Abstract
Purpose
To compare the foveal microstructures, such as the prevalence of epiretinal proliferation (EP) and residual ellipsoid zone (EZ), in eyes with lamellar macular hole (LMH), epiretinal retinal membrane (ERM) foveoschisis and macular pseudohole (MPH), and to investigate the association of the foveal microstructure with visual functions.
Method
In addition to the prevalence of EP, we calculated the residual EZ index within 1mm and 3 mm (rEZ1 and rEZ3) in all examined eyes. Comparisons were conducted to baseline characteristics (logMAR visual acuity [logMAR VA], metamorphopsia score [Mave], central retinal thickness [CRT], the prevalence of EP, rEZ1 and rEZ3) between MPH, ERM foveoschisis and LMH subgroups. The relationships (1) between logMAR VA and each of age, type (MPH, ERM foveoschisis and LMH), the prevalence of EP, rEZ1, rEZ3, spherical equivalent (SE) and CRT and (2) between Mave and each of variables were investigated.
Results
Fifty-one eyes of 48 patients were enroled. The mean age was 65.2 ± 11.1 years. Ten eyes were diagnosed as LMH, 22 eyes as ERM foveoschisis and 19 eyes as MPH, respectively. There was a significant difference in CRT only between LMH and ERM foveoschisis (p = 0.023). There was a tendency toward significance in rEZ1 between LMH and ERM foveoschisis (p = 0.057), but not in rEZ3. The optimal model for logMAR VA included age, rEZ1, SE and CRT. On the other hand, the optimal model for Mave included the prevalence of EP, rEZ1 and SE.
Conclusion
Microstructural observations are useful to predict visual functions in LMH, ERM foveoshisis and MPH.
Similar content being viewed by others
Introduction
Lamellar macular hole (LMH) was first reported by Gass in 1976 and is characterised by an irregular foveal contour, rupture of the inner foveal surface, and dissociation between the inner and outer foveal retinas [1, 2]. Until recently, however, the definition of LMH was ambiguous, and a consensus on the diagnostic criteria for the differential diagnosis of maculopathies such as LMH, epiretinal membrane (ERM) foveoschisis, and macular pseudohole (MPH) did not exist. Consequently, an expert panel recently proposed clear consensus diagnostic criteria for the differentiation of LMH from ERM foveoschisis and MPH using optical coherence tomography (OCT) [3]. These uniform definitions and terminology now enable precise research on LMH, ERM foveoschisis and MPH to be performed. Indeed, some studies have already reported the surgical outcomes of patients with these clinical entities [4, 5].
Several important features of OCT impact the utility of this modality in the diagnosis of LMH. In addition to ellipsoid zone (EZ) disruption, the integrity of residual EZ may be useful for predicting visual function [6, 7]. Additionally, epiretinal proliferation (EP), previously known as lamellar hole-associated epiretinal proliferation, is often associated with LMH. Associations between EZ parameters and visual function have been established for several retinal diseases [8,9,10]. Furthermore, we previously investigated the outcome of vitrectomy for the treatment of LMH and ERM foveoschisis and demonstrated that the preoperative visual acuity (VA) and the presence of EZ disruption, but not EP, were related to the final VA [5]. EP represents a non-tractional type of ERM with an unusual appearance, compared with normal ERM [2], raising the possibility that EP might be related to metamorphopsia. To the best of our knowledge, the prevalence of EP and the association between EP and metamorphopsia in eyes with MPH, ERM foveoschisis or LMH have not been previously investigated.
In the current study, we aimed to compare the clinical characteristics, such as the prevalence of EP and the status of the EZ, in eyes with MPH, ERM foveoschisis or LMH. In addition, the associations between clinical characteristics and visual function (VA and metamorphopsia) were analysed for these clinical entities using the residual EZ quantification using binarized OCT images, which has been shown to be a reliable marker of EZ integrity in other retinal conditions [6, 7].
Methods
This study was approved by the Research Ethics Committee of Yokohama City University School of Medicine. Written informed consent for all clinical information to be stored in the hospital database and to be used for research purposes was obtained from each participant. This study was performed according to the tenets of the Declaration of Helsinki.
We retrospectively reviewed the medical records of patients with MPH, ERM foveoschisis or LMH. Patients with a history of vitrectomy surgery were excluded from the present study. Patients with a history of retinal disease such as diabetic retinopathy or retinal vein occlusion were also excluded. In addition to comprehensive ophthalmologic examinations such as VA, M-CHARTS (Inami Co., Tokyo, Japan) were used to evaluate the degree of metamorphopsia. The metamorphopsia scores of vertical and horizontal line (MV and MH) were collected on each eye.
