Abstract
Background/objectives
The purpose of this study is to report cases of choroidal melanoma that developed extrascleral tumour recurrence after treatment with iodine-125 brachytherapy.
Subjects/methods
In this single-institution retrospective observational case series, all instances of biopsy-confirmed orbital melanoma after known intraocular melanoma were reviewed. Tumour characteristics, clinical course, time to recurrence, cytogenetics of initial tumour and recurrence, and presence of intraocular recurrence were documented.
Results
Five cases of orbital melanoma following treatment with plaque radiotherapy are described. Tumour staging was Ia (1), IIa (2), and IIb (2). The primary lesion in four of the five appeared to have undergone complete regression for an average of 2 years, with the orbital melanoma developing after this interval. Recurrence of the intraocular tumour was seen in conjunction with an extrascleral component in two cases. Four cases ultimately underwent enucleation or exenteration; three had evidence of direct extension of tumour through the sclera. Four cases in this series had molecular characteristics associated with high metastatic risk (three patients with monosomy 3, one with BAP1 mutation).
Conclusions
High-risk tumour biology may predispose to late appearance of extrascleral melanoma despite optimal treatment and adequate control of the intraocular tumour. Extended follow-up with detailed orbital examination and imaging is recommended for this population.
Similar content being viewed by others
Introduction
Uveal melanoma is the most common primary intraocular tumour in adults [1]. It can develop throughout the uveal tract, with 90% arising in the choroid, 7% in the ciliary body, and 3% in the iris [2]. Brachytherapy, in addition to proton beam therapy and stereotactic radiosurgery, for medium-sized choroidal melanoma is a common treatment of choice, as there is no reported difference in survival outcome relative to enucleation, and this strategy allows for the potential to preserve vision and the anatomic globe [3].
In patients with choroidal melanoma, distant metastases have been reported to occur in 25–60% of patients, depending on the length of follow-up [1, 4, 5]. Approximately 90% of patients with metastatic disease have liver involvement, and the median survival reported in the published literature is 4–5 months with a 1-year survival of 10–15% [1]. Metastatic disease typically occurs via hematogenous spread to distant sites of the body [6].
Less commonly, choroidal melanoma may extend into the orbit via direct invasion through the sclera [6]. This is generally a sign of advanced disease, and can be found in ~2.5% of cases at primary presentation [6]. Indirect orbital metastases are rare with only a few cases reported in the literature [7, 8]. Extraocular extension has been shown to occur via various routes, including aqueous drainage channels and Schlemm’s canal, anterior and posterior ciliary arteries, vortex veins, long and short ciliary nerves, optic nerve, and by direct scleral perforation [6].
Reports of extraocular extension following treatment with plaque brachytherapy are few and have been attributed to treatment failure with recurrence of the intraocular tumour [9]. Here we report our experience in the management of 5 cases of patients with choroidal melanoma who developed extrascleral extension after treatment with iodine-125 brachytherapy.
Materials/subjects and methods
This study was conducted in compliance with the Helsinki Declaration, the Institutional Review Board at the University of California, Los Angeles, and the Health Insurance Portability and Accountability Act regulations. Informed consent was obtained by all subjects involved. In this case series, all patients with choroidal melanoma who developed extrascleral extension after plaque brachytherapy over a 7-year period at our institution were reviewed. Cases are presented in observational format.
In all cases, transscleral fine needle aspiration biopsy (FNAB) was performed, followed by brachytherapy plaque placement in the same surgery. After a conjunctival peritomy and traction suture placement on the rectus muscles, the quadrants were inspected. Transillumination was utilised to identify the tumour, and the anterior border of the tumour was marked. Fine-needle aspiration biopsy was performed through the sclera using a short 30-gauge needle attached to tubing on a syringe, and the samples were passed off to the ocular pathologist. Surgery proceeded with placement of the plaque with or without pars plana vitrectomy with silicone oil.
Results
Case 1
A 56-year-old man was referred for a superotemporal, hyperpigmented lesion in the left eye. Ultrasonography revealed an elevated mass measuring 4.94 mm in height with a base of 14.5 mm × 14.1 mm. A diagnosis of choroidal melanoma (T2aN0M0, stage IIa) with overlying retinal detachment was made. The patient underwent iodine-125 brachytherapy with transscleral FNAB (eight samples) for molecular prognostication and pars plana vitrectomy with silicone oil (1000 centistokes) placement for radiation attenuation.
