877
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report.Pediatrics. 2011;128 (Suppl 5):S213–56.
Cohen J. Statistical power analysis for the behavioral sciences (revised ed.). New York: Academic Press; 1977.
Tu Y-K, Woolston A, Baxter PD, Gilthorpe MS. Assessing the impact of body size in childhood and adolescence on blood pressure: an application of partial least squares regression. Epidemiology. 2010;21:440–8.
Cole TJ. Can partial least squares regression separate the effects of body size and growth on later blood pressure?: Partial least squares regression. Epidemiology. 2010;21:449–51.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99.
Seaman SR, White IR, Copas AJ, Li L. Combining multiple imputation and inverse-probability weighting. Biometrics. 2012;68:129–37.
Hui LL, Wong MY, Lam TH, Leung GM, Schooling CM. Infant growth and onset of puberty: prospective observations from Hong Kong's "Children of 1997" birth cohort. Ann Epidemiol. 2012;22:43–50.
Wells JCK. The capacity-load model of non-communicable disease risk: understanding the effects of child malnutrition, ethnicity and the social determinants of health. Eur J Clin Nutr. 2018;72:688–97.
Acknowledgements
We would like to thank our colleagues at the Student Health Service and Family Health Service of the Department of Health for their assistance and collaboration. The authors also thank the late Dr. O Connie for coordinating the project and all the fieldwork for the initial study in 1997–1998.
Funding
This work is a substudy of the “Children of 1997” birth cohort, which was initially supported by the Health Care and Promotion Fund, Health and Welfare Bureau, Government of the Hong Kong Special Administrative Region (SAR; HCPF grant 216106), and was reestablished in 2005 funded by the Health and Health Services Research Fund (HHSRF grant 03040771), the Research Fund for the Control of Infectious Diseases (RFCID grant 04050172) Government of the Hong Kong SAR and the University Research Committee Strategic Research Theme of Public Health, The University of Hong Kong. This substudy was also supported by the Health and Health Services Research Fund (HHSRF grant 07080751) and the WYNG Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Rights and permissions
About this article
Cite this article
Cheng, T.S., Leung, G.M., Hui, L.L. et al. Associations of growth from birth to puberty with blood pressure and lipid profile at ~17.5 years: evidence from Hong Kong’s “Children of 1997” birth cohort. Hypertens Res 42, 419–427 (2019). https://doi.org/10.1038/s41440-018-0170-x
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0170-x