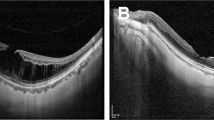
OCT measurements
All patients underwent examinations using Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany). The OCT images consisted of horizontal and vertical scans with a scan size of 30 degrees. We used the new definitions for LMH, ERM foveoschisis and MPH, as previously described [3] (Fig. 1). The mandatory criteria for the diagnosis of LMH were the presence of (1) an irregular foveal contour, (2) a foveal cavity with undermined edges and (3) the presence of at least one other sign evoking a loss of foveal tissue such as a pseudo-operculum or thinning of the fovea at its centre or central vicinity. Associated pathological changes including EP, a foveal bump and EZ disruption were also noted. The mandatory criteria for the diagnosis of ERM foveoschisis were the presence of (1) a contractile ERM and (2) foveoschisis at the level of Henle’s fibre layer (HFL, corresponding to the layer between the outer plexiform and outer nuclear layers). Optional criteria were the presence of (1) microcystoid spaces in the inner nuclear layer (INL), (2) retinal thickening and (3) retinal wrinkling. The mandatory criteria for MPH were (1) a foveal centre sparing the ERM, (2) retinal thickening and (3) a verticalized or steepened foveal profile. Minor criteria were (1) the presence of microcystoid spaces in the INL and (2) an almost normal central foveal thickness. To examine diagnostic reproducibility, each diagnosis was made by two examiners (KeN and TI). A consensus between the investigators was reached for all the examined eyes.
Horizontal OCT images in eyes with LMH (A), ERM foveoschisis (B), or MPH (C). A The EP is observed as a thick, homogeneous and isoreflective preretinal material over the internal limiting membrane (white arrow) and the EZ line is disrupted (yellow arrow) in LMH. B Foveoschisis is visible as a sharp separation between the outer nuclear layer and outer plexiform layer (yellow arrow). C MPH demonstrates retinal thickening and verticalized foveal profile. OCT optical coherence tomography, LMH lamellar macular hole, ERM epiretinal membrane, MPH macular pseudohole, EP epiretinal proliferation, EZ ellipsoid zone.
Quantification of residual ellipsoid zone
We calculated the residual EZ index (rEZ) for all the examined eyes using a previously described method [6] (Fig. 2). Horizontal and vertical scans through the fovea were obtained for each eye. The OCT images were then binarized using the Niblack method and publicly accessible ImageJ software (U.S. National Institute of Health, MD). Then, EZ lines with lengths of 1 mm and 3 mm were manually traced on the binarized image. Finally, the proportion of white area on the traced line was automatically calculated for both the horizontal and vertical directions in each examined eye. The averages of the horizontal and vertical residual EZ indices were regarded as rEZ1 and rEZ3, respectively.
A The horizontal and vertical OCT images were used to calculate the residual EZ index. White line below indicates 1 mm. Then, the image was binarized using the Niblack method with ImageJ software. B The EZ was traced within 1 mm (green line) and the proportion of white area on the traced line was calculated as rEZ1. EZ ellipsoid zone, OCT optical coherence tomography.
Statistical analysis
The baseline characteristics (age, logarithm of the minimum angle of resolution [logMAR] VA, MV score, MH score, average of MV and MH scores [Mave], central retinal thickness [CRT], spherical equivalent [SE], and presence of EP, rEZ1 and rEZ3) of the MPH, ERM foveoschisis and LMH groups were compared using the linear mixed model and Tukey multiple comparison test.
The relationships between (1) the logMAR VA and age, disease type (MPH, ERM foveoschisis or LMH), presence of EP, rEZ1, rEZ3, SE and CRT and (2) Mave and age, disease type, presence of EP, rEZ1, rEZ3, SE and CRT were investigated using a linear mixed model. In addition, Akaike information criterion (AICc) model selection was used to determine the best explanatory variables for logMAR VA and Mave, respectively. The selected variables were regarded as being statistically significant. All statistical analyses were performed using statistical software (The R Foundation for Statistical Computing, version 3.4.3, Vienna, Austria).
Results
Table 1 shows the demographic data of the participants in the current study.