Cytopathology confirmed choroidal melanoma. Fluorescent in situ hybridisation (FISH) analysis was inconclusive due to insufficient sample. The 3-month postoperative evaluation revealed a good response to treatment with resolution of the serous retinal detachment. The patient underwent subsequent vitrectomy for removal of silicone oil.
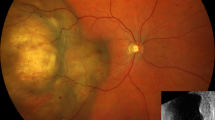
Four years following brachytherapy, the patient presented with pain and decreased vision in the left eye. Visual acuity was 20/20-2 in the right eye and 20/400 in the left. Ocular motility of the left eye was restricted in all directions of gaze. He was noted to have proptosis with a palpable mass in the superolateral orbit. Fundoscopic exam of the left eye revealed a large pigmented mass and two smaller pigmented lesions extending from 10–3 o’clock with associated subretinal fluid (Fig. 1A). Ultrasonography revealed an extra-scleral mass (Fig. 1B). CT scan of the thorax and abdomen showed no signs of distant metastasis.
A Fundus photograph revealing a large pigmented mass and two smaller pigmented lesions extending from 10 to 3 o’clock with associated subretinal fluid. B Ultrasound showing extraocular extension of the tumour. Case 2: A 65-year-old man experienced extrascleral extension of choroidal melanoma after iodine-125 brachytherapy treatment 3 years prior. C Fundus photograph revealing a tumour spanning 10:00-2:00 clockwise with the apex at 11:30. D Ultrasound showing 2 areas of echolucent spaces in the orbit posterior to the lesion, with noted connection to the intraocular lesion. The orbital lesion measured 4.55 mm in height. E Three months later, the orbital lesion height had increased to 5.47 mm. The intraocular lesion height remained stable at 2.91 mm. F At 6-month follow-up the orbital lesion height had increased to 6.73 mm while the intraocular lesion height remained stable.
FNAB of the orbital lesion confirmed the diagnosis of melanoma. The patient subsequently underwent exenteration of the left orbit for local tumour control. Pathological examination of the left orbital specimen revealed a brown necrotic mass located on the superior aspect of the posterior globe ~20 mm in diameter, extending extrasclerally. Immunohistochemistry showed expression of CD31+ in blood vessels, but no tumour was identified within vessels. The tumour cell nuclei were positive for mutation in BRCA-1 associated protein (BAP1), and FISH again yielded insufficient material for cytogenetic result.
One year status post exenteration, he developed a nonhealing area of the socket, which was biopsied. Pathology revealed a subepithelial nodule of malignant cells with focal lymphovascular invasion, consistent with residual or recurrent melanoma. CT of the abdomen demonstrated multiple liver lesions, which were determined to likely represent metastases. Systemic chemotherapy with Ipilimumab and Nivolumab was initiated by his oncologist. He was followed for an additional 2 years with no evidence of worsening disease on surveillance PET scans before being lost to follow-up.
Case 2
A 62-year-old man presented with left-sided oculodermal melanocytosis and a pigmented, choroidal lesion extending from 10 to 2 o’clock clockwise. Ultrasonography of the lesion measured 6.1 mm in height with a base of 13.6 mm × 12.4 mm. The patient was diagnosed with choroidal melanoma of the left eye (T3aN0M0, stage IIb) and underwent iodine-125 brachytherapy with transscleral FNAB (seven samples).
Cytology confirmed the diagnosis of malignant melanoma. FISH analysis revealed an extra signal of the 6p region in 31.0% (93/300) of the nuclei examined. There was a loss of one copy of chromosome 3 in 49.3% (148/300) of nuclei.
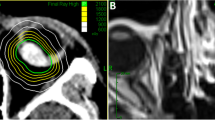
After 3 years of documented local tumour control, the intraocular tumour height remained stable at 3 mm, however B-scan ultrasonography revealed an extraocular lesion adjacent to the intraocular primary. These findings were suggestive of extraocular extension of choroidal melanoma or scleral necrosis (Fig. 1C, D). Three months later, repeat ultrasonography demonstrated an increase in size of the extraocular lesion but no change in ocular symptoms (Fig. 1E, F). MRI of the orbits confirmed ultrasonography findings and demonstrated a lesion extending from the globe posteriorly in the region of the previously treated melanoma.
The patient underwent modified subtotal exenteration with lateral orbitotomy, followed by external beam radiotherapy. Pathological studies confirmed malignant choroidal melanoma of the epithelioid type, with orbital involvement and an exudative retinal detachment.
Eight months later, he was treated with stereotactic radiosurgery for multifocal brain metastases. This therapy was repeated one year later, after which he decided to pursue palliative care hospice and died.