Fifty-one eyes in 48 patients (17 men and 31 women) were enroled. The mean (± standard deviation [SD]) age of the participants was 65.2 ± 11.1 years. Ten eyes were diagnosed as LMH, 22 eyes were diagnosed as ERM foveoschisis and 19 eyes were diagnosed as MPH. The mean logMAR VA of all 51 eyes was 0.16 ± 0.20. The Mave score was 0.38 ± 0.44, and the CRT was 159.1 ± 72.8 µm. The SE value was −4.18 ± 5.98 dioptre. Forty-three were phakic and eight were pseudophakic eyes. Twenty of the 51 eyes (39.2%) had EP, and the rEZ1 and rEZ3 values were 0.84 ± 0.25 and 0.88 ± 0.17, respectively.
In group analyses, the mean ± SD ages were 68.5 ± 8.8, 63.0 ± 9.8, and 66.1 ± 12.9 years in the LMH, ERM foveoschisis and MPH groups, respectively. A linear mixed model and Tukey multiple comparison test suggested no significant differences in age among the three groups (all p > 0.05). The logMAR VA values in the LMH, ERM foveoschisis and MPH groups were 0.22 ± 0.19, 0.19 ± 0.20 and 0.094 ± 0.17, respectively. No significant differences in logMAR VA were observed between groups (all p > 0.05, linear mixed model and Tukey multiple comparison test, Fig. 3A). The Mave values in the LMH, ERM foveoschisis, and MPH groups were 0.15 ± 0.14, 0.49 ± 0.51 and 0.37 ± 0.41, respectively. No significant differences in Mave were observed between groups (all p > 0.05, linear mixed model and Tukey multiple comparison test, Fig. 3B). The CRT values in the LMH, ERM foveoschisis, and MPH groups were 117.8 ± 50.7 μm, 184.0 ± 85.2 μm, and 151.9 ± 52.7 μm, respectively. A significant difference in CRT was seen between the LMH and ERM foveoschisis groups (p = 0.023), but no significant difference was seen between the LMH and MPH groups (p = 0.49) or between the MPH and ERM foveoschisis groups (p = 0.18, linear mixed model and Tukey multiple comparison test). The SE values were −5.63 ± 6.46, −3.89 ± 5.22 and −3.74 ± 6.41 in the LMH, ERM foveoschisis and MPH groups, respectively. A tendency toward a significant difference in SE was seen between the LMH and ERM foveoschisis groups (p = 0.067). However, no significant difference was seen between the LMH and MPH groups (p = 0.47) or between the MPH and ERM foveoschisis groups (p = 0.48, linear mixed model and Tukey multiple comparison test). Similar results were obtained for rEZ1 (LMH vs. ERM foveoschisis, p = 0.057; LMH vs. MPH, p = 0.39; and MPH vs. ERM foveoschisis p = 0.51). However, no significant differences in rEZ3 were seen among the groups (p > 0.05).
A The logMAR VA values were 0.22 ± 0.19 in the LMH group, 0.19 ± 0.20 in the ERM foveoschisis group and 0.094 ± 0.17 in the MPH group. No significant differences between groups were seen (all p > 0.05, linear mixed model and Tukey multiple comparison test). B The Mave values were 0.15 ± 0.14 in the LMH group, 0.49 ± 0.51 in the ERM foveoschisis group and 0.37 ± 0.41 in the MPH group; no significant differences between groups were seen. LogMAR logarithm of the minimum angle of resolution, VA visual acuity, Mave average of the vertical and horizontal metamorphopsia scores.
Using AICc model selection, the optimal model for logMAR VA included age, rEZ1, SE and CRT (AICc = −31.2, Table 2). The optimal model for logMAR VA was as follows:
LogMAR VA = −0.090 + 0.0051 (±0.0022) × age − 0.25 (±0.098) × rEZ1 − 0.010 (±0.0039) × SE + 0.00052 (±0.00032) × CRT.
On the other hand, the optimal model for Mave included the presence of EP, rEZ1 and SE (AICc = 58.8, Table 2):
Mave = 1.10–0.33 (±0.11) × EP – 0.59 (±0.22) × rEZ1 + 0.023 (±0.0094) × SE.
Discussion
In the present study, we investigated the relationships between visual functions (VA and metamorphopsia) and the retinal microstructure in eyes with LMH, ERM foveoschisis or MPH. As a result, the residual EZ index within the central 1-mm area (rEZ1) was found to be significantly correlated with VA. Moreover, the rEZ1 and the presence of EP were associated with metamorphopsia.
An association between the integrity of the EZ line and visual function has been reported for several retinal diseases [8,9,10]. VA is considered to reflect retinal function, especially in the foveal region. EZ was previously referred as “photoreceptor inner segment/outer segment (IS/OS) junction”, and is now considered to be a good biomarker of retinal photoreceptor cell function. Thus, the integrity of the EZ line in the fovea is one of determinant factors for visual acuity. Fujita et al. reported a significant relationship between the integrity of the EZ within a 1 × 1 mm area at the macula and VA as well as between the integrity of the EZ within a 3 × 3-mm area and retinal sensitivity, rather than VA, in eyes with chronic CSC [6]. Consistent with these previous findings, the rEZ1 was strongly correlated with logMAR VA in eyes with LMH, ERM foveoschisis or MPH in the presently reported study. To predict VA, rEZ1 appears to be sufficient, compared with rEZ3. In the present study, the rEZ1 values were 0.67 ± 0.28 in the LMH group, 0.89 ± 0.19 in the ERM foveoschisis group and 0.86 ± 0.26 in the MPH group; however, a tendency toward a significant difference was only observed between the LMH and ERM foveoschisis groups (p = 0.057). The relatively poor VA might be due to the lower residual EZ index in the LMH group; however, further study with a larger sample size is needed to clarify the correlation between the residual EZ index and VA in eyes with LMH, ERM foveoschisis or MPH.
EP has an unusual appearance, compared with normal ERM. Previous histological studies have suggested that EP consists of retinal glial cells, specifically Müller cells, while normal ERM consists of hyalocytes, fibroblasts and myofibroblasts, which might provide tractional properties [11]. Among the newly defined clinical entities, EP was observed in 100% of LMH cases, 31.8% of ERM foveoschisis cases, and 15.8% of MPH cases. The differences in the prevalence of EP may directly influence the degree of metamorphopsia in eyes with LMH, ERM foveoschisis, or MPH. Of note, rEZ1 was also negatively associated with metamorphopsia in the present study. Both the presence of EP and a relatively low rEZ were observed in the LMH group, although these parameters have opposite effects on metamorphopsia. A longitudinal study is needed to examine whether the development of EP precedes EZ disruption in eyes with LMH.
Our current result suggested that the SE values were significantly related to visual functions in eyes with LMH, ERM foveoschisis or MPH. A tendency toward a significant difference in SE was seen between the LMH and ERM foveoschisis groups (p = 0.067), on the other hand, no significant difference was seen between the LMH and MPH groups (p = 0.47) or between the MPH and ERM foveoschisis groups (p = 0.48, linear mixed model and Tukey multiple comparison test). Similar result was observed for rEZ1. It is possible that the SE might directly influence rEZ or the prevalence of EP. EP is found in various retinal disorders, including high myopia [12]. Previous reports suggested that LMH eyes with high myopia presented EP, indicating the higher prevalence compared with non-myopic LMH eyes [13, 14]. However, our present results suggested the SE was selected as an explanatory variable for visual functions, independent of rEZ1 or the presence of EP. Furthermore, the SE was not associated with both rEZ1 and the presence of EP (p = 0.079, p = 0.37, respectively, linear mixed model). The reason for these discrepant results still remains unclear, and a further study would be needed to precisely investigate the relationship between these parameters and axial length in eyes with LMH, ERM foveoschisis and MPH.
The present included some limitations. First, this study was retrospective and cross-sectional in nature, therefore the follow-up data were missing and this is a big drawback of our current analyses. Since visual functions and microstructural changes were assessed at the first visit, the relationships in these clinical entities still remain unclear. The impact of microstructural changes on the outcomes after intervention would make it a robust study. A further study is needed shedding light on this issue. Moreover, the temporal changes in OCT findings were not investigated. It would be interesting to monitor the progression of EZ disruption and/or the formation of EP in each of these clinical entities.
In conclusion, the residual EZ index is associated with logMAR VA in eyes with LMH, ERM foveoschisis or MPH. In addition, the residual EZ index and the presence of EP are associated with metamorphopsia. Microstructural observations are useful for evaluating visual function in these clinical entities.
Summary
What was known before
-
The criteria for the differential diagnosis of maculopathies such as LMH, epiretinal membrane (ERM) foveoschisis, and macular pseudohole (MPH) was recently proposed.