Case 3
A 65-year-old man presented with an elevated, choroidal lesion extending from 8 to 12 o’clock clockwise touching the optic nerve. The lesion measured 6.2 mm in height with a base of 9.8 mm × 6.2 mm (Fig. 2A, B). Systemic work up was negative, and he was diagnosed with a choroidal melanoma (T2aN0M0, Stage IIa). The patient underwent iodine-125 brachytherapy with transscleral FNAB (seven samples).
Cytopathology confirmed the diagnosis of choroidal melanoma. FISH analysis detected 3–4 copies of chromosome 6p-specific signal in 91.3% (274/300) of nuclei, indicating gain of 6p. The centromere 3 probe yielded normal results, consistent with disomy 3.
One year later, the patient presented with a 6-week history of increasing discomfort in his left eye. Fundoscopy of the left eye revealed a recurrence in the central portion of the initially treated tumour associated with diffuse exudates and serous retinal detachment. B-scan ultrasound showed an extrascleral lesion adjacent to the intraocular tumour (Fig. 2C, D). He subsequently underwent enucleation of the left eye, with excision extending beyond the retrobulbar extension of the tumour, and placement of an orbital implant.
Histopathology of the enucleated eye confirmed the diagnosis of malignant choroidal melanoma, mixed cell type with necrosis and microscopic broad front scleral invasion. The tumour was noted to have an amelanotic surface with underlying areas of haemorrhage and pigment and contained areas of infarction and early necrosis. Immuno-histochemical studies revealed epithelioid cells and frequent mitotic figures. The patient was lost to follow-up postoperatively.
Case 4
A 62-year-old man presented with an elevated, multi-lobular choroidal mass in the inferior temporal fundus of his right eye. Ultrasonography revealed an irregularly shaped lesion measuring 6.25 mm in height with a base of 13.9 mm × 13.9 mm (Fig. 3A, B). Metastatic work up was negative, and he was diagnosed with choroidal melanoma of the right eye (T3aN0M0, Stage IIb).
(A) B-scan ultrasonography revealed an irregularly shaped lesion measuring 6.25 mm in height with a base of 13.9 mm × 13.9 mm (B). Nine months after I-125 brachytherapy, fundus photograph showed no intraocular recurrence (C). Extrascleral extension of the tumour was noted on B-scan ultrasonography (D).
The patient underwent iodine-125 brachytherapy with transscleral FNAB (eight samples), pars plana vitrectomy and silicone oil (1000 centistokes) placement. During the procedure, the tumour was found to be more extensive than indicated by ultrasound, with additional ciliary body involvement. A second plaque was placed after the first was removed to cover the extent of the tumour.
Cytopathology confirmed the diagnosis of malignant melanoma. FISH analysis revealed loss of one copy of the chromosome 3 signal in 95.0% (285/300) of nuclei.
A good response to treatment was observed postoperatively with significant improvement in the serous retinal detachment at 1-month follow-up. At 3-months follow-up he was noted to have developed a cataract and macular puckering. He subsequently had cataract surgery, intraocular lens placement, and removal of the silicone oil.
Six months later during routine metastatic surveillance, he was found to have isolated aspartate aminotransferase elevation and an abnormal liver ultrasound. A PET/CT revealed positive liver and bone lesions. Fundus examination revealed regression of the intraocular tumour. Ultrasonography, however, showed an extra-scleral lesion adjacent to the site of the intraocular tumour (Fig. 3C, D). Biopsy of the liver lesions confirmed metastatic melanoma, with small nests of MART1+ and S100+ tumour cells.
The patient elected to participate in the MK3475 anti-programmed death ligand 1 (PD-1) clinical trial and received nine infusions. He tolerated the treatment well, but his liver metastases continued to progress. The orbital tumour remained asymptomatic and he required no further ocular intervention. He was lost to subsequent follow-up.
Case 5
A 74-year-old woman presented with a hyperpigmented elevated lesion at the 4 o’clock position, that measured 1.54 mm in height on ultrasound and had no associated subretinal fluid. She was treated conservatively and advised to have annual review. One year later, she was found to have an interval increase in the height of the choroidal lesion to 1.99 mm and an associated exudative retinal detachment (Fig. 4A, B). Systemic work up was negative, and she was diagnosed with a choroidal melanoma (T1aN0M0, Stage I). Iodine-125 plaque brachytherapy was performed with transscleral FNAB (three samples), pars plana vitrectomy, and silicone oil 1000 centistokes placement.
Exudative retinal detachment depicted in the fundus photograph (A) and B-scan ultrasonography (B). On follow-up 2 years post I-125 brachytherapy, fundus photograph (C) and ultrasound (D) demonstrated improvement in the lesion. Six months later, fundus photograph revealed a stable intraocular lesion with no evidence of local recurrence (E). B-scan ultrasound showed a 12.46 mm × 13.33 mm orbital mass (F).
Cytopathology confirmed the diagnosis of choroidal melanoma, and FISH was not performed due to insufficient tissue. The silicone oil was removed following resolution of the serous retinal detachment.
Two years later, fundus photograph and ultrasound demonstrated improvement in the lesion (Fig. 4C, D). Six months later, she developed proptosis on the affected left side. The choroidal lesion was unchanged on fundoscopic examination (Fig. 4E). Ultrasonography revealed an echogenic retrobulbar mass with medium internal reflectivity, measuring 12.46 mm × 13.3 mm and abutting the optic nerve (Fig. 4F).
Biopsy of the orbital mass was consistent with malignant melanoma. Exenteration was performed for local control. On pathology, there was a focal area of perforation of tumour through the sclera into the orbit suggesting direct extension of the mass, as well as a positive posterior margin. Repeat chromosome 3-6p FISH showed loss of one centromere 3-specific signal in 42.7% (128/300) nuclei.
Given the positive posterior margin, the patient underwent four months of radiation therapy to the left orbit. Three years later, she remains stable clinically without evidence of residual disease.
Discussion
In this study, we report five cases of extrascleral extension of uveal melanoma in patients who had previously undergone successful treatment of the intraocular component with plaque brachytherapy. The primary lesion, with the exception of one case, appeared to be in complete regression for an average of 2 years, and the extrascleral extension developed after this treated interval. Additionally, in three of the five cases the intraocular tumour remained well-treated after the extrascleral extension was observed.
Extrascleral extension in treatment naïve eyes occurs via various routes, including aqueous drainage channels, anterior and posterior ciliary arteries, vortex veins, long and short ciliary nerves, the optic nerve, and by direct scleral perforation [6]. Scleral thinning and necrosis have been reported following brachytherapy; however, this finding has not necessarily been associated with active tumour recurrence [10]. Extraocular extension following treatment is uncommon and in some, but not all cases, is associated with recurrence of the intraocular tumour [9]. Recurrence of the intraocular tumour in conjunction with the extra-scleral component was seen in two of the five cases in this series.
Cytogenetic and molecular genetic markers have become important prognostic tools and predictors of metastatic disease [11,12,13]. Chromosomal abnormalities that are associated with a higher risk of metastatic disease are monosomy 3, monosomy 6p and gains in chromosome 8q [11,12,13]. Gains in chromosome 6p are associated with a more favourable prognosis [12]. Sequencing of DNA in uveal melanoma has allowed for the identification of mutated genes, most significantly mutations in the BRCA-associated protein (BAP1) gene. BAP1 is a tumour suppressor gene, and mutations resulting in its inactivation or loss are associated with a higher metastatic risk [14, 15].
Four of the five cases in this series had molecular characteristics associated with high metastatic risk, with three patients demonstrating monosomy 3 and one being positive for the BAP1 mutation. The finding that molecular characteristics are associated with higher mortality rates and metastatic disease suggests that tumour biology is likely a key factor influencing the rates of metastasis and extrascleral extension. However, there are other factors that could be involved, including extension through the needle tract from FNAB or the vitrectomy ports from pars plana vitrectomy. This is particularly relevant for the cases without intraocular recurrence. Three of the five cases underwent pars plana vitrectomy with silicone oil at the time of plaque placement, with removal of silicone oil within 6 months. Two of these three cases did not have intraocular recurrence. While insertion and removal of the trocars could be a possible contributing factor to later orbital recurrence, some of the cases presented did not undergo vitrectomy. The small sample size of this series and complex pathophysiology of extrascleral extension render it difficult to determine the aetiology of recurrence. A larger comparative study investigating the incidence of choroidal melanoma recurrence after iodine-125 brachytherapy, as well as prevalence of monosomy 3/BAP1 in these cases, could be an area of future investigation and help elucidate risk factors for recurrence (Table 1).