-
The relationship between the foveal microstructures and optical coherence tomography parameter has not been compared.
What this study adds
-
Residual EZ index was correlated with VA. In addition, residual EZ index and the presence of EP were associated with metamorphopsia.
-
Microstructural observation is useful for predicting visual function in these clinical entities.
References
Gass JD. Lamellar macular hole: a complication of cystoid macular edema after cataract extraction. Arch Ophthalmol. 1976;94:793–800.
Witkin AJ, Ko TH, Fujimoto JG, Schuman JS, Baumal CR, Rogers AH, et al. Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology. 2006;113:388–97.
Hubschman JP, Govetto A, Spaide RF, Schumann R, Steel D, Figueroa MS, et al. Optical coherence tomography-based consensus definition for lamellar macular hole. Br J Ophthalmol. 2020;104:1741–7.
Lam M, Philippakis E, Gaudric A, Tadayoni R, Couturier A. Postoperative outcomes of idiopathic epiretinal membrane associated with foveoschisis. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2020-317982.
Omoto T, Asahina Y, Zhou HP, Fujino R, Takao M, Obata R, et al. Visual outcomes and prognostic factors of vitrectomy for lamellar macular holes and epiretinal membrane foveoschisis. PLoS ONE. 2021;16:e0247509. https://doi.org/10.1371/journal.pone.0247509.
Fujita A, Aoyama Y, Tsuneyoshi S, Sugiura A, Azuma K, Asano-Shimizu K, et al. Association between visual function and the integrity of residual ellipsoid zone in resolved central serous chorioretinopathy. Sci Rep. 2019;9:12433. https://doi.org/10.1038/s41598-019-48825-7.
Hara T, Zhou HP, Kitano M, Kure K, Asaoka R, Inoue T, et al. Quantification of residual ellipsoid zone and its correlation with visual functions in patients with cone-rod dystrophy. Eur J Ophthalmol. 2021;26:1120672121990561. https://doi.org/10.1177/1120672121990561.
Ota M, Tsujikawa A, Murakami T, Yamaike N, Sakamoto A, Kotera Y, et al. Foveal photoreceptor layer in eyes with persistent cystoid macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2008;145:273–80.
Inoue M, Morita S, Watanabe Y, Kaneko T, Yamane S, Kobayashi S, et al. Inner segment/outer segment junction assessed by spectral-domain optical coherence tomography in patients with idiopathic epiretinal membrane. Am J Ophthalmol. 2010;150:834–9.
Aizawa S, Mitamura Y, Baba T, Hagiwara A, Ogata K, Yamamoto S. Correlation between visual function and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Eye. 2009;23:304–8.
Schumann RG, Hagenau F, Guenther SR, Wolf A, Priglinger SG, Vogt D. Premacular cell proliferation profiles in tangential traction vitreo-maculopathies suggest a key role for hyalocytes. Ophthalmologica. 2019;242:106–12.
Chehaibou I, Pettenkofer M, Govetto A, Rabina G, Sadda SR, Hubschman JP. Identification of epiretinal proliferation in various retinal diseases and vitreoretinal interface disorders. Int J Retin Vitreous. 2020;6:31. https://doi.org/10.1186/s40942-020-00233-0.
dell’Omo R, Virgili G, Bottoni F, Parolini B, De Turris S, Di Salvatore A, et al. Lamellar macular holes in the eyes with pathological myopia. Graefes Arch Clin Exp Ophthalmol. 2018;256:1281–90. https://doi.org/10.1007/s00417-018-3995-8.
Lai TT, Yang CM. Lamellar hole-associated epiretinal proliferation in lamellar macular hole and full-thickness macular hole in high myopia. Retina. 2018;38:1316–23. https://doi.org/10.1097/IAE.0000000000001708.
Author information
Authors and Affiliations
Contributions
TI, YY, KeN and RyoA were responsible for writing the report, conducting the search, extracting and analysing data, interpreting results, updating reference lists. KoN, YT and ReiA contributed to extracting data. KK and MI provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakamura, K., Inoue, T., Nagura, K. et al. Foveal microstructure and visual function in patients with lamellar macular hole, epiretinal membrane foveoschisis or macular pseudohole. Eye 36, 2247–2252 (2022). https://doi.org/10.1038/s41433-021-01818-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01818-1
This article is cited by
-
Clinical characteristics of patients with epiretinal membrane-Foveoschisis
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)