Our series suggests that in spite of optimal treatment, melanoma with high biological risk can recur, and recurrence can be aggressive with extrascleral extension. Extrascleral disease can occur despite control of the intraocular tumour, and there can be a prolonged latency before extrascleral extension. Aggressive tumour biology is likely a precipitant, as four of the five patients in this series demonstrated molecular markers associated with high-risk tumour biology, though the pathophysiology is complex and there may be other factors involved as well. This series underscores the importance of extended follow-up in treated choroidal melanoma patients, with special consideration for detailed orbital examination with ultrasonography over time.
Summary table
What was known before
-
Choroidal melanoma may extend into the orbit via direct invasion through the sclera.
-
Reports of extraocular extension following treatment with plaque brachytherapy are few and have been attributed to treatment failure with recurrence of the intraocular tumour.
What this study adds
-
Extrascleral extension of choroidal melanoma can occur despite control of the intraocular tumour, and there can be a prolonged latency before extrascleral extension.
-
Aggressive tumour biology is likely a precipitant, as four of the five patients in this series demonstrated molecular markers associated with high risk tumour biology; however, there may be other factors involved as well.
References
Spagnolo F, Caltabiano G, Queirolo P. Uveal melanoma. Cancer Treat Rev. 2012;38:549–53.
Damato B. Treatment of primary intraocular melanoma. Expert Rev Anticancer Ther. 2006;6:493–506.
Margo CE. The Collaborative Ocular Melanoma Study: an overview. Cancer Control. 2004;11:304–9.
Kujala E, Mäkitie T, Kivelä T. Very long-term prognosis of patients with malignant uveal melanoma. Investig Ophthalmol Vis Sci. 2003;44:4651–9.
Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR, et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989–98.
Coupland SE, Campbell I, Damato B. Routes of extraocular extension of uveal melanoma: risk factors and influence on survival probability. Ophthalmology. 2008;115:1778–85.
Shields CL, Shields JA, Peggs M. Tumors metastatic to the orbit. Ophthal Plast Reconstr Surg. 1988;4:73–80.
Shields JA, Shields CL, Shakin EP, Kobetz LE. Metastasis of choroidal melanoma to the contralateral choroid, orbit, and eyelid. Br J Ophthalmol. 1988;72:456–60.
Sánchez-Tabernero S, García-Alvarez C, Muñoz-Moreno MF, Diezhandino P, Alonso-Martínez P, de Frutos-Baraja JM, et al. Pattern of local recurrence after i-125 episcleral brachytherapy for uveal melanoma in a Spanish referral ocular oncology unit. Am J Ophthalmol. 2017;180:39–45.
Pham CM, Couch SM, Harocopos GJ. Extrascleral tumor extension associated with localized scleral melt following plaque brachytherapy for uveal melanoma: clinical and histologic findings. Ocul Oncol Pathol. 2018;4:93–99.
Shields CL, Say EAT, Hasanreisoglu M, Saktanasate J, Lawson BM, Landy JE, et al. Cytogenetic abnormalities in uveal melanoma based on tumor features and size in 1059 patients: the 2016 W. Richard Green lecture. Ophthalmology. 2017;124:609–18.
McCannel TA. Fine-needle aspiration biopsy in the management of choroidal melanoma. Curr Opin Ophthalmol. 2013;24:262–6.
Damato B, Coupland SE. Translating uveal melanoma cytogenetics into clinical care. Arch Ophthalmol. 2009;127:423–9.
Yavuzyigitoglu S, Koopmans AE, Verdijk RM, Vaarwater J, Eussen B, van Bodegom A, et al. Uveal melanomas with SF3B1 mutations: a distinct subclass associated with late-onset metastases. Ophthalmology. 2016;123:1118–28.
Plasseraud KM, Cook RW, Tsai T, Shildkrot Y, Middlebrook B, Maetzold D, et al. Clinical performance and management outcomes with the DecisionDx-UM gene expression profile test in a prospective multicenter study. J Oncol. 2016;2016:5325762.
Funding
Unrestricted grant from Research to Prevent Blindness; The George E. and Ruth Moss Trust.
Author information
Authors and Affiliations
Contributions
HM was responsible for study design, institutional review board approval, data collection, analysis of data, constructing the tables and figures, and drafting and revising the manuscript. CL and LC were responsible for the study design, collection of data, and drafting and revising the manuscript. AT and RA were responsible for the collection of data and drafting and revising the manuscript. TM, RG and DS were responsible for the study design and drafting and revising the manuscript. All authors approve the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mustak, H., Lo, C., Cohen, L.M. et al. Extrascleral extension of choroidal melanoma after iodine-125 brachytherapy treatment: a case series. Eye 37, 249–255 (2023). https://doi.org/10.1038/s41433-021-01861-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01861-y